Acromioclavicular and Sternoclavicular Joint Injuries
Upper Extremity Fractures and Dislocations > 12 – Acromioclavicular
and Sternoclavicular Joint Injuries
-
Most common in the second decade of life, associated with contact athletic activities
-
More common in males (5 to 10:1)
-
The AC joint is a diarthrodial joint,
with fibrocartilage-covered articular surfaces, located between the
lateral end of the clavicle and the medial acromion. -
Inclination of the plane of the joint may be vertical or inclined medially 50 degrees.
-
The AC ligaments (anterior, posterior,
superior, inferior) strengthen the thin capsule. Fibers of the deltoid
and trapezius muscles blend with the superior AC ligament to strengthen
the joint. -
The AC joint has minimal mobility through
a meniscoid, intraarticular disc that demonstrates an age-dependent
degeneration until it is essentially nonfunctional beyond the fourth
decade. -
The horizontal stability of the AC joint
is conferred by the AC ligaments, whereas the vertical stability is
maintained by the coracoclavicular ligaments. -
The average coracoclavicular distance is 1.1 to 1.3 cm.
-
Direct: This is the most common
mechanism, resulting from a fall onto the shoulder with the arm
adducted, driving the acromion medial and inferior. -
Indirect: This is caused by a fall onto
an outstretched hand with force transmission through the humeral head
and into the AC articulation (Fig. 12.2).
-
Fractures: clavicle, acromion process, and coracoid process
-
Pneumothorax or pulmonary contusion with type VI AC separations
-
The patient should be examined while in
the standing or sitting position with the upper extremity in a
dependent position, thus stressing the AC joint and emphasizing
deformity. -
The characteristic anatomic feature is a downward sag of the shoulder and arm.
-
A standard shoulder examination should be
performed, including assessment of neurovascular status and possible
associated upper extremity injuries. Inspection may reveal an apparent
P.128
step-off
deformity of the injured AC joint, with possible tenting of the skin
overlying the distal clavicle. Range of shoulder motion may be limited
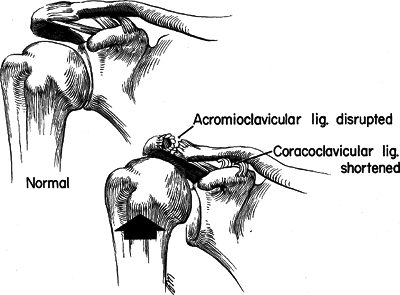
by pain. Tenderness may be elicited over the AC joint.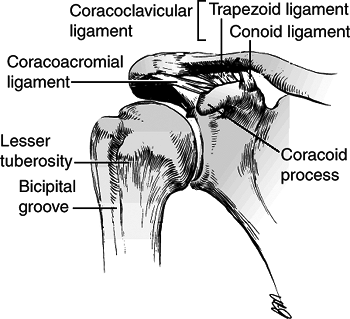 Figure 12.1. Normal anatomy of the acromioclavicular joint.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 12.1. Normal anatomy of the acromioclavicular joint.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
-
A standard trauma series of the shoulder
(anteroposterior [AP], scapular-Y, and axillary views) is usually
sufficient for the recognition of AC injury.![]() Figure
Figure
12.2. An indirect force applied up through the upper extremity (e.g., a
fall on the outstretched hand) may superiorly displace the acromion
from the clavicle, thus producing injury to the acromioclavicular
ligaments. However, stress is not placed on the coracoclavicular
ligaments.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Ligamentous injury to the
coracoclavicular joints may be assessed via stress radiographs, in
which weights (10 to 15 lb) are strapped to the wrists, and an AP
radiograph is taken of both shoulders to compare coracoclavicular
distances. This can differentiate grade III AC separations from partial
grade I to II injuries.
-
This injury is classified depending on the degree and direction of displacement of the distal clavicle (Table 12.1 and Fig. 12.3).Table 12.1. Classification of acromioclavicular (AC) joint injury
Type Anatomy Clinical Examination Radiographic Examination I Sprain of the AC ligament AC joint tenderness, minimal pain with arm motion, no pain in coracoclavicular interspace No abnormality II AC ligament tear with joint disruption, coracoclavicular ligaments sprained Distal clavicle slightly superior to acromion and mobile to palpation; tenderness in the coracoclavicular space Slight elevation of the distal
end of the clavicle; AC joint widening. Stress films show
coracoclavicular space unchanged from normal shoulder.III AC and coracoclavicular
ligaments torn with AC joint dislocation. The deltoid and trapezius
muscles are usually detached from the distal clavicle.The upper extremity and distal
fragment are depressed and the distal end of the proximal fragment may
tent the skin. The AC joint is tender, and coracoclavicular widening is
evident.Radiographs demonstrate the
distal clavicle superior to the medial border of the acromion; stress
views reveal a widened coracoclavicular interspace 25% to 100% greater
than the normal side.IV Distal clavicle displaced
posteriorly into or through the trapezius. The deltoid and trapezius
muscles are detached from the distal clavicle.There is more pain than in type III; the distal clavicle is displaced posteriorly away from the acromion. Axillary radiograph or computed tomography scan demonstrates posterior displacement of the distal clavicle. V Distal clavicle grossly and
severely displaced superiorly (>100%). The deltoid and trapezius
muscles are detached from the distal clavicle.Typically associated with tenting of the skin Radiographs demonstrate the coracoclavicular interspace to be 100% to 300% greater than the normal side. VI The AC joint is dislocated,
with the clavicle displaced inferior to the acromion or the coracoid;
the coracoclavicular interspace is decreased compared with normal. The
deltoid and trapezius muscles are detached from the distal clavicle.The shoulder has a flat
appearance with a prominent acromion; associated clavicle and upper rib
fractures and brachial plexus injuries result from high-energy trauma.One of two types of inferior dislocation: subacromial or subcoracoid
| Type I: | Rest for 7 to 10 days, ice packs, sling. Refrain from full activity until painless, full range of motion (2 weeks). |
| Type II: | Sling for 1 to 2 weeks, gentle range of motion as soon as possible. Refrain from heavy activity for 6 weeks. More than 50% of patients with type I and II injuries remain symptomatic at long-term follow-up. |
| Type III: | For inactive, nonlaboring, or recreational athletic patients, especially for the nondominant arm, nonoperative treatment is indicated: sling, early range of motion, strengthening, and acceptance of deformity. Younger, more active patients with more severe degrees of displacement and laborers who use their upper extremity above the horizontal plane may benefit from operative stabilization. Repair is generally avoided in contact athletes because of the risk of reinjury. |
| Type IV: | Open reduction and surgical repair of the coracoclavicular ligaments are performed for vertical stability. |
| Type V: | Open reduction and surgical repair of the coracoclavicular ligaments are indicated. |
| Type VI: | Open reduction and surgical repair of the coracoclavicular ligaments are indicated. |
-
Coracoclavicular ossification: not associated with increased disability
-
Distal clavicle osteolysis: associated with chronic dull ache and weakness
-
AC arthritis
-
Injuries to the SC joint are rare; Cave
et al. reported that of 1,603 shoulder girdle dislocations, only 3%
were SC, with 85% glenohumeral and 12% AC dislocations.
-
The SC joint is a diarthrodial joint,
representing the only true articulation between the upper extremity and
the axial skeleton. -
The articular surface of the clavicle is much larger than that of the sternum; both are covered with fibrocartilage. Less than
P.130P.131P.132
half of the medial clavicle articulates with the sternum; thus, the SC
joint has the distinction of having the least amount of bony stability
of the major joints of the body.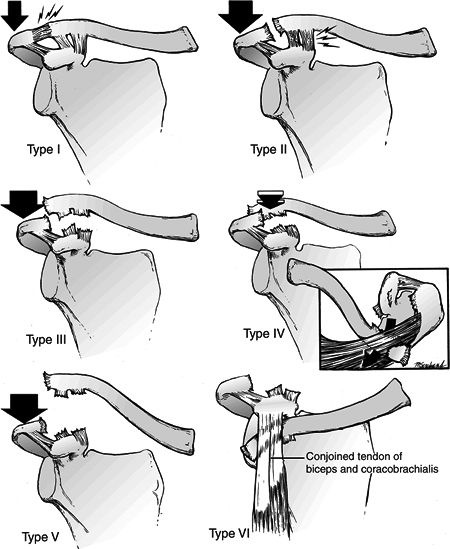 Figure
Figure
12.3. Classification of ligamentous injuries to the acromioclavicular
(AC) joint. Top left: In the Type I injury, a mild force applied to the
point of the shoulder does not disrupt either the AC or the
coracoclavicular ligaments. Top right: A moderate to heavy force
applied to the point of the shoulder will disrupt the AC ligaments, but
the coracoclavicular ligaments remain intact (Type II). Center left:
When a severe force is applied to the point of the shoulder, both the
AC and the coracoclavicular ligaments are disrupted (Type III). Center
right: In a Type IV injury, not only are the ligaments disrupted, but
also the distal end of the clavicle is displaced posteriorly into or
through the trapezius muscle. Bottom left: A violent force applied to
the point of the shoulder not only ruptures the AC and coracoclavicular
ligaments but also disrupts the muscle attachments and creates a major
separation between the clavicle and the acromion (Type V). Bottom
right: This is an inferior dislocation of the distal clavicle in which
the clavicle is inferior to the coracoid process and posterior to the
biceps and coracobrachialis tendons. The AC and coracoclavicular
ligaments are also disrupted (Type VI).(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)![]() Figure
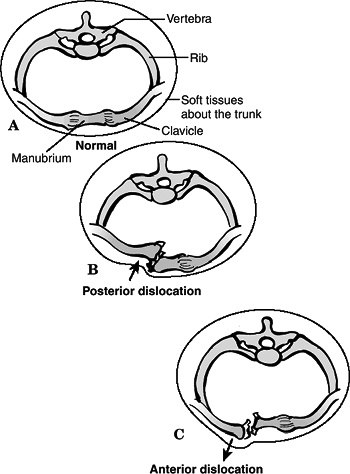
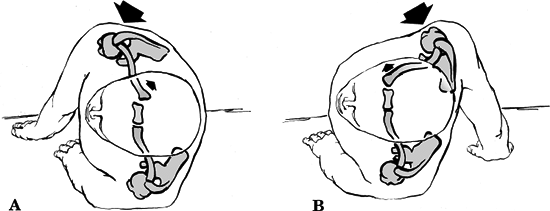
Figure
12.4. Cross sections through the thorax at the level of the
sternoclavicular joint. (A) Normal anatomic relations. (B) Posterior
dislocation of the sternoclavicular joint. (C) Anterior dislocation of
the sternoclavicular joint.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Joint integrity is derived from the
saddle-like configuration of the joint (convex vertically and concave
anteroposteriorly), as well as from surrounding ligaments:-
The intraarticular disc ligament is a checkrein against medial displacement of the clavicle.
-
The extraarticular costoclavicular ligament resists rotation and medial-lateral displacement.
-
The interclavicular ligament helps to maintain shoulder poise.
-
The capsular ligament (anterior, posterior) prevents superior displacement of the medial clavicle.
-
-
Range of motion is 35 degrees of superior
elevation, 35 degrees of combined AP motion, 50 degrees of rotation
around its long axis.
 |
|
Figure
12.5. Mechanisms that produce anterior or posterior dislocations of the sternoclavicular joint. (A) If the patient is lying on the ground and compression force is applied to the posterolateral aspect of the shoulder, the medial end of the clavicle will be displaced posteriorly. (B) When the lateral compression force is directed from the anterior position, the medial end of the clavicle is dislocated anteriorly. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Direct: Force applied to the anteromedial
aspect of the clavicle forces the clavicle posteriorly into the
mediastinum to produce posterior dislocation. This may occur when an
athlete is in the supine position and another athlete falls on him or
her, when an individual is run over by a vehicle, or when an individual
is pinned against a wall by a vehicle. -
Indirect: Force can be applied indirectly
to the SC joint from the anterolateral (producing anterior SC
dislocation) or posterolateral (producing posterior SC dislocation)
aspects of the shoulder. This is most commonly seen in football
“pileups,” in which an athlete is lying obliquely on his shoulder and
force is applied with the individual unable to change position.
-
The patient typically presents supporting
the affected extremity across the trunk with the contralateral,
uninjured arm. The patient’s head may be tilted toward the side of
injury to decrease stress across the joint, and the patient may be
unwilling to place the affected scapula flat on the examination table. -
Swelling, tenderness, and painful range
of shoulder motion are usually present, with a variable change of the
medial clavicular prominence, depending on the degree and direction of
injury. -
Neurovascular status must be assessed,
because the brachial plexus and major vascular structures are in the
immediate vicinity of the medial clavicle.
 |
|
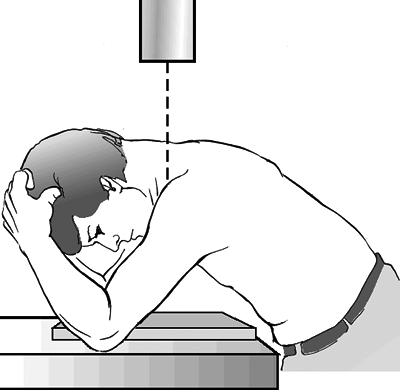
Figure 12.6. Hobbs view: positioning of the patient for x-ray evaluation of the sternoclavicular joint, as recommended by Hobbs.
(Modified from Hobbs DW. Sternoclavicular joint: a new axial radiographic view. Radiology 1968;90:801–802; in Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
AP chest radiographs typically
demonstrate asymmetry of the clavicles that should prompt further
radiographic evaluation. This view should be scrutinized for the
presence of pneumothorax if the patient presents with breathing
complaints. -
Hobbs view: In this 90-degree
cephalocaudal lateral view, the patient leans over the plate, and the
radiographic beam is angled behind the neck (Fig. 12.6). -
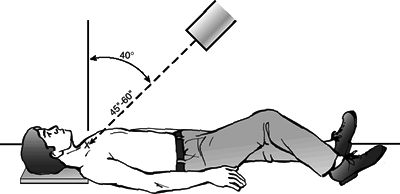
Serendipity view: This 40-degree cephalic
tilt view is aimed at the manubrium. With an anterior dislocation, the
medial clavicle lies above the interclavicular line; with a posterior
dislocation, the medial clavicle lies below this line (Fig. 12.7). -
Computed tomography (CT) scan: This is
the best technique to evaluate injuries to the SC joint. CT is able to
distinguish fractures of the medial clavicle from dislocation as well
as delineate minor subluxations that would otherwise go unrecognized.
-
Anterior dislocation: more common
-
Posterior dislocation
 |
|
Figure
12.7. Serendipity view: positioning of the patient to take the “serendipity” view of the sternoclavicular joints. The x-ray tube is tilted 40 degrees from the vertical position and is aimed directly at the manubrium. The nongrid cassette should be large enough to receive the projected images of the medial halves of both clavicles. In children, the tube distance from the patient should be 45 inches; in thicker-chested adults, the distance should be 60 inches. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Sprain or subluxation
-
Mild: joint stable, ligamentous integrity maintained
-
Moderate: subluxation, with partial ligamentous disruption
-
Severe: unstable joint, with complete ligamentous compromise
-
-
Acute dislocation: complete ligamentous disruption with frank translation of the medial clavicle
-
Recurrent dislocation: rare
-
Unreduced dislocation
-
Atraumatic: may occur with spontaneous
dislocation, developmental (congenital) dislocation, osteoarthritis,
condensing osteitis of the medial clavicle, SC hyperostosis, or
infection
-
Mild sprain: Ice is indicated for the
first 24 hours with sling immobilization for 3 to 4 days and a gradual
return to normal activities as tolerated. -
Moderate sprain or subluxation: Ice is
indicated for the first 24 hours with a clavicle strap, sling and
swathe, or figure-of-eight bandage for 1 week, then sling
immobilization for 4 to 6 weeks. -
Severe sprain or dislocation (Fig. 12.8).
-
Anterior: As for nonoperative treatment,
it is controversial whether one should attempt closed reduction because
it is usually unstable; a sling is used for comfort. Closed reduction
may be accomplished using general anesthesia, or narcotics and muscle
relaxants for the stoic patient. The patient is placed
P.136
supine
with a roll between the scapulae. Direct, posteriorly directed pressure
usually results in reduction. Postreduction care consists of a clavicle
strap, sling and swathe, or figure-of-eight bandage for 4 to 6 weeks.
Some advocate a bulky anterior dressing with elastic tape to maintain
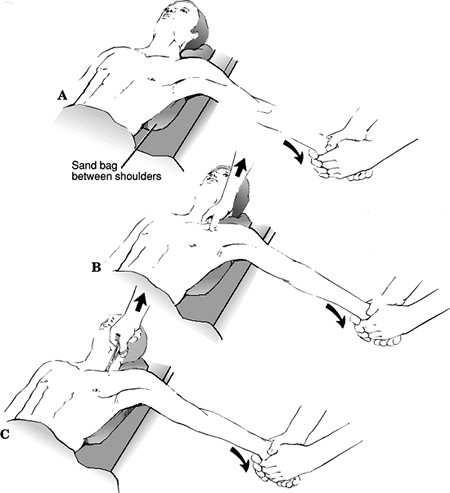
reduction.![]() Figure
Figure
12.8. Technique for closed reduction of the sternoclavicular joint. (A)
The patient is positioned supine with a sandbag placed between the two
shoulders. Traction is then applied to the arm against countertraction
in an abducted and slightly extended position. In anterior
dislocations, direct pressure over the medial end of the clavicle may
reduce the joint. (B) In posterior dislocations, in addition to the
traction it may be necessary to manipulate the medial end of the
clavicle with the fingers to dislodge the clavicle from behind the
manubrium. (C) In stubborn posterior dislocations, it may be necessary
to prepare the medial end of the clavicle in sterile fashion and to use
a towel clip to grasp around the medial clavicle to lift it back into
position.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Posterior: A careful history and physical
examination are necessary to rule out associated pulmonary or
neurovascular problems. Prompt closed or open reduction is indicated,
usually under general anesthesia. Closed reduction is often successful
and remains stable. The patient is placed supine
P.137
with
a roll between the scapulae. Closed reduction may be obtained with
traction with the arm in abduction and extension. Anteriorly directed
traction on the clavicle with a towel clip may be required. A clavicle
strap, sling and swathe, or figure-of-eight bandage is used for
immobilization for 4 to 6 weeks. A general or thoracic surgeon should
be available in the event that the major underlying neurovascular
structures are inadvertently damaged.
-
-
Medial physeal injury: Closed reduction
is usually successful, with postreduction care consisting of a clavicle
strap, sling and swathe, or figure-of-eight bandage immobilization for
4 to 6 weeks. -
Operative management of SC dislocation
may include fixation of the medial clavicle to the sternum using fascia
lata, subclavius tendon, or suture, osteotomy of the medial clavicle,
or resection of the medial clavicle. The use of Kirschner wires or
Steinmann pins is discouraged, because migration of hardware may occur.
-
Poor cosmesis is the most common complication with patients complaining of an enlarged medial prominence.
-
Complications are more common with
posterior dislocations and reflect the proximity of the medial clavicle
to mediastinal and neurovascular structures. The complication rate has
been reported to be as high as 25% with posterior dislocation.
Complications include the following:-
Pneumothorax
-
Laceration of the superior vena cava
-
Venous congestion in the neck
-
Esophageal rupture
-
Subclavian artery compression
-
Carotid artery compression
-
Voice changes
-
Severe thoracic outlet syndrome
-