Physical Evaluation of the Hip
to the surgeon to aid in the diagnosis of hip disease. Thorough history
and physical examination, however, remain the most important tools that
a physician possesses when evaluating a painful hip joint. Diagnostic
tests and procedures should be used in addition to and not as a substitute for a careful history and complete physical examination.
patient with suspected hip disease is the first and one of the most
critical steps in being able to properly diagnose pathology. This can
often lead to a preliminary diagnosis and will allow for a more
directed physical examination. A patient with hip pathology most
frequently complains of pain. True hip pathology usually presents with
pain located in the groin, anterior thigh, deep buttock, and
occasionally knee. Every patient who presents with knee pain or medial
thigh pain should have a thorough hip evaluation to rule out hip
pathology as a source of referred pain to the knee. Important questions
regarding the characteristics of pain include location, severity,
frequency, and radicular features. It is also important to note
circumstances that aggravate or relieve the pain. Arthritic pain
generally is aggravated by activity and relieved by rest. Pain that
occurs at night or during rest is less common in degenerative arthritis
and may indicate the presence of an inflammatory process or infection.
Referred pain from the lumbosacral region is common. This type of pain
is often located in the gluteal or posterior iliac crest region and may
present with radicular signs and symptoms. Several other conditions may
refer pain to the hip (Table 1-1). Nonarthritic hip conditions should also be evaluated (Table 1-2).
-
Previous history of hip pathology
(Perthes disease, slipped capital epiphysis, hip dysplasia, sepsis)
including surgery or other treatment -
History of trauma
-
Medication history including use of pain medications (e.g., narcotics) or corticosteroids.
-
Limitations of activities of daily living (walking, going up and down stairs, sitting)
-
Limitation of functional activities (getting into or out of car, getting shoes and socks on, foot hygiene)
-
Limitation of occupational and recreational activities
encounter. Noting how the patient rises from a chair, walks to the exam
room, and assumes certain postures can provide valuable information in
a non-exam-specific setting. Every patient should be disrobed and
appropriately gowned to allow for a thorough inspection of the hip and
surrounding areas.
(40%): initial, midswing, and terminal swing. Several types of abnormal
gait patterns can be indicative of hip pathology and are listed in Table 1-3.
Patients who experience pain with weight bearing on the affected limb
(antalgic or avoidance gait) will try to minimize the time on this limb
during the stance phase of gait, resulting in a limp. Abductor muscle
weakness will result in the pelvis tilting away from the affected limb
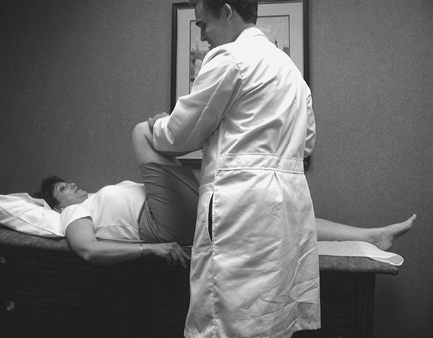
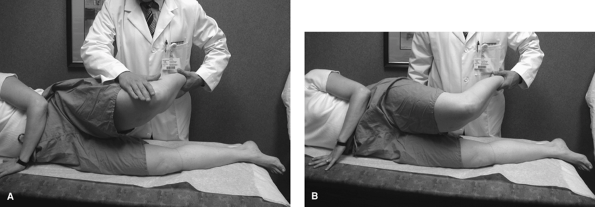
when that limb is in the stance phase of gait (Fig. 1-1).
To compensate, patients may lean over their affected hip to shift the
center of gravity, resulting in a so-called Duchenne gait. Patients
with a true leg length discrepancy may circumduct the long leg during
the swing phase of gait to allow for the limb to clear the floor.
particularly those planning to undergo arthroplasty. Several different
methods can be used.
|
TABLE 1-1 Conditions That May Refer Pain to The HIP
|
|
|---|---|
|
|
TABLE 1-2 Nonarthritic HIP Conditions
|
|
|---|---|
|
|
TABLE 1-3 Abnormal Gait Patterns
|
|
|---|---|
|
 |
|
Figure 1-1
The examiner places his hands on the patient’s pelvis. The patient is then asked to stand on the affected limb. If the abductors are functioning properly, the pelvis will remain level. With a weak or deficient abductor mechanism, the pelvis will tilt away from the affected limb. |
-
With the patient standing flat on ground,
the examiner sits behind the patient and places his or her hands on the
pelvic brim. Any asymmetry in pelvic height is noted. Measured blocks
can be placed under the short limb until the pelvis becomes level. The
height of the block used to level the pelvis can give an estimation of
the leg length discrepancy. The measurement will be affected by a fixed pelvic obliquity.![]() Figure 1-2 Hip flexion: Average ROM is 0 to 125 degrees.
Figure 1-2 Hip flexion: Average ROM is 0 to 125 degrees. -
Apparent leg length: With the patient supine on the exam table, measure each leg from the umbilicus to a fixed point on the medial malleolus. This measurement will also be affected by a fixed pelvic obliquity.
-
True leg length:
With the patient supine on the exam table, measure each leg from the
anterior superior iliac spine (ASIS) to a fixed point on the medial
malleolus. This measurement will not be affected by a fixed pelvic obliquity.
look for outward signs of trauma (swelling, ecchymosis) and infection
(warmth, erythema). All previous scars should be evaluated and noted.
Other sources of cutaneous pain about the hip such as lesions
associated with herpes zoster should be evaluated. Palpation of soft
tissue and bony landmarks around the hip is important to rule out
nonarticular causes of pain such as bursitis. Important bony landmarks
that may be palpated include the following:
 |
|
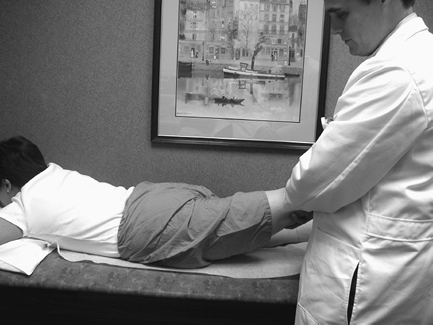
Figure 1-3 Hip extension: Average ROM is 0 to 25 degrees.
|
 |
|
Figure 1-4 Abduction: Average ROM is 0 to 40 degrees. Note that examiner’s hand stabilizes pelvis to prevent pelvic tilt.
|
-
Lumbar spine and sacrum
-
Greater trochanter
-
Anterior superior iliac spine (ASIS)
-
Posterior superior iliac spine (PSIS)
-
Ischial tuberosity
compared with the unaffected side. Patients with osteoarthritis will
have limited range of motion, and the extremes of motion may cause pain
and discomfort that is similar to their symptoms. In general, patients
with osteoarthritis tend to lose hip flexion and internal rotation
first (Figs. 1-2, 1-3, 1-4, 1-5, 1-6, 1-7).
 |
|
Figure 1-5 Hip adduction: Normal ROM is 0 to 30 degrees.
|
 |
|
Figure 1-6 Internal rotation of the hip: Normal ROM is 0 to 30 degrees.
|
 |
|
Figure 1-7 External rotation of the hip: Normal ROM is 0 to 60 degrees.
|
 |
|
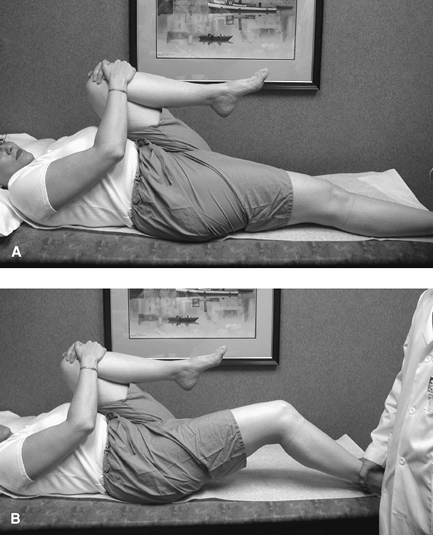
Figure 1-8 A. NormalB. Hip flexion contracture.
|
Both knees are brought to the chest and held with the arms (this
removes any lumbar lordosis). The leg to be tested is then released and
allowed to come back to the table while the opposite leg remains held
to the chest. A patient with a hip flexion contracture will be unable
to fully extend the hip back to the exam table. Estimate the
contracture by measuring the angle created by the patient’s leg and the
exam table.
the leg is slowly abducted with the knee flexed. From this position,
the leg is released. A patient with a tight iliotibial band will remain
in the abducted position whereas for those with a normal iliotibial
band, the leg will fall into an adducted position.
so the foot is placed against the contralateral knee. Pressure can then
be applied by placing one hand on the opposite pelvis and pressing down
the affected limb. Posterior pain indicates sacroiliac
joint pathology, whereas anterior groin pain is indicative of hip pathology.
 |
|
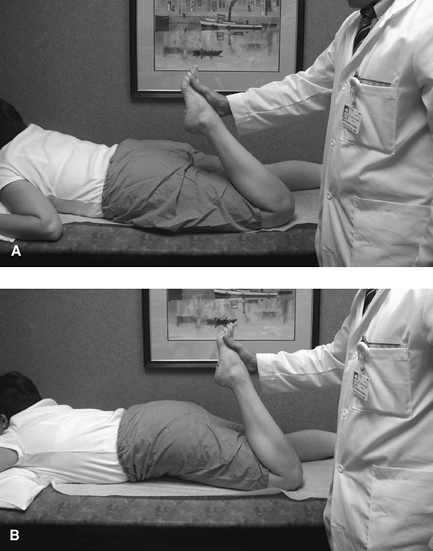
Figure 1-9 A. Normal test. B. Rectus femoris contracture.
|
the hip is flexed approximately 30 degrees with the knee fully
extended. The patient is then asked to resist the examiner’s downward
force by maintaining the hip in the flexed position. A positive test
reproduces pain across the hip joint.
 |
|
Figure 1-10 Iliotibial band tightness.
|
and vascular examination. Palpation and documentation of pulses in both
extremities is mandatory. This may include palpation of the femoral,
popliteal, and posterior tibialis and dorsalis pedis pulses.
muscle testing and assessment of sensation. Hip muscles can be grouped
into flexors, extensors, and medial and lateral rotators. Table 1-4
lists the muscles, innervation, and nerve root derivation of the hip
muscles. The strength of pertinent muscle groups should be graded and
documented. Strength can be graded on a standard scale of 0 to 5:
-
5/5: normal strength against resistance
-
4/5: normal strength against gravity with some resistance
-
3/5: strength against gravity with no resistance
-
2/5: movement with gravity eliminated
-
1/5: muscle contractility
-
0/5: no muscle contractility
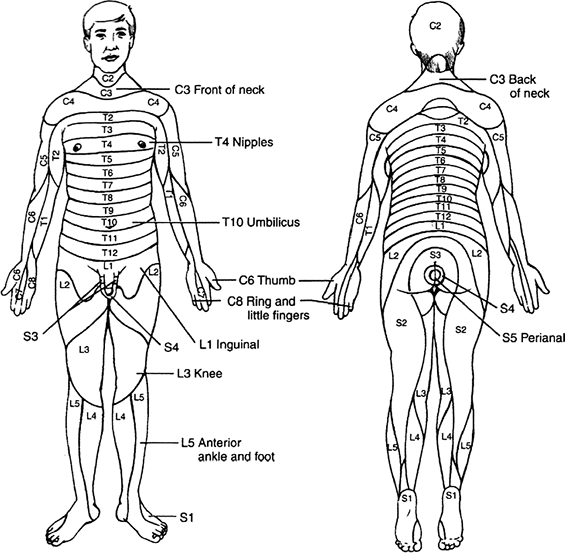
If any abnormalities are noted, a more thorough examination to include
assessment of pain, temperature, and vibration may be conducted.
Reflexes including the patellar (L2-4) and Achilles (S1) may be
evaluated and compared with the contralateral side.
arthroplasty, several questions are important in evaluating the cause.
Symptoms prior to surgery, dates of surgery, pain-free period after
surgery and onset of new symptoms must be evaluated. Patients who never
had any pain relief after surgery should be evaluated for other causes
of referred pain to the hip (Tables 1-1 and 1-2). All preoperative and immediate postoperative radiographs should be obtained and evaluated. Patients with no or only a limited
period of pain relief who continue to have discomfort that is not relieved by rest sould be evaluated for infection.
|
TABLE 1-4 Actions and Innervations of the Muscles of the HIP
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 1-11 Sacral and hip joint pathology.
|
 |
|
Figure 1-12 Loading hip joint in supine position.
|
 |
|
Figure 1-13 Dermatomes of the upper and lower extremity.
|
the femoral or acetabular component) have generally had a pain-free
period, then developed pain that has become progressive in frequency,
duration, and intensity over time. Patients generally do not have pain
at rest. They will often demonstrate a triphasic pain pattern,
characterized by pain with initial weight bearing that subsides as they
continue to walk (and the prosthesis finds a stable position) and then
returns as the patient continues to bear weight.
hip arthroplasty may demonstrate an antalgic gait or weakness of
surrounding muscles. They also may demonstrate instability or
apprehension at the extremes of motion.