Scapula Fractures: Open Reduction Internal Fixation
fractures in a comprehensive review of 4,390 broken bones. It is
estimated that scapula fractures account for 3% to 5% of all fractures
about the shoulder girdle. The well-endowed parascapular musculature,
the oblique plane mobility of the scapula on the thorax, and the
surrounding skeletal structures (which usually yield first) explain the
relative rarity of scapula fractures. However, increased recognition of
shoulder morbidity after high-energy trauma as well as improving
familiarity with surgical approaches to the scapula have clarified the
indications for nonoperative versus surgical treatment.
injuries based on the vector and mechanism of force to the shoulder.
Low-energy and sporting accidents often lead to partial articular
fractures that usually involve the anterior glenoid process and are
commonly associated with anterior shoulder dislocations. These
fractures are often referred to as bony Bankart lesions and may be
characterized by anterior shoulder instability. If shoulder instability
is present either clinically or on radiographic examination, then
operative intervention in an appropriate surgical candidate is
recommended. These criteria are usually present with fractures
involving more than 20% of the articular surface.
glenoid neck and body, and they generally occur as a result of
high-energy trauma. These fractures may or may not involve the glenoid
articular surface. Because of the mechanism causing the fracture,
associated injuries occur in many of these patients. In seriously
injured patients, diagnosis and subsequent treatment of a scapula
fracture are often delayed due to treatment of other life-threatening
or limb-threatening conditions. According to a common misconception,
scapulothoracic dissociation frequently occurs in the setting of
scapula fractures; however, scapulothoracic injury results from a
violent traction force to the upper extremity, which is quite the
opposite mechanism of a typical scapula fracture.
glenoid articular surface often require surgical treatment. Articular
fractures should be treated with open reduction and internal
fixation (ORIF) if a step off of 3 to 4 mm is encountered and more than 20% of the joint is involved (Fig. 2.1).
Lesser degrees of articular step off, gap, and percentage of joint
involvement, must be placed into the context of the patient’s
occupation, age, activity level, physiologic status, and hand dominance.
scapular fractures remains controversial. Recent studies support
internal fixation of scapula neck fractures since large displacement or
angulation leads to compromise of shoulder function. Ada and Miller
have recommended ORIF of scapular neck fractures when the glenoid is
medially displaced more than 9 mm or angular displacement exceeds 40
degrees. Their recommendation is based on a review of 16 patients
treated nonoperatively: 50% had pain, 40% had exertional weakness, and
20% had decreased motion at a follow-up of 15 months or later. Eight
patients in this same study were treated operatively, and all achieved
a painless range of motion.
glenoid up to 1 cm has been well tolerated in most patients. Therefore,
ORIF should be considered when medialization of the glenohumeral joint
measures more than 15 mm, angular deformity in the semicoronal plane is
more than 25 degrees, or fracture translation exceeds 100% at the
lateral border of the scapula (Fig. 2.2). The indications for surgery are even stronger when two or more of the noted severity criteria are met.
complex (SSSC), an osseoligamentous ring made up by the acromion,
coracoid, clavicle, and glenoid (Fig. 2.3).
Goss theorized that if two disruptions are found in the ring
structures, including their capsuloligamentous connections, then the
glenohumeral joint would be “floating”, a condition that describes
discontinuity between the axial and appendicular skeleton (Fig. 2.4).
Although this theory has been challenged by some authors, Goss
advocated surgery if two or more components of the SSSC are injured
simultaneously. Further studies have suggested that surgery is
indicated when the SSSC complex structures are displaced and unstable.
Somewhat arbitrarily, if each SSSC injury causes displacement of more
than 1 cm, the floating shoulder condition warrants surgery in an
appropriate candidate. Most commonly, the decision-making process leads
to surgical fixation of both injuries, which facilitates early
rehabilitation.
are less common. Acromion process and spine fractures occur as a result
of direct and concentrated blows to the superior shoulder region,
whereas coracoid process fractures result from traction injuries
through the biceps and coracobrachialis. If either an acromion or
coracoid fracture is displaced more than 10 mm, ORIF may be indicated
in a physiologically young and active patient. If the acromion fracture
is displaced, then a supraspinatus-outlet x-ray should be evaluated for
acromial depression, which may contribute to impingement syndrome, and
therefore warrant operative correction.
scapular fracture is displaced less than 10 mm and angulated less than
25 degrees because the outcomes of nonoperative treatment for even
moderately displaced scapula fractures are uniformly good. Active
mobility of the elbow and wrist are encouraged immediately, but a sling
and rest are indicated for 10 to 14 days. Scapula fractures heal
rapidly due to the rich blood supply in the shoulder girdle. Active
range of motion can be started by 4 weeks and maximized quickly.
Resistive exercises are begun by 8 weeks, and return to full activities
is usually possible by 12 weeks.
scapula fractures. The classification of Ada and Miller, as well as
that of Hardegger et al, are anatomically defined and comprehensive.
The classification scheme developed by Mayo et al is a reorganized
version of the Ideberg classification and is based on a consideration
of the imaging and operative findings of 27 intra-articular glenoid
fractures. The latter classification is helpful in directing surgical
decision making, and it takes into account the associated scapula body
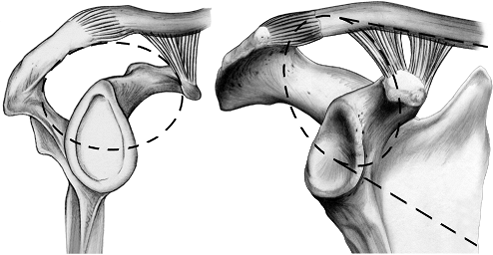
and process fractures (Fig. 2.5). The
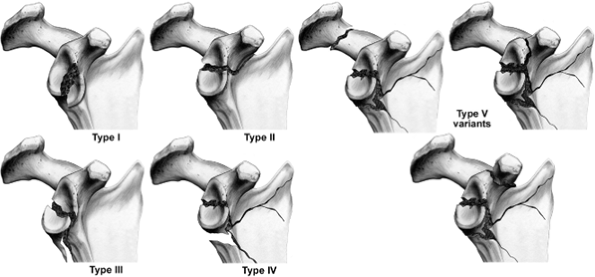
Orthopaedic Trauma Association (OTA) Classification System is an
alphanumeric system in which both intra-articular and extra-articular
variants are classified (Fig. 2.6).
 |
|
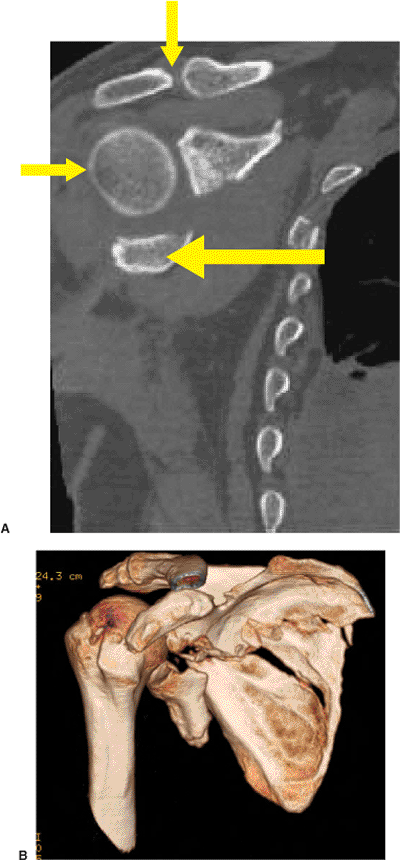
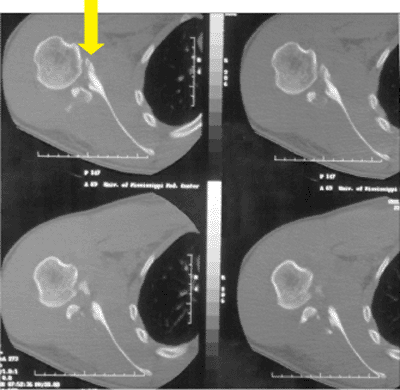
Figure 2.1. A.
A 2D-CT view, reformatted in the semicoronal plane, demonstrating the displacement between superior and inferior glenoid fragments. Most superior is the acromioclavicular joint (downward arrow), beneath which is the humeral head articulating with the superior glenoid fragment (rightward arrow). Below the articulating head is the smaller glenoid fragment (leftward arrow). B. A 3D-CT image for the same patient as shown in (A). It is easier to interpret relationships of key fragments with a 3D-CT; however, the 2D-CT is necessary because volume averaging causes three-dimensional reconstructions to miss minor fracture lines. |
less than distinct. Manual laborers who work with heavy loads and
high-demand athletes may need surgery with relatively few indications.
Also, if the injury occurs in the dominant extremity of an active
individual, or if a patient requires engagement in significant overhead
activity, then ORIF may be an attractive alternative treatment.
However, injuries more than 3 weeks old, in elderly patients, and in
individuals with multiple confounding co-morbidities, nonoperative
treatment is likely the best choice.
 |
|
Figure 2.2. A.
Medialization: a 3D-CT AP image of a scapula demonstrating medialization of the glenoid relative to the scapula body as seen both at the lateral border (rightward arrow) and at the superomedial angle at the vertebral border (two-way arrow). B. Angulation: a 3D-CT image of the same scapula in a plane parallel to the body mimicking the scapula Y x-ray view. Here the two lines marking the lateral borders on the two fragments create a 45-degree angle to each other. C. Translation: a 3D-CT image of the same scapula and in the same plane as B, but imaging has been taken from the medial side instead of from the lateral side. The amount of translation of the scapula borders, as indicated by the yellow two-way arrow, is easy to appreciate. |
 |
|
Figure 2.3.
This illustration depicts the SSSC, which is an osseoligamentous ring made up of the structures along the broken line circle in this illustration. Goss theorized that if two structures in the ring are disrupted, then a floating shoulder lesion, without osseous or ligamentous continuity between the axial skeleton and the forequarter, would exist. A case of a floating shoulder lesion is illustrated at the end of this chapter (Figs. 2.17, 2.18, 2.19, 2.20, 2.21, 2.22, 2.23, 2.24, 2.25, 2.26). |
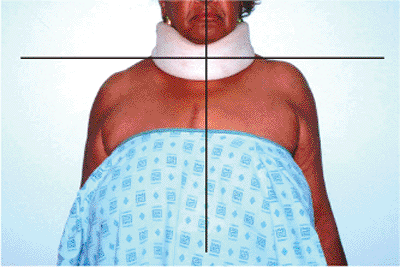
should follow the advanced trauma life support (ATLS) guidelines. In
less seriously injured patients, inspection of the shoulder in a
standing or sitting patient is helpful (Fig. 2.7).
Medial and caudad displacement of the shoulder may be obvious and cause
asymmetry, and it correlates well with the degree of medialization and
depression of the glenoid found on radiographs. Because of pain,
patients with displaced scapula fractures, particularly when associated
with multiple rib or clavicle fractures, cannot voluntarily forward
elevate or externally rotate their shoulders to any significant degree.
 |
|
Figure 2.4.
An AP x-ray of a shoulder that has sustained a double lesion to the SSSC, which has resulted in a floating shoulder. Note the distal clavicle fracture (downward arrow) and glenoid neck fracture (leftward arrow), which are both substantially displaced. |
 |
|
Figure 2.5.
This image depicts the Ideberg classification as it was modified by Mayo et al. The classification is specific for intra-articular glenoid fractures, and it allows for consideration of the commonly associated fractures of the body and processes. It is helpful for determining the surgical approach; for example, an Ideberg I, II fracture should be addressed via an anterior deltopectoral approach, but the Ideberg IV and V injury is best approached posteriorly because the surgeon needs to stabilize the lateral border. |
uncommon, require a careful assessment of the brachial plexus and
distal limb perfusion. Brachial-plexus injuries occur in up to 10% of
patients with scapula fractures and may at times be subtle. Axillary
nerve sensation should be documented; however, motor assessment is
frequently impossible with displaced fractures. The integrity of the
skin should be assessed because abrasions are common after the typical
direct-blow mechanism to the shoulder that causes scapula fractures (Fig. 2.8).
If the circulation in the upper extremity is questionable, vascular
surgery consultation and angiography is strongly recommended.
 |
|
Figure 2.6.
This figure shows the AO/OTA classification for scapula fractures. Though it provides a systematic way of classification, I have found it to be inadequate in classifying 15 out of 40 fracture patterns on which operations were performed consecutively between 1999 and 2002. Furthermore, the types of A, B, and C assigned to scapula fractures do not correspond with extra-articular, partial articular, and complete articular variants as they do for other long-bone articulations. The AO/OTA is currently reviewing and revising this classification scheme to address these concerns. |
proceeding to other studies, which include anteroposterior (AP),
scapula Y, and axillary views. The AP x-ray of the scapula should be
taken 35 degrees off the sagittal plane to correspond with the same
angular position of the scapula on the thorax. The orthogonal scapula Y
view is 90 degrees to the AP. The axillary lateral is the most
difficult to obtain because of patient discomfort, but it is extremely
important.
any x-ray view, then a two-dimensional computed tomography (2D-CT) scan
with 1 mm axial cuts, together with coronal and sagittal
reconstructions, are helpful to delineate articular displacement,
comminution, and fracture location (Fig. 2.9).
If more than 1 cm of fracture displacement is found at the scapula neck
in any x-ray view, then an opposite shoulder AP radiograph and a
three-dimensional (3D)-CT scan should be obtained to better define the
fracture displacement. Being misled with an AP view of the injured
shoulder is common because the glenoid may be significantly angulated
through the lateral border so that visualization of the glenohumeral
joint (clear space) is impossible. In these circumstances, a 3D-CT scan
is helpful in evaluating angular deformity and medialization of the
glenoid.
shoulder, which attaches the upper extremity to the axial skeleton
through the clavicle. Eighteen muscular origins and insertions on the
scapula aid in providing a stable base for glenohumeral mobility. The
goal of surgery is to restore this stable base as well as the
relationship of the axial and appendicular skeleton and thus allow for
early rehabilitation.
 |
|
Figure 2.7.
This image illustrates why a patient should be properly disrobed for an examination. The dramatic depression and medialization (black lines) of the forequarter can occur with high-energy injury. |
 |
|
Figure 2.8.
Severe scarring resulted from abrasions that occurred during impact of the patient’s forequarter. The injury mechanism was caused by a motorcycle crash, and one can imagine the shoulder hitting the gravel embankment at the roadside. To decrease the chance of infection, this patient’s operation was delayed 2.5 weeks until the skin re-epithelialized. |
 |
|
Figure 2.9.
This 2D-CT image illustrates the importance of such a study for the intra-articular variants. The surgeon can appreciate the extensive comminution of the joint and that best access and buttress plating will require a posterior approach. The top arrow depicts the anterior glenoid. |
 |
|
Figure 2.10. A.
A patient in the beach-chair position has an incision to address a clavicle and ipsilateral glenoid fracture (a common pattern). The isolated, anterior, glenoid fractures and Ideberg II fractures are best approached from this approach. In normal circumstances, a deltopectoral incision runs from the coracoid toward the deltoid insertion, but in this case, it was curved proximally and medially over the anterior clavicle. B. The same patient shown in (A) after fixation of the clavicle fracture with a 2.7-mm dynamic compression plate. The orientation is the same in (A) and (C) with the axilla to the left. C. The exposure of the glenoid fracture is shown. The sutures are tagging the infraspinatus, and a Fakuda retractor is inside the joint retracting the humeral head. One can see the interval developed between the deltoid and the infraspinatus as landmarked by the cephalic vein (yellow arrow). |
surgical approaches are used in the vast majority of patients with
displaced scapula fractures: the anterior deltopectoral and posterior
Judet approaches. Patient positioning and draping, implant selection,
cosmesis, and surgical risks are all affected by the approach.
associated transverse fracture extending in a coronal plane from the
superomedial angle or scapula vertebral border through the glenoid, are
best treated through a deltopectoral approach. In these injuries, the
superior glenoid is detached with the coracoid, as in the Mayo Type II
fracture. In most other fractures involving the scapula (scapula neck
or body fracture with or without glenoid involvement), a posterior
approach is preferred. Rarely, combined anterior and posterior
approaches are necessary; for example, they may be required in the case
of concomitant, anterior articular fractures combined with scapula neck
and body variants. The clavicle or acromioclavicular joint may require
a separate approach for fixation when indicated.
process is a curved osseous projection off the anterior neck. It is the
origin for five anatomic structures and an important surgical landmark.
The glenoid process, under the acromion, contains the pear-shaped
glenoid fossa, which is approximately 39 mm in a superior-inferior
direction and 29 mm in an anterior-posterior direction (in the lower
half).
bone with a thin translucent body surrounded by thick borders that are
well developed as points of muscular origins and insertions. The
lateral border of the scapula sweeps up from the inferior angle,
forming the thickest condensation of bone, which ends in the neck of
the glenoid process. The scapula borders and the glenoid neck provide
the best bone for reduction and fixation with plates and screws.
arm board attached to support the extremity. Positioning an x-ray plate
behind the shoulder during the setup will help to obtain an
intraoperative film following reduction and fixation. A small towel
roll under the ipsilateral shoulder helps thrust the shoulder forward.
Direct visualization of the joint will minimize the need for
intraoperative fluoroscopy; however, the surgeon should evaluate a
single, AP, shoulder x-ray after fixation.
point just lateral to the axillary fold, commonly named the
“deltopectoral groove” (Fig. 2.10). This
incision is deepened to the deltopectoral interval where the cephalic
vein is identified and retracted laterally with the deltoid and
protected in the flap. The interval between the deltoid and pectoralis
major is developed down to the clavipectoral fascia, which covers the
coracobrachialis and subscapularis tendon. This fascia is incised and
retractors are placed superiorly and inferiorly. The humerus should be
externally rotated to create tension on the subscapularis tendon and to
improve visualization of the lesser tuberosity. With the humerus in a
neutral position, the subscapularis tendon should be cut 1 cm from its
insertion for later repair. For an accurate closure, the surgeon should
dissect the subscapularis from the capsule as a distinct layer; this
approach is particularly helpful for an anterior glenoid fracture
because the surgeon needs to work on both sides (intra-articular and
extra-articular) of the capsule. The anterior, circumflex, humeral
vessels are at the inferior margin of the subscapularis.
Below
this leash of vessels is the axillary nerve. Stay sutures are placed on
each side of the subscapularis muscle to assist in closure and to avoid
damage to the axillary nerve.
 |
|
Figure 2.11.
This image demonstrates appropriate positioning of the patient when the surgeon is performing a posterior approach to the scapula. Soft-positioning wedges allow for a supportive working surface while protecting the downside arm. The body, positioned on a beanbag, should be allowed to flop forward. The entire arm should be prepped free to allow for manipulation and motion of the glenohumeral joint during the procedure. |
palpable glenoid rim and tagged, or the surgeon can work through the
fracture to wash out the joint (see Fig. 2.10C)
and then obtain an indirect articular reduction by working
extra-articularly with the fragment. Fracture reduction can be improved
with a dental pick or small bone hook, and provisional fixation is
obtained with Kirschner (K) wires. Depending on the size of the
fragment or the degree of comminution, implant (screw) choices may
range from 2.0 to 3.5 mm. Most frequently, a mini buttress plate on the
anterior-inferior edge is appropriate.
no. 2 braided suture. The subcutaneous tissue is approximated with no.
2-0 suture. The skin is closed with a monofilament, subcuticular,
absorbable suture.
high-energy scapula fractures in 10% to 20% of cases. Treatment
requires careful intraoperative patient position. Whenever possible,
the injured vertebral segments should be internally stabilized first to
insure protection of the spinal cord. However, if nonoperative spine
management is chosen, halo traction is preferable to a cervical collar
in terms of patient safety.
position, flopping slightly forward on a beanbag with an axillary roll
well placed. The affected upper extremity should be positioned on an
arm board or Mayo stand to support the extremity in a 90-degree
forward-flexed and slightly abducted position (Fig. 2.11).
The entire shoulder, chest wall, and neck should be prepped and draped
to allow for manipulation of the shoulder. The planned incision is
drawn on the skin with a sterile marker. It is made by following the
prominent posterolateral
acromion
and extending medially to the superomedial angle of the scapula, and
then the incision turns caudad along the vertebral border.
 |
|
Figure 2.12.
The patient is allowed to flop forward, and the scapula landmarks are detailed along with the fracture pattern. The healed abrasion is directly over the fractured posterior spine of the acromion. The incision depicted by the black line is slightly caudad to the acromial spine and lateral to the vertebral border of the scapula. |
and retract the shoulder to create scapulothoracic excursion, the
surgeon feels the bony landmarks with his/her opposite hand. A Judet
posterior incision is planned along these landmarks. The incision
should be 1 cm caudad to the acromial spine and 1 cm lateral to the
vertebral border, which allows closure over a plate and improves
lateral retraction of the flap during surgery (Fig. 2.12).
acromial spine, splitting the interval between trapezius and deltoid
insertions. The incision curves distally around the superomedial angle
and down the vertebral border. For access to the lateral border of the
scapula, the incision must be generous enough to allow for flap
mobilization should the surgeon require a more extensile approach.
Properly executed, the fascial incision along the acromial spine and
medial border should provide a cuff of tissue that is sutured back to
its bony origin at the end of the procedure.
limited or complete exposure of the posterior scapula; this should be
determined in the preoperative plan. Limited windows can be used to
access fractures at the lateral border, acromial spine, and vertebral
border (Fig. 2.13). An extensive approach can
be executed to expose the entire posterior scapula by elevating all
musculature off the infraspinatus fossa (Fig. 2.14).
The extensile approach preserves the entire subscapularis-muscular
sleeve on the anterior surface of the scapula, and of course, the
elevated flap respects vascular planes because the surgeon raises it on
its neurovascular pedicle (suprascapular artery and nerve) (see Fig. 2.14B).
I find it most helpful to utilize an extensile approach for fractures
over a week old by elevating the deltoid, infraspinatus, and teres
minor
in
a single flap. Also, for complex patterns, the extensive approach is
useful when there are more than three exit points around the ring of
the scapula. The extensile exposure allows the surgeon adequate control
of the fracture at multiple points to effect the reduction and mobilize
the fracture by breaking up intervening callus. It will not allow for
exposure of the glenoid due to the large flap, which cannot be
retracted sufficiently lateral for joint exposure.
 |
|
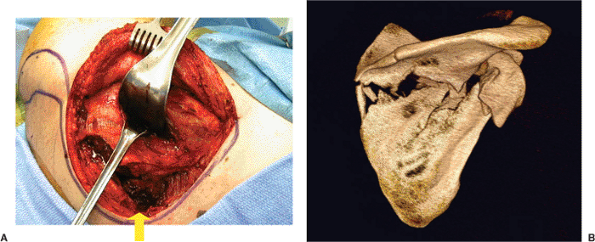
Figure 2.13. A.
An intraoperative photo of the limited windows technique shows that the subcutaneous tissue is elevated with the deltoid muscle (behind the rake retractor) off the rotator cuff. The window depicted by the upward yellow arrow is the superomedial angle shown after the infraspinatus has been dissected from the posterior scapula; the procedure creates an axis for fracture reduction at this common location (B). The other two retractors are in the interval between the infraspinatus and teres minor, and this interval is used to expose the lateral border. B. A 3D-CT scan shows a common fracture pattern, which lends itself to the exposure shown in (A). The exposure allows for reduction and fixation at two key points: the glenoid neck and the superomedial angle. Both sites will be plated. |
intervals around the scapula perimeter can be used to access specific
fracture locations. The muscle plane entered at the acromial
border
is between the trapezius and the deltoid, which lies at the inferior
margin of the spine and is elevated to uncover the rotator cuff
muscles. The deltoid should be dissected off the muscular origin of the
infraspinatus and tagged through its fascial cuff for reattachment
through bone tunnels later. A Key or Cobb elevator can be used to
elevate the infraspinatus and teres minor from the posterior fossa. At
the vertebral border of the scapula, the intermuscular plane is between
the infraspinatus–teres minor and the rhomboids.
 |
|
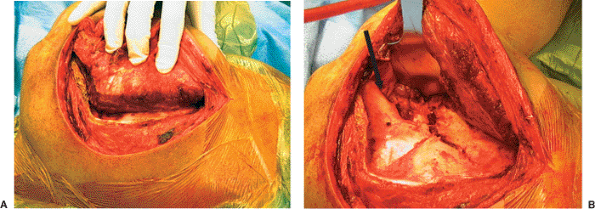
Figure 2.14. A.
The posterior Judet approach results in a flap from the acromial spine and vertebral borders. This extensile exposure will allow for visualization of the entire infraspinatus fossa (the posterior scapula) from the vertebral border to the lateral border as shown in (B). The surgeon’s fingers are reflecting the entire flap en mass, and a Cobb elevator is used to dissect the flap off the flat, posterior, scapular surface. This approach is best reserved for cases in which surgery has been delayed for more than 10 days from the time of injury or for cases in which severe comminution is present with several displaced-fracture lines exiting multiple scapular borders. It cannot be used when the surgeon desires intra-articular inspection. B. Image of same patient shown in (A) after flap elevation and retraction. This patient has a fracture variant that is characterized by a broken glenoid neck from the lateral border up into the supraglenoid notch. Extension of another fracture line into the body is apparent in this image, but the severe medialization and anteversion of the glenoid articular surface is not apparent. Note the threat of a retractor by virtue of traction on the suprascapular neurovascular bundle exiting from just below the acromion before it enters the infraspinatus muscle (black arrow). |
 |
|
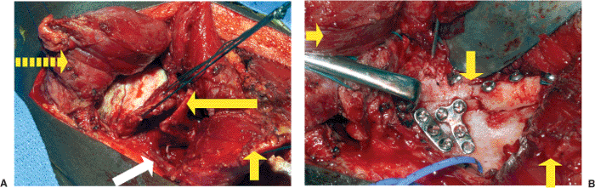
Figure 2.15. A.
Intraoperative photo demonstrating the exposure after a capsulotomy. This image was taken after the articular reduction of the glenoid, which had been in four major fragments. The rightward broken arrow points to the deltoid muscle taken off the acromial spine. The sutures are tagging and retracting the joint capsule. The leftward arrow points to a fragment of displaced lateral border (glenoid neck). The upward arrow points to the infraspinatus, which has been tenotomized for better joint exposure and is on its neurovascular pedicle; the suprascapular artery and nerve are depicted by the white arrow. B. This image is of the same patient depicted in (A) after undergoing reconstruction of the lateral border and with the joint capsule retracted to the left over the joint. The downward arrow points to the lateral border; the upward arrow points to the infraspinatus; the vessel loop is on the suprascapular nerve and artery; the rightward arrow points to the deltoid. |
is between the infraspinatus and teres minor because it allows access
to the lateral border of the scapula and glenohumeral joint.
Identification of the correct interval is important to avoid
denervation of the infraspinatus or injury to the axillary nerve and
posterior humeral-circumflex artery in the quadrangular space. Once
this important interval is developed, the lateral border of the scapula
is exposed to allow reduction and correction of glenoid version or
medialization. If the glenoid articular surface must be assessed
directly, then a transverse capsulotomy can be made so a retractor can
be placed on the anterior edge of the glenoid and the humeral head can
be retracted (Fig. 2.15).
scapula are important because specific retractors and reduction tools
have not been specifically designed for the scapula. At least two,
small, pointed, bone reduction clamps and two, 4-mm, Schantz pins with
a small external fixator set, as well as a pair of T-handle chucks, are
helpful. Often a 2.7-mm, dynamic, compression plate straddling the
lateral border fracture can be helpful for reduction (as well as
definitive fixation) because it can be applied perfectly straight on
this border. Pointed reduction tenacula are frequently inadequate due
to interference with the flap, so a Schantz pin in the proximal and
distal segments can be placed in the proper orientation with a small
external fixator to reduce the lateral border for subsequent plating.
If the reduction is still not stable, a provisional 2.0-mm plate and
screws placed slightly more medial can keep the lateral border aligned.
Furthermore, a clamp can be placed at an
associated
fracture at the acromial or vertebral border to help off-load stresses
on the lateral border while the reduction is maintained.
 |
|
Figure 2.16. A.
The superomedial angle postfixation with a 2.7-mm reconstruction plate. This implant is chosen for its malleability over a difficult contour. This is the same patient depicted in Figure 2.13. A 2.7-mm dynamic-compression plate was chosen for the lateral border because it is relatively strong and requires no contour to lay straight along the glenoid neck. B. An immediate postoperative AP chest x-ray that corresponds to the patient in Figure 2.16A. A chest x-ray is helpful to appreciate that the glenoid has been properly oriented relative to the opposite side. |
are sufficiently strong and are not associated with breakage. In
addition, they have a lower profile than 3.5 plates, are easier to
contour, and allow for greater screw options. A 2.7-mm
dynamic-compression plate is used on the lateral border where stresses
are greatest, and 2.7-mm reconstruction plates are used for the
acromial and vertebral borders of the scapula because they make
contoured fitting, particularly around the superomedial angle, much
easier (Fig. 2.16). I have found that two pediatric
Kocher clamps are useful for this maneuver. Longer plates with more
screws should be used at the acromial and vertebral borders because
each screw is typically 8 to 10 mm.
 |
|
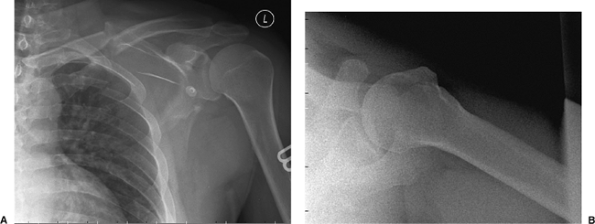
Figure 2.17. A.
AP shoulder x-ray taken at the patient’s first emergency room visit. This image reveals a minimally displaced clavicle fracture with a butterfly fragment, a scapula body fracture that exits the lateral border at the glenoid neck, and rib fractures of at least levels 2 through 5. Minimal glenoid medialization is found. B. An axillary view of the injured shoulder demonstrating no acromial nor coracoid process fractures, no intra-articular extension of the fracture, and no subluxation of the glenohumeral joint. |
intra-articular glenoid fracture with glenoid neck involvement and
minimal displacement or involvement of the acromial spine and vertebral
border, a direct posterior approach to the scapular neck or joint can
be employed. In these cases, the pathology can be determined and the
desired reduction and fixation can be accomplished through the interval
between the teres minor and the infraspinatus muscles.
comminution, greater exposure of the joint can be gained with an
infraspinatus tenotomy where 1 cm of cuff insertion is left at the
greater tuberosity for repair. This allows the slender musculotendinous
portion of the infraspinatus to be retracted off the superior glenoid
region for better access to the glenohumeral joint. It is repaired with
two heavy-braided no. 2 sutures at closure. External rotation against
resistance should be protected for 6 postoperative weeks in the case of
this repair.
extrinsic adhesions and shoulder stiffness are eliminated prior to
waking the patient; this is especially important in cases where surgery
has been delayed. This manipulation at the end of the procedure is one
reason the entire extremity is preoperatively prepped. To insure that
the repair is secure and early rehabilitation is possible, the wound is
closed over a suction drain under the flap through use of braided no. 2
nonabsorbable sutures placed through several drill holes at the
acromion spine and vertebral border. The rest of the musculofascial
closure can be performed with a no. 1 absorbable, braided suture. For
cosmesis, the skin is closed with a subcuticular absorbable stitch.
is based on an identical principle: stable fixation to withstand
physiologic stresses of early motion to minimize shoulder stiffness.
After surgery, full, passive range of motion should be instituted
during the first week. Continuous passive motion (CPM) is not commonly
used unless the patient cannot cooperate with rehabilitation adequately
or also has an ipsilateral proximal humerus or elbow injury. For
patients with profound brachial plexopathy, CPM may be used for
extended periods.
regain and maintain shoulder motion. Activities of daily living are
encouraged, but no lifting, pushing, pulling, or carrying is allowed
for 4 weeks. The use of pulleys, push-pull sticks in the opposite
extremity, and supine assisted motion is helpful. A regional anesthetic
block with an indwelling interscalene catheter for the first 48 to 72
postoperative hours is an excellent adjunctive method to promote early
shoulder motion. Ipsilateral elbow, wrist, and hand exercises including
3- to 5-lb weights (on a supported elbow) are encouraged. These
exercises will prevent muscular atrophy and promote reduction of limb
edema.
postoperatively, and an AP, scapula Y, and axillary radiographs are
obtained. Follow-up at 6 months and 1 year is appropriate to document
return of maximum function. Patients with associated brachial
plexopathy should be followed by an experienced specialist because some
patients may benefit from brachial plexus exploration, tendon
transfers, or neural grafting. For the patient with a dense or
irrecoverable plexus lesion (flail shoulder) an arthrodesis should be
strongly considered.
be protected against external rotation past neutral. Likewise, motion
against resistance should be avoided for a full 6 weeks to allow
healing of the subscapularis, which had been repaired during exposure
of the glenohumeral joint. After posterior approaches in which the
infraspinatus and teres minor have been mobilized from their origins
and in which the deltoid is taken off the acromial spine, these muscles
must be protected for 6 weeks. At 6 weeks, patients begin a weight
program, beginning with 3 to 5 lbs and increasing as the patient’s
symptoms allow.
improve with therapy. This is more common in patients with brachial
plexus injuries, a head injury, halo-vest protection
for
spine injury, or complex associated fractures of the ipsilateral
extremity. In these patients, a manipulation under anesthesia to
jump-start shoulder motion can be helpful. At 3 months after surgery,
restrictions can usually be lifted, and the patient can resume a
strength and endurance program until fully conditioned.
injuries to the ipsilateral extremity, particularly when the brachial
plexus is involved. Other complications include nonunion, malunion,
degenerative glenohumeral joint disease, and instability. Shoulder
instability and resultant pain and dysfunction can arise from severe
angular deformity of the glenoid neck. These complications are far less
likely to occur with anatomic restoration of the scapula and its
articular surface.
risk of suprascapular nerve injury. This leads to wasting of the
rotator cuff musculature, which may never recover. The surgeon must
take intraoperative care to avoid excessive traction on the
neurovascular bundle as the infraspinatus flap is retracted at the
lateral border.
Early aggressive rehabilitation, particularly in those patients with
ipsilateral injuries, is recommended. If at the 6 week follow-up,
motion is poor, manipulation of the patient’s shoulder under anesthesia
combined with shoulder arthroscopy is very useful in restoring shoulder
motion.
at work. He was evaluated at a hospital emergency room and subsequently
admitted with severe left-shoulder pain and difficulty breathing. He
was diagnosed with a broken scapula, clavicle, and multiple fractured
left ribs (Fig. 2.17). After 2 days of pain
control, the patient was sent home with a sling. He had been evaluated
by an orthopedic surgeon in the hospital who explained to the patient
that his broken bones would heal without additional treatment and that
his prognosis for normal recovery was good.
 |
|
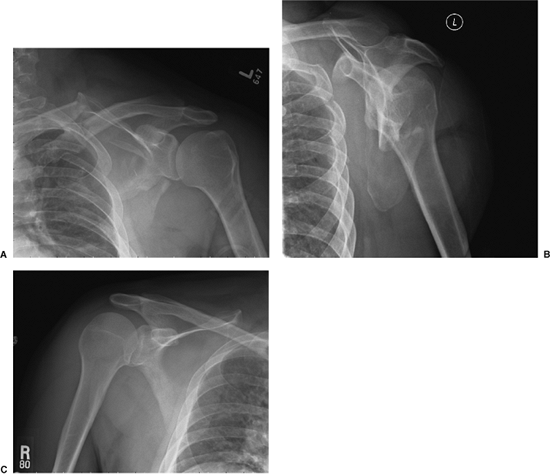
Figure 2.18. A.
This AP x-ray image of the shoulder reveals substantial displacement of all fractured bones, which had not been evident in the initial films of the injury. The clavicle is medialized well over 1 cm; the glenoid has medialized markedly and has a caudad-facing attitude; perhaps most impressive, the marked displacement of all the rib fractures indicates that the entire forequarter has medialized en mass. B. This is a scapula Y radiograph taken 3 weeks after the injury showing substantial translation of the lateral border. This border is displaced by approximately 3 cm, and significant angular deformity is evident. C. A comparison view of the opposite shoulder was used as a template to evaluate the injured shoulder (A). Side by side, these two images highlight the amount of scapular displacement, which is striking, as well as the coronal plane relationship to the chest wall. |
move his shoulder, the patient presented in my office with a workers’
compensation agent who had suggested that he obtain a second opinion.
Physical examination revealed that the left shoulder was markedly
depressed and medialized. The neurovascular exam at the level of the
left hand revealed no abnormality. When the patient was asked to try
and move his shoulder, the patient simply replied, “It won’t move even
when I want it to.” Attempts at active range of motion were indeed
futile; although he was taken passively to 30 degrees of forward
flexion before stiffness could not be overcome. The pain was
substantial. His neck was not tender, and his cervical motion was full,
but he experienced spasms in the trapezius muscle.
 |
|
Figure 2.19. A.
This is a 3D-CT reconstructed image of the scapula in the plane most perpendicular to the scapula body. This rotational image helps one to appreciate the medialization and angular deformity of the glenoid relative to the distal scapula-body fragment. The displacement of the scapula body at the superomedial angle can also be seen as a medialized, superior, scapula segment (attached to the glenoid). Comminution in the infraspinatus fossa is marked. The clavicular medialization is also confirmed in this image. B. A 3D-CT image representing the plane most parallel to the body of the scapula. In this view, semicoronal angular deformity can be measured off the proximal and distal scapula borders (35 degrees in this case). Also appreciated is the severe anteversion of the glenoid. |
and the patient learned the risks and benefits of surgery. Two days
later the patient was taken to the operating room for surgical fixation
of the scapula and clavicle. The relative indications for surgery were
multiple and included medial displacement of more than 15 mm, angular
deformity of greater than 25 degrees, grotesque clinical deformity,
seven broken bones in the forequarter, and a floating shoulder (double
lesion of the SSSC).
position, flopping slightly forward, and a Judet posterior approach was
used to mobilize the entire muscle flap. The callus was cleaned from
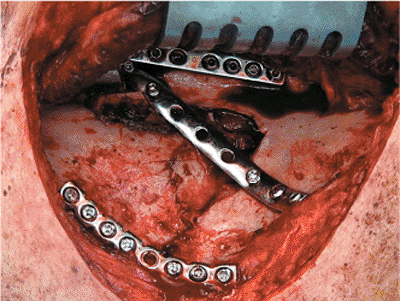
the fracture lines so that the reduction could be visualized (Fig. 2.20).
Schantz pin joysticks (with T-handled chucks) were used in the glenoid
neck and lateral border to achieve the reduction. The lateral border
was plated first followed by plating of the superomedial angle (Fig. 2.21).
 |
|
Figure 2.20.
This intraoperative photograph was taken from the vantage point of the surgeon, who stood on the posterior side of the patient. Behind the retractor is the muscle flap containing the deltoid, infraspinatus, and teres minor. Fracture callus has been removed and saved to pack into fracture lines before wound closure. The open approach, in which the entire flap is elevated, was used because 3.5 weeks had passed since the time of this patient’s injury; thus, this exposure was necessary to mobilize callus, and reduction aids were needed to overcome a static deformity. |
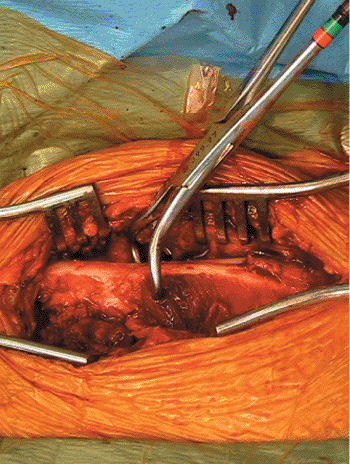
intraoperative shoulder x-ray revealed marked clavicle-fracture
displacement. The clavicle was subsequently fixed with a tension band
plate along the superior border (Figs. 2.22, 2.23, 2.24).
surgeon manipulated the shoulder until full motion was restored. This
manipulation also relieves the intrinsic and extrinsic contractures
that form in a month. Formal postoperative x-rays were taken in the
recovery room (Fig. 2.25). The patient worked
with physical therapy immediately on full and aggressive, passive,
range-of-motion exercises. He remarked (as most patients do) that his
shoulder felt completely “different and restored” the day after surgery
and that he was able to move it for the first time since his injury. At
1 month, he was advanced to full, active, range-of-motion activity with
light weights (3 to 5 lb) beginning at 6 weeks. By 3 months after
surgery, he had returned to work, had no pain, and stated that he had
full motion.
At 6 months, his shoulder was asymptomatic. His motion was within at
least 90% of the motion of opposite shoulder in all directions, and he
complained of no deficit in strength. His Disabilities of the Arm,
Shoulder, and Hand (DASH) exam score was 16 (scale 1–100;
normative-scale functional score = 10.1).
 |
|
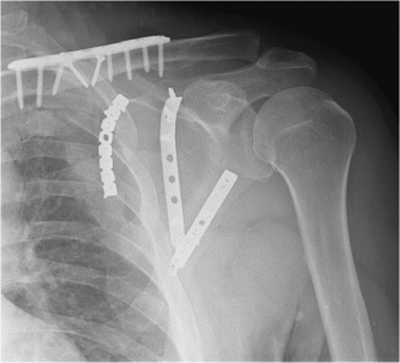
Figure 2.21.
This intraoperative photograph shows the fixation construct using a nine-hole 2.7-mm dynamic compression plate (Synthes, Paoli, PA) for the lateral border, an eight-hole 2.7-mm reconstruction plate (Synthes) contoured around the superomedial angle of the scapula, and a seven-hole locking, one-third, tubular plate with locking screws (Synthes) deployed in the proximal and distal body fragments. The locking plate off-loads the other two nonlocking plates that have short screws: 8 to 10 mm on the vertebral border and 12 to 16 mm on the acromial and lateral borders. Directly behind and to the right of the Israel retractor is the suprascapular neurovascular bundle as it exits from beneath the acromion. Great care must be exercised in retracting this flap to preserve the functional integrity of these structures. |
 |
|
Figure 2.22.
The surgical exposure of the clavicle fracture after it has been cleaned. The butterfly fragment is not in view; it had been reduced and fixed with 2.7-mm lag screws. The surgeon can access this site from either the anterior or posterior position. I have chosen to work from the posterior position (same as for the scapula) and thus the easiest access was to the superior border of the clavicle, which is more convenient in the patient who requires scapula surgery in the floppy lateral or forward position. The scapula and clavicle procedures can usually be done with a single prep and drape, but in this case, the procedures were done separately. |
 |
|
Figure 2.23.
A pointed, bone, reduction forceps was used to reduce the fracture. The photograph is taken from the vantage point of the anesthesiologist. |
 |
|
Figure 2.24. An eight-hole, precontoured, titanium, nonlocking plate (Acumed, Hillsboro, OR) was used for the clavicle stabilization.
|
 |
|
Figure 2.25. A.
Postoperative AP x-ray showing the reconstructed scapula and clavicle in proper orientation. Note the gap at the lateral border, which is often difficult to define and reduce in the comminuted variants that undergo delayed surgery. B. A postoperative scapula-Y x-ray image demonstrating proper alignment and orientation of the lateral border. C. A postoperative, axillary, x-ray view can be used to insure that all screws are in extra-articular position. |
 |
|
Figure 2.26. An x-ray image taken 6 months after the operation showing complete consolidation of fracture lines.
|
JP, Gabriel JP, Schneck SL, et al. The normal glenohumeral
relationships, an anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am 1992;74:491–500.
GR Jr, Naranja J, Klimkiewicz J, et al. The floating shoulder: a
biomechanical basis for classification and management. J Bone Joint Surg Am 2001;83A:1182–1187.
of the management of fractures and dislocations (based on analysis of
4,390 cases) by staff of the Fracture Service MGH, Boston. Philadelphia: JB Lippincott; 1938.
