Scapula Fractures
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > III – Upper Extremity Fractures and Dislocations > 13 – Scapula Fractures
13
Scapula Fractures
EPIDEMIOLOGY
-
This relatively uncommon injury represents only 3% to 5% of all shoulder fractures and 0.5% to 1% of all fractures.
-
The mean age of patients with fracture of the scapula is 35 to 45 years.
ANATOMY
-
This flat, triangular bone links the upper extremity to the axial skeleton.
-
Protection from impact is provided by the
large surrounding muscle mass as well as the mobility of the scapula on
the chest wall, further aiding in force dissipation.
MECHANISM OF INJURY
-
Significant trauma is required to
fracture the scapula, as is evidenced by the common cause of
injury—motor vehicle accident in approximately 50% of cases and
motorcycle accident in 11% to 25%. -
Indirect injury occurs through axial loading on the outstretched arm (scapular neck, glenoid, intraarticular fracture).
-
Direct trauma, often high energy, occurs
from a blow or fall (scapula body fracture) or through direct trauma to
the point of the shoulder (acromion, coracoid fracture). -
Shoulder dislocation may cause a glenoid fracture.
-
Muscles or ligaments may cause an avulsion fracture.
ASSOCIATED INJURIES
-
The presence of a scapula fracture should
raise suspicion of associated injuries, because 35% to 98% of scapula
fractures occur in the presence of comorbid injuries including:-
Ipsilateral upper torso injuries: fractured ribs, clavicle, sternum, shoulder trauma.
-
Pneumothorax: seen in 11% to 55% of scapula fractures.
-
Pulmonary contusion: present in 11% to 54% of scapula fractures.
-
Injuries to neurovascular structures: brachial plexus injuries, vascular avulsions.
-
Spine injuries: 20% lower cervical spine, 76% thoracic spine, 4% lumbar spine.
-
Others: concomitant skull fracture, blunt
abdominal trauma, pelvic fracture, and lower extremity injuries. These
are all seen with higher incidences in the presence of a scapula
fracture.
-
CLINICAL EVALUATION
-
A full trauma evaluation is indicated, with attention to airway, breathing, circulation, disability, and exposure.
-
A careful examination for associated injures should be performed, with a thorough neurovascular assessment.
-
Compartment syndrome overlying the
scapula is uncommon, but it must be ruled out in the presence of pain
out of proportion to the apparent injury. Comolli sign
is triangular swelling of the posterior thorax overlying the scapula
and is suggestive of hematoma resulting in increased compartment
pressures.
RADIOGRAPHIC EVALUATION
-
Initial radiographs should include a
trauma series of the shoulder, consisting of a true anteroposterior
view, an axillary view, and a scapular-Y view (true scapular lateral);
these generally are able to demonstrate most glenoid, scapular neck,
body, and acromion fractures.-
The axillary view may be used to delineate acromial and glenoid rim fractures further.
-
An acromial fracture should not be confused with an os acromiale,
which is a rounded, unfused apophysis and is present in approximately
3% of the population. When present, it is bilateral in 60% of cases. -
Glenoid hypoplasia, or scapular neck dysplasia,
is an unusual abnormality that may resemble glenoid impaction and may
be associated with humeral head or acromial abnormalities. It has a
benign course and is usually noted incidentally.
-
-
A 45-degree cephalic tilt (Stryker notch) radiograph is helpful to identify coracoid fractures.
-
Computed tomography may be useful for further characterizing intraarticular glenoid fractures.
-
Because of the high incidence of
associated injuries, especially to thoracic structures, a chest
radiograph is an essential part of the evaluation.
CLASSIFICATION
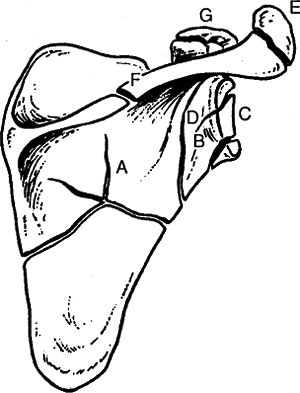
Anatomic Classification (Zdravkovic and Damholt) (Fig. 13.1)
 |
|
Figure 13.1. Anatomic classification. (A) scapula body; (B,C) glenoid; (D) scapula neck; (E) acromion; (F) scapula spine; (G) coracoid.
|
| Type I: | Scapula body |
| Type II: | Apophyseal fractures, including the acromion and coracoid |
| Type III: | Fractures of the superolateral angle, including the scapular neck and glenoid |
P.140
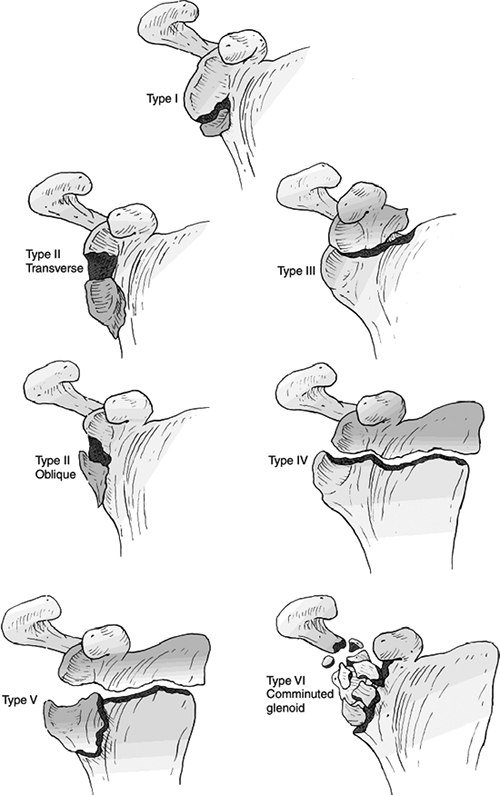
Ideberg Classification of Intraarticular Glenoid Fractures (Fig. 13.2)
| Type I: | Avulsion fracture of the anterior margin |
| Type IIA: | Transverse fracture through the glenoid fossa exiting inferiorly |
| Type IIB: | Oblique fracture through the glenoid fossa exiting inferiorly |
| Type III: | Oblique fracture through the glenoid exiting superiorly and often associated with an acromioclavicular joint injury |
| Type IV: | Transverse fracture exiting through the medial border of the scapula |
| Type V: | Combination of a type II and type IV pattern |
| Type VI: | Comminuted glenoid fracture |
Classification of Acromial Fractures (Kuhn et al.) (Fig. 13.3)
| Type I: | Minimally displaced |
| Type II: | Displaced but does not reduce the subacromial space |
| Type III: | Displaced with narrowing of the subacromial space |
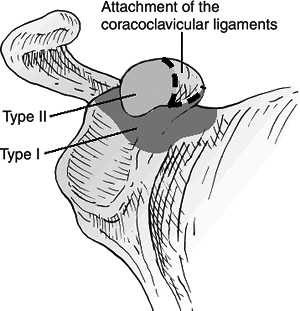
Classification of Coracoid Fractures (Ogawa et al.) (Fig. 13.4)
| Type I: | Proximal to the coracoclavicular ligament. |
| Type II: | Distal to the coracoclavicular ligament |
OTA Classification of Scapula Fractures
-
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT
Nonoperative
Most scapula fractures are amenable to nonoperative treatment, consisting of sling use and early range of shoulder motion.
Operative
-
Surgical indications are controversial, but include:
-
Displaced intraarticular glenoid fractures involving greater than 25% of the articular surface.
-
Scapular neck fractures with greater than 40-degree angulation or 1-cm medial translation.
-
Scapular neck fractures with an associated displaced clavicle fracture.
-
Fractures of the acromion that impinge on the subacromial space.
-
Fractures of the coracoid process that result in a functional acromioclavicular separation.
-
Comminuted fractures of the scapular spine.
![]() Figure
Figure
13.2. Ideberg classification of glenoid fractures into five types, with
the comminuted Type VI of Goss added. The classification is historical,
because decision making is based on displacement of the articular
component.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)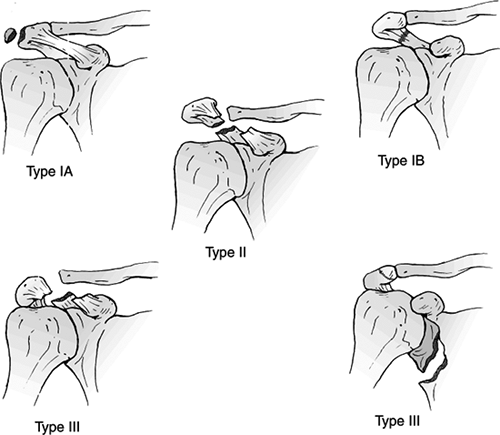 Figure
Figure
13.3. Type I acromion fractures are nondisplaced and include Type IA
(avulsion) and Type IB (complete fracture). Type II fractures are
displaced, but they do not reduce the subacromial space. Type III
fractures cause a reduction in subacromial space.(Modified from Kuhn JE, Blasier RB, Carpenter JE. Fractures of the acromion process: a proposed classification system. J Orthop Trauma 1994;8:6–13.)![]() Figure
Figure
13.4. Classification of coracoid fractures: Type I is proximal to the
coracoclavicular ligament attachment and Type II is distal.(Modified from Ogawa K, Yoshida A, Takahashi M, Ui M. Fractures of the coracoid process. J Bone Joint Surg Br 1979;79:17–19.)
-
-
Specific treatment options include:
-
Glenoid fractures (Ideberg classification):
Type I: Fractures involving greater
than one fourth of the glenoid fossa that result in instability may be
amenable to open reduction and internal fixation with screw fixation
using an anterior or posterior approach.Type II: Inferior subluxation of the
humeral head may result, necessitating open reduction, especially when
associated with a greater than 5-mm articular step-off. An anterior
approach typically provides adequate exposure.Type III: Reduction is often difficult
and may require superior exposure for superior to inferior screw
placement, partial-thickness clavicle removal, or distal clavicle
resection in addition to anterior exposure for reduction. Additional
stabilization of the superior suspensory shoulder complex (SSSC) may be
necessary.Type IV: Open reduction should be
considered for displaced fractures, especially those in which the
superior fragment of the glenoid displaces laterally.Type V: Operative management does not
necessarily result in improved functional results as compared with
nonoperative treatment with early motion, but it should be considered
for articular step-off greater than 5 mm.-
Scapular body fractures:
Operative fixation is rarely indicated, with nonoperative measures
generally effective. Open reduction may be considered when
neurovascular compromise is present and exploration is required. -
Glenoid neck fractures:
These generally may be treated symptomatically, with early
range-of-motion exercises. If the injury is accompanied by a displaced
clavicle fracture, an unstable segment may exist, including the
glenoid, acromion, and lateral clavicle. Internal fixation of the
clavicular fracture generally results in adequate stabilization for
healing of the glenoid fracture. -
Acromion fractures:
Os acromiale must first be ruled out, as well as concomitant rotator
cuff injuries. Displaced acromion fractures may be stabilized by dorsal
tension banding, if displacement causes subacromial impingement. -
Coracoid fractures:
Complete third-degree acromioclavicular separation accompanied by a
significantly displaced coracoid fracture is an indication for open
reduction and internal fixation of both injuries. -
Floating shoulder: This consists of double disruptions of the superior shoulder suspensory complex (SSSC).
-
-
The SSSC is a bone-soft tissue ring that
includes the glenoid process, coracoid process, coracoclavicular
ligaments, distal clavicle, acromioclavicular joint, and acromial
process (Fig. 13.5). -
The superior strut is the middle third clavicle.
-
The inferior strut is the lateral scapular body and spine.
-
Traumatic disruption of two or more
components of the SSSC usually secondary to high-energy injury is
frequently described as a floating shoulder.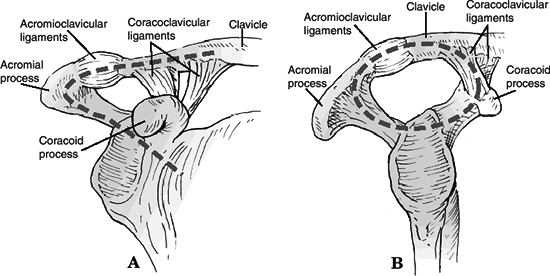 Figure 13.5. Superior shoulder suspensory complex anatomy. (A) Anteroposterior view. (B) True lateral view.(Modified from Goss TP. Double disruption of the superior shoulder suspensory complex. J Orthop Trauma 1993;7:99–106.)
Figure 13.5. Superior shoulder suspensory complex anatomy. (A) Anteroposterior view. (B) True lateral view.(Modified from Goss TP. Double disruption of the superior shoulder suspensory complex. J Orthop Trauma 1993;7:99–106.) -
Historically, operative management has been recommended because of potential instability and displacement of the glenoid.
-
Recent series of nonoperative treatment of floating shoulders reported good results.
P.144 -
P.141
P.142
P.143
COMPLICATIONS
-
Associated injuries: These account for
most serious complications, because of the high-energy nature of these
injuries. Increased mortality is associated with concomitant first rib
fracture. -
Malunion: Fractures of the scapula body
generally unite with nonoperative treatment; when malunion occurs, it
is generally well tolerated but may result in painful scapulothoracic
crepitus. -
Nonunion: This is extremely rare, but when present and symptomatic it may require open reduction and internal fixation.
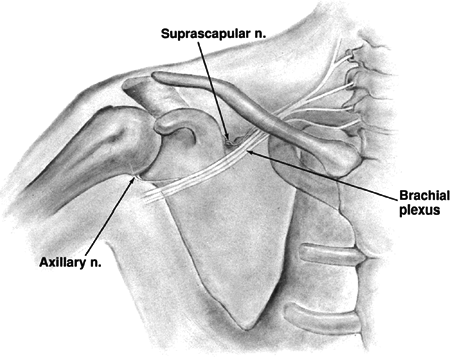
-
Suprascapular nerve injury: This may
occur in association with scapula body, neck, or coracoid fractures
that involve the suprascapular notch (Fig. 13.6).
Scapulothoracic Dissociation
-
This injury is a traumatic disruption of the scapula from the posterior chest wall.
-
This rare, life-threatening injury, is essentially a subcutaneous forequarter amputation.
-
The mechanism is a violent traction and rotation force, usually as a result of a motor vehicle or motorcycle accident.
-
Neurovascular injury is common:
-
Complete brachial plexopathy: 80%
-
Partial plexopathy: 15%
-
Subclavian or axillary artery: 88%
-
-
It can be associated with fracture or dislocation about the shoulder or without obvious bone injury.
![]() Figure 13.6. Schematic diagram showing the positions of the brachial plexus relative to the scapula.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 13.6. Schematic diagram showing the positions of the brachial plexus relative to the scapula.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Diagnosis includes:
-
Massive swelling of shoulder region.
-
A pulseless arm.
-
A complete or partial neurologic deficit.
-
Lateral displacement of the scapula on a nonrotated chest radiograph, which is diagnostic (Fig. 13.7).
-
-
Classification
Type I: Musculoskeletal injury alone Type IIA: Musculoskeletal injury with vascular disruption Type IIB: Musculoskeletal injury with neurologic impairment Type III: Musculoskeletal injury with both neurologic and vascular injury -
Initial treatment
-
Patients are often polytraumatized.
-
Advanced trauma life support protocols should be followed.
-
Angiography of the limb with vascular repair and exploration of brachial plexus are performed as indicated.
-
Stabilization of associated bone or joint injuries is indicated.
-
-
Later treatment
-
Neurologic
-
At 3 weeks, electromyography is indicated.
-
At 6 weeks, cervical myelography or magnetic resonance imaging is performed.
-
Shoulder arthrodesis and/or above elbow amputation may be necessary if the limb is flail.
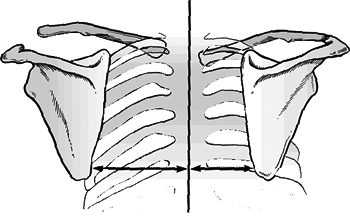 Figure 13.7. Diagram of scapulothoracic dissociation, demonstrating lateral displacement of the scapula on the injured side (left) compared with the normal side (right) on a nonrotated chest radiograph.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 13.7. Diagram of scapulothoracic dissociation, demonstrating lateral displacement of the scapula on the injured side (left) compared with the normal side (right) on a nonrotated chest radiograph.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Nerve root avulsions and complete deficits have a poor prognosis.
-
Partial plexus injuries have good prognosis, and functional use of the extremity is often regained.
P.146 -
-
Osseous
-
If initial exploration of the brachial plexus reveals a severe injury, primary above elbow amputation should be considered.
-
If cervical myelography reveals three or more pseudomeningoceles, the prognosis is similarly poor.
-
-
-
This injury is associated with a poor outcome including flail extremity in 52%, early amputation in 21%, and death in 10%.
P.145
Intrathoracic Dislocation of the Scapula
-
This is extremely rare.
-
The inferior angle of the scapula is locked in the intercostal space.
-
Chest computed tomography may be needed to confirm the diagnosis.
-
Treatment consists of closed reduction
and immobilization with a sling and swathe for 2 weeks, followed by
progressive functional use of the shoulder and arm.