Glenohumeral Dislocation
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > III – Upper Extremity Fractures and Dislocations > 14 – Glenohumeral Dislocation
14
Glenohumeral Dislocation
EPIDEMIOLOGY
-
The shoulder is the most commonly dislocated major joint of the body, accounting for up to 45% of dislocations.
-
Most shoulder dislocations are anterior;
this occurs between eight and nine times more frequently than posterior
dislocation, the second most common direction of dislocation. -
Inferior and superior shoulder dislocations are rare.
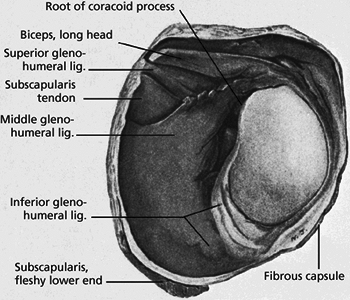
ANATOMY (FIG. 14.1)
-
Glenohumeral stability depends on various passive and active mechanisms, including:
-
Passive:
-
Joint conformity.
-
Vacuum effect of limited joint volume.
-
Adhesion and cohesion owing to the presence of synovial fluid
-
Scapular inclination: for >90% of
shoulders, the critical angle of scapular inclination is between 0 and
30 degrees, below which the glenohumeral joint is considered unstable
and prone to inferior dislocation. -
Ligamentous and capsular restraints (Fig. 14.2).
-
Joint capsule: Redundancy prevents
significant restraint, except at terminal ranges of motion. The
anteroinferior capsule limits anterior subluxation of the abducted
shoulder. The posterior capsule and teres minor limit internal
rotation. The anterior capsule and lower subscapularis restrain
abduction and external rotation. -
Superior glenohumeral ligament: This is the primary restraint to inferior translation of the adducted shoulder.
-
Middle glenohumeral ligament: This is
variable, poorly defined, or absent in 30%. It limits external rotation
at 45 degrees of abduction. -
Inferior glenohumeral ligament: This
consists of three bands, the superior of which is of primary importance
to prevent anterior dislocation of the shoulder. It limits external
rotation at 45 to -90 degrees of abduction.
-
-
Glenoid labrum.
-
Bony restraints: acromion, coracoid, glenoid fossa.
-
-
Active:
-
Biceps, long-head.
-
Rotator cuff.
-
-
-
Coordinated shoulder motion involves:
-
Glenohumeral motion.
-
Scapulothoracic motion.
-
Clavicular and sternoclavicular motion.
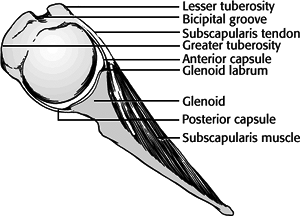 Figure 14.1. Views of the shoulder bony anatomy.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 14.1. Views of the shoulder bony anatomy.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Acromioclavicular motion.
P.148 -
-
Pathoanatomy of shoulder dislocations:
-
Stretching or tearing of the capsule.
-
Usually off the glenoid, but occasionally off the humeral avulsion of the glenohumeral ligaments (HAGL lesion).
-
-
Labral damage.
![]() Figure
Figure
14.2. Anterior glenohumeral ligaments. This drawing shows the
anterosuperior, anteromedial, and anteroinferior glenohumeral
ligaments. The anteromedial and anteroinferior glenohumeral ligaments
are often avulsed from the glenoid or glenoid labrum in traumatic
anterior instability.(From Grant’s Atlas of Anatomy, 4th ed. Baltimore: Williams & Wilkins, 1956.)P.149-
A “Bankart” lesion refers to avulsion of
anteroinferior labrum off the glenoid rim. It may be associated with a
glenoid rim fracture (“bony Bankart”).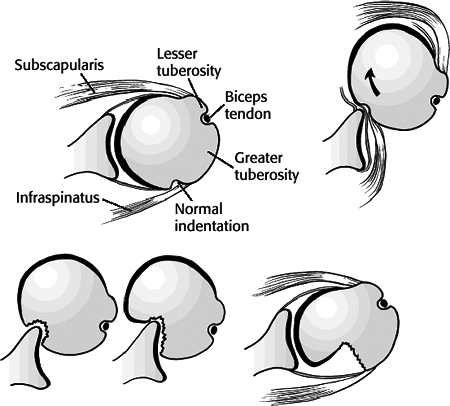 Figure
Figure
14.3. Hill-Sachs lesion associated with anterior shoulder dislocation.
On dislocation, the posterior aspect of the humeral head engages the
anterior glenoid rim. The glenoid rim then initiates an impression
fracture that can enlarge.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
-
-
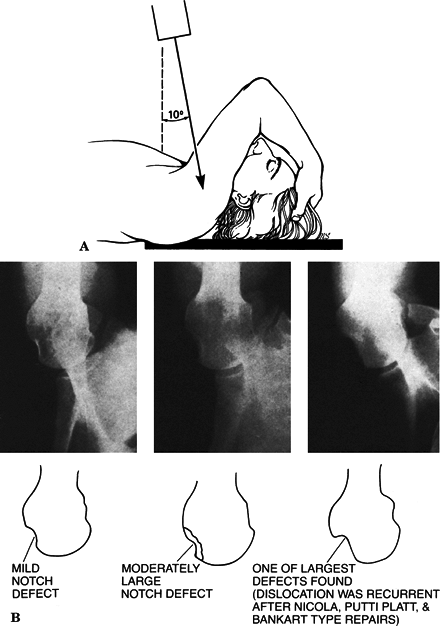
Hill-Sachs lesion: A posterolateral head
defect is caused by an impression fracture on the glenoid rim; this is
seen in 27% of acute anterior dislocations and 74% of recurrent
anterior dislocations (Fig. 14.3). -
Shoulder dislocation with associated rotator cuff tear.
-
This is common in older patients.
-
>40 years of age: 35% to 40%
-
>60 years of age: may be as high as 80%
-
-
Beware of inability to lift the arm in an older patient following a dislocation.
-
ANTERIOR GLENOHUMERAL DISLOCATION
Incidence
-
Anterior dislocations represent 90% of shoulder dislocations.
Mechanism of Injury
Anterior glenohumeral dislocation may occur as a result of trauma, secondary to either direct or indirect forces.
-
Indirect trauma to the upper extremity
with the shoulder in abduction, extension, and external rotation is the
most common mechanism. -
Direct, anteriorly directed impact to the posterior shoulder may produce an anterior dislocation.
-
Convulsive mechanisms and electrical
shock typically produce posterior shoulder dislocations, but they may
also result in an anterior dislocation. -
Recurrent instability related to
congenital or acquired laxity or volitional mechanisms may result in
anterior dislocation with minimal trauma.
P.150
Clinical Evaluation
-
It is helpful to determine the nature of
the trauma, the chronicity of the dislocation, pattern of recurrence
with inciting events, and the presence of laxity or a history of
instability in the contralateral shoulder. -
The patient typically presents with the
injured shoulder held in slight abduction and external rotation. The
acutely dislocated shoulder is painful, with muscular spasm. -
Examination typically reveals squaring of
the shoulder owing to a relative prominence of the acromion, a relative
hollow beneath the acromion posteriorly, and a palpable mass anteriorly. -
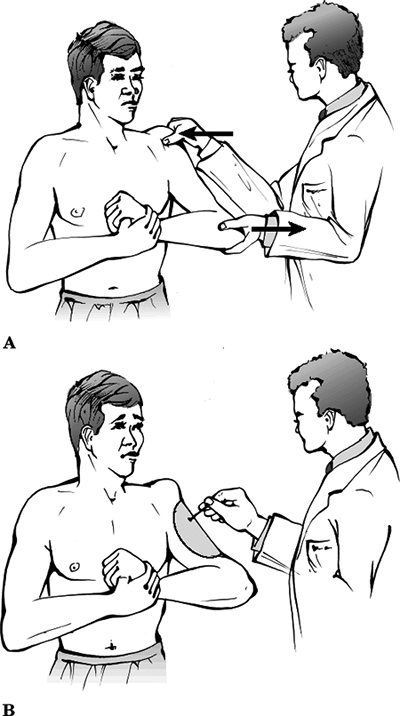
A careful neurovascular examination is
important, with attention to axillary nerve integrity. Deltoid muscle
testing is usually not possible, but sensation over the deltoid may be
assessed. Deltoid atony may be present and should not be confused with
axillary nerve injury. Musculocutaneous nerve integrity can be assessed
by the presence of sensation on the anterolateral forearm (Fig. 14.4). -
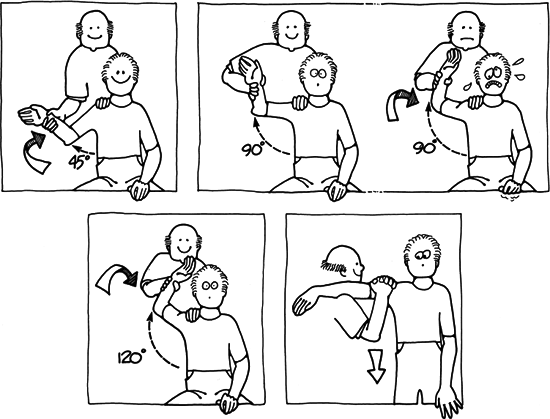
Patients may present after spontaneous
reduction or reduction in the field. If the patient is not in acute
pain, examination may reveal a positive apprehension test,
in which passive placement of the shoulder in the provocative position
(abduction, extension, and external rotation) reproduces the patient’s
sense of instability and pain (Fig. 14.5).
Radiographic Evaluation
-
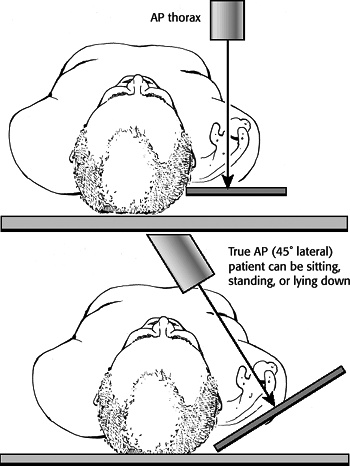
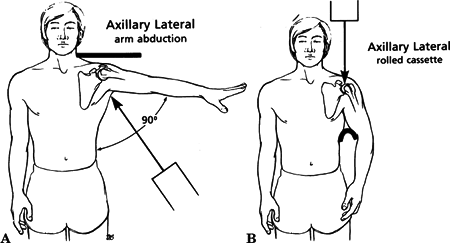
Trauma series of the affected shoulder: Anteroposterior (AP), scapular-Y, and axillary views taken in the plane of the scapula (Figs. 14.6 and 14.7).
-
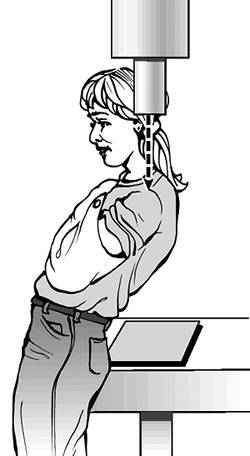
Velpeau axillary: If a standard axillary
cannot be obtained because of pain, the patient may be left in a sling
and leaned obliquely backward 45 degrees over the cassette. The beam is
directed caudally, orthogonal to the cassette, resulting in an axillary
view with magnification (Fig. 14.8). -
Special views:
-
West Point axillary: This is taken with
patient prone with the beam directed cephalad to the axilla 25 degrees
from the horizontal and 25 degrees medial. It provides a tangential
view of the anteroinferior glenoid rim (Fig. 14.9). -
Hill-Sachs view: This AP radiograph is
taken with the shoulder in maximal internal rotation to visualize a
posterolateral defect. -
Stryker notch view: The patient is supine
with the ipsilateral palm on the crown of the head and the elbow
pointing straight upward. The x-ray beam is directed 10 degrees
cephalad, aimed at the coracoid. This view can visualize 90% of
posterolateral humeral head defects (Fig. 14.10). -
Computed tomography may be useful in
defining humeral head or glenoid impression fractures, loose bodies,
and anterior labral bony injuries (bony Bankart lesion).![]() Figure
Figure
14.4. Technique for testing axillary nerve function. With the arm
adducted and stabilized by the examiner, the patient is asked to abduct
the arm. The motor component (A) of the axillary nerve is documented by
observing or palpating deltoid muscle contraction. The sensory
component (B) of the axillary nerve is documented by testing the
sensation to the lateral aspect of the upper arm.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
P.151 -
-
Single- or double-contrast arthrography may be utilized to evaluate rotator cuff pathologic processes.
-
Magnetic resonance imaging may be used to
identify rotator cuff, capsular, and glenoid labral (Bankart lesion)
pathologic processes.
P.152
Classification
 |
|
Figure
14.5. Evaluation of the injured shoulder in varying degrees of abduction. Top left: External rotation force is applied to the arm in 45 degrees of abduction. Top right: The shoulder is abducted 90 degrees. Next, the external rotation force with some extension is applied, which produces pain, usually posteriorly, and marked apprehension in the patient. This position most commonly produces pain and severe apprehension. Bottom left: The external rotation and extension force is applied to the arm in 120 degrees of abduction. This causes apprehension in some patients but not as marked with the arm in 90 degrees of abduction. Bottom right: The Feagin test. With the patient’s elbow resting on the top of the physician’s shoulder, a downward force on the proximal humerus in some instances produces apprehension. (From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2001.)
|
| Degree of Stability: | Dislocation versus Subluxation |
| Chronology: | Congenital Acute versus chronic Locked (fixed) Recurrent Acquired: generally from repeated minor injuries (swimming, gymnastics, weights); labrum often intact but with capsular laxity; increased glenohumeral joint volume; subluxation common |
| Force: | Atraumatic: usually owing to congenital laxity; noinjury; often asymptomatic; self-reducing Traumatic: usually caused by one major injury; anterior or inferior labrum may be detached (Bankart lesion); unidirectional; generally requires assistance for reduction |
| Patient contribution: | Voluntary versus involuntary |
| Direction: | Subcoracoid Subglenoid Intrathoracic |
P.153
Treatment
 |
|
Figure
14.6. Technique for obtaining anteroposterior (AP) (upper panel) and true AP (lower panel) x-rays of the shoulder. In an AP view, the x-ray actually represents an oblique view of the shoulder joint. In a true AP view, the x-ray beam is parallel to the joint so overlap between the humeral head and the glenoid surface is minimal. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
Nonoperative
-
Closed reduction should be performed
after adequate clinical evaluation and administration of analgesics
and/or sedation. Described techniques include:-
Traction-countertraction (Fig. 14.11)
 Figure
Figure
14.7. (A) The axillary lateral x-ray view. Ideally, the arm is abducted
70 to 90 degrees and the beam is directed superiorly up to the x-ray
cassette. (B) When the patient cannot fully abduct the arm, a curved
cassette can be placed in the axilla and the beam can be directed
inferiorly through the glenohumeral joint onto the cassette.(From Rockwood CA, Szalay EA, Curtis RJ, et al. X-ray evaluation of shoulder problems. In: Rockwood CA, Matsen FA III, eds. The Shoulder. Philadelphia: WB Saunders, 1990:119–225.)![]() Figure 14.8. Positioning of the patient for the Velpeau axillary lateral view x-ray.(Modified from Bloom
Figure 14.8. Positioning of the patient for the Velpeau axillary lateral view x-ray.(Modified from Bloom
MH, Obata WG. Diagnosis of posterior dislocation of the shoulder with
use of Velpeau axillary and angle-up roentgenographic views. J Bone Joint Surg Am 1967;49: 943–949.) -
Hippocratic technique:
This is effective with only one person performing reduction, with one
foot placed across the axillary folds and onto the chest wall, with
gentle internal and external rotation with axial traction on the
affected upper extremity.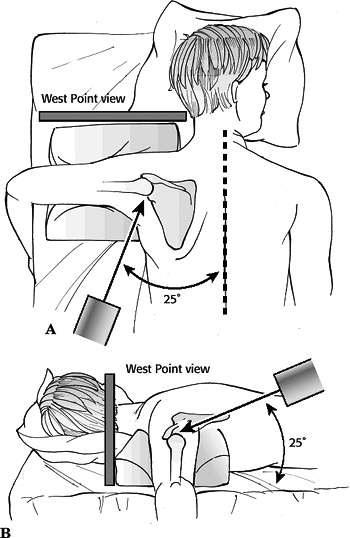 Figure
Figure
14.9. West Point view for the identification of a glenoid rim lesion.
This x-ray is taken with the patient in the prone position. The beam is
angled approximately 25 degrees (A) to provide a tangential view of the
glenoid. In addition, the beam is angled 25 degrees downward (B) to
highlight the anterior and posterior aspects of the glenoid. In this
fashion, the entire glenoid rim can be clearly visualized.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
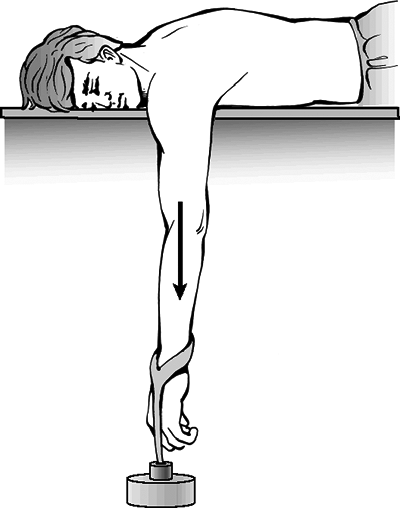
Stimson technique:
After administration of analgesics and/or sedatives, the patient is
placed prone on the stretcher with the affected upper extremity hanging
free. Gentle, manual traction or 5 lb of weight is applied to the
wrist, with reduction effected over 15 to 20 minutes (Fig. 14.12). -
Milch technique:
With the patient supine and the upper extremity abducted and externally
rotated, thumb pressure is applied by the physician to push the humeral
head into place.![]() Figure
Figure
14.10. (A) The position of the patient for the Stryker notch view. The
patient is supine with the cassette posterior to the shoulder. The
humerus is flexed approximately 120 degrees so the hand can be placed
on top of the patient’s head. Note that the angle of the x-ray tube is
10 degrees superior. (B) Defects in the posterolateral aspect of the
humeral head are seen in three different patients with recurring
anterior dislocations of the shoulder.(Modified from Hall RH, Isaac F, Booth CR. Dislocation of the shoulder with special reference to accompanying small fractures. J Bone Joint Surg 1959;41:489–494.) -
Kocher maneuver:
The humeral head levered on the anterior glenoid to effect reduction;
this is not recommended because of increased risk of fracture. Figure 14.11. Closed reduction of the left shoulder with traction against countertraction.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 14.11. Closed reduction of the left shoulder with traction against countertraction.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
P.154P.155P.156P.157 -
-
Postreduction care includes
immobilization for 2 to 5 weeks. A shorter period of immobilization may
be used for patients older than 40 years of age because stiffness of
the ipsilateral hand, wrist, elbow, and shoulder tends to complicate
treatment. Younger patients with a history of recurrent dislocation may
require longer periods of immobilization. -
In comparison to a simple sling,
immobilization in a Velpeau dressing does not appear to alter the
subsequent development of recurrent instability. -
Aggressive occupational therapy should be
instituted following immobilization, including increasing degrees of
shoulder external rotation, flexion, and abduction as time progresses,
accompanied by full, active range of motion to the hand, wrist, and
elbow. -
Irreducible acute anterior dislocation (rare) is usually the result of interposed soft tissue and requires open reduction.
Operative
-
Indications for surgery include:
-
Soft tissue interposition.
-
Displaced greater tuberosity fracture.
-
Glenoid rim fracture >5 mm in size.
-
Selective repair in the acute period (e.g., in young athletes).
-
-
Surgical options for stabilization
include repair of the anterior labrum, capsular shift, capsulorrhaphy,
muscle or tendon transfers, and bony transfers. Recent developments
include the use of arthroscopy for diagnostic and therapeutic purposes
(e.g.,
P.158
arthroscopic anterior labral repair), as well as thermal capsulorrhaphy.![]() Figure
Figure
14.12. The Stimson technique for closed shoulder reduction. With the
patient in prone position, a weight is hung from the wrist to distract
the shoulder joint. Eventually, with sufficient fatigue in the shoulder
musculature, the joint can be easily reduced.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Postoperative management typically
includes the use of a shoulder immobilizer for 3 weeks in patients
<30 years, 2 weeks for patients 30 to 40 years, and 1 to 2 weeks for
patients >50 years of age, depending on the type of surgical
stabilization. Patients are allowed to remove the immobilizer two to
four times per day for shoulder, wrist, and hand range-of-motion
exercises. Occupational therapy is aimed at active and passive range of
motion and regaining upper extremity strength.
Complications
-
Recurrent anterior dislocation: related to ligament and capsular changes.
-
The most common complication after dislocation is recurrent dislocation
-
Incidence:
-
Age 20 years: 80% to 92% (lower in non-athletes)
-
Age 30 years: 60%
-
Age 40 years: 10% to 15%
-
-
Most recurrences occur within the first 2 years and tend to occur in men.
-
Prognosis is most affected by age at the time of initial dislocation.
-
Incidence is unrelated to the type or length of immobilization.
-
Patient activity has been identified as an independent factor for developing recurrent instability.
P.159 -
-
Osseous lesions:
-
Hill-Sachs lesion
-
Glenoid lip fracture (“bony Bankart lesion”)
-
Greater tuberosity fracture
-
Fracture of acromion or coracoid
-
Posttraumatic degenerative changes
-
-
Soft tissue injuries:
-
Rotator cuff tear (older patients)
-
Capsular or subscapularis tendon tears
-
-
Vascular injuries: These typically occur
in elderly patients with atherosclerosis and usually involve the
axillary artery. They may occur at the time of open or closed reduction. -
Nerve injuries: These involve
particularly the musculocutaneous and axillary nerves, usually in
elderly individuals; neurapraxia almost always recovers, but if it
persists beyond 3 months it requires further evaluation with possible
exploration.
POSTERIOR GLENOHUMERAL DISLOCATION
Incidence
-
These injuries represent 10% of shoulder dislocations and 2% of shoulder injuries.
-
They are often unrecognized by primary care and emergency physicians, with 60% to 80% missed on initial examination.
Mechanism of Injury
-
Indirect trauma: This is the most common mechanism.
-
The shoulder typically is in the position of adduction, flexion, and internal rotation.
-
Electric shock or convulsive mechanisms
may produce posterior dislocations owing to the greater muscular force
of the internal rotators (latissimus dorsi, pectoralis major, and
subscapularis muscles) compared with the external rotators of the
shoulder (infraspinatus and teres minor muscles).
-
-
Direct trauma: This results from force
application to the anterior shoulder, resulting in posterior
translation of the humeral head.
Clinical Evaluation
-
Clinically, a posterior glenohumeral
dislocation does not present with striking deformity; the injured upper
extremity is typically held in the traditional sling position of
shoulder internal rotation and adduction. -
A careful neurovascular examination is
important to rule out axillary nerve injury, although it is much less
common than with anterior glenohumeral dislocation. -
On examination, limited external rotation
(often <0 degrees) and limited anterior forward elevation (often
<90 degrees) may be appreciated. -
A palpable mass posterior to the shoulder, flattening of the anterior shoulder, and coracoid prominence may be observed.
P.160
Radiographic Evaluation
-
Trauma series of the affected shoulder:
AP, scapular-Y, and axillary views. A Velpeau axillary view (see
earlier) may be obtained if the patient is unable to position the
shoulder for a standard axillary view. -
On a standard AP view of the shoulder, signs suggestive of a posterior glenohumeral dislocation include:
-
Absence of the normal elliptic overlap of the humeral head on the glenoid.
-
Vacant glenoid sign: The glenoid appears partially vacant (space between anterior rim and humeral head >6 mm).
-
Trough sign: impaction fracture of the
anterior humeral head caused by the posterior rim of glenoid (reverse
Hill-Sachs lesion). This is reported to be present in 75% of cases. -
Loss of profile of neck of humerus: The humerus is in full internal rotation.
-
Void in the superior/inferior glenoid fossa, owing to inferosuperior displacement of the dislocated humeral head.
-
-
Glenohumeral dislocations are most
readily recognized on the axillary view; this view may also demonstrate
the reverse Hill-Sachs defect. -
Computed tomography scans are valuable in assessing the percentage of the humeral head involved with an impaction fracture.
Classification
Etiologic Classification
| Traumatic: | Sprain, subluxation, dislocation, recurrent, fixed (unreduced) |
| Atraumatic: | Voluntary, congenital, acquired (due to repeated microtrauma) |
Anatomic Classification
| Subacromial (98%): | Articular surface directed posteriorly with no gross displacement of the humeral head as in anterior dislocation; lesser tuberosity typically occupies glenoid fossa; often associated with an impaction fracture on the anterior humeral head |
| Subglenoid (very rare): | Humeral head posterior and inferior to the glenoid |
| Subspinous (very rare): | Humeral head medial to the acromion and inferior to the spine of the scapula |
P.161
Treatment
Nonoperative
-
Closed reduction requires full muscle relaxation, sedation, and analgesia.
-
The pain from an acute, traumatic
posterior glenohumeral dislocation is usually greater than with an
anterior dislocation and may require general anesthesia for reduction. -
With the patient supine, traction should
be applied to the adducted arm in the line of deformity with gentle
lifting of the humeral head into the glenoid fossa. -
The shoulder should not be forced into
external rotation, because this may result in a humeral head fracture
if an impaction fracture is locked on the posterior glenoid rim. -
If prereduction radiographs demonstrate
an impaction fracture locked on the glenoid rim, axial traction should
be accompanied by lateral traction on the upper arm to unlock the
humeral head.
-
-
Postreduction care should consist of a
sling and swathe if the shoulder is stable. If the shoulder subluxes or
redislocates in the sling and swathe, a shoulder spica should be placed
with amount of external rotation determined by the position of
stability. Immobilization is continued for 3 to 6 weeks, depending on
the age of the patient and stability of the shoulder.-
With a large anteromedial head defect, better stability may be achieved with immobilization in external rotation.
-
External rotation and deltoid isometric exercises may be performed during the period of immobilization.
-
After discontinuation of immobilization, an aggressive internal and external rotator strengthening program is instituted.
-
Operative
-
Indications for surgery include:
-
Major displacement of an associated lesser tuberosity fracture.
-
A large posterior glenoid fragment.
-
Irreducible dislocation or an impaction fracture on the posterior glenoid preventing reduction.
-
Open dislocation.
-
An anteromedial humeral impaction fracture (reverse Hill-Sachs lesion):
-
Twenty to 40% humeral head involvement:
transfer the lesser tuberosity with attached subscapularis into the
defect (modified McLaughlin procedure). -
Greater than 40% humeral head involvement: hemiarthroplasty with neutral version of the prosthesis.
-
-
Surgical options include open reduction,
infraspinatus muscle/tendon plication (reverse Putti-Platt procedure),
long head of the biceps tendon transfer to the posterior glenoid margin
(Boyd-Sisk procedure), humeral and glenoid osteotomies, and
capsulorraphy. -
Voluntary dislocators should be treated nonoperatively, with counseling and strengthening exercises.
P.162
Complications
-
Fractures: These include fractures of the
posterior glenoid rim, humeral shaft, lesser and greater tuberosities,
and humeral head. -
Recurrent dislocation: The incidence is
increased with atraumatic posterior glenohumeral dislocations, large
anteromedial humeral head defects resulting from impaction fractures on
the glenoid rim, and large posterior glenoid rim fractures. They may
require surgical stabilization to prevent recurrence. -
Neurovascular injury: This is much less
common in posterior versus anterior dislocation, but it may include
injury to the axillary nerve as it exits the quadrangular space or to
the nerve to the infraspinatus (branch of the suprascapular nerve) as
it traverses the spinoglenoid notch. -
Anterior subluxation: This may result
from “overtightening” posterior structures, forcing the humeral head
anteriorly. It may cause limited flexion, adduction, and internal
rotation.
INFERIOR GLENOHUMERAL DISLOCATION (LUXATIO ERECTA)
-
This very rare injury is more common in elderly individuals.
Mechanism of Injury (Fig. 14.13)
-
It results from a hyperabduction force
causing impingement of the neck of the humerus on the acromion, which
levers the humeral head out inferiorly.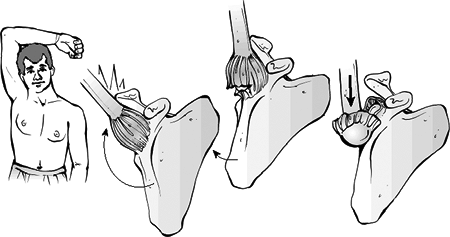 Figure 14.13. Locked inferior dislocation of the glenohumeral joint, also known as luxatio erectae.
Figure 14.13. Locked inferior dislocation of the glenohumeral joint, also known as luxatio erectae.
With hyperabduction of the arm, the lateral acromion acts as a lever
against the proximal humerus to dislocate the shoulder inferiorly.
After dislocation, the humeral head is locked inferior to the glenoid
rim. In these patients, the rotator cuff tendons are typically detached
from the humeral head, and there may also be an associated fracture of
the greater tuberosity.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
The superior aspect of articular surface
is directed inferiorly and is not in contact with the inferior glenoid
rim. The humeral shaft is directed superiorly. -
Rotator cuff avulsion and tear,
pectoralis injury, proximal humeral fracture, and injury to the
axillary artery or brachial plexus are common.
P.163
Clinical Evaluation
-
Patients typically present in a
characteristic “salute” fashion, with the humerus locked in 110 to 160
degrees of abduction and forward elevation. Pain is usually severe. -
The humeral head is typically palpable on the lateral chest wall and axilla.
-
A careful neurovascular examination is essential, because neurovascular compromise almost always complicates these dislocations.
Radiographic Evaluation
-
Trauma series of the affected shoulder: AP, scapular-Y, and axillary views are taken.
-
The AP radiograph is typically
diagnostic, with inferior dislocation of the humeral head and superior
direction of the humeral shaft along the glenoid margin. -
The radiograph must be carefully
scrutinized for associated fractures, which are common and may be
clinically not detected because of a diffusely painful shoulder.
Treatment
Nonoperative
-
Reduction may be accomplished by the use of traction-countertraction maneuvers.
-
Axial traction should be performed in
line with the humeral position (superolaterally), with a gradual
decrease in shoulder abduction. Countertraction should be applied with
a sheet around the patient, in line with, but opposite to the traction
vector. -
The arm should be immobilized in a sling
for 3 to 6 weeks, depending on the age of the patient. Older
individuals may be immobilized for shorter periods to minimize shoulder
stiffness.
Operative
-
Occasionally, the dislocated humeral head
“buttonholes” through the inferior capsule and soft tissue envelope,
preventing closed reduction. Open reduction is then indicated with
enlarging of the capsular defect and repair of the damaged structures.
Complications
-
Neurovascular compromise: This
complicates nearly all cases of inferior glenohumeral dislocation, but
it usually recovers following reduction.
P.164
SUPERIOR GLENOHUMERAL DISLOCATION
-
This very rare injury is less common than inferior glenohumeral dislocation.
Mechanism of Injury
-
Extreme anterior and superior directed
force applied to the adducted upper extremity, such as a fall from a
height onto the upper extremity, forces the humeral head superiorly
from the glenoid fossa. -
It is associated with fractures of the
acromion, clavicle, coracoid, and humeral tuberosities, as well as
injury to the acromioclavicular joint. -
Typically it is accompanied by soft
tissue injury to the rotator cuff, glenohumeral capsule, biceps tendon,
and surrounding musculature.
Clinical Evaluation
-
The patient typically presents with a foreshortened upper extremity held in adduction.
-
Clinical examination typically reveals a palpable humeral head above the level of the acromion.
-
Neurovascular injuries are common and must be ruled out.
Radiographic Evaluation
-
Trauma series of the affected shoulder: AP, scapular-Y, and axillary views are obtained.
-
The AP radiograph is typically diagnostic, with dislocation of the humeral head superior to the acromion process.
-
The radiograph must be carefully
scrutinized for associated fractures, which are common and may be
clinically not detected because of a diffusely painful shoulder.
Treatment
-
Closed reduction should be attempted with the use of analgesics and sedatives.
-
Axial traction with countertraction may
be applied in an inferior direction, with lateral traction applied to
the upper arm to facilitate reduction. -
As with inferior dislocations, soft
tissue injury and associated fractures are common; irreducible
dislocations may require open reduction.
Complications
-
Neurovascular complications are usually present and typically represent traction injuries that resolve with reduction.