Tibial Plateau
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 36 – Tibial Plateau
36
Tibial Plateau
EPIDEMIOLOGY
-
Tibial plateau fractures constitute 1% of all fractures and 8% of fractures in the elderly.
-
Isolated injuries to the lateral plateau
account for 55% to 70% of tibial plateau fractures, as compared with
10% to 25% isolated medial plateau fractures and 10% to 30% bicondylar
lesions. -
From 1% to 3% of these fractures are open injuries.
ANATOMY
-
The tibia is the major weight-bearing bone of the leg, accounting for 85% of the transmitted load.
-
The tibial plateau is composed of the
articular surfaces of the medial and lateral tibial plateaus, on which
are the cartilaginous menisci. The medial plateau is larger and is
concave in both the sagittal and coronal axes. The lateral plateau
extends higher and is convex in both sagittal and coronal planes. -
The normal tibial plateau has a 10-degree posteroinferior slope.
-
The two plateaus are separated from one
another by the intercondylar eminence, which is nonarticular and serves
as the tibial attachment of the cruciate ligaments. Three bony
prominences exist 2 to 3 cm distal to the tibial plateau. Anteriorly is
the tibial tubercle on which the patellar ligament inserts. Medially,
the pes anserinus serves as attachment for the medial hamstrings.
Laterally, the Gerdy tubercle is the insertion site of the iliotibial
band. -
The medial articular surface and its
supporting medial condyle are stronger than their lateral counterparts.
As a result, fractures of the lateral plateau are more common. -
Medial plateau fractures are associated
with higher energy injury and more commonly have associated soft tissue
injuries, such as disruptions of the lateral collateral ligament
complex, lesions of the peroneal nerve, and damage to the popliteal
vessels.
MECHANISM OF INJURY
-
Fractures of the tibial plateau occur in
the setting of varus or valgus forces coupled with axial loading. Motor
vehicle accidents account for the majority of these fractures in
younger individuals, but elderly patients with osteopenic bone may
experience these after a simple fall. -
The direction and magnitude of the
generated force, age of the patient, bone quality, and amount of knee
flexion at the moment of impact determine fracture fragment size,
location, and displacement:-
Young adults with strong, rigid bone
typically develop split fractures and have a higher rate of associated
ligamentous disruption. -
Older adults with decreased bone strength
and rigidity sustain depression and split-depression fractures and have
a lower rate of ligamentous injury. -
A bicondylar split fracture results from a severe axial force exerted on a fully extended knee.
P.383 -
CLINICAL EVALUATION
-
Neurovascular examination is essential,
especially with high-energy trauma. The trifurcation of the popliteal
artery is tethered posteriorly between the adductor hiatus proximally
and the soleus complex distally. The peroneal nerve is tethered
laterally as it courses around the fibular neck. -
Hemarthrosis frequently occurs in the
setting of a markedly swollen, painful knee on which the patient is
unable to bear weight. Knee aspiration may reveal marrow fat. -
Direct trauma is usually evident on
examination of the overlying soft tissues, and open injuries must be
ruled out. Intraarticular instillation of 50 to 75 mL saline may be
necessary to evaluate possible communication with overlying lacerations -
Compartment syndrome must be ruled out, particularly with higher-energy injuries.
-
Assessment for ligament injury is essential.
ASSOCIATED INJURIES
-
Meniscal tears occur in up to 50% of tibial plateau fractures.
-
Associated ligamentous injury to the cruciate or collateral ligaments occurs in up to 30% of tibial plateau fractures.
-
Young adults, whose strong subchondral
bone resists depression, are at the highest risk of collateral or
cruciate ligament rupture. -
Fractures involving the medial tibial
plateau are associated with higher incidences of peroneal nerve or
popliteal neurovascular lesions owing to higher-energy mechanisms; it
is postulated that many of these represent knee dislocations that
spontaneously reduced. -
Peroneal nerve injuries are caused by stretching (neurapraxia); these will usually resolve over time.
-
Arterial injuries frequently represent
traction induced intimal injuries presenting as thrombosis; only rarely
do they present as transection injuries secondary to laceration or
avulsion.
RADIOGRAPHIC EVALUATION
-
Anteroposterior and lateral views
supplemented by 40-degree internal (lateral plateau) and external
rotation (medial plateau) oblique projections should be obtained. -
A 10- to 5-degree caudally tilted plateau view can be used to assess articular step-off.
-
Avulsion of the fibular head, the Segond
sign (lateral capsular avulsion) and Pellegrini-Steata lesion
(calcification along the insertion of the medial collateral ligament)
are all signs of associated ligamentous injury. -
A physician-assisted traction view is
often helpful in higher-energy injuries with severe impaction and
metadiaphyseal fragmentation to delineate the fracture pattern better
and to determine the efficacy of ligamentotaxis for fracture reduction. -
Stress views, preferably with the patient
under sedation or anesthesia and with fluoroscopic image
intensification, are occasionally useful for the detection of
collateral ligament ruptures. -
Computed tomography with two- or
three-dimensional reconstruction is useful for delineating the degree
of fragmentation or depression of the articular surface, as well as for
preoperative planning. -
Magnetic resonance imaging is useful for
evaluating injuries to the menisci, the cruciate and collateral
ligaments, and the soft tissue envelope. -
Arteriography should be performed if there is a question of vascular compromise.
P.384
CLASSIFICATION
Schatzker (Fig. 36.1)
| Type I: | Lateral plateau, split fracture |
| Type II: | Lateral plateau, split depression fracture |
| Type III: | Lateral plateau, depression fracture |
| Type IV: | Medial plateau fracture |
| Type V: | Bicondylar plateau fracture |
| Type VI: | Plateau fracture with separation of the metaphysis from the diaphysis |
-
Types I to III are low-energy injuries.
-
Types IV to VI are high-energy injuries.
-
Type I usually occurs in younger individuals and is associated with medial collateral ligament injuries
-
Type III usually occurs in older individuals (Fig. 36.1)
OTA Classification of Tibial Plateau Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT
Nonoperative
-
Indicated for nondisplaced or minimally displaced fractures and in patients with advanced osteoporosis.
-
Protected weight bearing and early range of knee motion in a hinged fracture-brace are recommended.
-
Isometric quadriceps exercises and
progressive passive, active-assisted, and active range-of-knee motion
exercises are indicated. -
Partial weight bearing (30 to 50 lb) for 8 to 12 weeks is allowed, with progression to full weight bearing.
Operative
-
Surgical indications:
-
The reported range of articular depression that can be accepted varies from <2 mm to 1 cm.
-
Instability >10 degrees of the nearly
extended knee compared to the contralateral side is an accepted
surgical indication. Split fractures are more likely to be unstable
than pure depression fractures in which the rim is intact.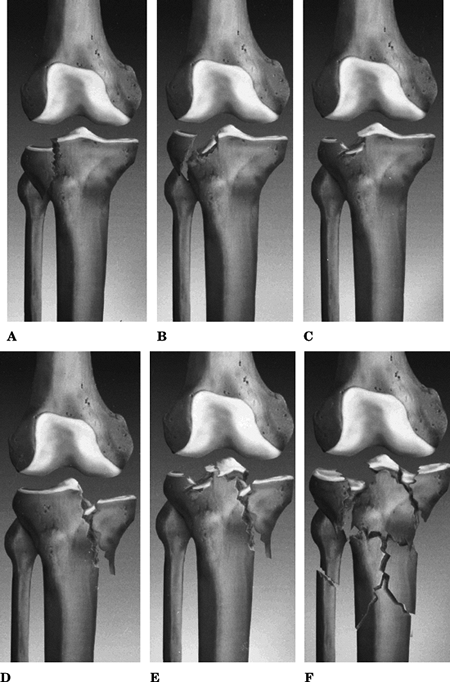 Figure 36.1. Schatzker classification.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 36.1. Schatzker classification.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Open fractures should be treated surgically.
-
Compartment syndrome is a surgical indication.
-
Associated vascular injury is an indication.
P.385P.386 -
-
Operative treatment principles
-
Reconstruction of the articular surface, followed by reestablishment of tibial alignment, is the goal.
-
Treatment involves buttressing of elevated articular segments with bone graft or bone graft substitute.
-
Fracture fixation can involve use of plates and screws, screws alone, or external fixation.
-
The choice of implant is related to the
fracture patterns, the degree of displacement, and familiarity of the
surgeon with the procedure. -
Adequate soft tissue reconstruction
including preservation and/or repair of the meniscus as well as
intraarticular and extraarticular ligamentous structures should be
addressed.
-
-
Spanning external fixation across the
knee can be used as a temporizing measure in patients with
higher-energy injuries. The external fixator is used to keep the soft
tissues out to length and provides some degree of fracture reduction
before definitive surgery. -
Arthroscopy may be used to evaluate the
articular surfaces, the menisci, and the cruciate ligaments. It may
also be used for evacuation of hemarthrosis and particulate debris, for
meniscal procedures, and for arthroscopic-assisted reduction and
fixation. Its role in the evaluation of rim disorders and its utility
in the management of complicated fractures are limited. -
An avulsed anterior cruciate ligament
with a large bony fragment should be repaired. If the fragment is
minimal or the ligament has an intrasubstance tear, reconstruction
should be delayed. -
Surgery in isolated injuries should
proceed after a full appreciation of the personality of the fracture.
This delay will also allow swelling to subside and local skin
conditions to improve. -
Schatzker type I to IV fractures can be
fixed with percutaneous screws or lateral placed periarticular plate.
If satisfactory closed reduction (<1-mm articular step-off) cannot
be achieved with closed techniques, open reduction and internal
fixation are indicated. -
The menisci should never be excised to facilitate exposure.
-
Depressed fragments can be elevated from
below en masse by using a bone tamp working through the split component
or a cortical window. The metaphyseal defect should be filled with
cancellous autograft, allograft, or a synthetic substitute. -
Type V and VI fractures can be managed
using plate and screws, a ring fixator, or a hybrid fixator. Limited
internal fixation can be added to restore the articular surface. -
Percutaneous inserted plating, which is a
more biologic approach, has been described. In this technique, the
plate is slid subcutaneously without soft tissue stripping. -
Use of locked plates has eliminated the need for double plating bicondylar tibial plateau fractures.
-
Fractures of the posterior medial plateau may require a posteromedial incision for fracture reduction and plate stabilization.
-
Postoperative non–weight bearing with continuous passive motion and active range of motion is encouraged.
-
Weight bearing is allowed at 8 to 12 weeks.
P.387
COMPLICATIONS
-
Knee stiffness: This is common, related
to trauma from injury and surgical dissection, extensor retinacular
injury, scarring, and postoperative immobility. -
Infection: This is often related to
ill-timed incisions through compromised soft tissues with extensive
dissection for implant placement. -
Compartment syndrome: This uncommon but
devastating complication involves the tight fascial compartments of the
leg. It emphasizes the need for high clinical suspicion, serial
neurovascular examinations, particularly in the unconscious or obtunded
patient, aggressive evaluation, including compartment pressure
measuring if necessary, and expedient treatment consisting of emergency
fasciotomies of all compartments of the leg. -
Malunion or nonunion: This is most common
in Schatzker VI fractures at the metaphyseal-diaphyseal junction,
related to comminution, unstable fixation, implant failure, or
infection. -
Posttraumatic osteoarthritis: This may
result from residual articular incongruity, chondral damage at the time
of injury, or malalignment of the mechanical axis. -
Peroneal nerve injury: This is most
common with trauma to the lateral aspect of the leg where the peroneal
nerve courses in proximity to the fibular head and lateral tibial
plateau. -
Popliteal artery laceration.
-
Avascular necrosis of small articular fragments: This may result in loose bodies within the knee.
