Thoracolumbar Spine
-
Neurologic injury complicates 15% to 20% of fracture at the thoracolumbar level.
-
Sixty-five percent of thoracolumbar
fractures occur as a result of motor vehicle trauma or fall from a
height, with the remainder caused by athletic participation and assault. -
Recent data have indicated that
motorcycle accidents are associated with a greater chance of severe and
multiple level spinal column injuries than other types of vehicular
trauma.
-
The thoracolumbar spine consists of 12 thoracic vertebrae and 5 lumbar vertebrae.
-
The thoracic level is kyphotic, the
lumbar region lordotic. The thoracolumbar region, as a transition zone,
is especially prone to injury. -
The thoracic spine is much stiffer than
the lumbar spine in flexion-extension and lateral bending, reflecting
the restraining effect of the rib cage as well as the thinner
intervertebral discs of the thoracic spine. -
Rotation is greater in the thoracic
spine, achieving a maximum at T8-T9. The reason is the orientation of
the lumbar facets, which limit the rotation arc to approximately 10
degrees for the lumbar spine versus 75 degrees for the thoracic spine. -
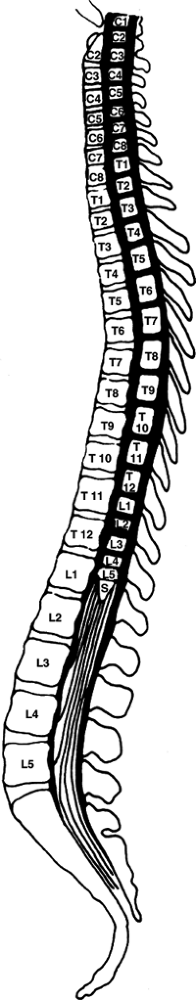
The conus medullaris is found at the
L1-L2 level. Caudal to this is the cauda equina, which comprises the
motor and sensory roots of the lumbosacral myelomeres (Fig. 10.1). -
The corticospinal tracts demonstrate polarity, with cervical fibers distributed centrally and sacral fibers peripherally.
-
The ratio of the spinal canal dimensions
to the spinal cord dimensions is smallest in the T2-T10 region, which
makes this area prone to neurologic injury after trauma. -
Neurologic deficits secondary to skeletal
injury from the first through the tenth thoracic levels are frequently
complete deficits, primarily related to spinal cord injury with varying
levels of root injury. The proportion of root injury increases with
more caudal injuries, with skeletal injuries caudal to L1 causing
entirely root injury. -
The region between T2 and T10 is a
circulatory watershed area, deriving its proximal blood supply from
antegrade vessels in the upper thoracic spine and distally from
retrograde flow from the artery of Adamkiewicz, which can be variably
located between T9 to L2. -
Most thoracic and lumbar injuries occur
within the region between T11 and L1, commonly referred to as the
thoracolumbar junction. This increased susceptibility can be explained
by a variety of factors. The thoracolumbar junction is a transition
P.104P.105
zone between the relatively stiff thoracic spine and the more mobile lumbar spine.
 |
|
Figure 10.1. The relationship between myelomeres (spinal cord segments) and the vertebral bodies.
(From Benson DR, Keenen TL. Evaluation and treatment of trauma to the vertebral column. Instr Course Lect 1990;39:577.)
|
-
These generally represent high-energy injuries, typically from motor vehicle accident or falls from a height.
-
They may represent a combination of flexion, extension, compression, distraction, torsion, and shear.
-
Patient assessment: This involves airway, breathing, circulation, disability, and exposure (ABCDE).
-
Initiate resuscitation: Address
life-threatening injuries. Maintain spine immobilization. Watch for
neurogenic shock (hypotension and bradycardia). -
Evaluate the level of consciousness and neurologic impairment: Glasgow Coma Scale.
-
Assess head, neck, chest, abdominal, pelvic, extremity injury.
-
Ascertain the history: mechanism of
injury, witnessed head trauma, movement of extremities/level of
consciousness immediately following trauma, etc. -
Physical examination
-
Back pain and tenderness
-
Lacerations, abrasions and contusions on back
-
Abdominal and/or chest ecchymosis from seat belt injury (also suggestive of liver, spleen or other abdominal injury)
-
-
Neurologic examination
-
Cranial nerves
-
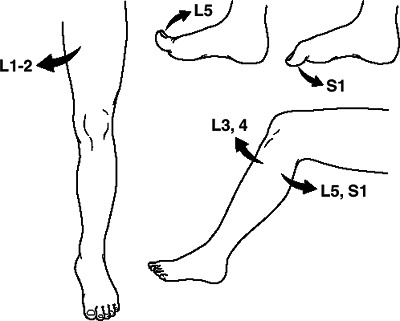
Complete motor and sensory examination (Figs. 10.2 and 10.3)
-
Upper and lower extremity reflexes
![]() Figure
Figure
10.2. A screening examination of the lower extremities assesses the
motor function of the lumbar and first sacral nerve roots: hip
adductors, L1-L2; knee extension, L3-L4; knee flexion, L5-S1; great toe
extension, L5; and great toe flexion, S1.(From Benson DR, Keenen TL. Evaluation and treatment of trauma to the vertebral column. Instr Course Lect 1990;39:583.) -
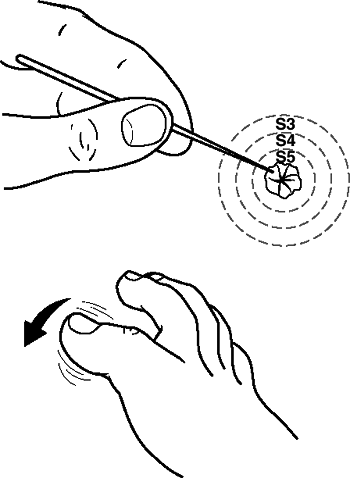
Rectal examination: perianal sensation, rectal tone (Fig. 10.4)
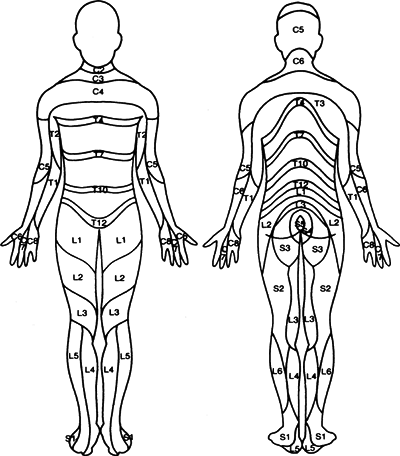 Figure
Figure
10.3. A pain and temperature dermatome chart. These sensory modalities
are mediated by the lateral spinothalamic tract. Note that C4 includes
the upper chest just superior to T2. The rest of the cervical and T1
roots are located in the upper extremities. There is overlap in the
territories subserved by each sensory root and variation among
individuals.(From Benson DR, Keenen TL. Evaluation and treatment of trauma to the vertebral column. Instr Course Lect 1990;39:584.) -
Bulbocavernosus reflex (Fig. 10.5)
-
-
In the alert and cooperative patient, the
thoracic and lumbar spine can be “cleared” with the absence of pain or
tenderness or distraction mechanism of injury and a normal neurologic
examination. Otherwise, imaging is required.
-
Anteroposterior (AP) and lateral views of the thoracic and lumbar spine are obtained.
-
Abnormal widening of the interpedicular
distance signifies lateral displacement of vertebral body fragments,
typical of burst fractures. -
Vertebral body height loss can be measured by comparing the height of the injured level with adjacent uninjured vertebrae.
![]() Figure 10.4. Sacral sparing may include the triad of perianal sensation, rectal tone, and great toe flexion.(From Benson DR, Keenen TL. Evaluation and treatment of trauma to the vertebral column. Instr Course Lect 1990;39:580.)
Figure 10.4. Sacral sparing may include the triad of perianal sensation, rectal tone, and great toe flexion.(From Benson DR, Keenen TL. Evaluation and treatment of trauma to the vertebral column. Instr Course Lect 1990;39:580.)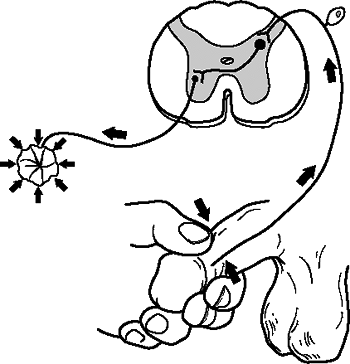 Figure
Figure
10.5. The bulbocavernosus reflex arc is mediated by the conus
medullaris and the lower three sacral roots. Stimulation of the glans
penis, glans clitoris, or gentle traction on a Foley catheter to
stimulate the bladder will evoke contraction of the rectal sphincter.(From Benson DR, Keenen TL. Evaluation and treatment of trauma to the vertebral column. Instr Course Lect 1990;39:578.) -
Quantification of sagittal plane alignment can be performed using the Cobb method.
-
Chest and abdominal radiographs obtained
during the initial trauma survey are not adequate for assessing
vertebral column injury. -
Computed tomography (CT) and/or magnetic
resonance imaging of the injured area may be obtained to characterize
the fracture further, to assess for canal compromise, and to evaluate
the degree of neural compression. -
CT scans provide finer detail of the bony
involvement in thoracolumbar injuries, and MRI can be used to evaluate
for soft tissue injury to the cord, intervertebral discs or for
posterior ligamentous disruption.
middle osteoligamentous complex (posterior longitudinal ligament,
posterior half of vertebral body and posterior annulus fibrosus)
-
Axial compression
-
Axial distraction
-
Translation within the transverse plane
-
Wedge-compression fracture.
-
Stable burst fracture.
-
Unstable burst fracture.
-
Chance fracture.
-
Flexion-distraction injury.
-
Translational injuries.
-
This is a “load-sharing classification.”
-
A point value is assigned to the degree
of vertebral body comminution, fracture fragment apposition, and
kyphosis. Based on their primary outcome of hardware failure, McCormack
et al. concluded that injuries with scores greater than 6 points would
be better treated with the addition of anterior column reconstruction
to posterior stabilization. A recent study demonstrated very high
interobserver and intraobserver reliability of this classification
system.
-
Articular process fractures (1%)
-
Transverse process fractures (14%)
-
Spinous process fractures (2%)
-
Pars interarticularis fractures (1%)
 |
|
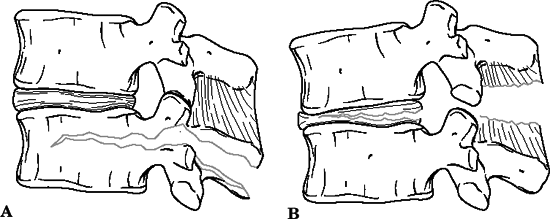
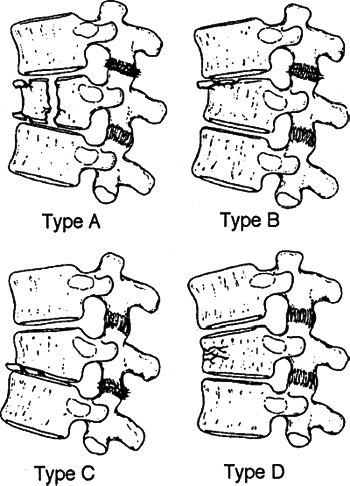
Figure 10.6. Compression fractures.
(From Browner BD, Jupiter JD, Levine MA, eds. Skeletal Trauma. Philadelphia: WB Saunders, 1992:746.)
|
-
Compression fractures (48%)
-
Burst fractures (14%)
-
Fracture-dislocations (16%)
-
Seat belt–type injuries (5%)
-
Compression fractures
-
These can be anterior (89%) or lateral (11%).
-
They are rarely associated with neurologic compromise.
-
They are generally stable injuries,
although they are considered unstable if associated with loss of
>50% vertebral body height, angulation >20 to 30 degrees, or
multiple adjacent compression fractures. -
The middle column remains intact; it may
act as a hinge with a posterior column distraction injury (seen with
compression in 40% to 50%). -
Four subtypes are described based on endplate involvement (Fig. 10.6):
Type A: Fracture of both endplates (16%) Type B: Fracture of superior endplate (62%) Type C: Fracture of inferior endplate (6%) Type D: Both endplates intact (15%) -
Treatment includes an extension orthosis
(Jewett brace or thoracolumbar spinal orthosis) with early ambulation
for most fractures, which are stable. Unstable fractures (>50%
height loss or 20 to 30 degrees of kyphosis in nonosteoporotic
P.110
bone
strongly suggests the possibility of posterior ligament complex
disruption, which places the patient at risk of increasing kyphotic
deformity or neurologic deficit) may require hyperextension casting or
open reduction and internal fixation. Upper thoracic fractures are not
amenable to casting or bracing and require surgical management to
prevent significant kyphosis.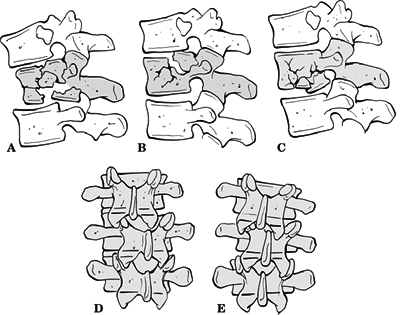 Figure
Figure
10.7. (A–E) Denis classification of burst fractures. Type A involves
fractures of both endplates, type B involves fractures of the superior
endplate, and type C involves fractures of the inferior endplate. Type
D is a combination of a type A fracture with rotation. Type E fractures
exhibit lateral translation.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
-
-
Burst fractures
-
No direct relationship exists between the percentage of canal compromise and the degree of neurologic injury.
-
The mechanism is compression failure of the anterior and middle columns under an axial load.
-
An association between lumbar burst fractures, longitudinal laminar fractures, and neurologic injury.
-
These injuries result in loss of posterior vertebral body height and splaying of pedicles on radiographic evaluation.
-
Five types are recognized (Fig. 10.7):
Type A: Fracture of both endplates (24%) Type B: Fracture of the superior endplate (49%) Type C: Fracture of inferior endplate (7%) Type D: Burst rotation (15%) Type E: Burst lateral flexion (5%) -
Treatment may consist of hyperextension casting if no neurologic compromise exists and the fracture pattern is stable (see compression fractures, earlier).
-
Early stabilization is advocated to restore sagittal and coronal plane alignment in cases with:
-
Neurologic deficits.
-
Loss of vertebral body height >50%.
-
Angulation >20 to 30 degrees.
-
Canal compromise of >50%.
-
Scoliosis >10 degrees.
-
-
Anterior, posterior, and combined approaches have been used.
-
Posterior surgery relies on indirect
decompression via ligamentotaxis and avoids the morbidity of anterior
exposure in patients who have concomitant pulmonary or abdominal
injuries; it also has shorter operative times and decreased blood loss.
Anterior approaches allow for direct decompression. Posterior
instrumentation alone cannot directly reconstitute anterior column
support and is therefore somewhat weaker in compression than anterior
instrumentation. This has lead to a higher incidence of progressive
kyphosis and instrumentation failure when treating highly comminuted
fractures. -
Instrumentation should provide distraction and extension moments.
-
Harrington rods tend to produce kyphosis and are thus contraindicated for use in the lower lumbar spine.
-
Laminectomies should not be done without instrument stabilization.
P.111 -
-
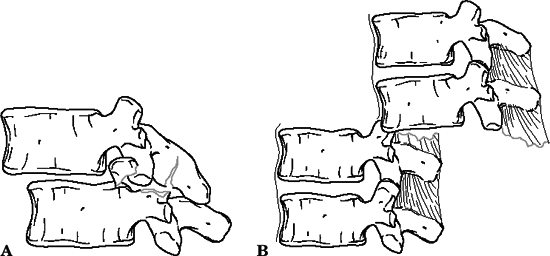
Flexion-distraction injuries (Chance fractures, seat belt–type injuries).
-
Patients are usually neurologically intact.
-
Up to 50% may have associated abdominal injuries.
-
Flexion-distraction injury results in
compression failure of the anterior column and tension failure of the
posterior and middle columns. -
Injuries rarely occur through bone alone and are most commonly the result of osseous and ligamentous failure. (Fig. 10.8).
-
One may see increased interspinous distance on the AP and lateral views.
-
Four types are recognized:
Type A: One-level bony injury (47%) Type B: One-level ligamentous injury (11%) Type C: Two-level injury through bony middle column (26%) Type D: Two-level injury through ligamentous middle column (16%) -
Treatment consists of hyperextension casting for type A injuries.
-
For injuries with compromise of the
middle and posterior columns with ligamentous disruption (types B,C,D),
posterior spinal fusion with compression should be performed. -
The primary goal of surgery for
flexion-distraction injuries is not to reverse neurologic deficit, but
to restore alignment and stability to enable early patient mobilization
and to prevent secondary displacement. -
Unless a herniated disc is noted on a
preoperative MRI and warrants anterior discectomy, posterior reduction
and compressive stabilization of the involved segment are usually
adequate.![]() Figure
Figure
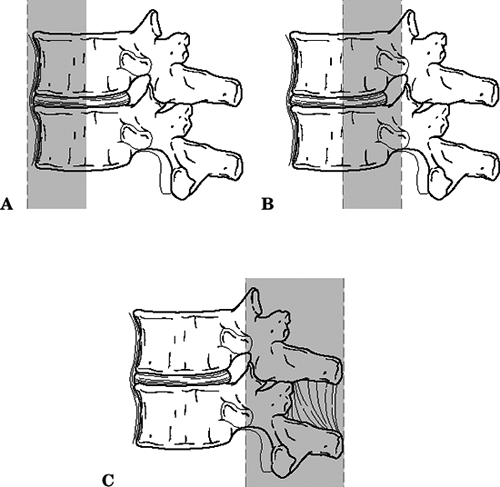
10.8. Flexion-distraction injuries. The bony Chance fracture (A) is
often associated with lap seat-belt use. This fracture was originally
described by Bohler years before Chance. A flexiondistraction injury
can occur entirely through soft tissue (B).(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
P.112 -
-
Fracture dislocations
-
All three columns fail under compression, tension, rotation, or shear, with translational deformity.
-
Three types, with different mechanisms (Denis), are known, as follows:
Type A: Flexion-rotation: posterior
and middle column fail in tension and rotation; anterior column fails
in compression and rotation; 75% with neurologic deficits, 52% of these
being complete lesions (Fig. 10.9)Type B: Shear: shear failure of all
three columns, most commonly in the posteroanterior direction; all
cases with complete neurologic deficit (Fig. 10.10)Type C: Flexion-distraction: tension
failure of posterior and middle columns, with anterior tear of annulus
fibrosus and stripping of the anterior longitudinal ligament; 75% with
neurologic deficits (all incomplete) (Fig. 10.11)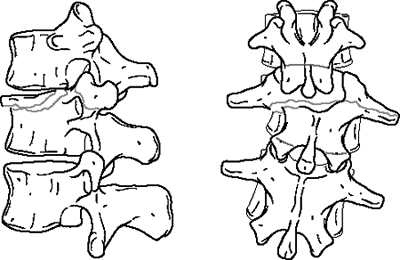 Figure 10.9. A flexion-rotation type of fracture-dislocation.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
Figure 10.9. A flexion-rotation type of fracture-dislocation.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)![]() Figure
Figure
10.10. A posteroanterior (A) shear-type fracture-dislocation. An
anteroposterior (B) shear-type fracture-dislocation. This nomenclature
is based on the direction of the shear force that would produce the
injury when applied to the superior vertebra.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.) -
Generally, these are highly unstable injuries that require surgical stabilization.
-
Posterior surgery is usually most useful for achieving reduction and stability in these injuries.
-
The characteristic deformity of
fracture-dislocations is translational malalignment of the involved
vertebrae. Realigning the spine is often difficult and is best
performed by direct manipulation of the vertebra with bone clamps or
elevators. Gradual distraction may be needed to reduce dislocations
with no associated fracture. -
Patients whose fractures are stabilized
within 3 days of injury have a lower incidence of pneumonia and a
shorter hospital stay than those with fractures stabilized more than 3
days after injury. -
Patients without neurologic deficit do
not typically need urgent surgery. Surgery can be performed when the
patient has been adequately stabilized medically. A similar approach
P.114
should be employed in patients that have complete neurologic injuries when there is little chance for significant recovery.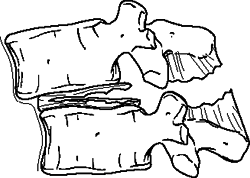 Figure 10.11. A flexiondistraction type of dislocation.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
Figure 10.11. A flexiondistraction type of dislocation.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
P.113 -
physiologic loads cause further neurologic damage, chronic pain, and
unacceptable deformity.
|
Table 10.1. Thoracic and thoracolumbar spine stability scale
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||
|
Table 10.2. Lumbar spine stability scale
|
|||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||
|
Table 10.3. Basic types of spinal fractures and columns involved in each
|
|||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||
-
Anterior column: anterior longitudinal ligament, anterior half of the vertebral body, and anterior annulus
-
Middle column: posterior half of vertebral body, posterior annulus, and posterior longitudinal ligament
-
Posterior column: posterior neural arches
(pedicles, facets, and laminae, and posterior ligamentous complex
(supraspinous ligament, interspinous ligament, ligamentum flavum, and
facet capsules)
-
Instability exists with disruption of any two of the three columns
-
Thoracolumbar stability usually follows the middle column: if it is intact, then the injury is usually stable.
-
First degree (mechanical instability): potential for late kyphosis
-
Severe compression fractures
-
Seat belt–type injuries
-
-
Second degree (neurologic instability): potential for late neurologic injury
-
Burst fractures without neurologic deficit
-
-
Third degree (mechanical and neurologic instability)
-
Fracture-dislocations
-
Severe burst fractures with neurologic deficit
-
with early progression of neurologic deficits and spinal deformity as
well as late onset of neurologic deficits and mechanical back pain.
-
Factors indicative of instability in burst fractures:
-
>50% canal compromise
-
>15 to 25 degrees of kyphosis
-
>40% loss of anterior body height
-
-
In general, fractures associated with
low-velocity gunshot wounds are stable fractures. This is the case with
most handgun injuries. They are associated with a low infection rate
and can
P.116
be
prophylactically treated with 48 hours of a broad-spectrum antibiotic.
Transintestinal gunshot wounds require special attention. In these
cases, the bullet passes through the colon, intestine, or stomach
before passing through the spine. These injuries carry a significantly
higher rate of infection. Broad-spectrum antibiotics should be
continued for 7 to 14 days. High-energy wounds, as caused by a rifle or
military assault weapon, require open debridement and stabilization.![]() Figure
Figure
10.12. The three columns of the spine, as proposed by Francis Denis.
The anterior column (A) consists of the anterior longitudinal ligament,
anterior part of the vertebral body, and the anterior portion of the
annulus fibrosis. The middle column (B) consists of the posterior
longitudinal ligament, posterior part of the vertebral body, and
posterior portion of the annulus. The posterior column (C) consists of
the bony and ligamentous posterior elements.(Modified from Denis F. The three-column spine and its significance in the classification of acute thoracolumbar spine injuries. Spine 1983;8:817–831.) -
Neural injury is often secondary to a
blast effect in which the energy of the bullet is absorbed and
transmitted to the soft tissues. Because of this unique mechanism,
decompression is rarely indicated. One exception is when a bullet
fragment is found in the spinal canal between the level of T12 and L5
in the presence of a neurologic deficit. Rarely, delayed bullet
extraction may be indicated for lead toxicity or late neurologic
deficits owing to migration of a bullet fragment. Steroids after
gunshot wounds to the spine are not recommended, because they have
demonstrated no neurologic benefit and appear to be associated with a
higher rate of nonspinal complications.
-
These authors modified the Frankel
grading system of neurologic injury for thoracolumbar injuries,
dividing Frankel D types (impaired but functional motor function) based
on degree of motor function as well as bowel and bladder function:Type A: Complete motor and sensory loss Type B: Preserved sensation, no voluntary motor Type C: Preserved motor, nonfunctional Type D1: Low-functional motor (3+/5+) and/or bowel or bladder paralysis Type D2: Midfunctional motor (3+ to 4+/5+) and/or neurogenic bowel or bladder dysfunction Type D3: High-functional motor (4+/5+) and normal voluntary bowel or bladder function Type E: Complete motor and sensory function normal -
In patients with thoracolumbar spine
fractures and incomplete neurologic injuries, greater neurologic
improvement (including return of sphincter control) was found in
patients treated by anterior spinal decompression versus posterior or
lateral spinal decompression.
-
They prospectively examined neurologic
injury and recovery patterns for T12-L1 burst fractures with partial
paralysis and >30% initial canal compromise. -
Conclusions
-
Severity of neurologic injury did not correlate with fracture pattern or amount of CT measured canal compromise.
-
Neurologic recovery did not correlate with the treatment method or amount of canal decompression.
-
Neurologic recovery did correlate with the initial fracture pattern (four types):
Type I: <15 degrees of kyphosis; maximal canal compromise at level of ligamentum flavum Type II: <15 degrees of kyphosis; maximal compromise at the bony posterior arch Type III: >15 degrees of kyphosis; maximal compromise at the bony arch Type IV: >15 degrees of kyphosis; maximal compromise at the level of the ligamentum flavum
-
-
Type I or Type II: Significant neurologic
recovery occurred in >90%, regardless of the severity of the initial
paralysis or treatment method. -
Type III: Significant neurologic recovery occurred in <50%.
-
Type IV: The response was variable.
-
They associated dural tears in 37% of burst fractures with associated laminar fractures; all patients had neurologic deficits.
-
They concluded that the presence of a
preoperative neurologic deficit in a patient who had a burst fracture
and an associated laminar fracture was a sensitive (100%) and specific
(74%) predictor of dural laceration, as well as a predictor of risk for
associated entrapment of neural elements.
-
They reported an 8% incidence of dural tears in all surgically treated spine fractures, 25% in lumbar burst fractures.
-
In patients with burst fractures and a
dural tear, 86% had neurologic deficits versus 42% in those with burst
fractures without a dural tear.