The Wrist and Hand
 |
|
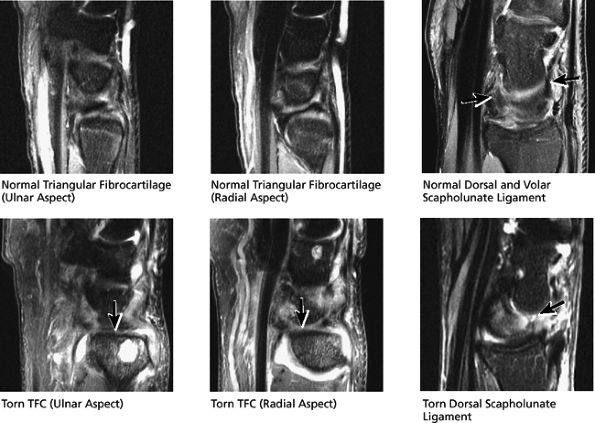
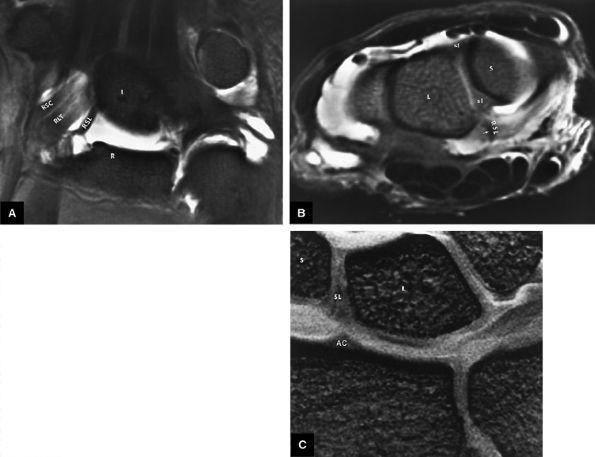
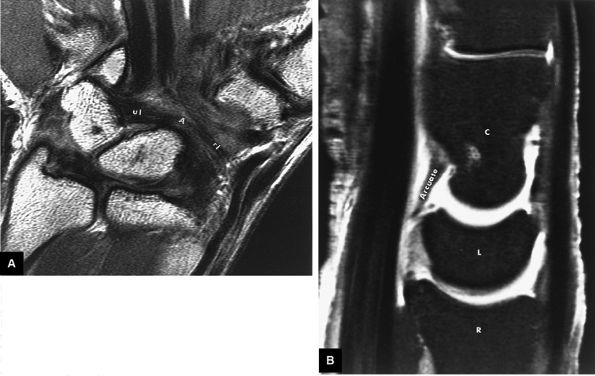
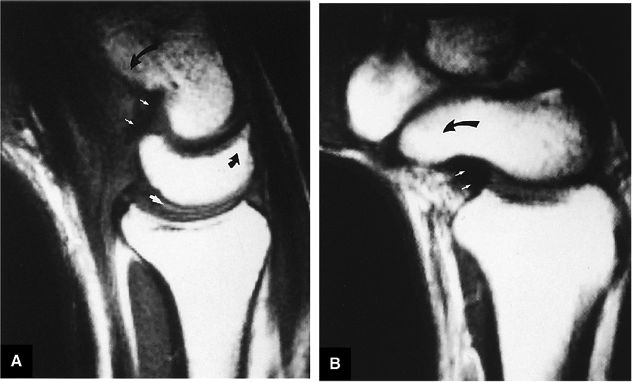
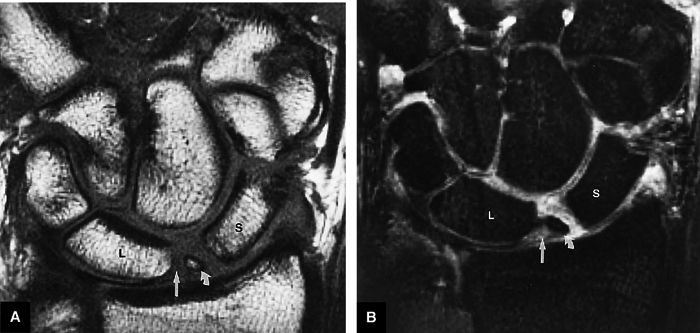
FIGURE 10.1 ● A 3D fast spoiled GRASS (FSPGR) with intra-articular contrast injected into the radiocarpal compartment. The torn lunotriquetral ligament (straight arrow) allows extension of contrast into the midcarpal compartment and the torn radial attachment of the TFC (curved arrow) directs contrast into the distal radioulnar joint. Note the superior trabecular bone detail on this image (coronal image; TR, 40.4 msec; TE, 14.5 msec; FOV, 4 cm; slice thickness, 2.0 mm; matrix, 512 × 256; flip angle, 30°).
|
 |
|
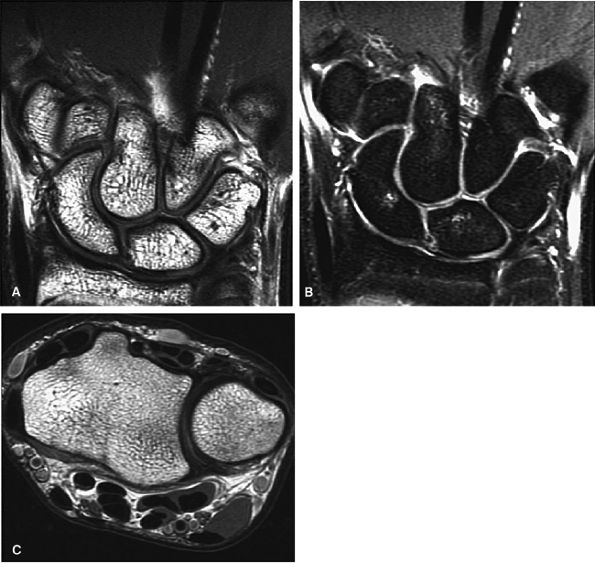
FIGURE 10.2 ● Optimized signal-to-noise in routine wrist imaging using a four-channel phased-array wrist coil on a 3T imager. (A) Coronal PD FSE image. (B) Coronal FS PD FSE image. (C) Axial PD FSE image.
|
coil design, the patient's arm may be positioned at his or her side. Anatomic symmetry of both extremities can be demonstrated in the same FOV by placing both hands in a large-diameter coil. When high-spatial-resolution images requiring smaller FOVs are necessary for the opposite wrist or hand, separate acquisitions can be performed in the area of suspected pathology and a comparison of normal and abnormal anatomy can be made. Proper positioning requires alignment of the long axis of the distal radius and central metacarpal axis with the wrist in neutral position. Oblique prescriptions are not required to produce orthogonal images with this colinear alignment of the distal radius and carpus. Radial or ulnar deviation and dorsal or volar angulation should be avoided to maintain consistent alignment of the carpus. The wrist is usually positioned in pronation, with the fingers held in extension. The position of the wrist may change relative to the design of the surface coil used. When the wrist is studied in the thumbs-up position, coronal images are obtained by prescribing a sagittal plane acquisition. In this case, oblique imaging may be required to produce orthogonal plane images through the plane of the TFC and intrinsic ligaments of the wrist.
-
MR or MR arthrography has replaced conventional single- or three-compartment arthrograms.
-
Dedicated four- or eight-channel phased-array coils are required for wrist and finger imaging.
-
Although TFC degeneration is best demonstrated on T2* gradient-echo images, FS PD FSE sequences are more frequently used in routine examinations to provide improved contrast between hypointense intrinsic ligaments and hyperintense fluid.
-
T1- and PD-weighted images are obtained in the axial, coronal, and sagittal planes. Coronal images are acquired with 2- to 2.5-mm sections, using a 6-cm FOV and a 512 × 256 or 256 × 256 matrix.
-
Pathology of the TFC and intrinsic ligaments is displayed on FS PD FSE coronal images, which create an arthrography-like effect by displaying the hyperintensity of fluid in contrast to the lower signal intensity of ligaments and fibrocartilage. The sequence may also be used in the axial and sagittal planes.
-
FS PD FSE sequences use a repetition time (TR) of 3,000 msec, an echo time (TE) between 40 and 60 msec, an 8-cm FOV, a 2- to 3-mm slice thickness, and a 256 × 256 matrix interpolated to 512. Higher matrix and TE values and lower echo train lengths produce images with less blurring.
-
T2*-weighted coronal images also produce excellent contrast between ligaments (the intercarpal ligaments and the TFC complex) and fluid. In fact, intrasubstance TFC degeneration is best demonstrated using T2* gradient-echo techniques, even though the intrinsic ligaments are better visualized on FS PD FSE images.
-
3D SPGR techniques are used to display detailed anatomy of the TFC complex and intrinsic ligaments. Using these sequences, it is possible to achieve higher-resolution MR images with a FOV between 4 and 6 cm and a lower receiver band, ± 8 kHz. Pixel resolution at a 4-cm FOV and 256 × 256 matrix is approximately 100 μm, which allows visualization of trabecular bone detail as well. FS is recommended, however, to increase the conspicuity of fluid in abnormal or injured articular cartilage.
and tilting of the lunate or the degree of scaphoid flexion or extension. The anteroposterior location of TFC tears is determined on FS PD FSE sagittal images. Fluid in the dorsal or volar ligaments of the capsule is also shown in this plane.
 |
|
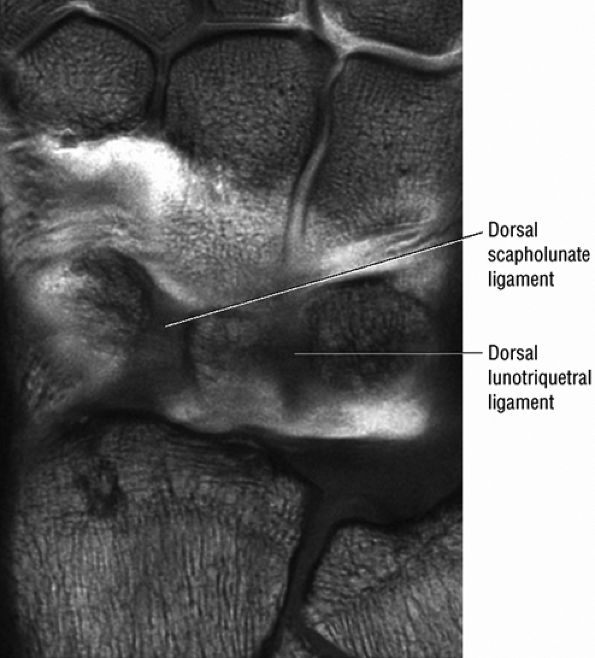
FIGURE 10.3 ● Identification of the dorsal fibers of the scapholunate and lunotriquetral ligaments on a coronal T1-weighted arthrogram. Although MR arthrography is frequently performed with FS, this decreases signal-to-noise. Routine FS PD FSE sequences are still used when performing MR arthrography, usually in the coronal and axial planes, to evaluate muscle and tendon pathology, chondral abnormalities, subchondral marrow edema, and noncommunicating ganglions. Postarthrogram sequences limited to FS T1-weighted sequences alone are inadequate for comprehensive diagnostic assessment.
|
 |
|
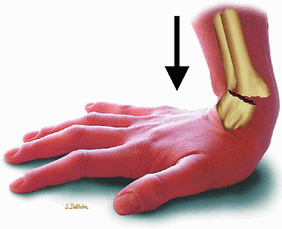
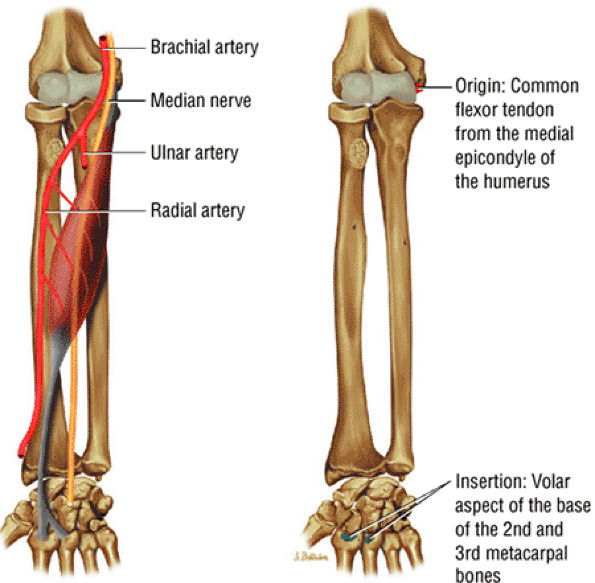
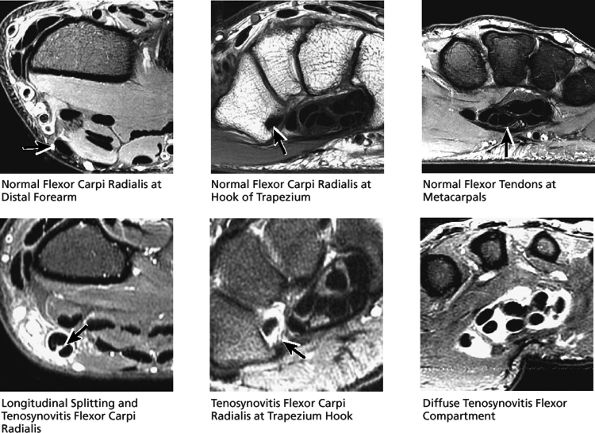
FIGURE 10.4 ● FLEXOR CARPI RADIALIS The flexor carpi radialis lies radial to the palmaris longus and ulnar to the pronator teres throughout its course. It contributes to flexion and abduction of the wrist. Distal flexor carpi radialis tendon rupture, usually occurring after a fall on the outstretched hand, can clinically mimic a scaphoid fracture.
|
 |
|
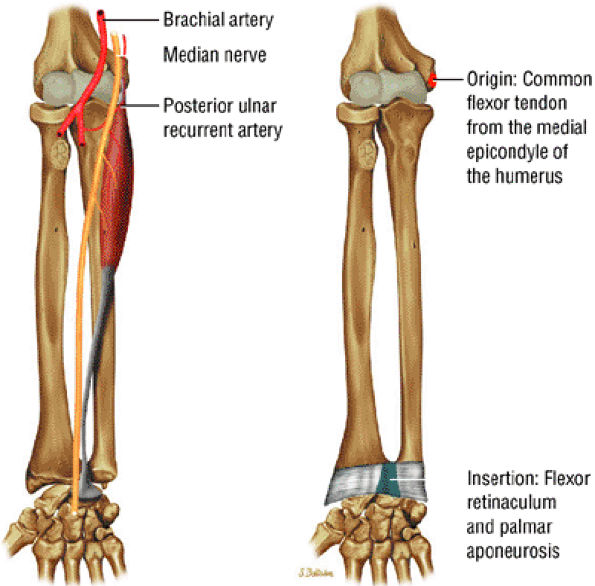
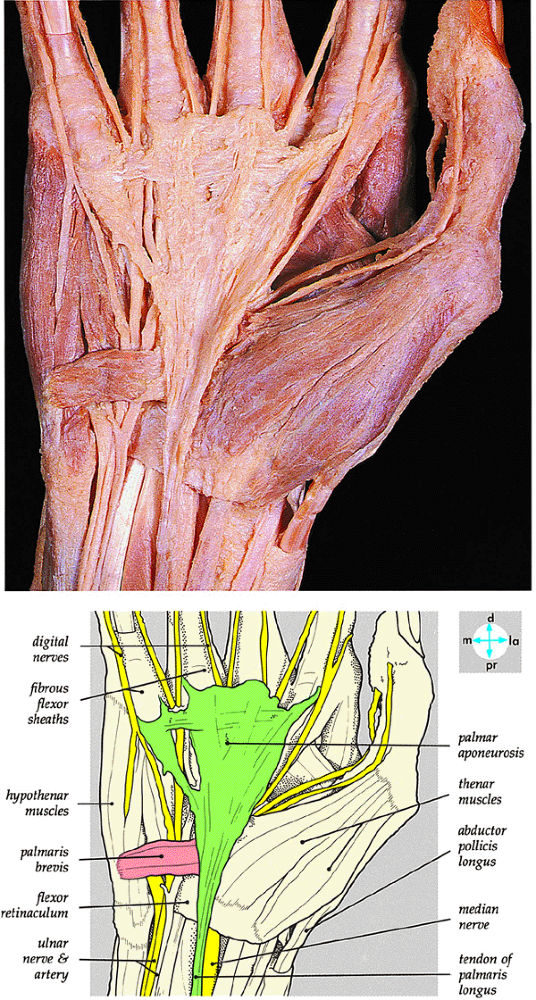
FIGURE 10.5 ● PALMARIS LONGUS The palmaris longus is present in approximately 85% of the population and functions to flex the wrist and tighten the palmar aponeurosis. It does not have a tendon sheath but has a paratenon.
|
 |
|
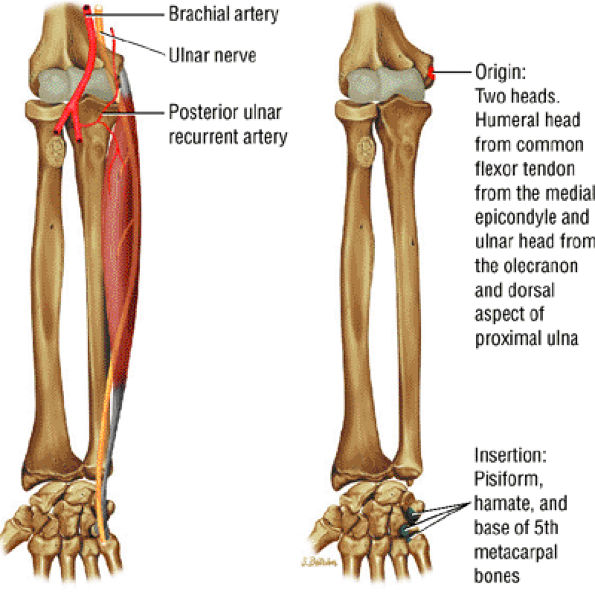
FIGURE 10.6 ● FLEXOR CARPI ULNARIS The flexor carpi ulnaris flexes and adducts the hand. It is an important dynamic stabilizer of the pisotriquetral joint and contributes superficial fibers to the pisohamate ligament. Since it lies superficial and just medial to the ulnar nerve, it serves as a marker when ulnar nerve block is performed.
|
 |
|
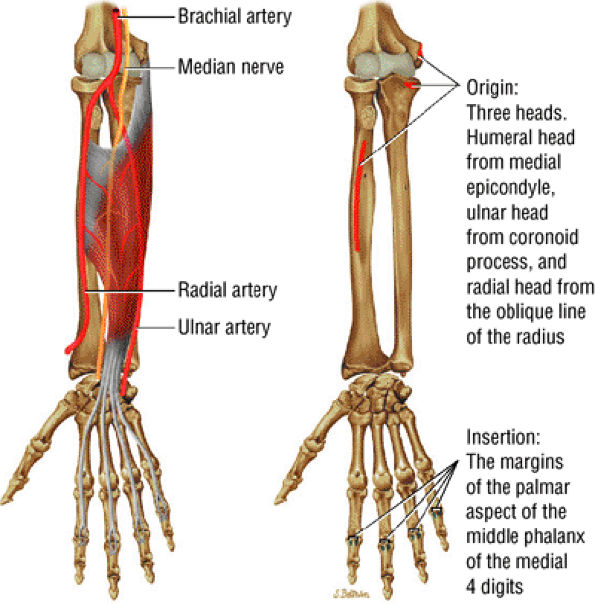
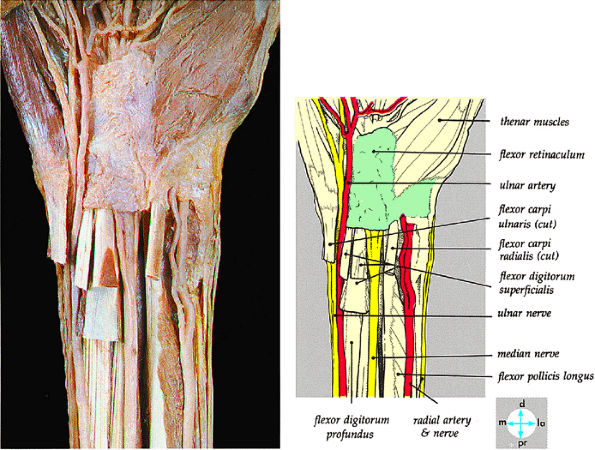
FIGURE 10.7 ● FLEXOR DIGITORUM SUPERFICIALIS The flexor digitorum superficialis tendons flex the middle phalanges of each finger and, using the pulley system as a fulcrum, contribute to flexion of the fingers at the metacarpophalangeal joint. The deep fibers of the flexor digitorum superficialis origin are closely apposed with the anterior bundle of the ulnar collateral ligament at the elbow, which is why edema and hemorrhage in the flexor digitorum superficialis are commonly seen in the setting of ulnar collateral ligament tears. In the forearm, the median nerve lies just deep to the arch of the flexor digitorum superficialis muscle, and this is an area of potential nerve compression. The flexor digitorum superficialis divides into four musculotendinous units in the distal forearm, and the tendons travel though the carpal tunnel before dividing again at the level of the proximal phalanges.
|
 |
|
FIGURE 10.8 ● FLEXOR DIGITORUM PROFUNDUS The flexor digitorum profundus tendons flex the distal phalanges at the distal interphalangeal joints and assist in flexion of the wrist and proximal phalanges. The flexor digitorum profundus divides into four musculotendinous units in the distal forearm, and the tendons travel though the carpal tunnel deep to the flexor digitorum superficialis tendons. Distal avulsions of a flexor digitorum profundus tendon, or jersey finger, can occur when an athlete gets a finger caught in an opposing player's jersey.
|
 |
|
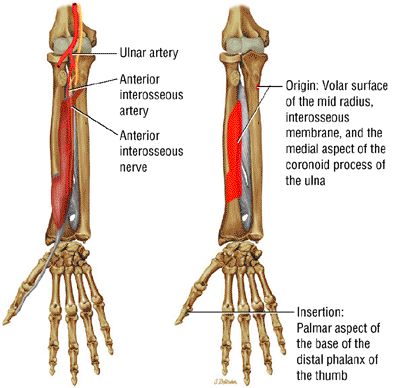
FIGURE 10.9 ● FLEXOR POLLICIS LONGUS The flexor pollicis longus flexes the thumb. Compression of the anterior interosseous nerve can lead to denervation of the flexor pollicis longus muscle, which may be isolated or concomitant with flexor digitorum profundus and pronator quadratus denervation.
|
 |
|
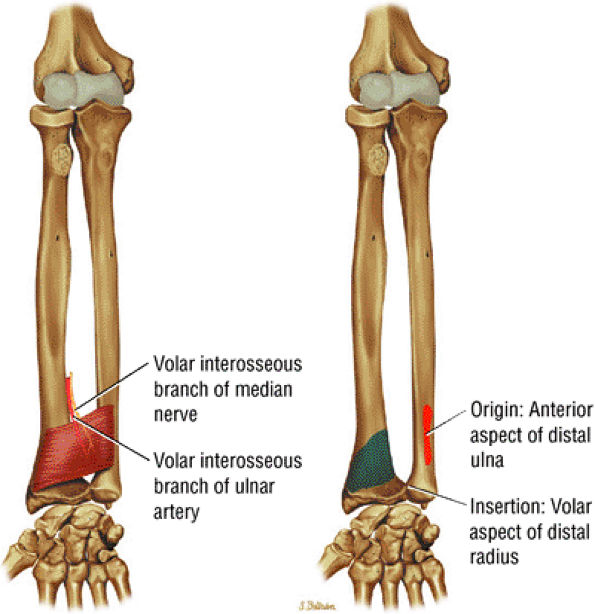
FIGURE 10.10 ● PRONATOR QUADRATUS The pronator quadratus acts synergistically with the pronator teres to pronate the forearm. Denervation changes can be seen with anterior interosseous nerve compression.
|
 |
|
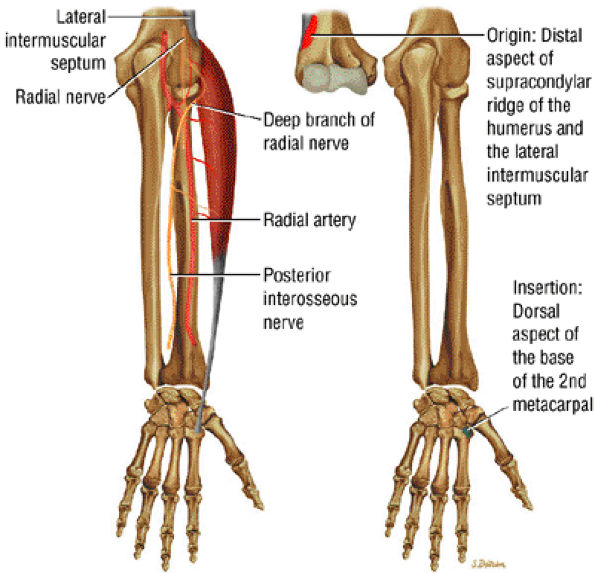
FIGURE 10.11 ● EXTENSOR CARPI RADIALIS LONGUS The extensor carpi radialis longus extends and abducts the wrist. If extensor carpi ulnaris function is lost due to posterior interosseus nerve palsy, the extensor carpi radialis causes radial deviation because normally the attachment of the extensor carpi ulnaris to the ulnar aspect of the fifth metacarpal functions to neutralize the abduction movement applied by the extensor carpi radialis longus.
|
 |
|
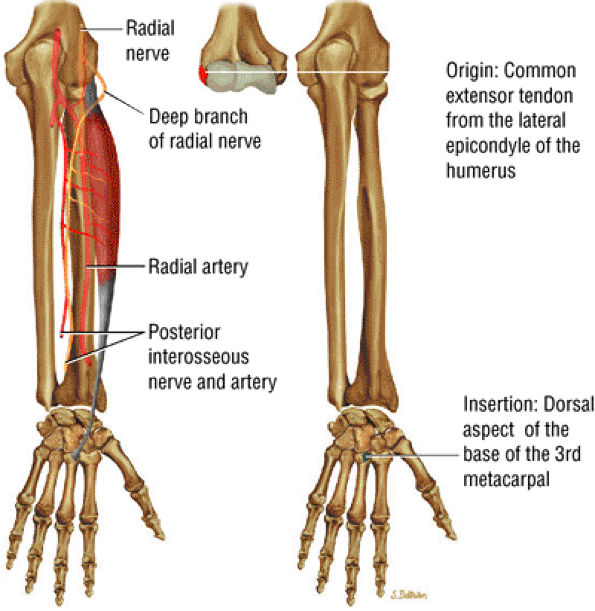
FIGURE 10.12 ● EXTENSOR CARPI RADIALIS BREVIS The extensor carpi radialis brevis provides neutral extension of the wrist. Distal ruptures of the extensor carpi radialis brevis significantly affect wrist extension.
|
 |
|
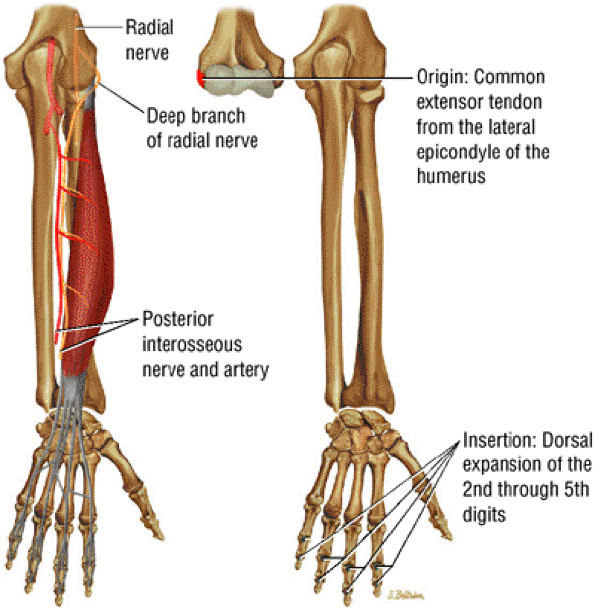
FIGURE 10.13 ● EXTENSOR DIGITORUM The extensor digitorum extends the medial four digits at the metacarpophalangeal joints and contributes to wrist extension. The extensor digitorum tendons are connected at the level of the metacarpal bones by fibrous bands called juncturae tendinum. Boutonnière deformity results from disruption of the central slip component of the extensor tendon at its insertion into the middle phalanx.
|
 |
|
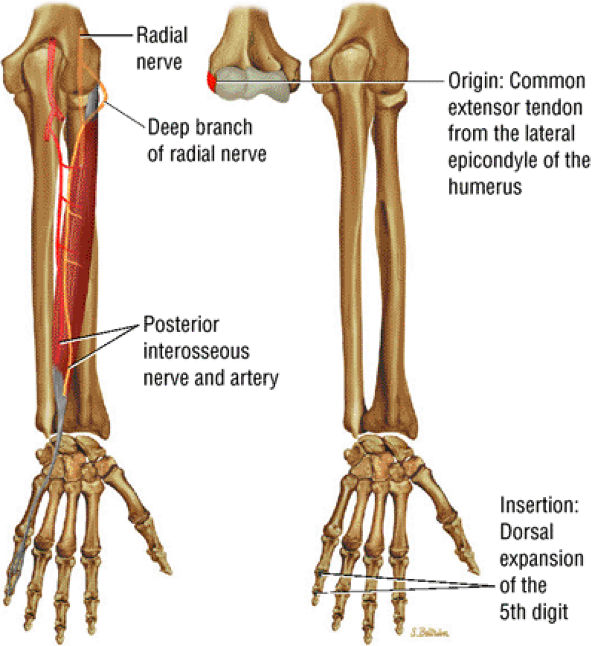
FIGURE 10.14 ● EXTENSOR DIGITI MINIMI The extensor digiti minimi extends the proximal phalanx of the little finger at the metacarpophalangeal joint and contributes to wrist extension. Because the extensor digiti minimi tendon lies just superficial to the radioulnar articulation, it is often the first tendon to be involved in rheumatoid arthritis.
|
 |
|
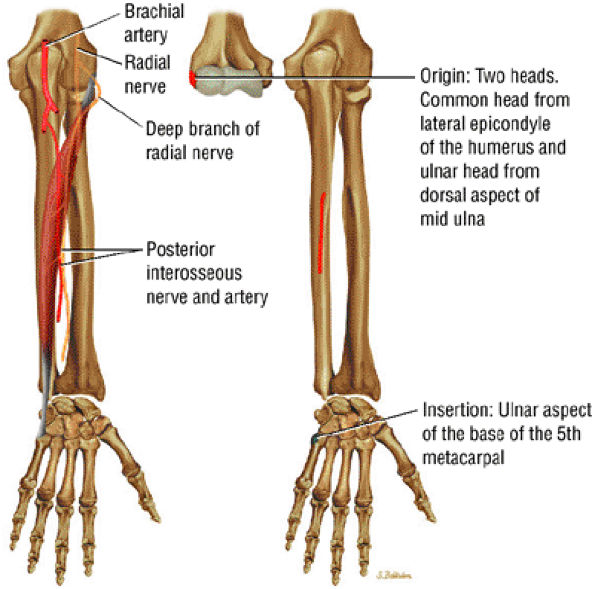
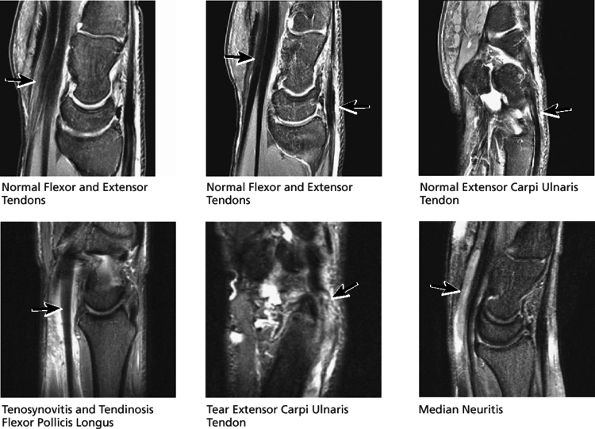
FIGURE 10.15 ● EXTENSOR CARPI ULNARIS The extensor carpi ulnaris tendon extends and adducts the wrist. It is commonly affected in tendinosis and tenosynovitis as it passes through the groove on the distal ulna. Subluxation of the extensor carpi ulnaris can also occur at this location related to disruption or insufficiency of the ligament that covers the tendon in this groove. The extensor carpi ulnaris tendon subsheath is a component of the triangular fibrocartilage complex.
|
 |
|
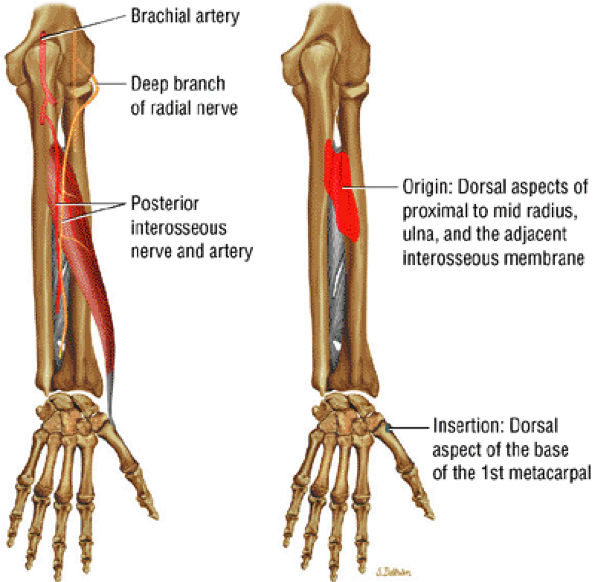
FIGURE 10.16 ● ABDUCTOR POLLICIS LONGUS The abductor pollicis longus abducts and extends the thumb at the carpometacarpal joint. It travels in the first extensor compartment of the wrist with the extensor pollicis brevis and may become involved with a stenosing tenosynovitis located under the extensor retinaculum at the distal radial groove. This condition, known as de Quervain's tenosynovitis, is distinguished from intersection syndrome, which is a result of friction-related repetitive trauma to the second extensor compartment tendons (at the point where the abductor pollicis longus and the extensor pollicis brevis muscle bodies cross). Intersection syndrome occurs proximal to the extensor retinaculum.
|
 |
|
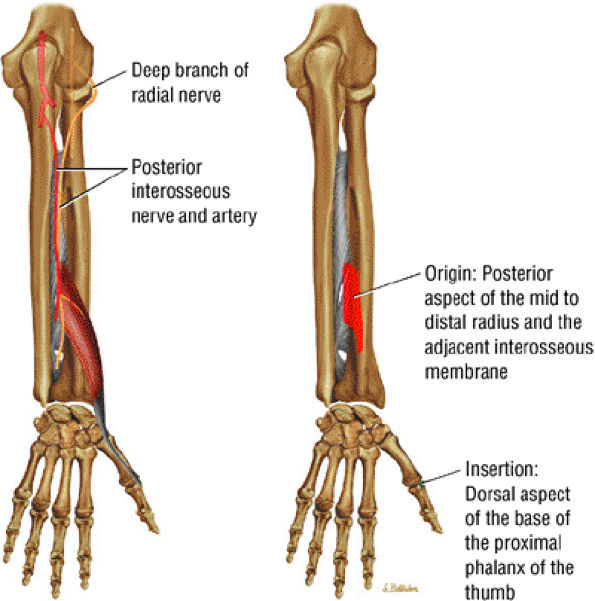
FIGURE 10.17 ● EXTENSOR POLLICIS BREVIS The extensor pollicis brevis travels with the abductor pollicis longus in the first extensor compartment and forms the lateral margin of the anatomic snuffbox. It is usually affected concomitantly with the abductor pollicis longus in de Quervain's tenosynovitis. The extensor pollicis brevis extends from the proximal phalanx of the thumb at the carpometacarpal joint.
|
 |
|
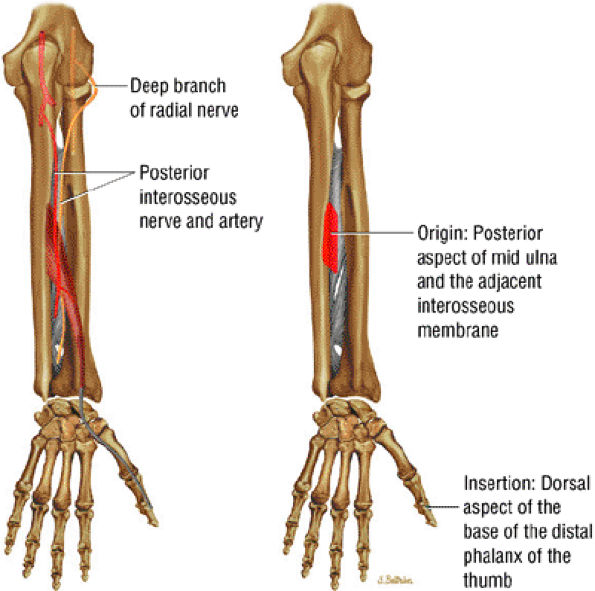
FIGURE 10.18 ● EXTENSOR POLLICIS LONGUS The extensor pollicis longus tendon has a separate tendon sheath throughout its course. It can be injured in Colles' fractures of the distal radius and is sometimes involved in delayed injury following conservative treatment of nondisplaced fractures. This delayed injury is thought to be related to ischemia secondary to edema or hemorrhage compromising the fibro-osseous canal. The extensor pollicis longus extends the distal phalanx of the thumb at the carpometacarpal and interphalangeal joints.
|
 |
|
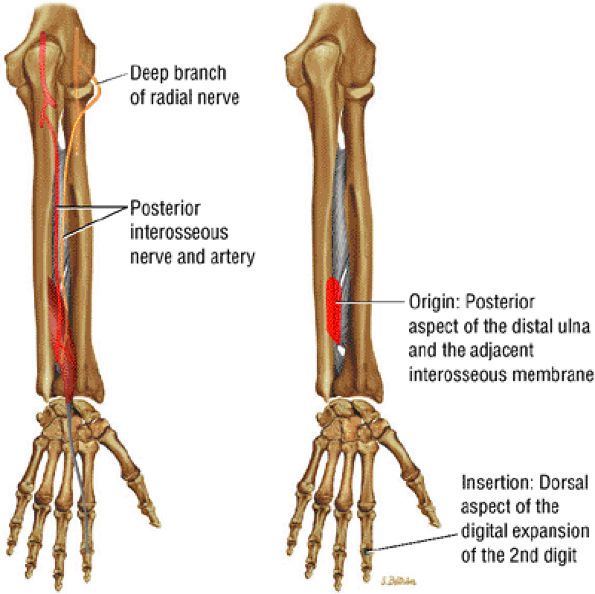
FIGURE 10.19 ● EXTENSOR INDICIS The extensor indicis, the only extensor that has muscle fibers that extend to or beyond the level of the radiocarpal joint, extends the second finger and contributes to wrist extension. The extensor indicis is sometimes transferred surgically to replace a torn extensor pollicis longus tendon.
|
 |
|
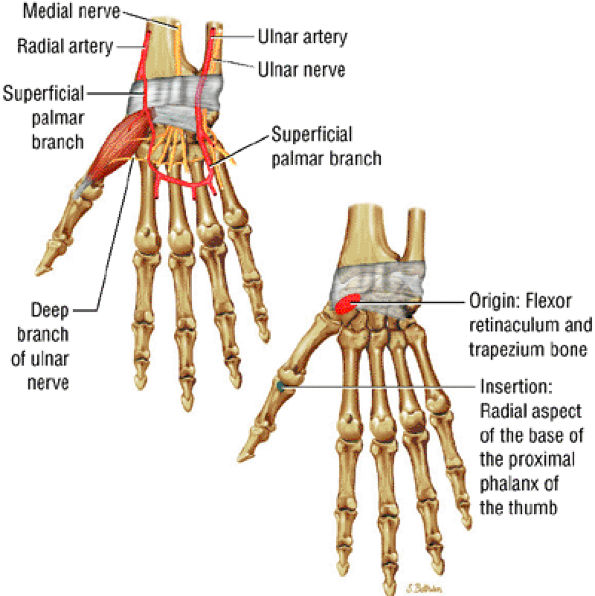
FIGURE 10.20 ● ABDUCTOR POLLICIS BREVIS The abductor pollicis brevis acts in conjunction with the opponens pollicis longus to abduct the thumb. It contracts during the early stages of thumb opposition and in the process also acts to rotate the phalanx. In longstanding carpal tunnel syndrome, the abductor pollicis brevis as well as the other thenar muscles may atrophy because they are supplied by the median nerve.
|
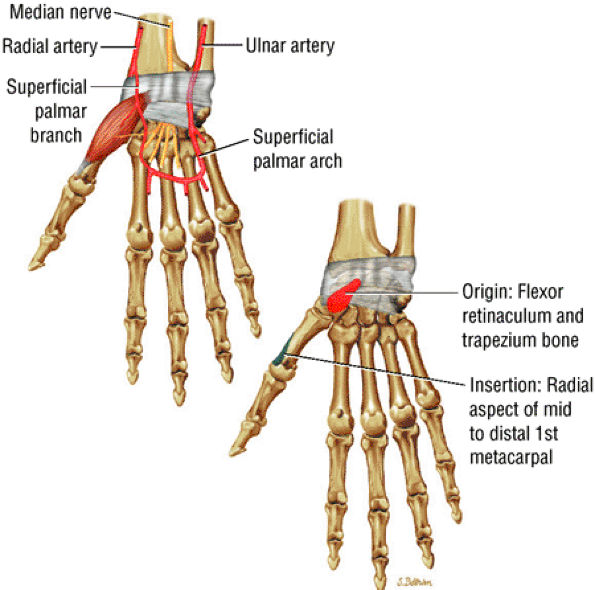 |
|
FIGURE 10.21 ● OPPONENS POLLICIS The opponens pollicis is part of the thenar eminence along with the abductor pollicis brevis and the flexor pollicis brevis. It acts to draw the first metacarpal laterally into a position that is favorable to opposition.
|
 |
|
FIGURE 10.22 ● FLEXOR POLLICIS BREVIS The flexor pollicis brevis passes along the radial side of the tendon of the flexor pollicis longus. It has two portions, lateral and medial. The lateral portion arises from the flexor retinaculum and the medial portion arises from the trapezium. It acts to flex the thumb at the metacarpophalangeal joint.
|
 |
|
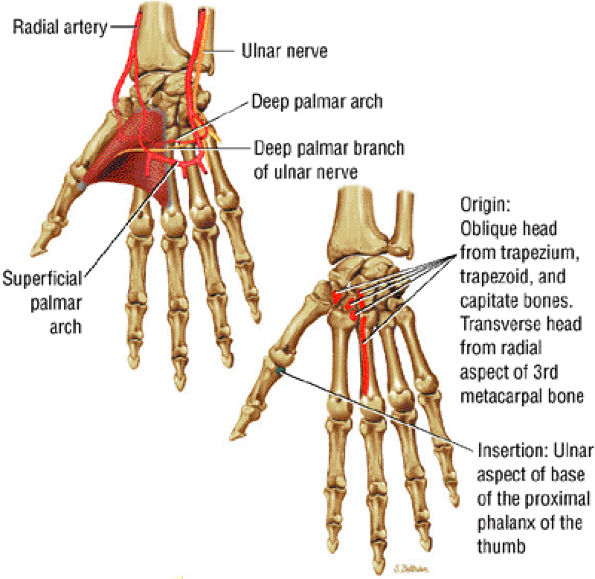
FIGURE 10.23 ● ADDUCTOR POLLICIS The adductor pollicis has two heads that converge into a tendon that inserts, along with fibers from the adjacent flexor pollicis brevis, onto the ulnar side of the base of the first phalanx of the thumb. There is a sesamoid bone present in the tendon. In tears of the ulnar collateral ligament of the thumb (gamekeeper's thumb), the adductor pollicis aponeurosis can interpose between the torn ulnar collateral ligament and the thumb, precluding healing (Stener's lesion). Stener's lesions must be surgically corrected to prevent persistent instability of the metacarpophalangeal joint.
|
 |
|
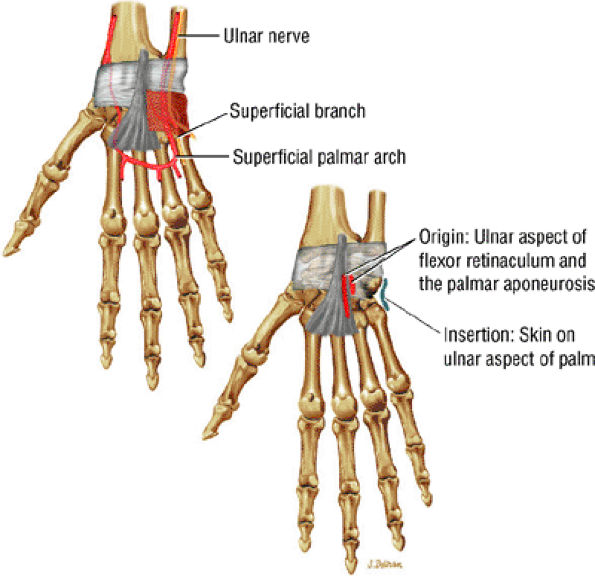
FIGURE 10.24 ● PALMARIS BREVIS The palmaris brevis is a thin superficial muscle that connects the flexor retinaculum to the ulnar skin. Rarely it is hyperactive, resulting in spasm.
|
 |
|
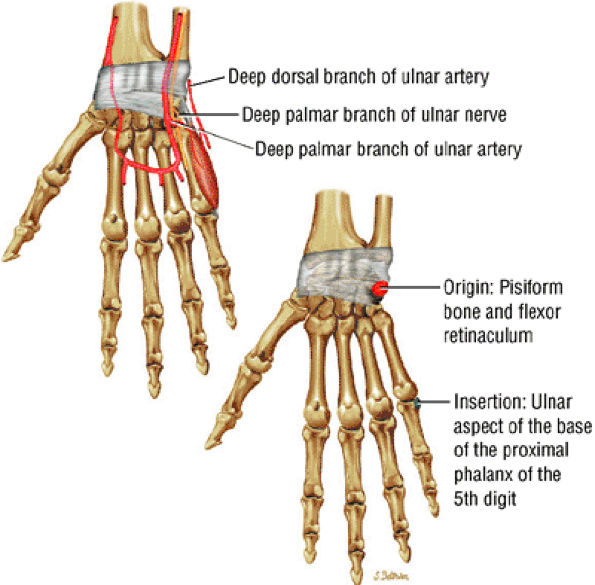
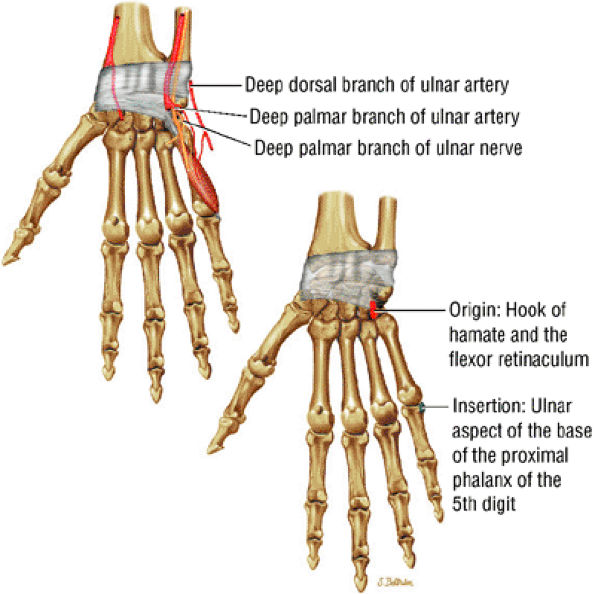
FIGURE 10.25 ● ABDUCTOR DIGITI MINIMI The abductor digiti minimi abducts the little finger and contributes to flexion of its proximal phalanx at the metacarpophalangeal joint. In connective tissue diseases such as rheumatoid arthritis, prolonged contraction of the abductor digiti minimi can occur, resulting in ulnar deviation that requires surgical release.
|
 |
|
FIGURE 10.26 ● FLEXOR DIGITI MINIMI The flexor digiti minimi brevis is part of the hypothenar eminence, along with the abductor digiti minimi and the opponens digiti minimi. It lies radial to the abductor digiti minimi and functions to flex the little finger at the metacarpophalangeal joint.
|
 |
|
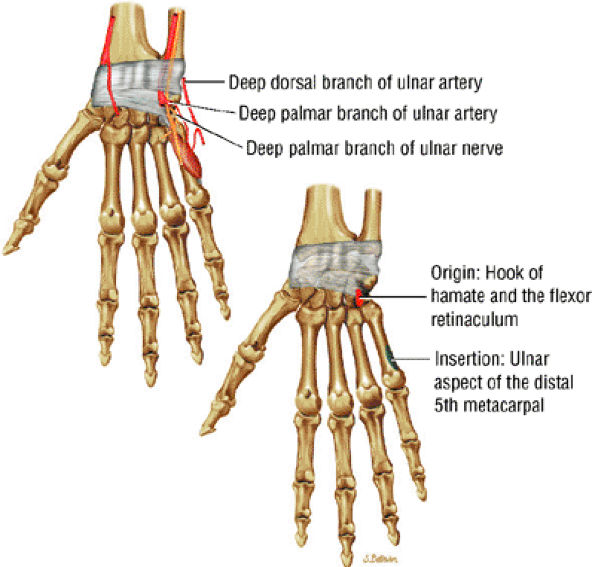
FIGURE 10.27 ● OPPONENS DIGITI MINIMI The opponens digiti minimi is the deep component of the hypothenar eminence. It stabilizes ulnar grip by rotating the fifth metacarpal and moves it anteriorly. In doing this, it brings the fifth finger into opposition with the thumb.
|
 |
|
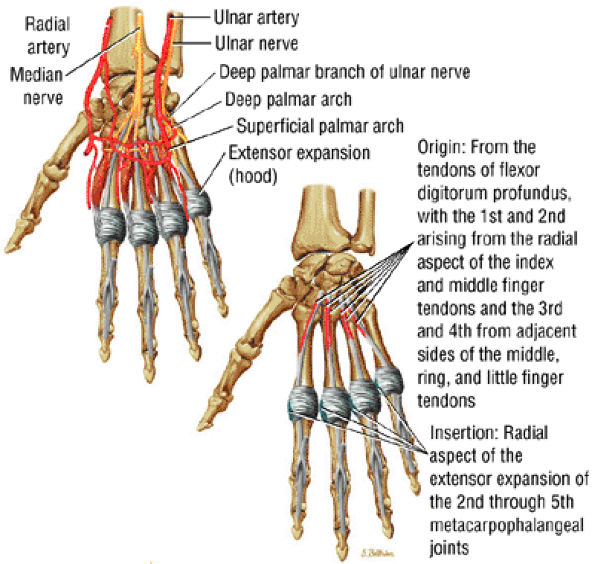
FIGURE 10.28 ● LUMBRICALS The lumbricals have no bony attachments. They originate from the tendons of the flexor digitorum profundus, and along with the interossei they merge to form part of the extensor expansion, which extends to the distal phalanx. They are important flexors of the metacarpophalangeal joints and also contribute to extension of the proximal and distal interphalangeal joints.
|
 |
|
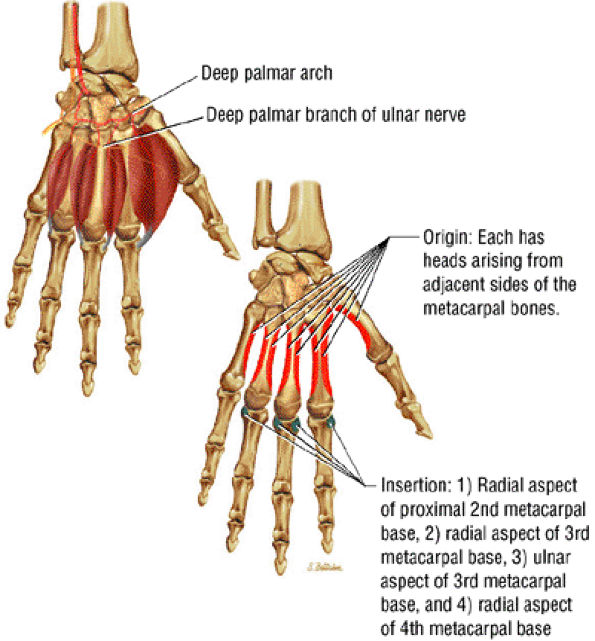
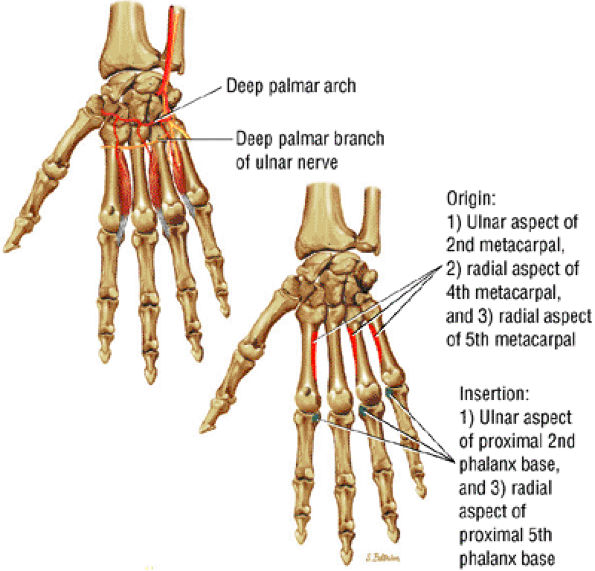
FIGURE 10.29 ● DORSAL INTEROSSEI The dorsal interossei occupy the intervals between the metacarpal bones. They abduct the second through fourth fingers from the axis of the middle finger and assist in flexing proximal phalanges of the second through fourth fingers at the metacarpophalangeal joints.
|
 |
|
FIGURE 10.30 ● PALMAR INTEROSSEI The palmar interossei adduct the second, fourth, and fifth fingers relative to the axis of the middle finger. They also flex the same fingers at the metacarpophalangeal joint while extending them at the interphalangeal joints.
|
-
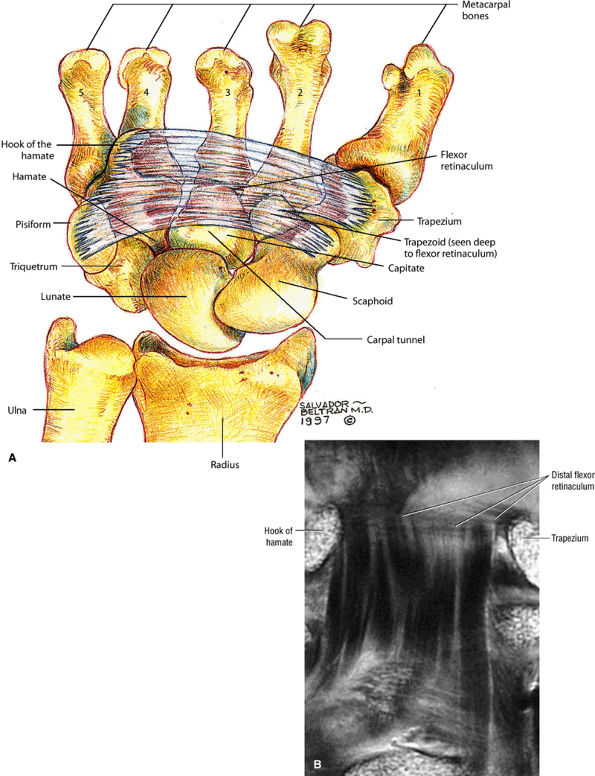
On volar images, the flexor retinaculum is seen superficial to the flexor tendons as a transverse band.
-
En face, the hypointense bands of the flexor digitorum tendons are seen passing through the carpal tunnel between the hook of the hamate and the trapezium.
-
The intermediate-signal-intensity median nerve may also be discerned in this plane of section.
-
The pisohamate and pisometacarpal ligaments are shown in sections at the level of the hook of the hamate and pisiform.
-
The abductor pollicis longus and extensor pollicis brevis tendons border the volar radial aspect of the wrist in sections through the volar surfaces of the scaphoid and lunate.
-
The TFC is seen as a curvilinear bowtie band of hypointense, homogeneous signal intensity. The band extends horizontally to the base of the ulnar styloid process from the ulnar surface of the distal radius.
-
The meniscal homologue demonstrates intermediate signal intensity on T1- and T2*-weighted images.
-
The radioscaphocapitate ligament and the radiolunotriquetral ligament, also sometimes referred to as the long radiolunate ligament, are visualized volarly and extend from the radial styloid in an ulnar-distal direction. These fibers are seen as parallel bands of striations. The more ulnarly located radioscapholunate ligament is usually seen in the same plane as the radioscaphocapitate and radiolunotriquetral ligaments and is a less substantial structure compared with the other volar extrinsic carpal ligaments. The proximal portion of the radiolunotriquetral ligament is represented by obliquely directed fibers extending from the volar radius to the lunate, volar to the proximal pole of the scaphoid.
-
The distal radioulnar joint and compartment are separated from the radiocarpal compartment by the TFC.
-
The scapholunate and lunotriquetral interosseous ligaments are routinely visualized on 3-mm coronal T1- and T2*-weighted images.
-
The extensor carpi ulnaris tendon borders the ulnar aspect of the wrist on the same coronal sections that display the TFC and interosseous ligaments.
-
The radial collateral ligament may be partially visualized between the scaphoid and radial styloid.
-
The articular cartilage surfaces of the carpal bones demonstrate intermediate signal intensity on T1-weighted images and increase in signal intensity on T2*-weighted images.
-
On dorsal images through the carpus, the interosseous ligaments of the distal carpal row can be defined. Dorsally, the obliquely oriented extensor digiti minimi tendon on the ulnar side of the triquetrum and the extensor carpi radialis longus tendon are seen. Lister's tubercle, which contains fatty marrow, is situated between and separates the ulnar aspect of the extensor pollicis longus from the radial aspect of the extensor carpi radialis brevis. The dorsal interossei muscles are demonstrated between the midcarpal shafts.
-
The flexor digitorum superficialis and profundus tendons are seen as tubular hypointense structures with invested synovial sheaths.
-
In proximal sections, the flexor pollicis longus is seen deep to the median nerve. Distally, it is flanked by the adductor pollicis medially and by the thenar muscles laterally, toward the thumb.
-
At the level of the distal radioulnar joint, the volar distal radioulnar ligament is identified as a thin, hypointense band, deep to the flexor digitorum profundus tendons and Parona's space. The position of the distal ulna in relation to the sigmoid notch is determined at this level.
-
The TFC complex is displayed on the ulnar aspect of the ulnar styloid.
-
The curve of the ulnolunate ligament is demonstrated at the level of the proximal lunate and distal radius, where it follows the contour of the ulnar and volar aspect of the lunate.
-
The palmaris longus tendon is superficial to the median nerve.
-
The thin hypointense flexor retinaculum spans the palmar border of the carpal tunnel. Its distal attachments to the hook of the lunate and tubercle of the trapezium are more reliably defined than the proximal attachments to the tubercles of the pisiform and scaphoid.
-
The separate extensor tendons of the extensor carpi ulnaris, extensor digiti minimi, extensor digitorum and indicis, extensor carpi radialis brevis, extensor pollicis longus, and extensor carpi radialis longus are displayed from the ulnar to the radial dorsal aspect of the wrist.
-
The lunotriquetral and scapholunate ligaments are usually demonstrated at the level of the proximal carpal row.
-
The arcuate ligament is seen volar to the capitate and deep to the flexor tendons.
-
The radial collateral ligament is closely applied to the radial surface of the scaphoid.
-
The palmaris longus tendon is superficial to the median nerve and the flexor retinaculum.
-
The two central tendons of the superficial flexor group are located superiorly within the carpal tunnel before they fan out to their insertions on the middle phalanx.
-
On axial plane images, it is possible to differentiate the four separate tendons of the flexor profundus group.
-
The lumbrical muscle origins are seen deep to the flexor tendons on axial sections through the distal carpal tunnel and demonstrate intermediate signal intensity.
-
The median nerve, also of intermediate signal intensity, can be identified in the superficial radial aspect of the carpal tunnel.
-
On axial images through the midmetacarpals, the flexor tendons are seen anterior to the palmar interossei muscles, whereas the dorsal interossei are seen lying between the metacarpal bones.
-
Blood vessels display low signal intensity, except in venous structures demonstrated by even-echo rephasing or paradoxical enhancement secondary to slow flow. With gradient-echo techniques, both arterial and venous structures demonstrate hyperintensity.
|
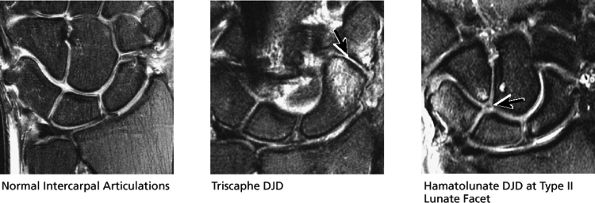
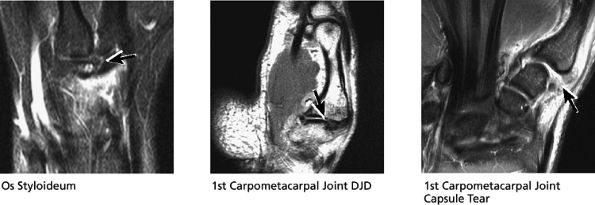
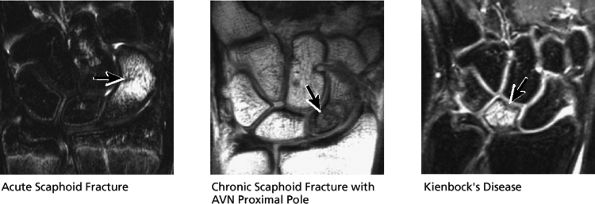
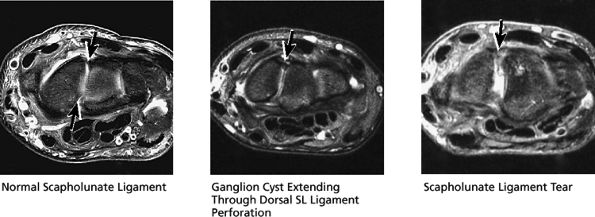
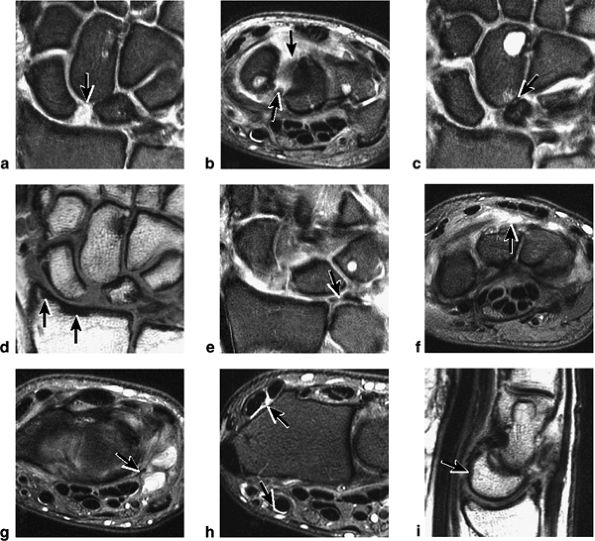
FIGURE 10.31 ● Normal coronal anatomy. (A) Fatty atrophy or denervation of the thenar muscles raises the possibility of median neuritis, and in such cases the median nerve is closely examined for enlargement or increased signal. (B) Tenosynovitis of the flexor tendons with fluid in the tendon sheaths can occasionally cause enough mass effect on the median nerve to cause median neuritis. (C) The first carpometacarpal joint (the articulation between the trapezium and the base of the first metacarpal) is a common location for degenerative arthrosis, often visualized at the corner of a coronal image. (D) Fluid in the pisotriquetral recess is a common finding. In the absence of other findings such as degenerative changes at the joint, a small amount of fluid in the pisotriquetral recess is probably of no significance. (E) Fractures of the distal scaphoid extending to the articular surface should be characterized as entering the lunate fossa (the radial articulation with the lunate) or the scaphoid fossa (the radial articulation with the scaphoid). Such articular extension, particularly if depressed or displaced, can lead to significant radiocarpal degenerative disease. (F) The triscaphe joint consists of the distal pole of the scaphoid articulating with the trapezoid and trapezium and is considered the second most common site of wrist arthrosis. (G) The proximal row should normally form a continuous smooth convex curve. Any subtle offset of the triquetrum from the lunate, or the scaphoid from the lunate, is suggestive of a tear of the lunotriquetral or scapholunate ligaments. (H) The triangular fibrocartilage attachment to the radius may attach to hyaline articular cartilage, and it is important not to mistake the gray cartilage signal at the attachment for a tear, which is usually of fluid signal intensity. (I) The proximal pole of the hamate may occasionally articulate with a normal variant type II lunate facet located on the distal ulnar aspect of the lunate. When this occurs, degenerative changes are visualized at the hamate-lunate articulation in almost half of cases. (J) Small degenerative perforations in the membranous component of the scapholunate ligament are not uncommon in older patients, and in this population they may be asymptomatic and unassociated with carpal instability. (K) The TFC has insertions at the tip and at the base of the ulnar styloid. Therefore, fractures at the base of the ulnar styloid may disrupt the integrity of the TFC and potentially cause distal radial ulnar joint instability. (L) On coronal images through the dorsal wrist, the dorsal component of the scapholunate ligament may occasionally be discretely identified. The dorsal component is considered the most important of the scapholunate ligament components for maintaining carpal stability. (M) Another significant and commonly overlooked location for degenerative arthrosis is at the base of the third metacarpal, where a common protuberance, called a carpal boss, articulates with the capitate. Unusually prominent carpal bosses may become hypertrophic and articulate with a spur on the distal capitate, which can often be palpated by the patient as a tender bump just beneath the skin along the dorsal wrist. (N) Ganglion cysts can be visualized extending through the dorsal capsular ligaments on coronal images through the dorsal wrist. Common sites of origin are the scapholunate ligament, the triscaphe joint, and the third carpometacarpal joint (often associated with degenerative change at a carpal boss).
|
|
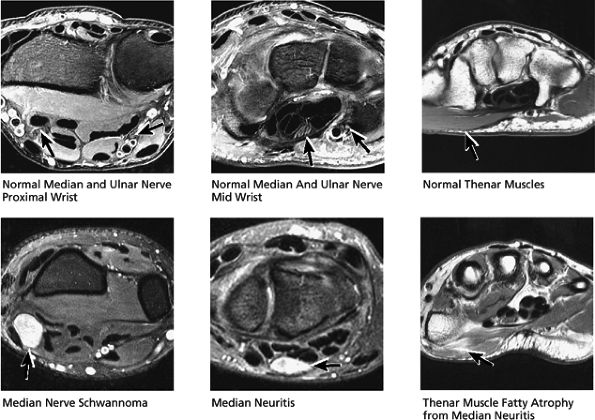
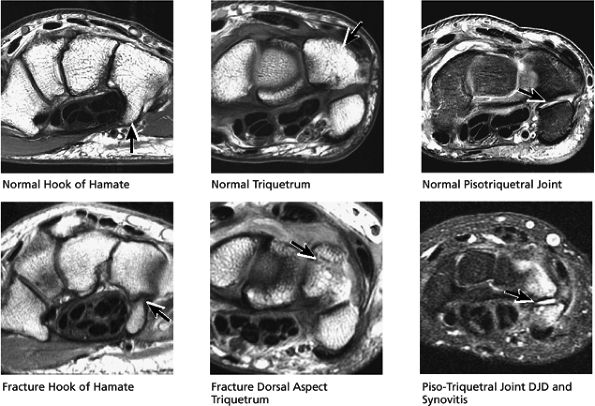
FIGURE 10.32 ● Normal axial anatomy. (A) Fractures of the hook of the hamate, commonly occult on plain films, are easily visualized on axial MR images through the hamate. (B) The flexor carpi radialis is visualized cradled by the hook of the trapezium. This is a common location for tenosynovitis and tendinosis of the flexor carpi radialis tendon. (C) The thenar muscles (abductor and flexor pollicis brevis) are visualized volar to the radial aspect of the distal carpus. Median neuritis should be suspected when selective fatty atrophy or denervation of the thenar muscles is visualized. (D) The median nerve within the carpal tunnel may display evidence of median neuritis, such as increased signal or enlargement. A mass lesion of the carpal tunnel at this level may cause mass effect within the carpal tunnel and impinge the median nerve. (E) The pisotriquetral joint is a common location for severe degenerative arthritis and synovitis, associated with significant ulnar-sided pain. (F) The extensor pollicis longus crosses obliquely dorsal to the extensor pollicis longus and brevis tendons. This is a not uncommon location for tears of the extensor pollicis longus tendon. (G) The scapholunate articulation is a common location for ganglion cysts, usually found directly dorsal to the scapholunate ligament. Even small dorsal ganglion cysts in this location can be exquisitely tender and painful. Often, a small neck of fluid signal extends from the dorsal ganglion cyst back toward the scapholunate ligament, and in certain cases a small perforation of the scapholunate ligament can be suggested. (H) The extensor pollicis brevis and abductor pollicis longus tendons are located lateral to the distal radius. Tendinosis and tenosynovitis of these tendons is known as de Quervain's stenosing tenosynovitis. (I) Not uncommonly the extensor carpi ulnaris tendon is subluxed over the ulnar styloid, particularly when the patient is supinated, with the ulnar styloid pointing dorsally. This is not necessarily an abnormal finding, particularly when the extensor carpi ulnaris tendon otherwise appears normal. (J) The triangular shape of the TFC complex is best appreciated on axial images, with the apex of the triangle attaching at the ulnar styloid and the broader base of the triangle attaching at the radius. (K) The distal radioulnar joint is examined in the axial plane to view the alignment of the radius with respect to the ulna. The ulna lies within the concave groove in the medial aspect of the radius called the sigmoid notch, and the two bones lie grossly in the same plane. Mild apparent dorsal shift of the ulna with respect to the radius is normal when the wrist is scanned in full pronation (the ulnar styloid pointing ulnar-volar). (L) When the triangular fibrocartilage is torn, or if there is a displaced fracture at the base of the ulnar styloid, the distal radial ulnar joint may become somewhat destabilized, ultimately resulting in degenerative arthrosis and synovitis. Another cause of distal radioulnar joint degenerative change is the ulnar impingement syndrome, in which a short ulna erodes the ulnar aspect of the distal radius.
|
-
The abductor pollicis longus and extensor pollicis brevis tendons can be seen on radial sagittal images.
-
The scaphoid is identified on sagittal sections through the trapezium and, more dorsally, the trapezoid.
-
The hypointense radioscaphocapitate ligament is represented by fibers seen along the volar aspect of the scaphoid between the volar distal radius and the distal pole of the scaphoid.
-
The extensor pollicis longus tendon is dorsal to the radioscaphoid articulation.
-
The pronator quadratus muscle extends along the volar surface of the radial metaphysis and distal diaphysis.
-
The low-signal-intensity tendon of the flexor carpi radialis is draped volarly over the distal pole of the scaphoid.
-
The long axis (i.e., vertical orientation) of the flexor pollicis longus tendon is seen at the ulnar aspect of the scaphoid.
-
The capitate, lunate, and radius are colinearly aligned in sagittal images through the third metacarpal axis.
-
The radial limb of the deltoid or arcuate ligament extends proximally from the volar aspect of the capitate to the scaphoid. In the sagittal plane, the deltoid ligament may appear to connect to the volar distal surface of the lunate.
-
The radiolunate ligament is located between the volar lunate surface and the distal radius at the radiolunate articulation, deep to the flexor digitorum profundus tendon.
-
The ulnolunate ligament is radial to the TFC.
-
The flexor digitorum superficialis and profundus tendons are best seen volar to the capitate and lunate. The flexor retinaculum is a thin hypointense line superficial to the flexor digitorum superficialis. The ulnar limb of the arcuate ligament is seen volar to the radial aspect of the triquetrum and the ulnar aspect of the lunate, ulnar to the plane of section through the capitate.
-
The fourth metacarpal, the hook of the hamate, and the triquetrum are seen in the same sagittal section at the ulnar-most aspect of the lunate or radial aspect of the ulna. The lunotriquetral interosseous ligament is also seen at this level.
-
The TFC complex is located between the lunate and the ulna and has a concave distal surface.
-
On ulnar sagittal images, the flexor carpi ulnaris extends in a volar direction to insert on the pisiform.
-
The pisohamate and pisometacarpal ligaments attach to the hook of the hamate and the base of the fifth metacarpal, respectively.
-
The intermediate-signal-intensity ulnar nerve is deep to the flexor carpi ulnaris.
-
The ulnar collateral ligament component of the TFC complex extends between the triquetrum and ulna, as can be seen on ulnar sagittal images out of the plane of the TFC.
-
The thick extensor carpi ulnaris tendon is seen as a groove in the posterior aspect of the distal ulna. In peripheral ulnar sagittal sections, it can be seen to extend dorsal to the triquetrum and insert onto the base of the fifth metacarpal.
-
The intrinsic carpal ligaments, including the scapholunate and lunotriquetral ligaments
-
The triangular fibrocartilage, including the dorsal and volar margins
-
The radial and ulnar styloid (for fractures) and the scaphoid and lunate fossa of the distal radius for fractures and cartilage degeneration
-
The triscaphe articulation (for degenerative changes)
-
The distal radioulnar articulation, radiocarpal joints, intercarpal joints, and carpometacarpal joints for evidence of arthrosis or posttraumatic change
|
FIGURE 10.33 ● Normal sagittal anatomy. (A) The first carpometacarpal joint, visualized at the top of the field of view on sagittal images, is a common location for degenerative arthrosis. (B) Similar to the hamate, the trapezium also has a “hook,” although it is smaller and is rarely fractured. (C) An anteriorly tipped (or “flexed”) scaphoid is a sign of carpal instability, often associated with scapholunate ligament tears or scaphoid fractures. (D) DISI is suggested when the capitate lunate angle exceeds 30°. When DISI is present, the scapholunate ligament is evaluated for associated tears. (E) Sagittal images afford another opportunity to examine the hook of the hamate for fractures. (F) Triquetral fractures usually occur when the dorsal aspect of the triquetrum is avulsed by the radiotriquetral ligament. Similar to the lateral view on plain films, sagittal images demonstrate the dorsal triquetral avulsion fracture fragment. (G) Sagittal images through the abductor pollicis longus and extensor pollicis brevis tendon afford additional opportunities to identify and characterize the findings of de Quervain's stenosing tenosynovitis. (H) Occasionally, focal prominence of tortuous veins and arteries about the wrist can mimic ganglion cysts on sagittal fluid-sensitive sequences. These vessels can be distinguished from ganglions by viewing successive images and visualizing continuity of the vascular structures. (I) Tears and sprains of the dorsal and volar extrinsic capsular ligaments are optimally visualized in the sagittal plane. (J) The longitudinal extent and length of median nerve involvement in median neuritis can be measured and characterized in the sagittal plane. (K) Near its radial attachment, the triangular fibrocartilage fans out to a broad, bowtie-shaped structure, resembling the appearance of the meniscus on sagittal images of the knee. (L) Near its ulnar attachment, the triangular fibrocartilage is visualized as a short, narrow band of hypointense cartilage that represents the convergence of the dorsal and volar radial ulnar ligaments at the apex of the triangular TFC.
|
 |
|
FIGURE 10.34 SCAPHOLUNATE LIGAMENT.
|
-
The intrinsic ligaments, with the axial plane allowing assessment of the separate dorsal and volar components of the scapholunate and lunotriquetral ligament
-
The extensor tendons, including the extensor carpi ulnaris tendon on the ulnar aspect of the wrist, and the extensor pollicis brevis and abductor pollicis longus tendon on the radial aspect of the wrist, for tendinosis, tears, or tenosynovitis
-
The flexor tendons and the carpal tunnel on the volar aspect of the wrist
-
The median nerve and ulnar artery
-
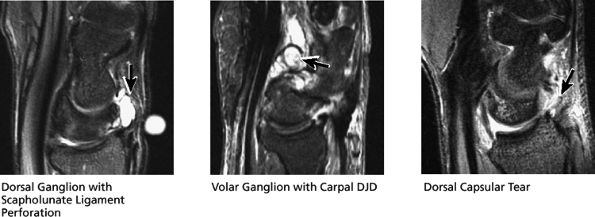
The dorsal and volar capsule and ligaments, for the presence of ganglion cysts or sprain of the capsule
-
The hook of the hamate, for fracture
-
The TFC
-
The distal radioulnar joint, for instability, thenar and hypothenar atrophy (indicative of median neuritis), or strain, and to confirm or characterize fractures
-
Abnormal carpal alignment suggesting carpal instability
-
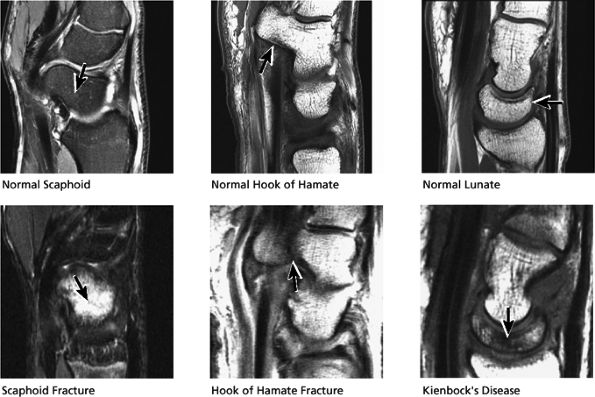
Fractures of the carpal bones, including the hook of the hamate, scaphoid, and lunate
-
Triangulation on abnormalities of the TFC, scapholunate, and triquetrolunate ligaments
-
Ganglion cysts
-
Capsular sprain
-
Fractures
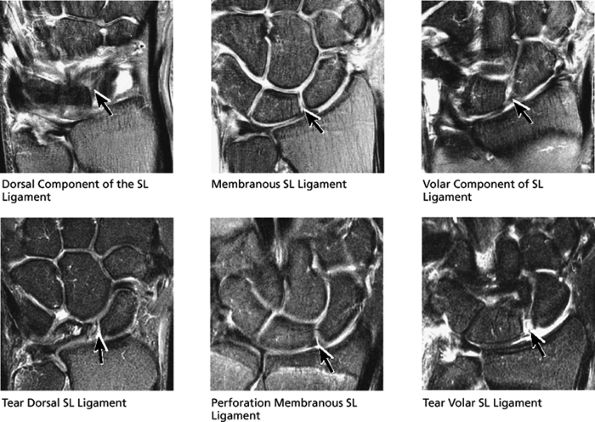
However, a fluid-filled gap interposed between the membranous scapholunate ligament and the cartilage or bones should be interpreted as a perforation or detachment. Such membranous scapholunate ligament perforations and detachments are more common with advancing age (similar to tears of the TFC central disc), and in isolation may not necessarily result in carpal instability or significant symptoms. The volar-most images demonstrate the volar scapholunate ligament, which courses obliquely and attaches to bone on either side of the ligament. Tears of the volar and radial aspects of the scapholunate ligament suspected in the coronal plane can be confirmed in the axial plane. After identifying a scapholunate ligament tear, the scapholunate interval is assessed for widening, reactive bone marrow changes on either side of the scapholunate articulation, and bony or cartilaginous avulsions at the site of tearing or detachment. In addition, in the setting of scapholunate ligament tears, associated patterns of carpal instability, such as dorsal intercalated segment instability (DISI) pattern, can be identified on corresponding sagittal images.
 |
|
FIGURE 10.35 LUNOTRIQUETRAL LIGAMENT.
|
aspect of the lunate fossa. The distal lateral tip of the radius is known as the radial styloid. Fractures through the radial styloid may extend into the scaphoid fossa. Fractures through the lunate and scaphoid fossae can lead to subsequent radiocarpal degenerative arthrosis. Fractures of the ulnar styloid are characterized as occurring either at the distal ulnar styloid or at the base of the ulnar styloid. Fractures that occur at the base of the ulnar styloid can destabilize the ulnar attachments of the TFC, leading to subsequent distal radial ulnar joint instability.
 |
|
FIGURE 10.36 Triangular Fibrocartilage.
|
ulnar styloid can chronically impact the proximal triquetrum.
 |
|
FIGURE 10.37 DISTAL RADIUS AND ULNA.
|
 |
|
FIGURE 10.38 RADIOCARPAL JOINT.
|
(ulnolunate) impaction syndrome, whereas ulnar negative variance may be associated with Kienböck's disease of the lunate. With distal radioulnar joint instability, the ulna is dorsally or volarly subluxed with respect to the radius, usually due to severe TFC complex tears.
 |
|
FIGURE 10.39 CARPAL JOINTS.
|
 |
|
FIGURE 10.40 CARPOMETACARPAL JOINTS.
|
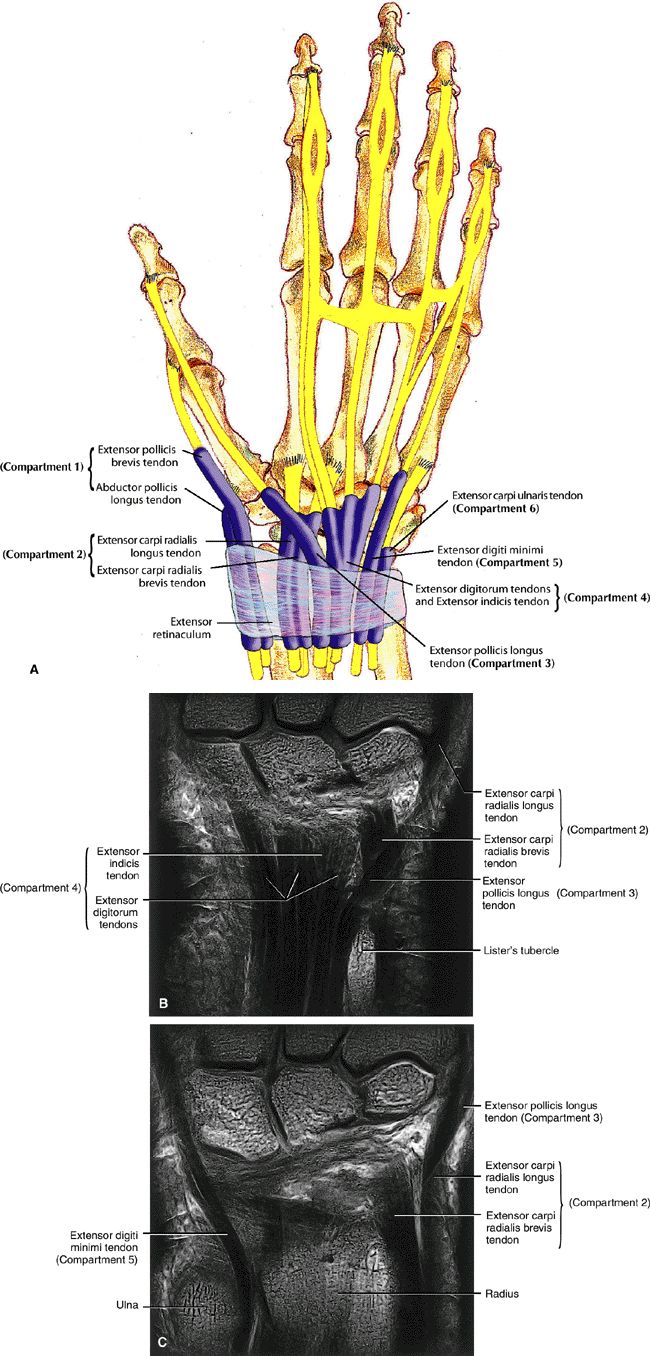
-
Compartment 1 lies along the lateral aspect of the radius and contains the extensor pollicis brevis and the abductor pollicis longus.
-
Compartment 2 contains the extensor carpi radialis brevis and longus.
-
Compartment 3 contains the extensor pollicis longus.
-
Compartment 4 contains the extensor digitorum tendons.
-
Compartment 5 contains the extensor digiti minimi.
-
Compartment 6 contains the extensor carpi ulnaris, which runs within the groove formed by the ulnar styloid.
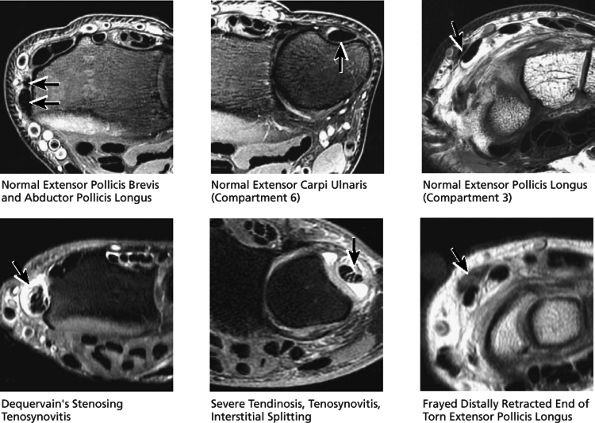
radial aspect of the distal forearm (proximal to the wrist), where the first compartment muscles cross over the second extensor compartment tendons. Tendinosis and tearing of the extensor carpi ulnaris (in compartment 6) is also common and presents as dorsal ulnar-sided pain. The extensor pollicis longus (in compartment 3) can also occasionally tear. The distally retracted, thickened, and frayed end of the torn extensor pollicis longus is often visualized at the level of the proximal carpal row, where the extensor pollicis longus tendon crosses dorsal to the extensor carpi radialis brevis and longus tendons.
 |
|
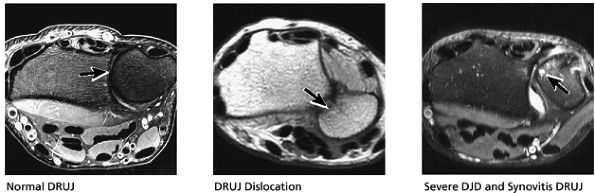
FIGURE 10.41 DISTAL RADIOULNAR JOINT.
|
 |
|
FIGURE 10.42 SCAPHOID AND LUNATE.
|
abnormalities. In particular, close attention should be paid to the hook of the hamate in the axial plane. Pisotriquetral arthrosis and synovitis are also evaluated on axial images.
 |
|
FIGURE 10.43 SCAPHOLUNATE LIGAMENT.
|
 |
|
FIGURE 10.44 EXTENSOR COMPARTMENT.
|
 |
|
FIGURE 10.45 FLEXOR COMPARTMENT.
|
 |
|
FIGURE 10.46 MEDIAN AND ULNAR NERVE.
|
 |
|
FIGURE 10.47 CARPUS.
|
 |
|
FIGURE 10.48 GANGLION CYSTS.
|
-
In a neutral position the ulnar styloid is located medially.
-
In pronation the ulnar styloid points volarly.
-
In supination the ulnar styloid points dorsally.
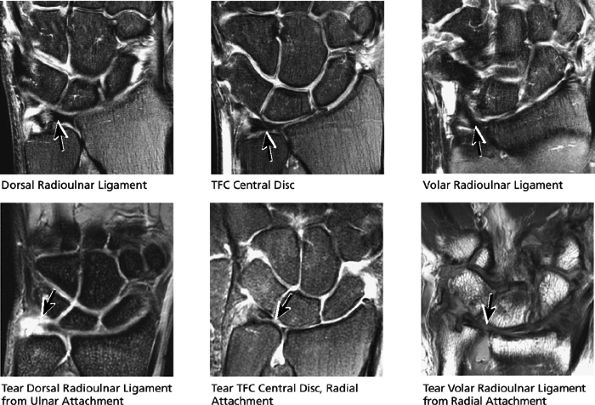
The dorsal radioulnar ligament and palmar radioulnar ligament are the primary ligamentous stabilizers of the distal radioulnar joint and on axial plane images are seen coursing on both the dorsal and volar sides of the TFC, at the level of the base of the ulnar styloid, where the ligaments insert. Tears of the dorsal radioulnar ligament are associated with volar subluxation of the ulna. Tears of the volar radioulnar ligament are associated with dorsal subluxation of the ulna. Distal radioulnar joint instability is suggested when the ulnar head is abnormally subluxed or dislocated with respect to the radius, beyond the normal range of motion allowed for pronation and supination. In addition to ligamentous injury, osseous injuries such as fractures at the base of the ulnar styloid also may lead to distal radioulnar joint instability.
 |
|
FIGURE 10.49 DISTAL RADIOULNAR JOINT.
|
 |
|
FIGURE 10.50 CARPUS.
|
exceeds 30°. When DISI is present, the scapholunate ligament is evaluated for associated tears. The position of the scaphoid with respect to the rest of the carpus is also assessed. An anteriorly tipped or “flexed” scaphoid is an additional sign of DISI. When the lunate is tipped in a volar direction, with palmar translocation of the carpus, volar intercalated segmental instability (VISI) is suggested. VISI is associated with lunotriquetral ligament tears and dorsal extrinsic ligament injuries.
 |
|
FIGURE 10.51 CARPAL ALIGNMENT.
|
 |
|
FIGURE 10.52 GANGLION CYSTS AND DORSAL CAPSULE.
|
similar to the meniscus. Tears of the TFC are visualized as defects or gaps in the substance of the TFC. Tears of the membranous portion of the TFC manifest as a gap with a diastasis between the two ends of the bow-tie. The scapholunate and lunotriquetral ligaments are harder to visualize on sagittal images. However, tears of the dorsal or volar components of these ligaments, or ganglion cysts extending through these ligaments, are occasionally seen and further characterized on sagittal images.
 |
|
FIGURE 10.53 NORMAL TENDONS AND NERVES.
|
 |
|
FIGURE 10.54 TRIANGULAR FIBROCARTILAGE AND SCAPHOLUNATE LIGAMENT.
|
-
Scapholunate ligament diastasis with greater than 4 mm of diastasis of the scapholunate ligament. Superim-posed arthrosis of the capitolunate articulation.
-
Mild sclerosis of the radial styloid scapholunate articulation consistent with a component of SLAC arthritis.
-
Fraying of the proximal and distal aspects of the triangular fibrocartilage.
-
Mild degenerative change in the lunotriquetral ligament.
-
Synovitis and ganglion cyst in communication with the pisiform triquetral articulation.
-
DISI instability of the wrist with dorsal tilting of the lunate.
the metacarpals. There are three major compartments of the wrist as defined by arthrographic studies:
-
The radiocarpal compartment
-
The midcarpal compartment
-
The distal radioulnar joint compartment
 |
|
FIGURE 10.55
|
-
Anatomy of the Wrist
-
The carpal bones absorb stress from the palm to the radius, change geometric shape in response to motion, and form a proximal row intercalary segment.
-
The extrinsic ligaments, which connect the radius or ulna to the carpal bones or the metacarpal to the carpal bones, provide gross stability.
-
The intrinsic ligaments include the intercarpal ligaments, which provide intermediate stability, and the interosseous ligaments, which provide for “fine-tune” stability.
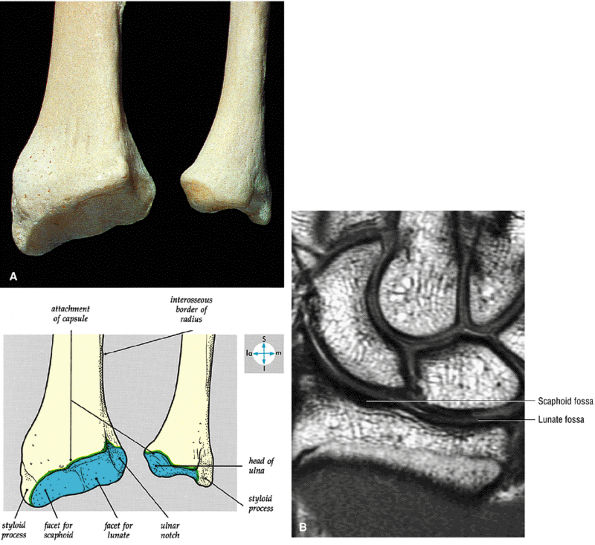
At the site of the radiolunate articulation, the distal articular surfaces of the radius and ulna are usually at the same level (i.e., neutral ulnar variance). Alternatively, the ulna may be relatively long (positive ulnar variance), leading to an ulnar abutment syndrome, or relatively short (negative ulnar variance), as is often seen in Kienböck's disease. The distal radius forms two facets that articulate with the scaphoid and lunate of the proximal carpal row. This articulation of the proximal pole of the scaphoid in the scaphoid fossa is quite congruent, and even a small degree of malrotation of the scaphoid may cause incongruent loading of the articular cartilage and subsequent degeneration (such as that which accompanies a SLAC wrist, as described by Watson and Ryu37). The lunate facet commonly becomes incongruent following distal radius fractures, especially die-punch-type fractures. The interosseous ligaments join the proximal carpal bones at their proximal edges.36
 |
|
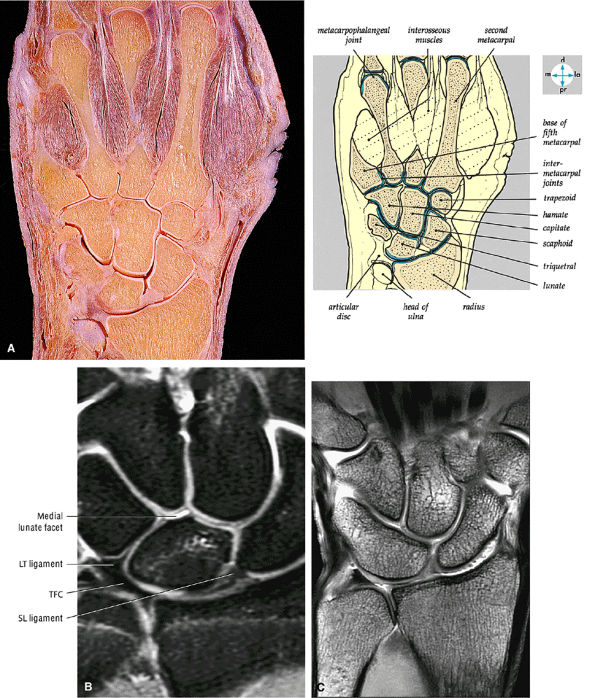
FIGURE 10.56 ● (A) An anterior view of the distal ends of the radius and ulna. The bones have been separated to reveal the ulnar notch. (B) Corresponding scaphoid and lunate fossa on coronal PD FSE image. The scaphoid has five articulations: the trapezium and trapezoid distally, the radius proximally, and the capitate and lunate medially. The lunate articulates with five bones: the radius proximally, the capitate and hamate distally, the scaphoid laterally, and the triquetrum medially.
|
 |
|
FIGURE 10.57 ● The articular surface of the distal end of the radius and the adjacent triangular cartilage are exposed by removal of the carpal bones.
|
 |
|
FIGURE 10.58 ● Lister's tubercle (dorsal tubercle) of the distal radius on a coronal PD FSE image. Lister's tubercle functions as a pulley for the extensor pollicis longus.
|
All arthroscopic portals are, of necessity, dorsally placed, making examination of the volar ligaments especially easy. As a result, the dorsal ligaments initially received less attention. Definition of pathologic conditions naturally followed elucidation of the ligamentous anatomy, resulting in the development of a variety of treatment procedures.39
 |
|
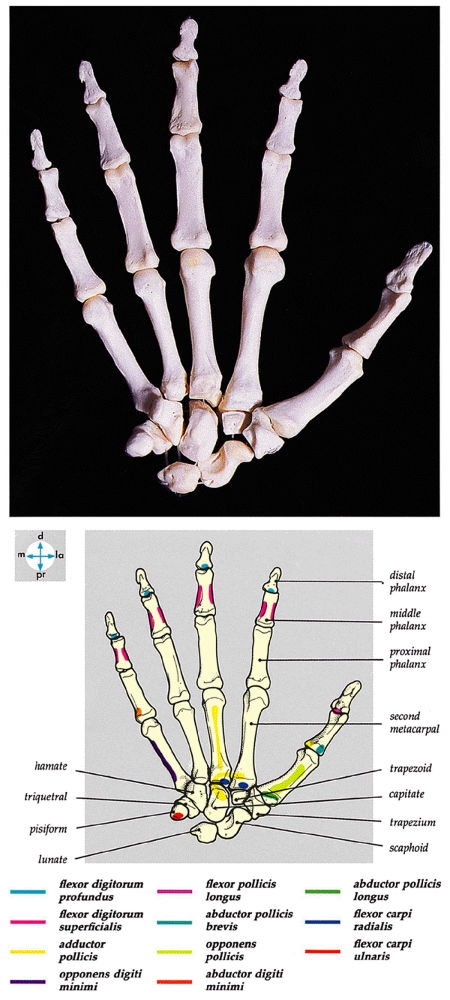
FIGURE 10.59 ● The bones of the hand. Adjacent bones, particularly in the carpus, have been slightly separated to reveal their articular surfaces.
|
 |
|
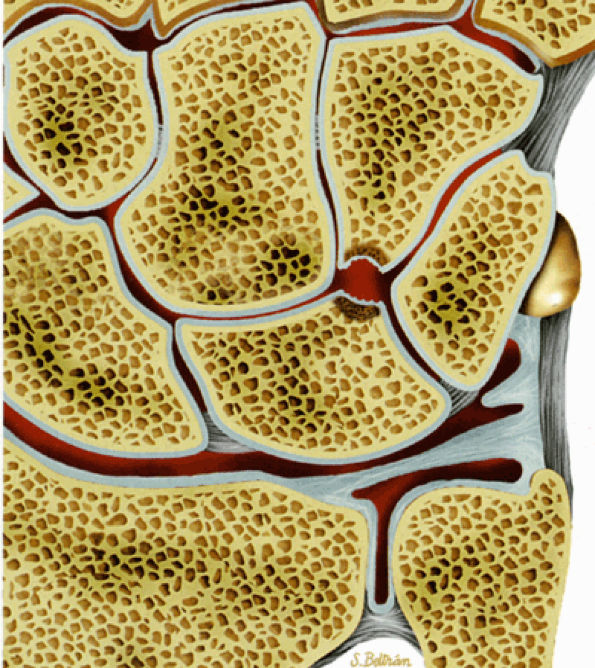
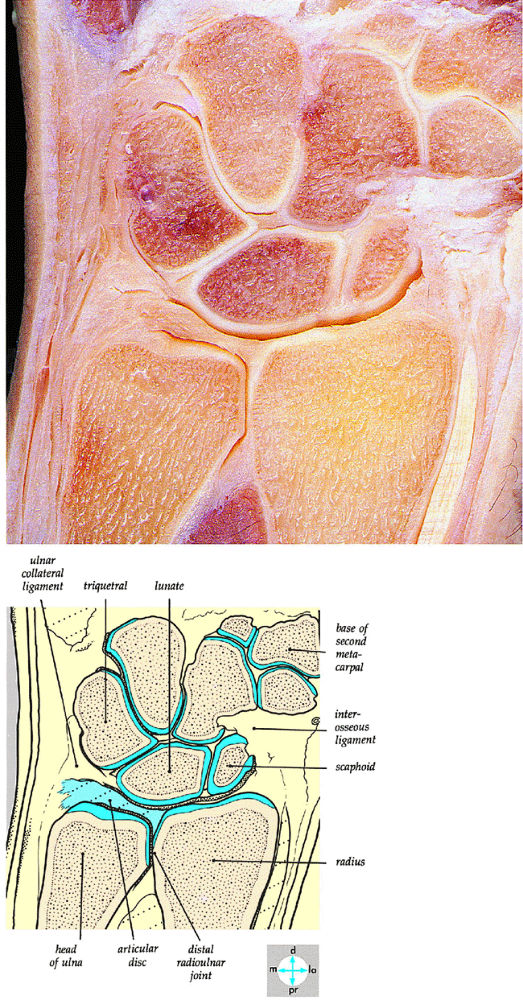
FIGURE 10.60 ● (A) A coronal section of the hand shows the joints of the carpal region. The thumb and little finger are anterior to the plane of section. (B) Coronal FS PD FSE image demonstrating the membranous components of the scapholunate (SL) and lunotriquetral (LT) ligaments. The central disc of the TFC is identified. (C) Complete osseous lunotriquetral coalitions are fibrous, cartilaginous, or osseous. Osseous coalitions may be incomplete or complete.
|
scaphoid, and also inserts on the center of the capitate.43 The radioscaphocapitate ligament forms a supporting sling at the waist of the scaphoid. As the fibers cross the proximal pole of the scaphoid, there is a fold of synovium that separates them from the bone.44 In this position, the ligament can be interposed between the fragments of a scaphoid fracture and contribute to nonunion. The radioscaphocapitate ligament, which has a striated appearance on volar coronal MR images, is located distal to the radiolunotriquetral ligament, which has a similar ulnodistal obliquity (Fig. 10.62). Sagittal images demonstrate the volar location of the radioscaphocapitate in cross-section relative to the waist of the scaphoid.
|
TABLE 10.1 Extrinsic and Intrinsic Ligaments of the Wrist
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
FIGURE 10.61 ● The radioscapholunate ligament courses between the short and long radio-lunate (radiolunotriquetral) ligaments. The fibers of the short radiolunate ligament contribute to the floor of the radiolunate space. (From Stoller DW. MRI, arthroscopy, and surgical anatomy of the joints. Philadelphia: Lippincott.)
|
similar to the radioscaphocapitate ligament. There is an interligamentous sulcus between the radioscaphocapitate and the radiolunotriquetral ligaments on sagittal images (Fig. 10.65). The radiolunotriquetral is a strong ligament that stabilizes the proximal carpal row on the radius and should be differentiated from the radioscapholunate ligament.
 |
|
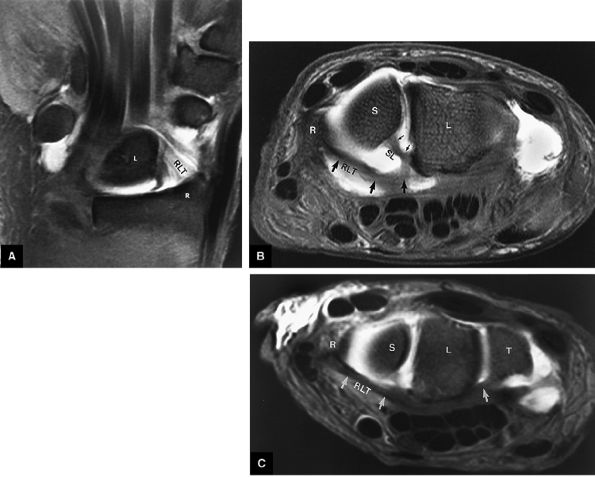
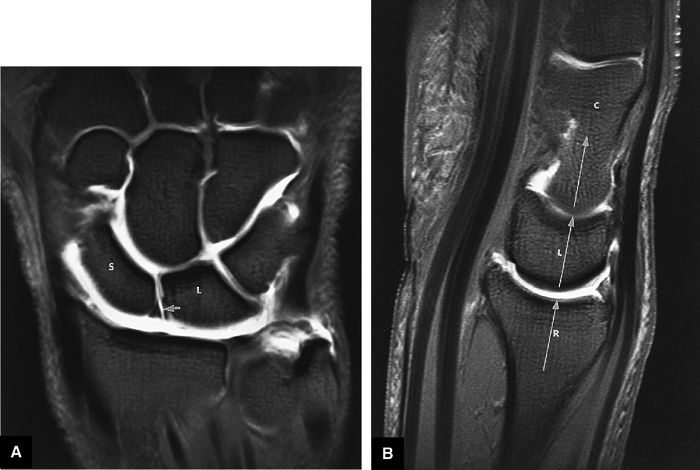
FIGURE 10.62 ● Anatomy of the radioscaphocapitate (RSC), radiolunotriquetral (RLT), and radioscapholunate (rsl) ligaments at the level of the distal volar radius (R). T, triquetrum; S, scaphoid. FS T1-weighted arthrogram after radiocarpal injection.
|
 |
|
FIGURE 10.63 ● The long radiolunate or radiolunotriquetral (RLT) ligament. (A) The RLT ligament is divided into a radiolunate ligament and lunotriquetral component. The RLT ligament functions as a volar sling for the lunate. L, lunate; R, radius. Volar FS coronal T1-weighted arthrogram. FS axial T1-weighted arthrograms obtained at the level of the proximal (B) and distal (C) aspects of the radial styloid show the volar course of the RLT ligament (large arrows) from the radial styloid (R) inserting into the lunate (L) and blending with the volar portion of the lunotriquetral interosseus ligament. The lunate attachment of the scapholunate interosseous ligament volar fibers is deep to the lunate attachment of the RLT ligament (B). S, scaphoid; T, triquetrum; SL, scapholunate ligament.
|
a straight course or minimally convex radial border directed toward the scapholunate interval. The radioscapholunate ligament does not have the striations previously described for the radioscaphocapitate and radiolunotriquetral ligaments on coronal images. The proximal attachment of the radioscapho-lunate ligament should never be confused with the normal articular cartilage ridge that separates the scaphoid and lunate fossa of the distal radius. This articular cartilage ridge has a broad-based attachment to the distal radius.
 |
|
FIGURE 10.64 ● The radiolunotriquetral or long radiolunate ligament. This ligament acts as a volar sling for the lunate. Coronal T1-weighted arthrogram.
|
The dorsal ligaments do not exist as discrete anatomic entities, and they vary considerably from subject to subject. Two major components can be discerned:
-
The first component is the dorsal radioscapholunotriquetral ligament, a thickening of the dorsal capsule that courses from the dorsal lip of the radius and inserts on the dorsal surfaces of the scaphoid, lunate, and triquetrum. This ligament acts as a checkrein on the proximal carpal row and prevents it from assuming a position of excessive volarflexion. Biomechanical studies have shown that in the final stage of ulnar-sided perilunate instability, it is the radioscapholunotriquetral ligament that is injured.49 Laxity of the radioscapholunotriquetral ligament has been implicated in palmar midcarpal instability patterns in which the lunate is allowed to go into volarflexion, leading to instability.
-
The second major component of the dorsal ligamentous structure is the scaphotriquetral (or triquetroscaphoid) ligament. This is a transversely oriented thickening of the dorsal capsular fibers that runs from the scaphoid to the triquetrum.
 |
|
FIGURE 10.65 ● The interligamentous sulcus between the radioscaphocapitate (RSC) and radiolunotriquetral ligaments is seen on an FS sagittal T1-weighted arthrogram at the level of the scaphoid (S). The volar aspect of the wrist is labeled. The radio-lunotriquetral ligament is proximal to the RSC ligament.
|
 |
|
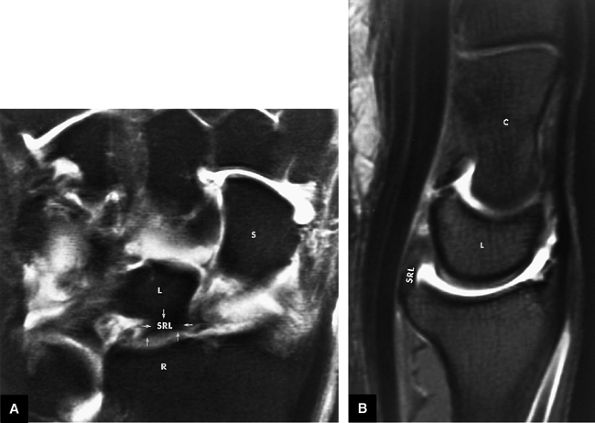
FIGURE 10.66 ● The short radiolunate ligament (SRL). (A) The SRL (arrows) can be seen extending volarly to the lunate fossa of the distal radius to its insertion on the radial volar aspect of the lunate. S, scaphoid. FS T1-weighted coronal arthrogram. (B) The SRL is identified on an FS T1-weighted sagittal image at the level of the capitate (C) and lunate (L).
|
-
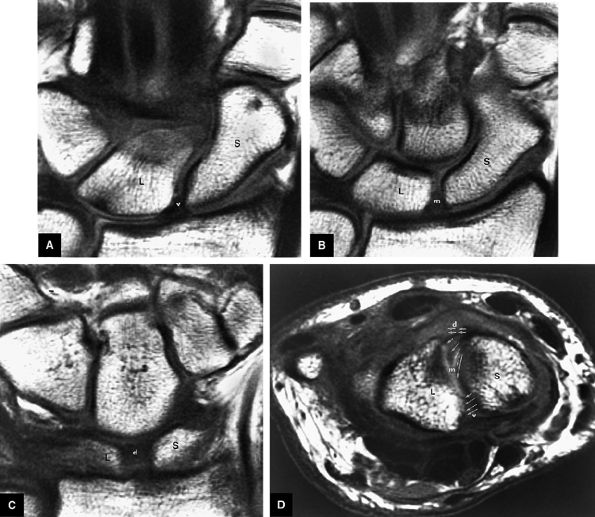
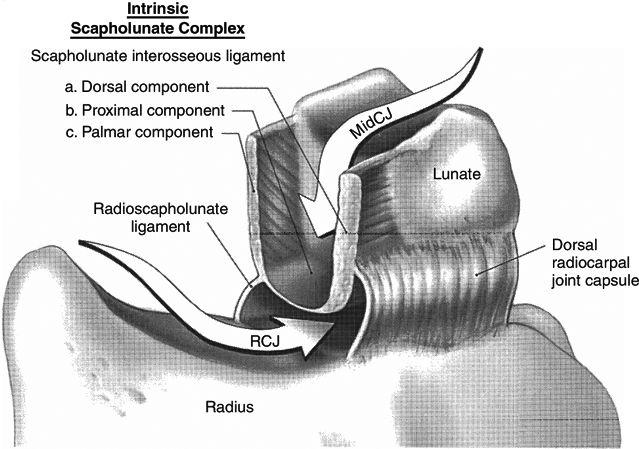
The scapholunate ligament is triangular on coronal section and is peripherally attached at the scapholunate interval. The inner apex of the triangular ligament is not attached to bone and is free within the scapholunate joint (Fig. 10.74).52
-
The dorsal fibers of the scapholunate ligament are oriented transversely, or perpendicular to the joint, and form a thick bundle. The dorsal portion of the scapho-lunate ligament is considered to be the most important component in maintaining carpal stability.
-
The membranous scapholunate ligament fibers course peripherally and obliquely from the scaphoid downward to the lunate. The membranous scapholunate ligament fibers attach to both bone and articular cartilage, whereas the dorsal and volar portions of the scapholunate ligament attach directly to bone.
-
The volar scapholunate ligament fibers course obliquely between the volar aspects of the lunate and scaphoid.
-
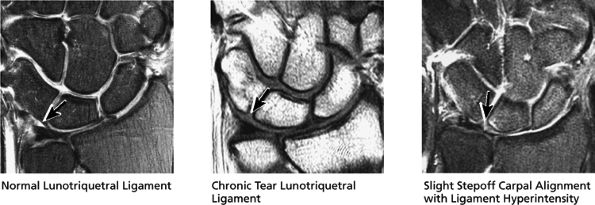
The lunotriquetral ligament is usually visualized as a thin horseshoe-shaped structure that may appear more lax than the scapholunate ligament on MR imaging.43 The lunotriquetral ligament does not extend as far distally into the lunotriquetral joint as the longer proximal distal portion of the scapholunate ligament does within the scapholunate joint.
-
The volar and dorsal portions of the lunotriquetral ligament attach directly to bone, whereas its midportion attaches to the hyaline articular cartilage of the lunotriquetral joint.43
-
Smith and Snearly53 have shown that on coronal MR images the lunotriquetral ligament is most commonly delta-shaped (triangular) or linear.
 |
|
FIGURE 10.67 ● Anatomy of the radioscapholunate (RSL) and radioscaphocapitate (RSC) ligaments. (A) The RSL ligament represents a neurovascular structure extending from the distal radius into the scapholunate articulation. This ligament, which has also been referred to as the ligament of Testut and Kuenz, is located volar to the intrinsic scapholunate ligament. RLT, radiolunotriquetral ligament; L, lunate; R, radius. FS coronal T1-weighted arthrogram. (B) RSL (arrow) extending to the scapholunate interval between the scaphoid (S) and lunate (L). Note the relative volar location of the extrinsic RSL to the intrinsic scapholunate ligament. sl, dorsal and volar portions of the intrinsic scapholunate ligament. FS axial T1-weighted arthrogram. (C) At the level of the distal radius, the normal articular cartilage (AC) ridge between the scaphoid fossa and lunate fossa demonstrates a triangular appearance and is seen in the same plane as the intrinsic scapholunate ligament. This articular cartilage ridge should not be mistaken for a site of ligamentous attachment. Spoiled GRASS (SPGR) coronal image with a 4-cm FOV and 1-mm slice thickness.
|
-
The ulnar arcuate ligament extends from the volar surface of the lunate and triquetrum to the neck of the capitate
P.1690P.1691
and plays a role in preventing the proximal row from volarflexion (see Fig. 10.75). Progressing radially, the substance of this structure becomes quite thin in the region of the capitolunate articulation. -
The radial limb (i.e., radial arcuate ligament) of this V-shaped ligament runs from the capitate to the distal pole of the scaphoid.
 |
|
FIGURE 10.68 ● A coronal section of the wrist joint shows the articular surfaces and triangular cartilage.
|
 |
|
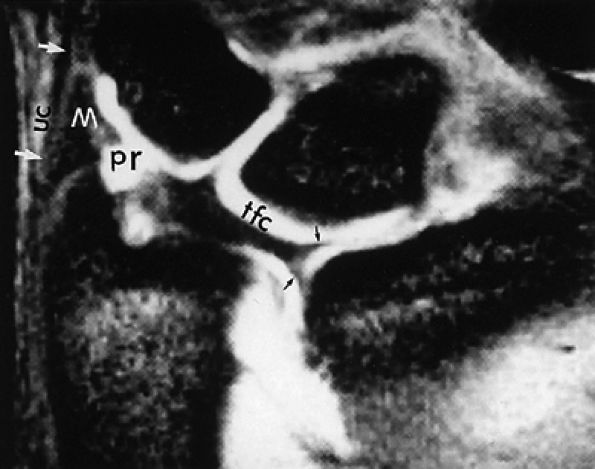
FIGURE 10.69 ● A T2*-weighted image showing the TFC complex. Black arrows, radial attachments of TFC; white arrows and UC, ulnar collateral ligament; M, meniscus homologue; pr, prestyloid recess.
|
-
The superficial palmaris longus tendon is fused to the midline of the flexor retinaculum and expands distally into the palmar aponeurosis.
-
Guyon's canal, a site of potential compression of the ulnar nerve, is formed by an ulnar extension of the flexor retinaculum superficial to the ulnar nerve and artery.
-
The concave volar surface of the carpus and the flexor retinaculum form the anatomic boundaries of the carpal tunnel for passage of the long flexor tendons of the fingers and thumb (Fig. 10.79).
-
The four flexor digitorum superficialis tendons are arranged in two rows, with the tendons to the third (i.e., middle) and fourth (i.e., ring) digits superficial to the tendons for the second (i.e., index) and fifth (i.e., little) digits (Fig. 10.80). After entering their respective fibrous flexor sheaths, the tendons of the flexor digitorum superficialis divide into two halves opposite the proximal phalanx and partially decussate around the flexor digitorum profundus tendons. Distal to the site of perforation by the flexor digitorum profundus, the superficialis tendons pass deep to the flexor digitorum profundus and send slips to attach to the sides of the middle phalanx.
-
The tendons of the flexor digitorum profundus are arranged in the same plane and pass deep to the flexor digitorum superficialis (Fig. 10.81). The tendons of the flexor digitorum profundus attach distally to the base of the terminal phalanx and change from a deep to a superficial location at the partial decussation of the superficialis at the level of the middle phalanx (Fig. 10.82).
 |
|
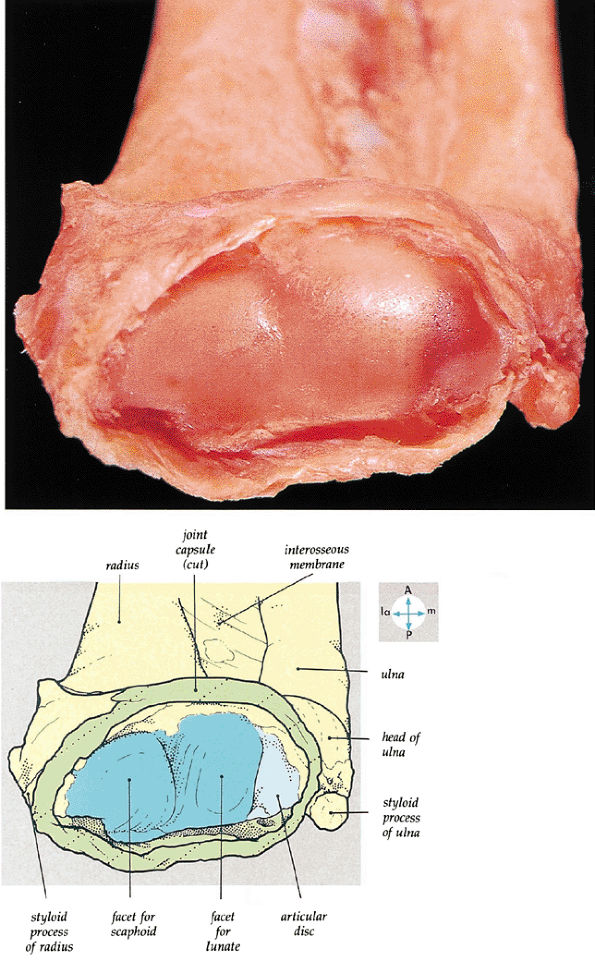
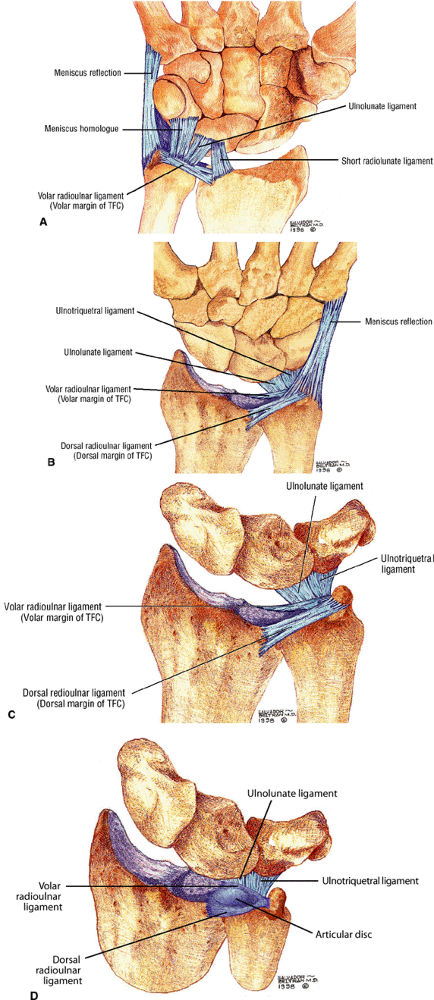
FIGURE 10.70 ● TFC complex. (A) Volar view of the ligaments of the ulnar side of the carpus. The meniscus homologue and meniscus reflection are shown. The meniscus homologue inserts onto the volar surface of the triquetrum. The meniscus homologue shares a common origin from the dorsal ulnar corner of the radius with the TFC. The TFC extends in a volar direction from the meniscus homologue to the base of the ulnar styloid. The ulnolunate component of the ulnocarpal ligament is considered to be part of or a continuation of the short radiolunate ligament. (B) In this dorsal view, the ulnar and dorsal aspect of the TFC complex is invested by a thick ligamentous layer (the meniscus reflection) with proximal attachment to the TFC complex and ulna and distal attachment to the base of the fifth metacarpal. (C, D) The dorsal views of the TFC complex show the dorsal and volar radioulnar ligaments as separate from the articular disc of the TFC. The term TFC refers to the central horizontal articular disc and adjoining volar and dorsal radioulnar ligaments. The term TFC complex refers to the TFC and any additional ulnar ligamentous structures, such as the meniscus homologue, ulnar collateral ligament, subsheath of the extensor carpi ulnaris tendon, and ulnolunate and ulnotriquetral ligaments.
|
 |
|
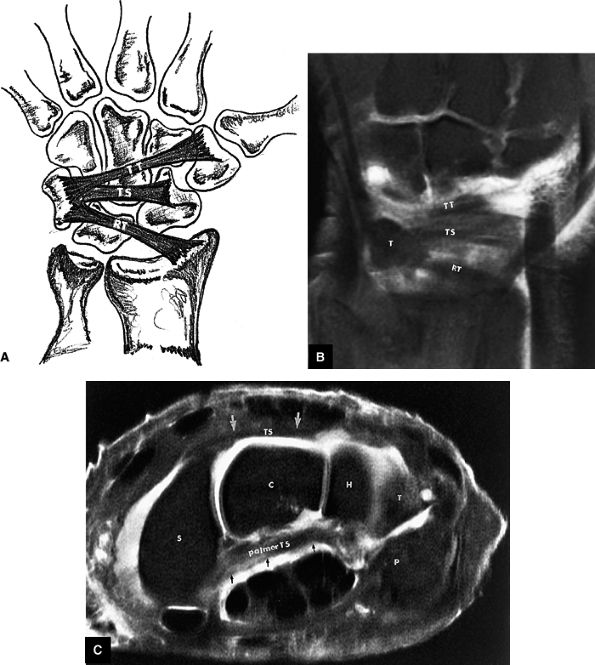
FIGURE 10.71 ● Patterns of the dorsal carpal ligaments. (A) Illustration and (B) corresponding FS T1-weighted coronal image of a single radiotriquetral ligament (RT) and the triquetroscaphoid (TS) and triquetrotrapezial (TT) fascicles of the dorsal intercarpal ligament. T, triquetrum. (C) On an FS PD FSE axial image, the TS fascicle is seen dorsally between the triquetral bone and dorsal pole of the scaphoid (S). The TS fascicle (arrows) extends over the hamate (H) and capitate (C). The palmar TS ligament is also identified at this level (arrows). P, pisiform.
|
 |
|
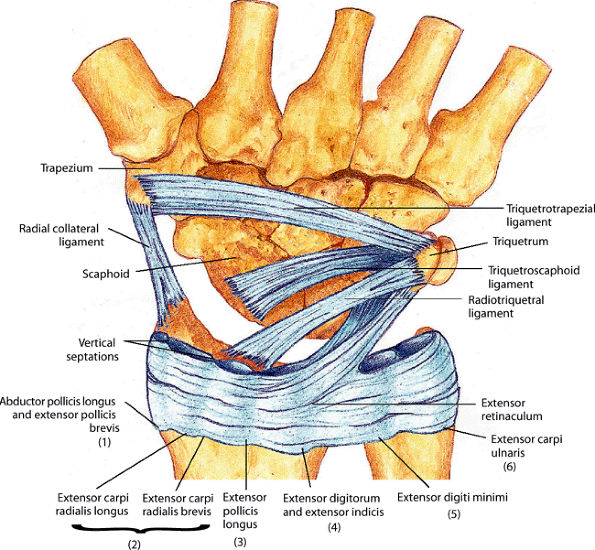
FIGURE 10.72 ● The extensor retinaculum and dorsal carpal ligaments. The radiotriquetral ligament (an extrinsic dorsal capsular ligament) and the dorsal intercarpal ligament (an intrinsic dorsal capsular ligament) are illustrated. The dorsal intercarpal ligament is composed of separate triquetroscaphoid and triquetrotrapezial fascicles. The radial collateral ligament and the bilaminar extensor retinaculum are also shown. The vertical septations of the extensor retinaculum define the six extensor compartments (1-6). A slip of the extensor retinaculum attaches to the dorsal triquetrum.
|
 |
|
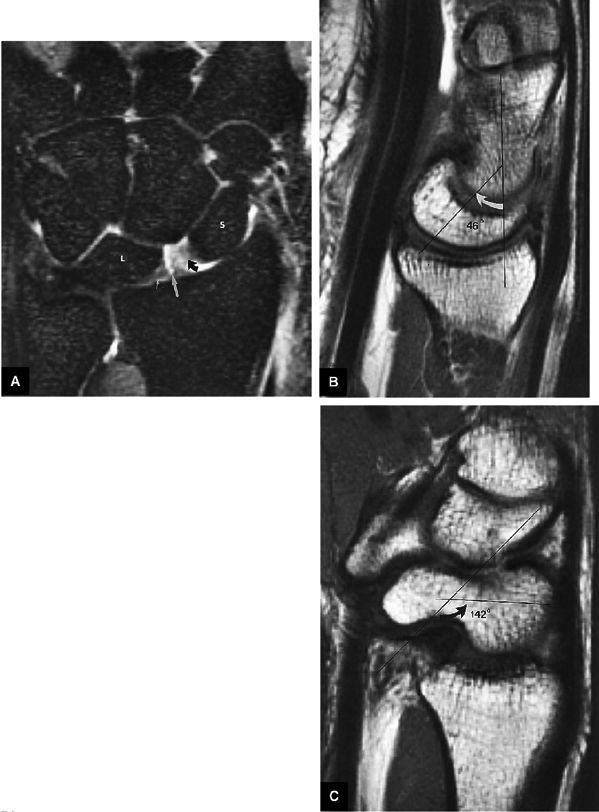
FIGURE 10.73 ● Anatomy of the scapholunate ligament complex on three separate coronal images. (A) Volar component. (B) Membranous component. (C) Dorsal component. (D) On a corresponding axial image all three components of the scapholunate ligament complex are demonstrated. The dorsal scapholunate ligament is horizontally oriented and is perpendicular to the joint. The fibers of the membranous portion of the scapholunate ligament course peripherally and obliquely from the scaphoid downward toward the lunate in a dorsal-to-volar direction. The volar scapholunate ligament courses obliquely from the scaphoid downward to the lunate. This arrangement of scapholunate ligament fibers biomechanically hinges the joint dorsally at the level of the dorsal transverse fibers. In forced extension, scapholunate ligament failure initiates in its volar aspect. S, scaphoid; L, lunate; v, volar component; m, membranous component; d, dorsal component. Arrows correspond to the course of each component of the scapholunate ligament.
|
 |
|
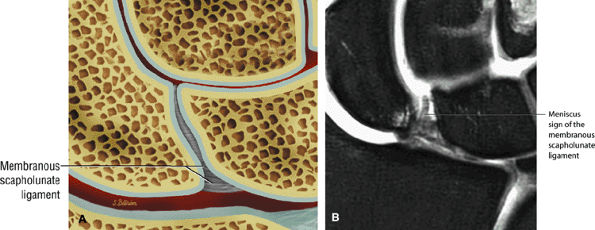
FIGURE 10.74 ● Membranous wedge-shaped component of the scapholunate ligament with direct proximal attachment to the articular surfaces of the scaphoid and lunate. The distal apex is free without direct attachment and presents as a prominent distal protrusion into the scapholunate articulation. (A) Coronal color illustration. (B) Coronal FS PD FSE image.
|
 |
|
FIGURE 10.75 ● The arcuate or deltoid ligament. (A) The ulnar limb (ul) and radial limb (rl) of the volar intrinsic arcuate ligament are shown in the same volar plane on a T1-weighted coronal image. Both limbs attach centrally to the capitate. (B) The arcuate ligament is shown between the capitate (C) and lunate (L) on a midsagittal FS T1-weighted arthrogram. The ulnar limb of the arcuate or deltoid ligament is the capitoscaphoid arm, and the radial limb of the arcuate ligament is the capitotriquetral arm.
|
 |
|
FIGURE 10.76 ● The palmar aponeurosis is revealed by removing the skin and superficial fascia. The investing fascia has been removed proximal to the flexor retinaculum. R, radius.
|
 |
|
FIGURE 10.77 ● The flexor retinaculum and its superficial relations and structures are seen entering the carpal tunnel.
|
-
Carpal instabilities can be grouped as perilunar, midcarpal, or proximal.
-
Perilunar instabilities include lesser arc injuries (primarily ligamentous [e.g., scapholunate or lunotriquetral injuries]) and greater arc injuries (primary osseous [e.g., scaphoid fracture]).
-
Stability refers to the ability of two structures to maintain a normal physiologic spatial relationship under applied physiologic loading.
-
Similarly, two structures are said to be unstable if they cannot maintain this normal relationship under physiologic loading conditions.
 |
|
FIGURE 10.78 ● Flexor retinaculum. The concave volar surface of the carpus and the flexor retinaculum form the anatomic boundaries of the carpal tunnel (for passage of the long flexor tendons of the fingers and thumb). Medially, the flexor retinaculum is attached to the pisiform and hook of the hamate and laterally to the tuberosities of the scaphoid and trapezium. (A) Coronal color illustration (volar perspective). (B) Coronal T1-weighted image at the level of the retinaculum.
|
 |
|
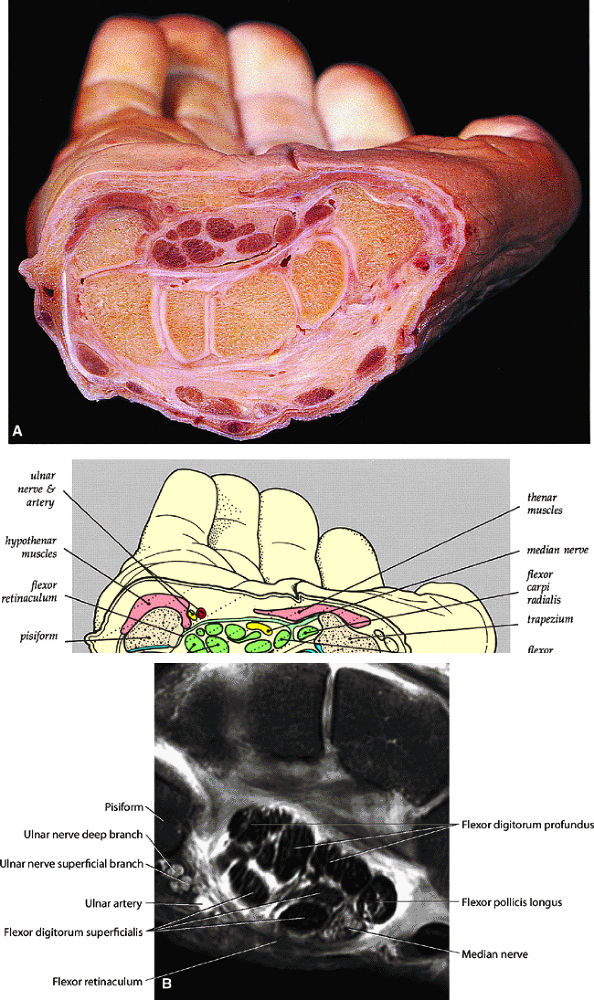
FIGURE 10.79 ● (A) A transverse section through the carpus shows the carpal tunnel and its contents. (B) Axial FS PD FSE high-resolution image of the carpal tunnel.
|
-
A stable equilibrium exists when displacement of a body from its position results in a restoring force that tends to return the body to its equilibrium position. When all of the supporting constraints of the wrist are normal and intact, any load within physiologic limits may change the spatial relationship of the components, but there will be a simultaneous increase in the tension within these constraining structures that counteracts the deforming force and tends to return the components to their normal spatial relationship. Neutral, dorsiflexion, and palmarflexion motions can be used as an example of the different colinear relationships among the capitate, lunate, and radius (Figs. 10.85, 10.86, and 10.87).
-
Conversely, an unstable equilibrium exists when displacement of a body from its position results in a force that tends to push the body further from the equilibrium position.57 This condition occurs in the wrist when the constraining structures are incompetent. Constraining or supporting structures about the wrist include not only the ligamentous structures discussed earlier but also the tendons that cross the joint, as well as the geometry of the carpal bones and their surrounding articular surfaces.
-
With radial deviation the radial border must shorten, and this is accomplished by rotation of the scaphoid into a flexed position.
-
The ulnar border is lengthened as the triquetrum slides out from beneath the hamate.
-
On plain radiographs or coronal MR images in this position, the scaphoid is foreshortened and the joint space is evident between the hamate and the triquetrum; no superimposition of these bones occurs.
-
The lunate is linked or associated with the scaphoid and triquetrum through the interosseous ligaments, which are displayed as homogeneous hypointense structures on coronal MR images. The scapholunate ligament has a triangular morphology, whereas the lunotriquetral ligament is more linear in shape. Lunate motion is thus a reflection of this proximal carpal row linkage, as well as the compressive forces placed on it by the capitate.
-
At extreme radial deviation, the summation of these forces produces slight volarflexion of the lunate. Since the wrist is in a condition of stable equilibrium, the bones of the proximal carpal row return to their neutral position when the force causing radial deviation is removed. Thus, in radial deviation, a flexion torque predominates, and compression of the scaphotrapeziotrapezoid joint and proximal carpal row flexion produce a physiologic VISI pattern.
-
With ulnar deviation, the radial side of the flexible spacer must lengthen and the ulnar side must shorten.
-
The scaphoid becomes more horizontal or extended to lengthen the radial side, and the triquetrum slides beneath the hamate to shorten the ulnar side.
-
PA radiographs show an elongated scaphoid and superimposition of the hamate on the triquetrum.
-
Coronal MR images demonstrate the triquetral movement in an ulnar direction on the slope of the hamate.
-
Palmar movement of the triquetrum in relationship to the hamate results in a palmar position of the lunate axis, relative to the capitate.
-
Compression forces transmitted by the capitate produce dorsal rotation or dorsiflexion of the lunate. Associated volar shift of the lunate maintains colinear alignment of the capitate and radius.
-
During lunate dorsiflexion, there is elevation of the distal pole of the scaphoid (i.e., scaphoid extension). Thus, in ulnar deviation, an extension torque predominates, and interaction at the triquetrohamate helicoid slope and proximal carpal row extension produces a physiologic DISI pattern.
 |
|
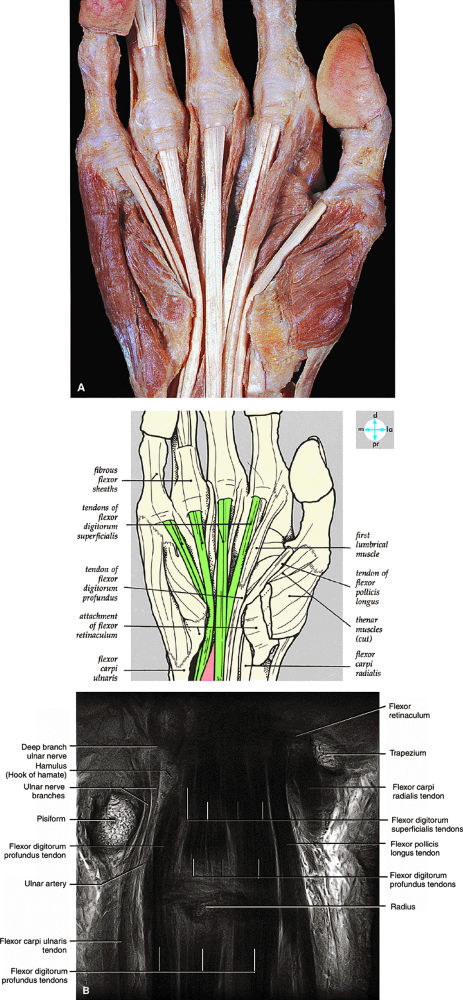
FIGURE 10.80 ● (A) The palmar aponeurosis, flexor retinaculum, investing fascia, and palmar vessels and nerves have been removed to reveal the tendons of the flexor digitorum superficialis in the palm. (B) Coronal T1-weighted image at the level of the flexor tendons.
|
of both scapholunate and lunotriquetral ligament pathology. MR imaging is superior to conventional arthrography, allowing identification of the size, morphology, and location of a scapholunate or lunotriquetral ligament tear. This information is important because communication across a pinhole or small perforation or deficiency of the thin membranous portion of the ligament may not be significant in the presence of grossly intact dorsal and volar ligaments. In fact, evaluations of communicating perforations in cadaver wrists have shown that 28% of cadaver wrists have degenerative perforations of the central membranous scapholunate ligament.59 Degenerative perforations of the membranous lunotriquetral ligament can be seen in 36% of cadaver wrists. In our experience, degenerative perforations occur twice as often in the lunotriquetral ligament as in the scapholunate ligament.
 |
|
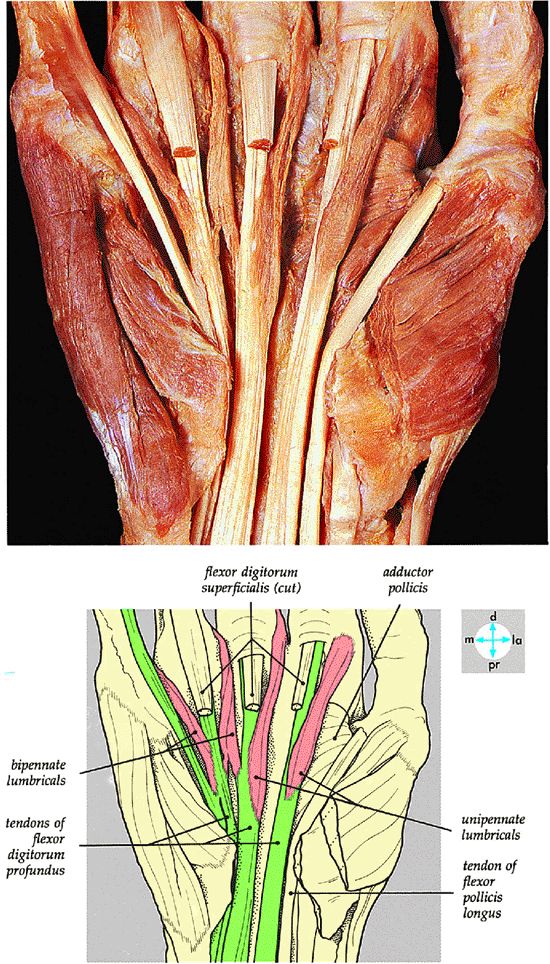
FIGURE 10.81 ● Removal of the tendons of the flexor digitorum superficialis reveals the attachments of the lumbrical muscles to the tendons of the flexor digitorum profundus.
|
 |
|
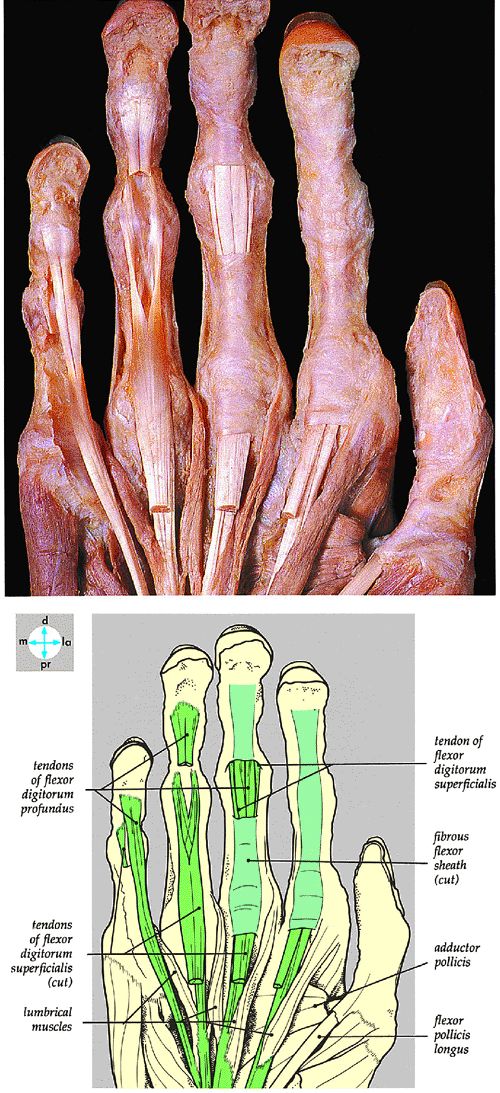
FIGURE 10.82 ● Partial cutting away of the fibrous flexor sheath of the middle finger exposes the tendons of the flexor digitorum superficialis and profundus, revealing the phalangeal attachments in the ring and little fingers.
|
 |
|
FIGURE 10.83 ● (A) The extensor tendons are arranged into six compartments on the dorsum of the wrist. (B, C) Extensor tendon anatomy on T1-weighted coronal MR images (A is dorsal to B).
|
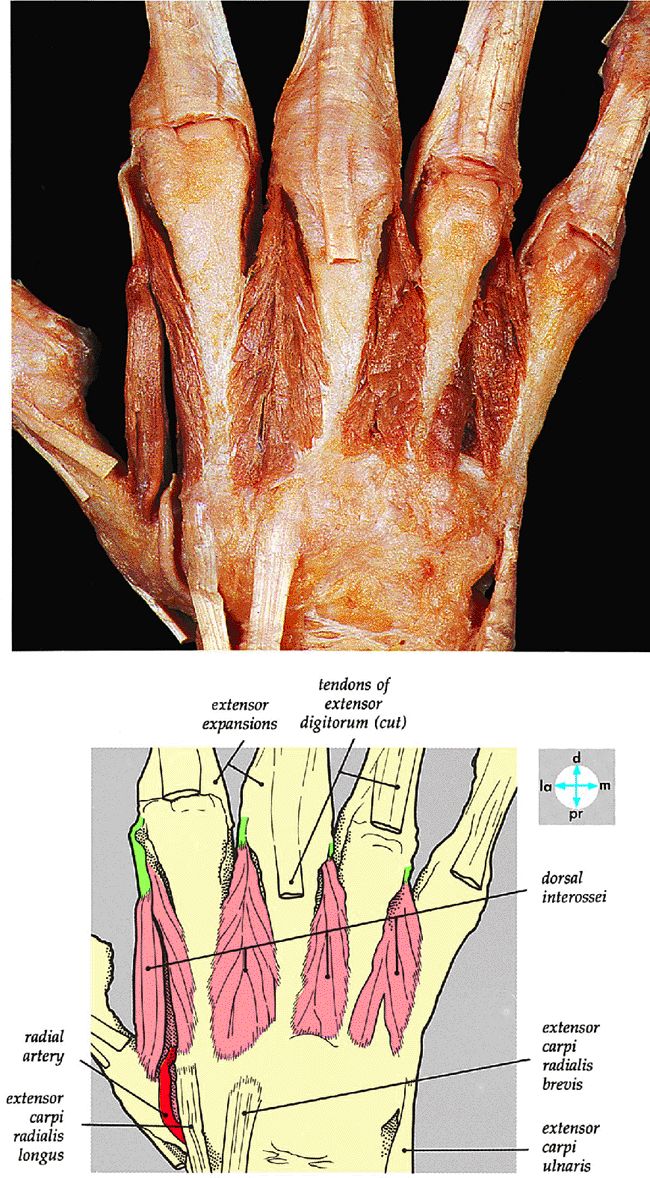 |
|
FIGURE 10.84 ● The dorsal interossei is exposed by removing the deep fascia and the tendons of the extensor digitorum.
|
 |
|
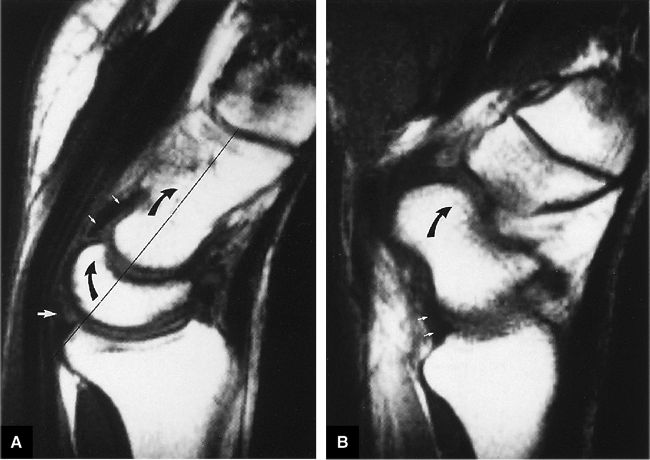
FIGURE 10.85 ● (A) In wrist dorsiflexion, there is colinear alignment (long thin black line) of the dorsiflexed capitate and lunate (curved arrows). The deltoid or arcuate ligament (small white arrows) and the radiolunate (short radiolunate) ligament (large white arrow) are also indicated. Dorsiflexion occurs primarily at the radiocarpal joint. (B) The radioscaphocapitate ligament (small white arrows) also tightens during wrist dorsiflexion, locking any motion between the proximal and distal carpal rows and creating a sling across the waist of the scaphoid. Both the scaphoid (curved arrow) and capitate are thus dorsiflexed.
|
 |
|
FIGURE 10.86 ● (A) With the wrist in a neutral position, there is normal colinear alignment of the capitate, lunate, and radius (black line). The normal capitolunate angle is between 0° and 30°. (B) When the scaphoid is positioned without dorsiflexion or palmarflexion, the normal scapholunate angle is between 30° and 60°.
|
 |
|
FIGURE 10.87 ● (A) Palmarflexion occurs primarily at the midcarpal articulation. Palmar flexion of the capitate (long curved arrow) and some palmar flexion of the lunate (short curved arrow) can be seen. The arcuate or deltoid ligament (small white arrows) is more lax. Large white arrow, radiolunate articulation. (B) Flexion of the scaphoid (curved arrow) with a lax radioscaphocapitate ligament (straight arrows).
|
 |
|
FIGURE 10.88 ● Scapholunate ligament tear without carpal instability. (A) FS T1-weighted coronal image demonstrates a vertical high-signal-intensity tear (arrow) of the lunate attachment of the scapholunate ligament. The lunotriquetral ligament is absent. (B) Corresponding FS T1-weighted sagittal image demonstrates colinear (straight line) alignment of the capitate (C) and lunate (L) with a normal capitolunate angle. There is no static instability pattern.
|
-
Scaphotrapezial ligament
-
A thin palmar scaphotrapeziotrapezoid capsule/thick fibrous floor of the flexor carpi radialis tendon sheath
-
Scaphocapitate capsular ligament
-
Dorsal capsular ligament (minimal contribution to stability).
-
All three components of the scapholunate ligament should be evaluated on coronal and axial images.
-
Dorsal component scapholunate ligament tears are more likely to be symptomatic.
-
Scapholunate ligament failure represents stage I perilunar instability.
 |
|
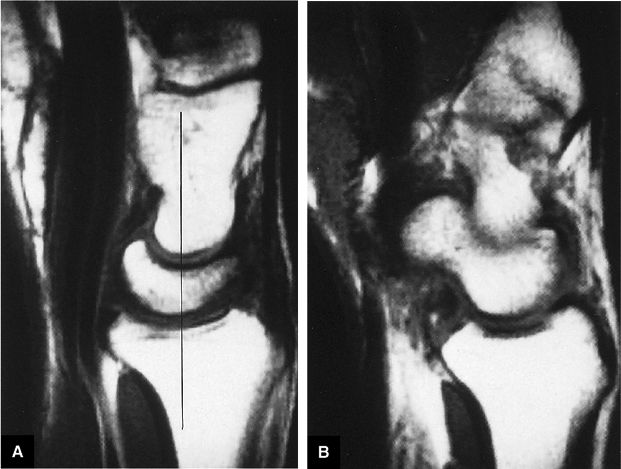
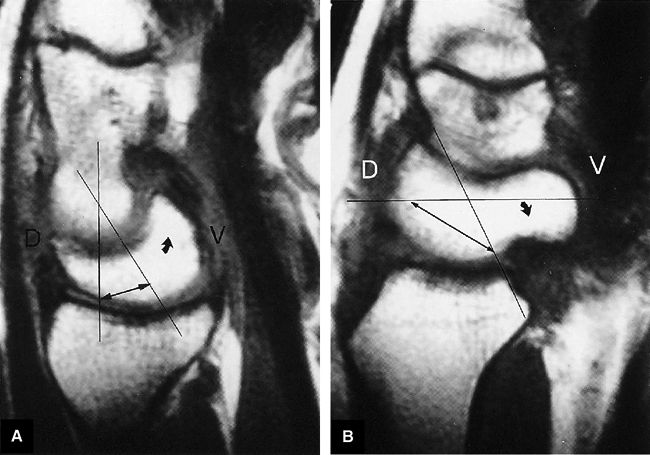
FIGURE 10.89 ● (A) DISI with dorsal tilting of the lunate (curved arrow) without volar shift. Note the dorsal displacement of the capitate relative to the radius. The capitolunate angle (double-headed arrow) measures 32°. (B) Palmar tilting of the scaphoid (curved arrow) causes an abnormally increased scapholunate angle (double-headed arrow) of 124°. D, dorsal; V, volar.
|
-
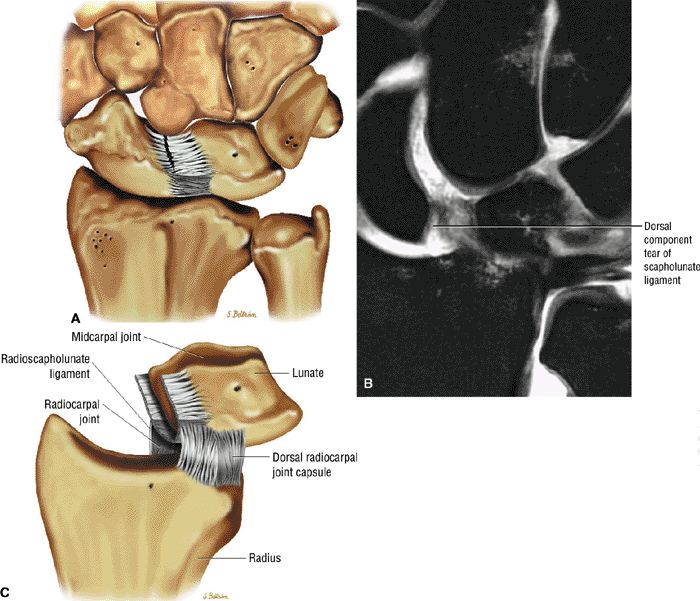
Disruption of the scapholunate ligament is shown on T2*-weighted or STIR images as either complete ligamentous disruption or as a discrete area of linear hyperintensity in a partial or complete tear (Fig. 10.90).
-
In complete tears, synovial fluid communication between the radiocarpal and midcarpal compartments may be identified. Associated stretching (i.e., redundancy) or tearing of the radiolunate ligament and the radioscaphocapitate ligament is shown on sagittal images.
-
A flap tear may not be appreciated without the use of MR arthrography. MR arthrography is also helpful in evaluation of perforations and integrity of the dorsal component of the scapholunate ligament.
-
A perforation, identified by communication of fluid across a focal discontinuity, constitutes a communicating defect or tear. Small membranous perforations may exist in the presence of intact dorsal and volar portions of the scapholunate ligament. In fact, most degenerative perforations occur in the thin membranous portion of the scapholunate ligament, which is not thought to be biomechanically significant.59,60
-
Partial-thickness perforations or noncommunicating defects may be associated with ligamentous tissue degeneration or sprains and may be difficult to appreciate on MR images.61
-
A complete scapholunate ligament tear may not be associated with scapholunate interval diastasis or static carpal instability as assessed on sagittal images, especially when the volar extrinsic ligaments are intact.
-
Axial MR images are used to distinguish among tears of the dorsal, membranous, and volar portions of the scapholunate ligament. The location of the tear can then be directly correlated with dorsal or volar coronal images.
-
The scaphoid attachment of the scapholunate ligament is more likely to avulse than is the stronger lunate attachment.59 The insertion of the scapholunate ligament into hyaline cartilage covering the scaphoid is thus relatively weak. In fact, a scapholunate ligament
P.1713P.1714
tear may be associated with a scaphoid avulsion fracture (Fig. 10.91). -
Potential sites of injury of the intrinsic scapholunate ligament complex (the scapholunate interosseous ligament) (Fig. 10.92) include its dorsal component (an important key stabilizer), a membranous component, and a volar component.
-
Less frequently injured is the extrinsic radiocarpal ligament complex, composed of the radioscaphocapitate, the long radiolunate (radiolunotriquetral), the short radiolunate, and the radioscapholunate (ligament of Testut). Associated synovitis, ganglions, or ligamentous hyperintensity may be seen in trauma.
-
The size of the tear varies depending on associated osseous or ligamentous disruption of major carpal links; the scaphotrapeziotrapezoid is the radial link and the triquetrohamate is the ulnar link.
-
Acute injuries (less than 6 weeks) may be classified as either stable injuries (partial ligament disruption) (Fig. 10.93) or dynamic or static unstable injuries (complete ligament disruption) (Fig. 10.94).
-
Chronic injuries are considered to be stable, unstable, or fixed. They are associated with a variety of secondary changes, including capsular contractures, degenerative arthritis, pancarpal arthrosis, intercarpal collapse, and SLAC wrist (progressive proximal capitate migration, radioscaphoid and capitolunate arthrosis in untreated scapholunate dissociation). DISI deformity with midcarpal collapse may also be seen.
-
The scaphoid attachment of the scapholunate ligament has fewer Sharpey's fibers than the lunate attachment and is therefore more susceptible to tearing (Fig. 10.95).
 |
|
FIGURE 10.90 ● Scapholunate ligament tear with DISI. (A) Traumatic avulsion of the lunate aspect of the scapholunate ligament on a fast STIR coronal image. The scapholunate interval is widened with direct extension of fluid filling the tear site (large straight arrow). Ligament fibers are still attached to the radial aspect of the lunate (small straight arrow). Morphology is amorphous at the avulsed scaphoid remnant (curved arrow). (B) The capitolunate angle (arrow) is increased to 46°, and there is associated dorsal tilting of the lunate. (C) The scaphoid tilts palmarly with an increased scapholunate angle (arrow) of 142°.
|
-
Dissociation (Fig. 10.96), indicated by an increased scapholunate gap (more than 3 mm), comparable to the Terry Thomas sign on radiography
-
Volar or palmar flexion of the scaphoid on sagittal images (Fig. 10.97)
-
DISI with dorsal tilting of lunate, an increased capito-lunate angle (more than 30°), and an increased scapho-lunate angle (more than 80°) (Fig. 10.98)
-
Linear signal in a partial or complete tear
-
Complete ligamentous disruption with a fluid-filled gap and synovial fluid communication between the radiocarpal and midcarpal compartments
-
Disruption of the dorsal component of the scapholunate ligament
-
Associated synovitis of the extrinsic volar radiocarpal ligaments
-
Degenerative perforations in the membranous portion with intact volar and dorsal components (Fig. 10.99)
-
Associated dorsal ganglions in the dorsal or dorsal/membranous scapholunate ligament pathology (Fig. 10.100).
 |
|
FIGURE 10.91 ● (A) T1-weighted and (B) STIR coronal images of a chronic avulsion fracture of the ulnar aspect of the scaphoid. The scapholunate ligament (straight arrow) is still attached to both the lunate and the surface of displaced scaphoid fracture fragment (curved arrow). S, scaphoid; L, lunate.
|
 |
|
FIGURE 10.92 ● The scapholunate ligament forms a C-shaped complex, which is open distally at the level of the midcarpal joint. The membranous or proximal component forms the base of this C-shaped complex. The dorsal radiocarpal joint capsule inserts proximally into the dorsal component. The proximal aspect of the dorsal and volar components merges with the membranous component. Volarly, the radioscapholunate ligament inserts at the junction of the volar and membranous components of the scapholunate ligament.
|
 |
|
FIGURE 10.93 ● Dorsal fiber disruption of the scapholunate ligament on color illustration (A) and coronal FS PD FSE image (B). Tearing of the strong dorsal fibers is frequently associated with either degeneration or tears of the membranous component. (C) Normal dorsal scapholunate ligament fibers shown for comparison.
|
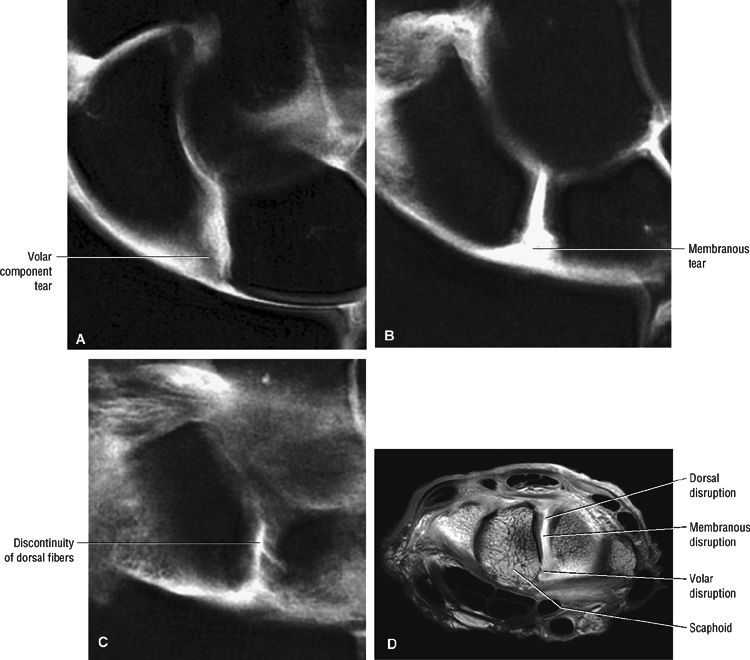 |
|
FIGURE 10.94 ● Coronal FS PD FSE images showing complete disruption of the volar (A), membranous (B), and dorsal (C) components of the scapholunate (SL) ligament. (D) A corresponding axial T1-weighted arthrogram demonstrates lack of scapholunate ligament fibers from the dorsal to volar aspects of the interval.
|
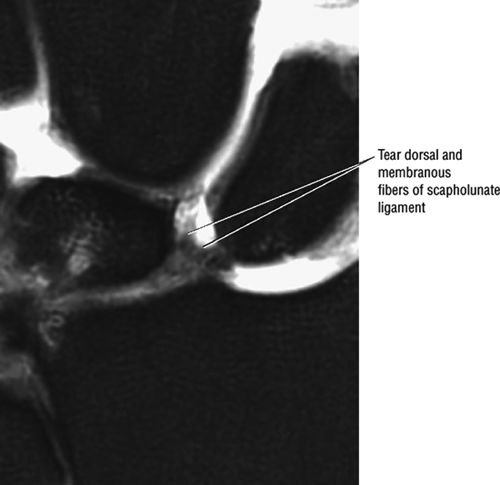 |
|
FIGURE 10.95 ● Preferential disruption of the dorsal and membranous scapholunate ligament from the scaphoid, which has a weaker attachment to the interosseus ligament. Coronal FS PD FSE image.
|
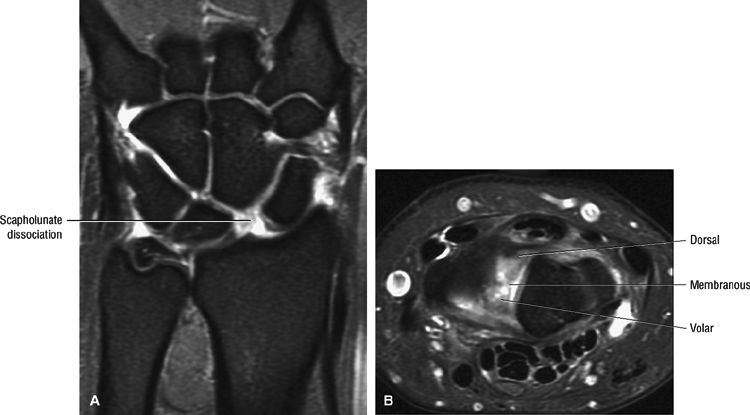 |
|
FIGURE 10.96 ● Scapholunate (SL) dissociation (A) associated with disruption of all three components of the scapholunate ligament. (B). (A) Coronal FS PD FSE image. (B) Axial FS PD FSE image.
|
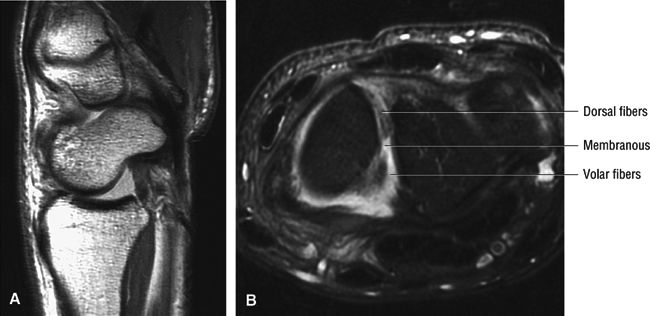 |
|
FIGURE 10.97 ● Scaphoid flexion (A) associated with disruption of the dorsal, membranous, and volar fibers of the scapholunate ligament (B). (A) Sagittal T1-weighted image. (B) Axial FS PD FSE image.
|
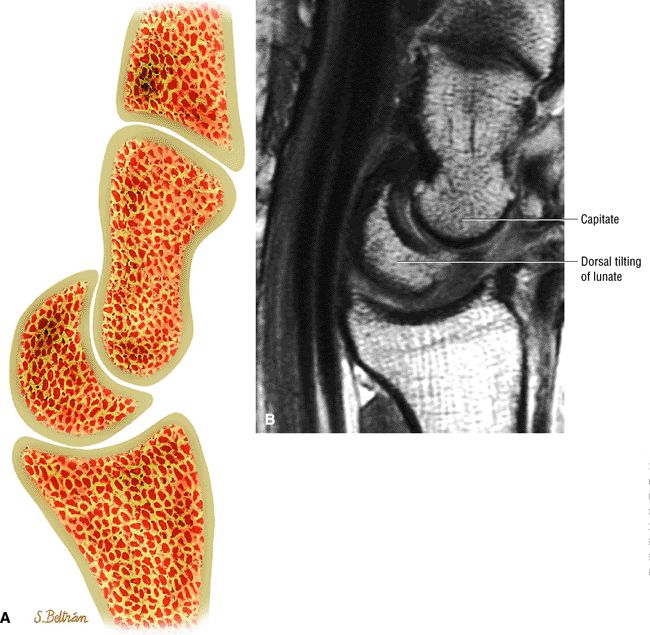 |
|
FIGURE 10.98 ● DISI deformity with lunate extension or dorsal tilting of the lunate and proximal movement of the capitate. DISI deformity is characterized by a scapholunate angle greater than 70°, a capitolunate angle greater than 20°, and a dorsiflexed and volarly displaced lunate. DISI deformity is not pathognomonic for scapholunate instability and can be associated with unstable scaphoid fractures (bony DISI), distal radius fractures (compensatory DISI), radius malunion (adaptive DISI), and capsular/ligamentous pathology, including scapholunate instability (ligamentous DISI). (A) Lateral graphic of DISI with dorsal tilting of the lunate. (B) Corresponding T1-weighted sagittal image of DISI with the concave surface of the lunate directed dorsally with proximal shift of the capitate.
|
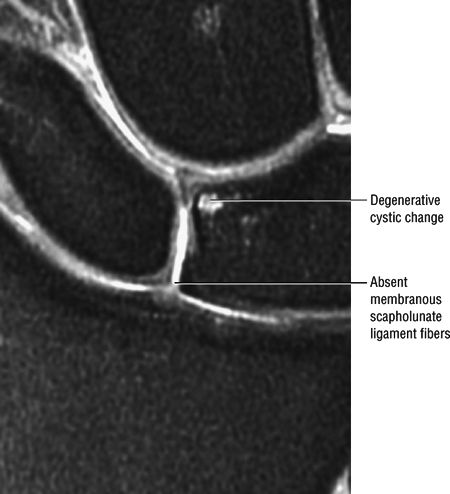 |
|
FIGURE 10.99 ● Absence of membranous fibers of the scapho-lunate ligament allows direct extension of fluid from the radiocarpal joint. Coronal FS PD FSE image.
|
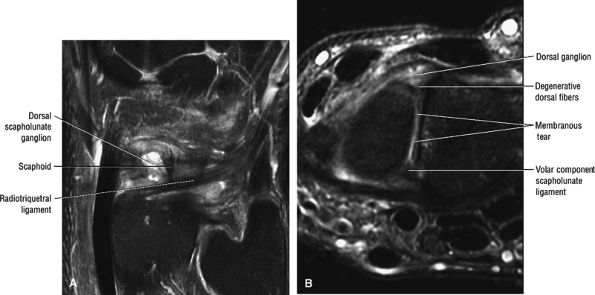 |
|
FIGURE 10.100 ● Dorsal ganglion communicating with a tear of the membranous scapholunate ligament with herniation of fluid through the dorsal scapholunate ligament fibers. (A) Coronal FS PD FSE image. (B) Axial FS PD FSE image.
|
-
Stage I: scapholunate failure
-
Stage I: capitolunate failure
-
Stage III: triquetrolunate failure
-
Stage IV: dorsal radiocarpal ligament failure with volar rotation of the lunate
-
Lunotriquetral tears may be associated with ulnocarpal impaction syndrome.
-
The carpal arc offset between the triquetrum and lunate should be assessed.
-
Lunotriquetral ligament injury occurs as part of stage III PLI, which includes triquetral dislocation and radiotriquetral ligament failure.
associated TFC complex lesions, and associated chondral lesions of proximal lunate, triquetrum, and distal ulna in cases of positive ulnar variance. Improved visualization of radiocarpal and midcarpal communication is also afforded by these sequences.
-
Disruption of the lunotriquetral ligament is most frequently identified by a fluid-filled gap on coronal images (Fig. 10.101).
-
An insertional site tear or perforation is often appreciated on MR arthrography. FS PD FSE sequences provide sufficient contrast to produce an arthrogram-like effect without injection of contrast (Fig. 10.102).
-
Lunotriquetral ligament tears may be associated with TFC degenerative tears.43
-
A VISI pattern usually requires disruption of both the lunotriquetral intrinsic and dorsal extrinsic ligaments (i.e., dorsal radiocarpal ligament).
-
Smith and Snearly53 described the intact lunotriquetral ligament as linear in 63% and delta-shaped in 35% of asymptomatic individuals (Fig. 10.103).
-
The intact lunotriquetral ligament demonstrates homogeneous hypointensity in 73% and linear intermediate signal intensity within its substance in 25% of wrists studied.53 Insertional signal intensity varies with the distribution of hyaline articular cartilage on either side of the lunotriquetral ligament.
-
Asymmetric hyaline articular cartilage signal intensity should not be mistaken for an eccentric tear unless fluid signal intensity communication is seen across the ligament cartilage interface. Linear fluid signal intensity communicating between the radiocarpal and midcarpal compartments through lunotriquetral space indicates tearing.
-
Sagittal MR images are used to assess static VISI instability with palmar tilting of the lunate and scaphoid (Fig. 10.104).
-
There may be discontinuity of the normal lunotriquetral ligament across the lunotriquetral interval (Fig. 10.105)
-
All lunotriquetral ligament components may be affected (Fig. 10.106), including the dorsal, membranous, and volar components.
-
The size of the tear varies based on associated injuries, including distal radioulnar joint subluxation and arthritis, chondromalacia of the distal ulna, TFC complex injury, and triquetrohamate instability.
-
There may be flap tears at the triquetral attachment or complete absence of the horseshoe-shaped ligament (Fig. 10.107).
-
Loss of the normal smooth convexity of the proximal carpal row is not uncommon.
-
Disruption of the lunotriquetral interval is pronounced with ulnar deviation.
-
There may be dorsiflexion of the triquetrum relative to the lunate on sagittal images.
-
On coronal images, triquetral offset may be distal relative to the lunate convexity.
-
An increased distance between the lunate and the triquetrum is sometimes seen, although it is not common (Fig. 10.108).
-
Extension of fluid is possible with membranous degeneration but intact dorsal and volar lunotriquetral ligament components.
-
The scapholunate angle is less than 30° to 40° and the capitolunate angle is greater than 10°.
-
Associated findings of ulnocarpal (ulnolunate) impaction are frequently seen with lunotriquetral ligament tears (Fig. 10.109).
-
Ganglions (Fig. 10.110) are less commonly associated with lunotriquetral ligament tears than with scapholunate ligament injury.
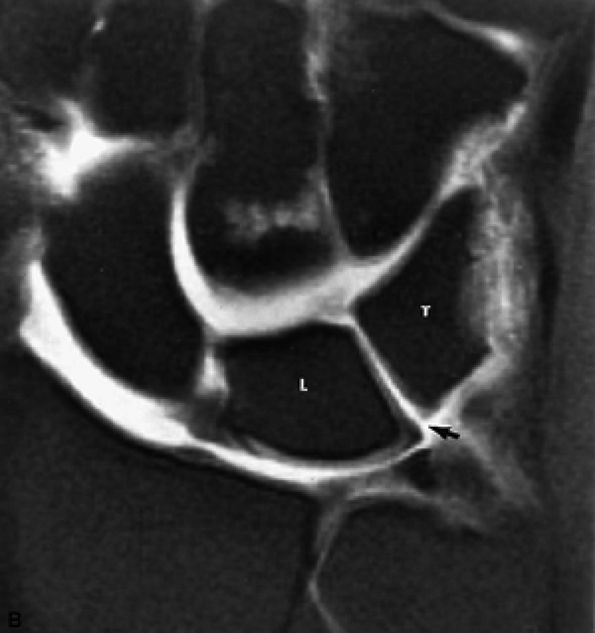 |
|
FIGURE 10.101 ● Tear with absence of the lunotriquetral ligaments (arrow) on FS T1-weighted arthrograms. The lunotriquetral ligament tear could be missed by using only gradient-echo sequence. L, lunate; T, triquetrum.
|
often diagnosed in radiographs taken for other reasons. However, achieving a stable lunotriquetral fusion has proven difficult, and most series show significant rates of nonunion (i.e., up to 40%). Techniques using larger bone grafts and compression fixation devices have improved the success of this procedure. We have had 100% success in achieving fusion using the Herbert bone screw with precompression of the fusion site.
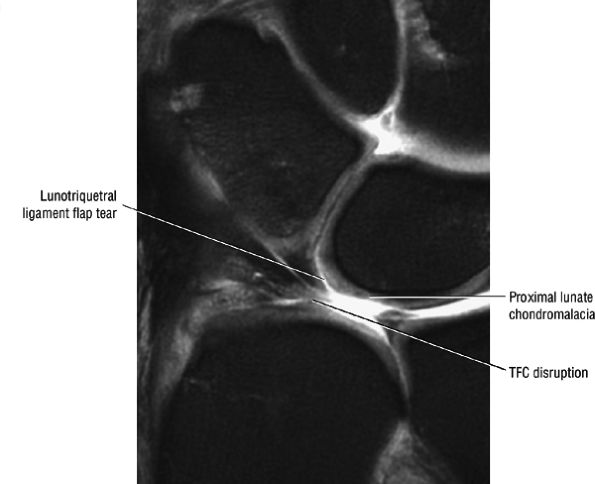 |
|
FIGURE 10.102 ● Flap tear of the lunotriquetral ligament associated with TFC tear and proximal lunate chondromalacia. Coronal FS PD FSE image.
|
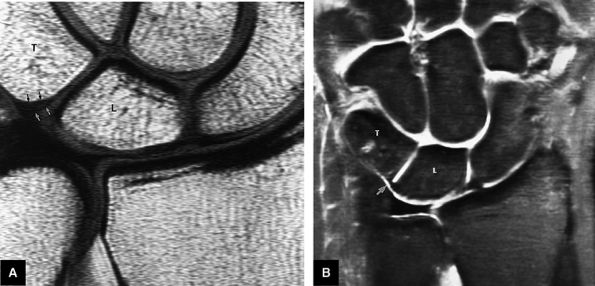 |
|
FIGURE 10.103 ● Normal variants of the lunotriquetral interosseous ligament. (A) Eccentric ulnar position of the delta-shaped lunotriquetral ligament with intermediate-signal-intensity hyaline cartilage seen on the lunate insertion (white arrows) of the ligament. There is direct contact between the lunotriquetral ligament and the low-signal-intensity cortex of the triquetrum (black arrows). (B) Commonly seen linear morphology of the lunotriquetral ligament (arrow). There is no hyaline cartilage signal intensity at the insertion sites of the ligament. T, triquetrum; L, lunate.
|
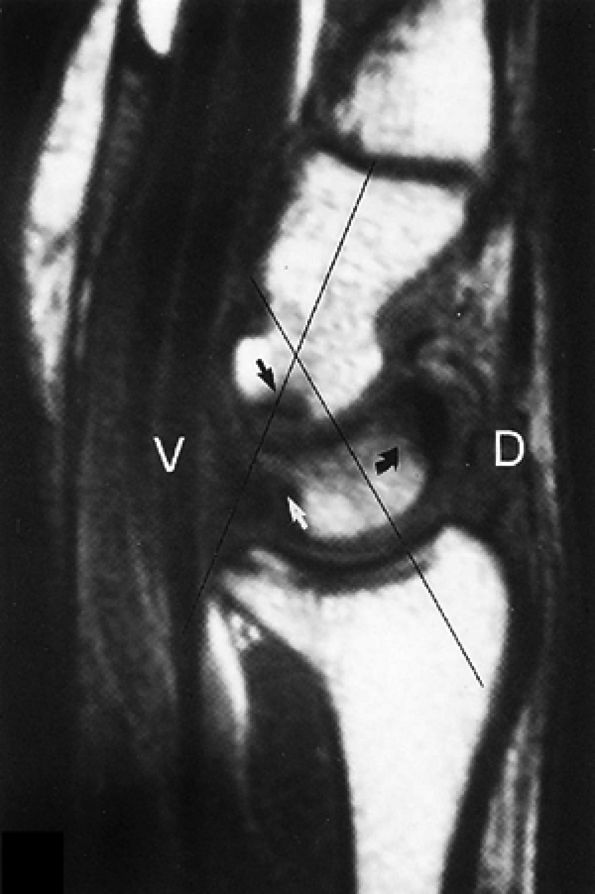 |
|
FIGURE 10.104 ● A VISI pattern is apparent in clinical midcarpal instability. This sagittal T1-weighted image shows the volar tilt of the lunate (curved black arrow), increased capitolunate angle, and subchondral sclerosis of the opposing surfaces of the capitate (straight black arrow) and lunate (white arrow). The ulnar arm of the arcuate ligament is not visible in midcarpal instability. MR imaging was the first modality able to document degeneration of the proximal pole of the capitate in subluxation of the capitate on the lunate.
|
-
Severity (categorized as dynamic, static subluxation, or static dislocation)
-
Direction of displacement: dorsal (DISI), volar (VISI), or radioulnar/proximodistal translation (e.g., ulnar, radial, distal, proximal)
-
Location of injury
-
Type of injury
-
Lesser arc injuries involve scapholunate ligament, lunotriquetral ligament, and complete perilunate instabilities.
-
Greater arc injuries are divided into scaphoid fractures, naviculocapitate syndrome (scaphoid fracture plus perilunate dislocation), and transscaphoid transtriquetral perilunate dislocation.
-
Stage I: The scapholunate ligament fails, leading to an scapholunate ligament instability.
-
Stage II: There is progression to failure of the midportion of the radioscaphocapitate ligament.
-
Stage III: There is failure of the capitolunate and triquetrolunate joints with failure of the radiotriquetral ligaments.
-
Stage IV: There is failure of the dorsal radioscapho-lunotriquetral ligament, resulting in complete palmar dislocation of the lunate.
as the wrist moves into ulnar deviation. This instability is due to a congenital or acquired laxity of the ulnar arm of the volar arcuate ligament. This is a true transverse laxity, as all of the instability occurs between the proximal and distal rows. This subluxation/relocation can be prevented by a dorsally directed force on the pisiform, which reduces the static VISI of the proximal row. On cine films, the proximal carpal row suddenly snaps from a volar-flexed position to a dorsal or neutral position. This movement is in contrast to the smooth, fluid transition seen in the normal wrist. Dorsal midcarpal instabilities are most commonly seen after malunion of a distal radius fracture that leaves the distal radius articular surface in a dorsiflexed position. Correction with an osteotomy of the distal radius restores the normal volar tilt.
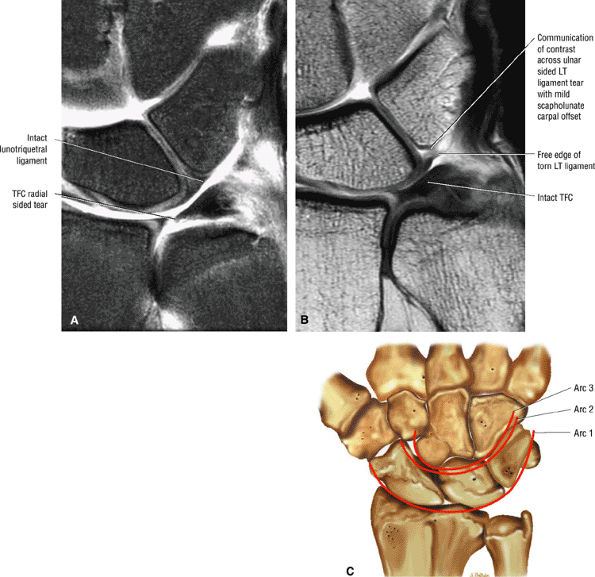 |
|
FIGURE 10.105 ● Comparison of normal intact lunotriquetral ligament (A) with an ulnar-sided lunotriquetral ligament tear at the triquetral attachment (B). (C) Normal congruity of carpal arcs. Arc 1 connects the proximal articular surfaces of the scaphoid, lunate, and triquetrum. Arc 2 connects the distal concave surfaces of the scaphoid, lunate, and triquetrum. Arc 3 outlines the proximal convexity of the capitate and hamate. (A) Coronal FS PD FSE image. (B) Coronal T1-weighted arthrogram. (C) Coronal color illustration.
|
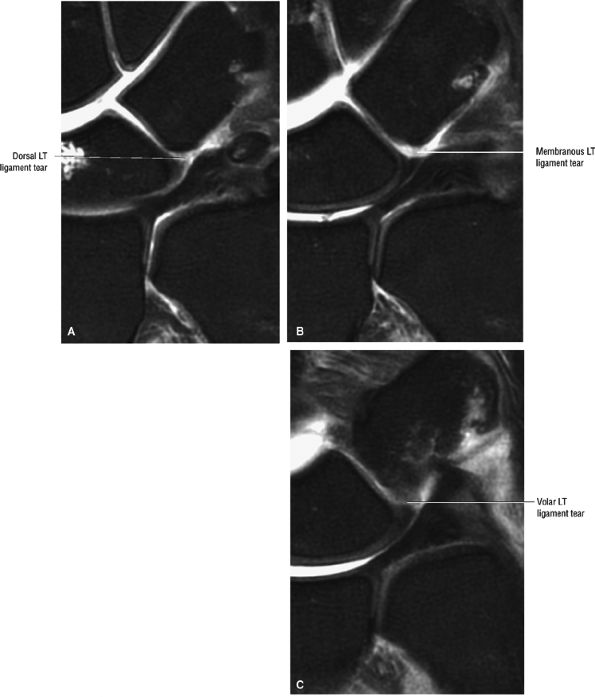 |
|
FIGURE 10.106 ● Coronal FS PD FSE images showing tear of the dorsal (A), membranous (B), and volar (C) components of the lunotriquetral (LT) ligament. Offset of the normally congruous lunatotriquetral arc (B) is a secondary sign of lunotriquetral ligament tear and instability.
|
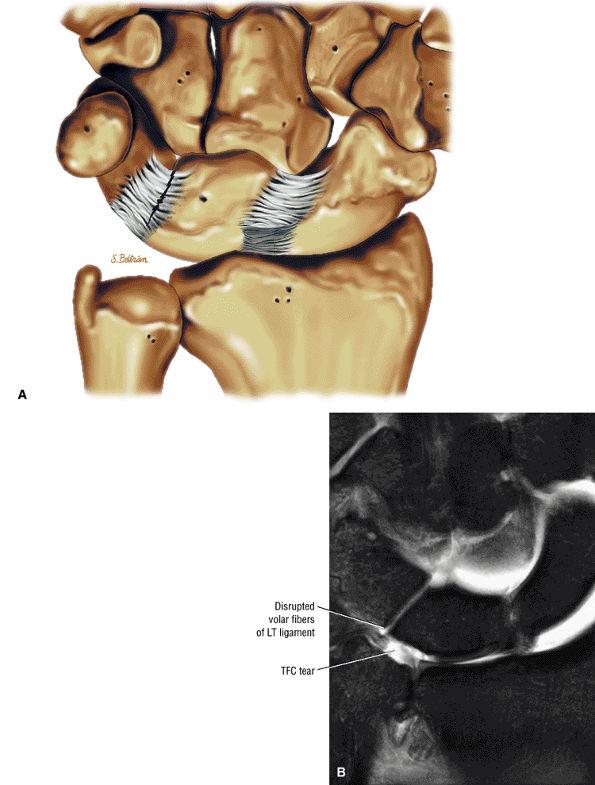 |
|
FIGURE 10.107 ● Volar component tear of the lunotriquetral (LT) ligament. (A) Coronal color illustration. (B) Coronal FS PD FSE image.
|
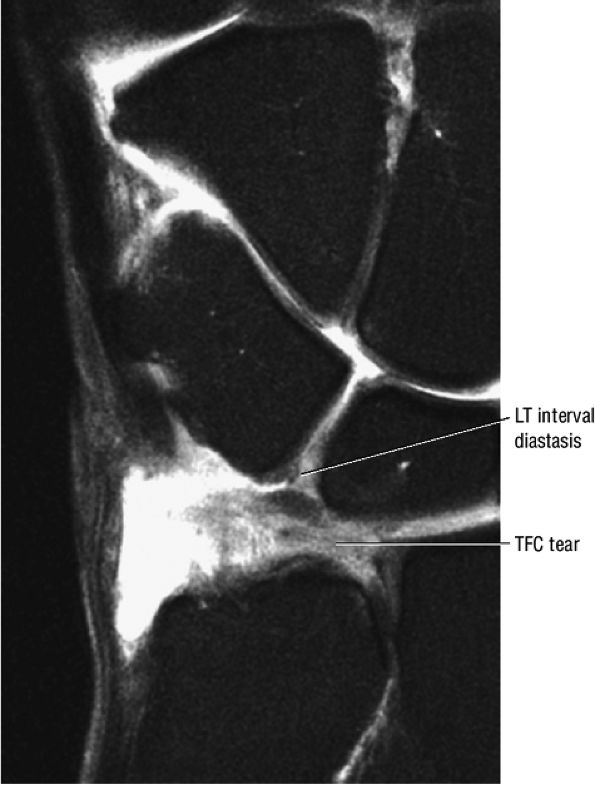 |
|
FIGURE 10.108 ● Lunotriquetral (LT) ligament diastasis associated with lunotriquetral ligament and TFC disruption. Coronal FS PD FSE image.
|
-
Ulnar translocation of the carpus (secondary to rheumatoid disease or trauma, or iatrogenically introduced by excision of the ulnar head or radial styloid)
-
Dorsal instability (secondary to a dorsal rim distal radial fracture'a dorsal Barton's fracture)
-
Palmar instability (secondary to a volar rim distal radial fracture'a volar Barton's fracture)
no longer move together.65 There are three major types of injuries:
-
Carpal instabilities, dissociative are injuries affecting intracapsular intercarpal ligaments, as described in the earlier examples.
-
Carpal instabilities, nondissociative are injuries involving the capsular ligaments with no dissociation of the carpal bones themselves.
-
Complex carpal instabilities are injuries that involve both dissociative and nondissociative elements.
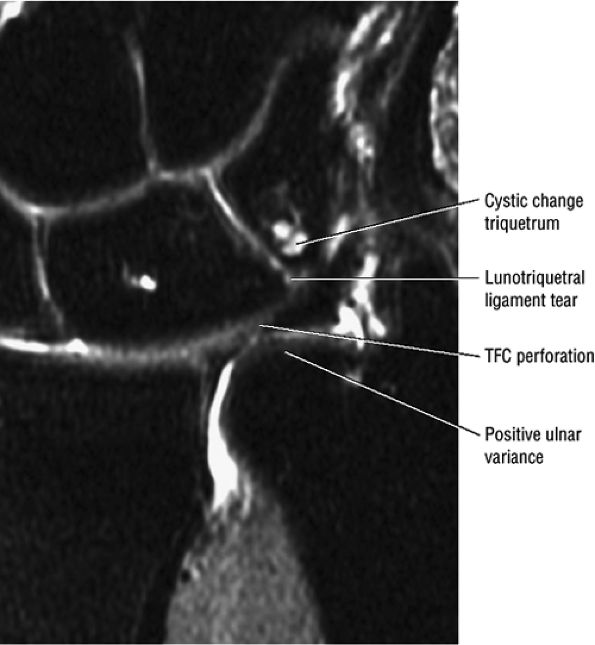 |
|
FIGURE 10.109 ● Ulnocarpal (ulnolunate) impaction with positive ulnar variance, TFC degenerative tear, and lunotriquetral (LT) ligament disruption. Lunate and triquetral proximal cystic change and sclerosis and edema may be visualized on either side of the lunotriquetral interval. Coronal FS PD FSE image.
|
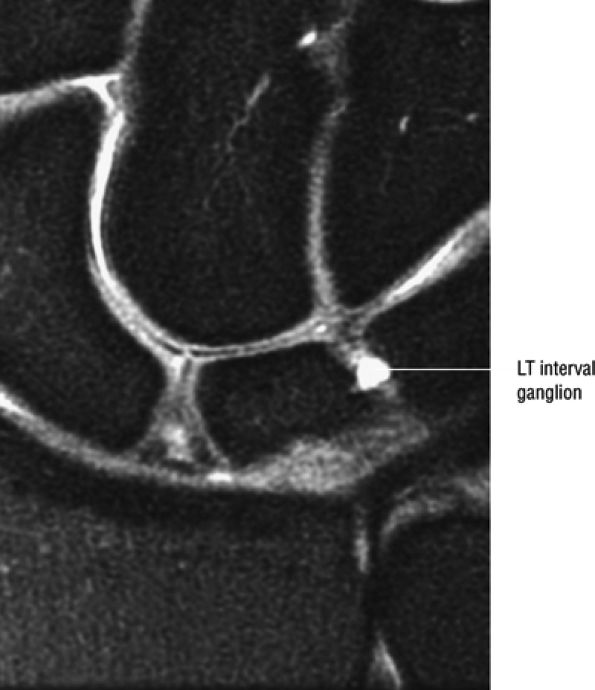 |
|
FIGURE 10.110 ● Dorsal lunotriquetral (LT) ligament ganglion overlying dorsal fibers on a coronal FS PD FSE image.
|
-
Clinical signs and symptoms, including the characteristic carpal clunk, must be considered in combination with MR findings.
-
Clunking of the carpus may be present in asymptomatic wrists.
-
Associated capitolunate sclerosis or VISI deformity may be demonstrated on sagittal images.
-
Injury with laxity of the ulnar arm of the arcuate ligament and the dorsal radiolunotriquetral ligament is seen in palmar midcarpal instability.
-
A palmar sag of the ulnar side of the carpus
-
A prominent ulnar head with the wrist in neutral deviation
-
Localized synovitis
-
Tenderness over the ulnar carpus and triquetrohamate joint
-
Active ulnar deviation of pronated wrist reproduces the clunk.
-
With extreme ulnar deviation (after the clunk), the volar sag of the ulnar carpus is absent.
-
A positive midcarpal shift test (a painful clunk with passive ulnar deviation)
-
Sclerosis between the distal lunate and the proximal capitate
-
An attenuated or disrupted lunotriquetral ligament
-
Fluid extension across the lunotriquetral or scapholunate interval
-
Synovitis, attenuation, or laxity of the ulnar arm of the arcuate ligament (Fig. 10.111) and dorsal radiotriquetral ligament (in palmar midcarpal instability) (Fig. 10.112)
-
Ulnar minus variance
-
Associated extension of contrast directly communicating across the scapholunate or lunotriquetral interval on MR arthrograms
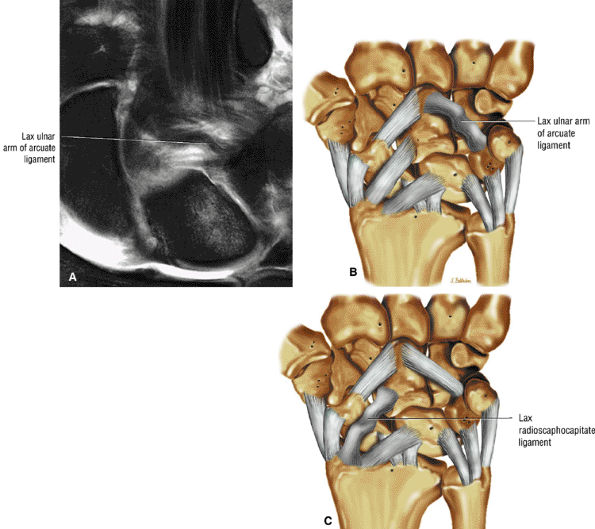 |
|
FIGURE 10.111 ● Palmar midcarpal instability (MCI) is the most common pattern of midcarpal instability. Palmar MCI is associated with laxity of the ulnar arm of the arcuate ligament and the dorsal radiotriquetral ligament with palmar (volar) translation of the distal carpal row. (A) Laxity of the ulnar arm of the arcuate ligament on a coronal FS PD FSE image. (B) Coronal illustration of the lax ulnar arm of the arcuate ligament. (C) Coronal illustration of the lax radioscaphocapitate ligament as seen in dorsal midcarpal instability in contrast to palmar midcarpal instability. Dorsal midcarpal instability is a much less common variant of midcarpal instability.
|
detailed discussion of the treatment of carpal instability is found below.
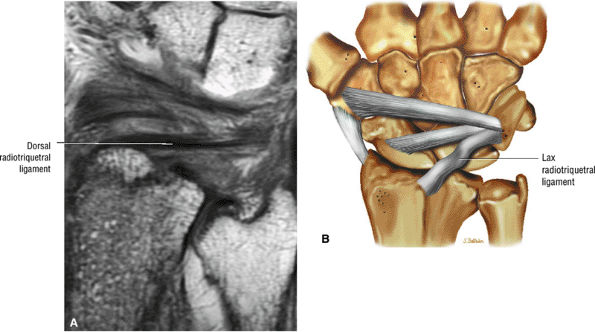 |
|
FIGURE 10.112 ● (A) The course of the dorsal radiotriquetral ligament, which passes obliquely across the dorsal surface of the lunate (to which it is attached) and terminates in the dorsal triquetrum. A fracture fragment of the lip of the distal radius is attached to the proximal radiotriquetral ligament on this PD-weighted coronal image. (B) Coronal illustration with lax radiotriquetral ligament (dorsal view).
|
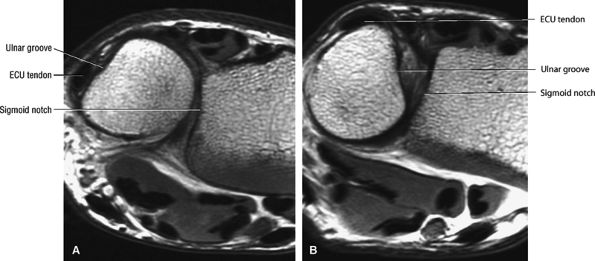 |
|
FIGURE 10.113 ● Normal biomechanics of the distal radioulnar joint. (A) Mild dorsal shift of the ulna relative to the sigmoid notch of the distal radius in full pronation is normal. The extensor carpi ulnaris tendon is located within its groove in the medial distal aspect of the ulna. (B) Mild volar shift of the ulna in full wrist supination is normal. The extensor carpi ulnaris tendon may be located within its ulnar groove or subluxed medially in extreme supination, as shown in this example.
|
-
Eccentric lunate sclerosis (ulnar-sided) is associated with ulnocarpal abutment.
-
Positive ulnar variance is not required.
-
Ulnocarpal abutment represents the spectrum of findings in Palmer class 2 degenerative lesions of the TFC complex.
-
Palmer class IIA lesions represent TFC complex wear.
-
Palmer class IIB lesions represent TFC complex wear and lunate, triquetrum, and possibly ulnar chondromalacia.
-
Palmer class IIC lesions represent TFC complex perforation and lunate, triquetrum, and possibly ulnar chondromalacia.
-
Palmer class IID lesions represent TFC complex perforation and lunate, triquetrum, and ulnar chondromalacia and lunotriquetral ligament perforation.
-
Palmer class IIE lesions represent TFC complex perforation and lunate, triquetrum, and ulnar chondromalacia, lunotriquetral perforation, and ulnocarpal arthritis.
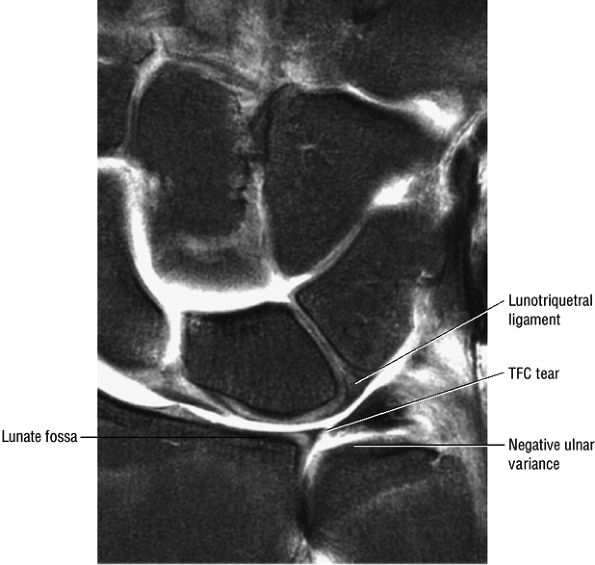 |
|
FIGURE 10.114 ● Negative ulnar variance with the articular surface of the ulna projecting proximal to the articular surface of the radius. In cases of severe negative ulnar variance, the TFC has a deformed morphology and extends proximally.
|
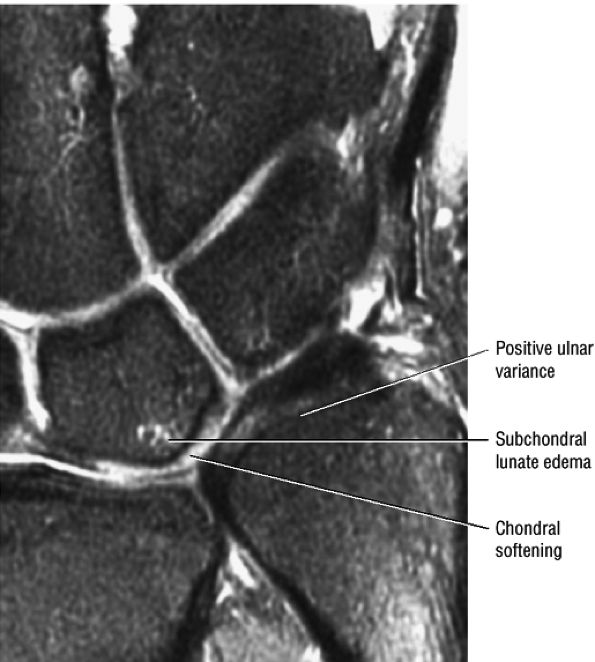 |
|
FIGURE 10.115 ● Positive ulnar variance with the articular surface of the ulna projecting distal to the lunate fossa of the distal radius. There are initial changes of ulnocarpal (ulnolunate) abutment with subchondral edema of the proximal lunate. Coronal FS PD FSE image.
|
-
Eccentric sclerosis of the proximal ulnar aspect of the lunate and the proximal radial aspect of the triquetrum
-
Subchondral sclerosis and cystic changes occur more often in the lunate than in the triquetrum.
-
Normal marrow fat signal distal and radial to the sclerosis in the lunate
-
Neutral or positive ulnar variance, although less commonly there may be negative ulnar variance
-
Possible associated trauma to the distal radius or ulnar styloid
-
Attenuated centrum or a central perforation of the TFC
-
Chondromalacia involving the articular cartilage of the ulna (Fig. 10.117)
-
Fluid across the torn lunotriquetral ligament or lunate-triquetrum proximal arc offset associated with lunotriquetral ligament tear
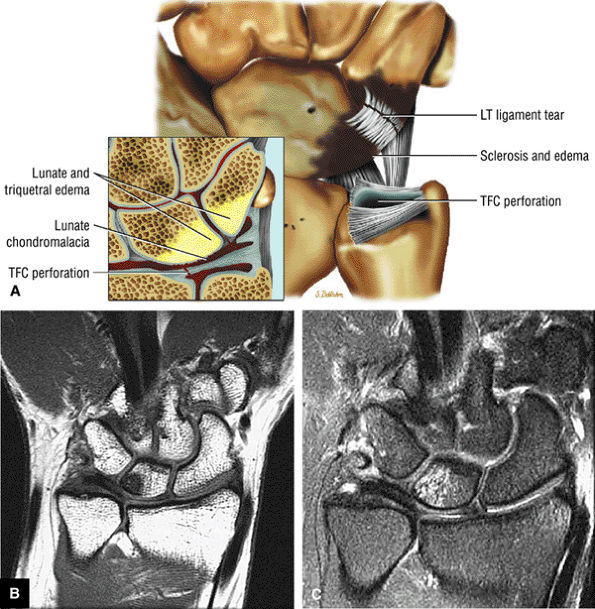 |
|
FIGURE 10.116 ● (A) Coronal color illustration of ulnocarpal (ulnolunate) abutment with associated lunotriquetral ligament tear. TFC perforation and reactive subchondral edema are shown in the lunate and triquetrum. Coronal T1-weighted (B) and FS PD FSE (C) images demonstrate ulnar-sided eccentric sclerosis and edema of the proximal lunate in conjunction with positive ulnar variance.
|
for Colles', Smith's, Galeazzi's, and Essex-Lopresti fractures. A younger population is at risk for traumatic injury and older individuals are at risk for injury associated with osteoporosis.
-
Axial images in full pronation and supination are used to identify the location of the ulna relative to the sigmoid notch.
-
The dorsal and volar radioulnar ligaments of the TFC are evaluated on coronal, axial, and sagittal images.
-
Ulnar dorsal dislocation in hyperpronation is associated with disruption of the volar distal radioulnar ligament.
-
Ulnopalmar (ulnovolar) dislocation in hypersupination occurs with disruption of the dorsal distal radioulnar ligament.
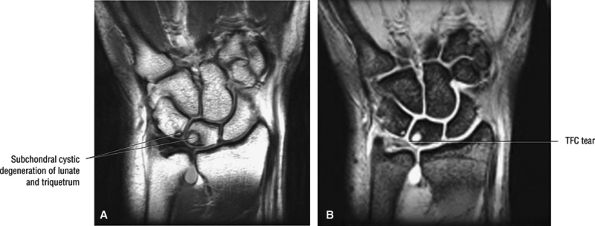 |
|
FIGURE 10.117 ● Chondromalacia involving subchondral cystic change of the proximal ulnar aspect of the lunate and proximal radial aspect of the triquetrum in ulnocarpal (ulnolunate) abutment. There is disruption of the lunotriquetral ligament of the TFC. (A) Coronal PD FSE image. (B) Coronal T2* gradient-echo image.
|
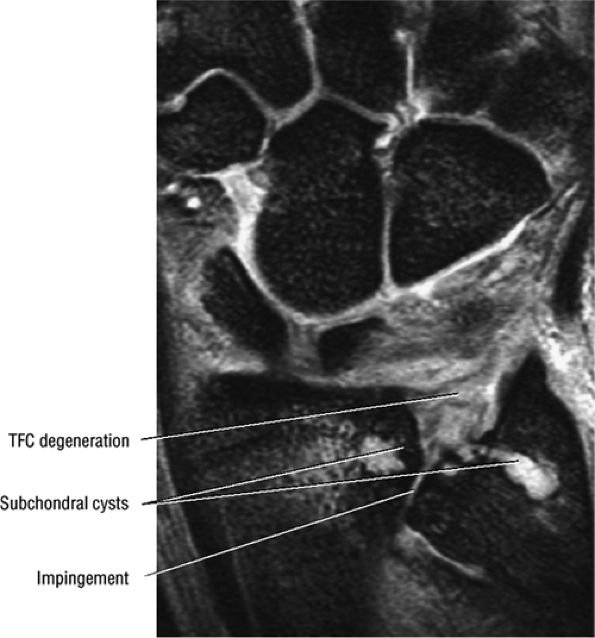 |
|
FIGURE 10.118 ● Radioulnar impingement with degenerative distal radioulnar joint changes, including subchondral cysts, chondromalacia, and TFC degeneration. Coronal T2* gradient-echo image.
|
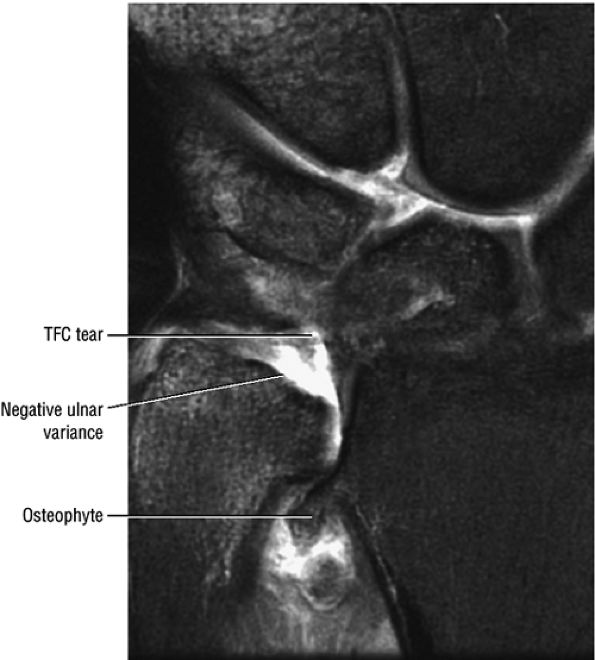 |
|
FIGURE 10.119 ● Hypertrophic osteophyte associated with distal radioulnar joint. Coronal FS PD FSE image.
|
-
Type I: Dislocation of the distal radioulnar joint secondary to disruption of the primary soft-tissue structures or to osseous injury (ulnar styloid fracture).
-
Type II: Intra-articular distal radioulnar joint fracture-dislocations
-
Type III: Extra-articular distal radioulnar joint fracture-dislocations
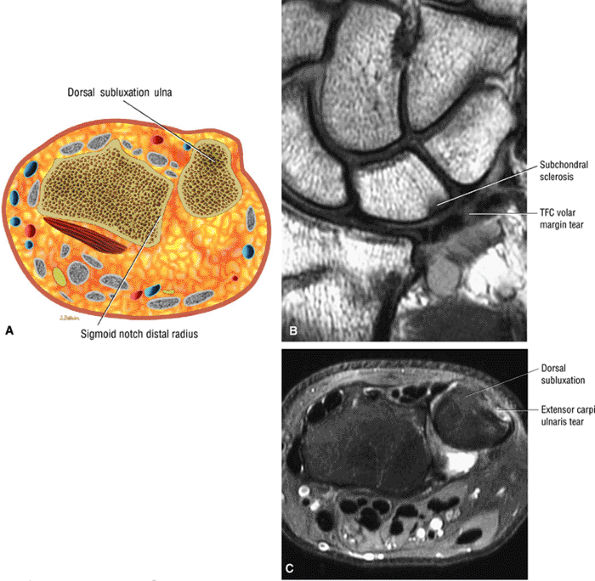 |
|
FIGURE 10.120 ● (A) Dorsal subluxation of the ulna relative to the sigmoid notch. Axial color graphic. (B) Disruption of the volar margin of the TFC (volar radioulnar ligament and volar aspect of the TFC in association with a distal radius fracture). Coronal T1-weighted image. (C) Ulnar dorsal subluxation (radial volar subluxation) secondary to disruption of the volar radioulnar ligament. The extensor carpi ulnaris tendon and subsheath are also ruptured. Axial FS PD FSE image.
|
-
Dorsal or volar (palmar) subluxation of the ulnar head relative to the sigmoid notch on axial images
-
Dorsal prominence of the ulna (ulna-dorsal) on sagittal images
-
A flattened or shallow sigmoid notch
-
Distal radioulnar joint diastasis on coronal images in ulnar dorsal subluxation
-
Massive disruption of the stabilizing capsuloligamentous structures (e.g., as in a Galeazzi fracture)
-
Subluxation or interposition of the extensor carpi ulnaris tendon
-
Associated intercalated segment instability pattern, either VISI (volar) or DISI (dorsal)
-
Palmar (volar) distal radioulnar ligament disruption associated with ulnar dorsal dislocation
-
Dorsal distal radioulnar ligament disruption associated with ulnar palmar dislocation
-
Ulnocarpal ligamentous complex hyperintensity (tear associated with ulnar dorsal pattern)
-
A tear of the dorsal infratendinous extensor retinaculum (the subsheath of the extensor carpi ulnaris, seen in ulnar dorsal dislocation)
-
Pronator quadratus and distal interosseous membrane hyperintensity on FS PD FSE images as part of forced hypersupination and ulnar palmar dislocation
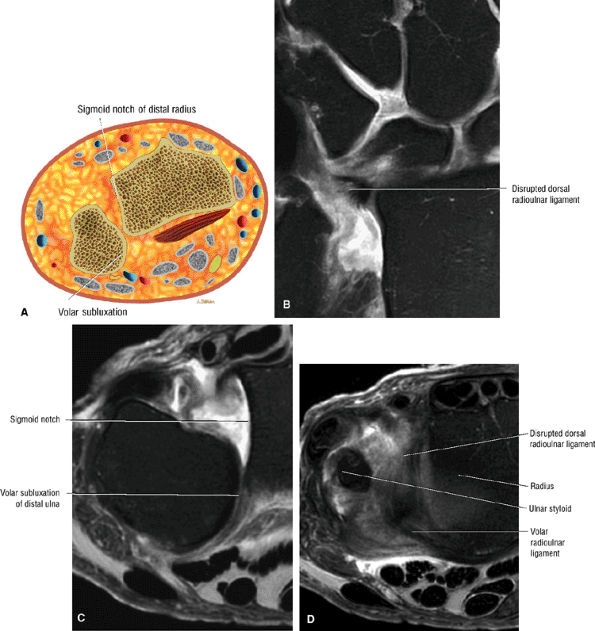 |
|
FIGURE 10.121 ● Volar subluxation of the distal ulna (dorsal subluxation of the distal radius) with disruption of the dorsal margin of the TFC (dorsal radioulnar ligament). (A) Axial color graphic. (B) Coronal FS PD FSE image. (C, D) Axial FS PD FSE images.
|
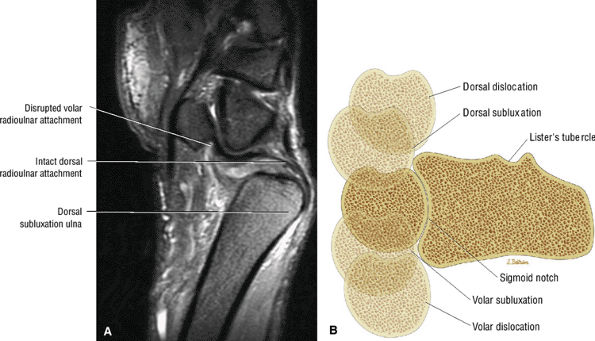 |
|
FIGURE 10.122 ● (A) Ulnar dorsal dislocation in hyperpronation with torn volar radioulnar attachment. Sagittal FS PD FSE image. (B) Axial section of the distal radioulnar joint demonstrating the positions of subluxation and dislocation of the distal ulna relative to the sigmoid notch of the distal radius.
|
carpal row. With a strong radial attachment of the TFC, the ligaments that have or share TFC attachment function to connect the volar aspect of the carpus to the radius.
-
Coronal T1- and PD-weighted or T2* gradient-echo images are used to improve the conspicuity of TFC intrasubstance degeneration. FS PD FSE sequences are used to evaluate contour irregularities, including partial and complete tears.
-
The distal radioulnar ligaments (volar and dorsal margins of the TFC) are evaluated on coronal and sagittal images.
-
Class IA: Perforation or traumatic tear of the TFC disc proper (Fig. 10.123)
-
Class IB: Ulnar avulsion of the TFC complex with or without associated ulnar styloid fracture (Fig. 10.124)
-
Class IC: Distal avulsions of the TFC complex through its lunate attachment (the ulnolunate ligament) or its triquetrum attachment (the ulnotriquetral ligament) (Fig. 10.125)
-
Class ID: Radial avulsions at the level of the distal sigmoid notch with or without associated sigmoid notch fracture (Fig. 10.126)
 |
|
FIGURE 10.123 ● Class IA lesion with slit-like tear or perforation (straight arrow) of the radial aspect of the TFC medial to its radial origin. There is communication of radiocarpal joint contrast (curved arrow) with the distal radioulnar joint. FS T1-weighted coronal arthrogram.
|
-
Class IIA: TFC complex wear (Fig. 10.127)
-
Class IIB: TFC complex wear with associated lunate and/or ulnar chondromalacia (Fig. 10.128)
-
Class IIC: TFC complex perforation in association with lunate or ulnar chondromalacia (Fig. 10.129)
-
Class IID: TFC complex perforation, lunate or ulnar chondromalacia, and lunotriquetral ligament perforation (Fig. 10.130)
-
Class IIE: Class IID injuries with the additional finding of ulnocarpal arthritis (Fig. 10.131)
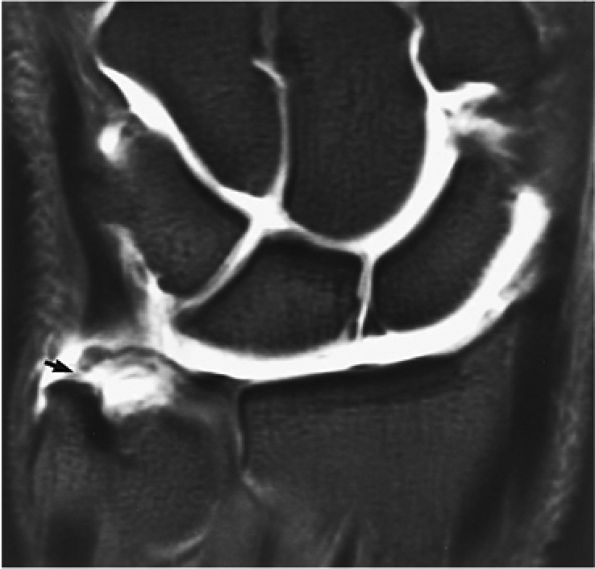 |
|
FIGURE 10.124 ● Class IB lesion with traumatic avulsion of the ulnar attachment of the TFC. There is direct extension of contrast between the ulnar styloid and the avulsed TFC (arrow). In addition, this patient has an avulsion of the ulnar aspect of the scapholunate ligament and absent lunotriquetral ligament. FS T1-weighted coronal arthrogram.
|
 |
|
FIGURE 10.125 ● FS sagittal T1-weighted arthrograms comparing (A) intact (black and white straight arrow) ulnocarpal (ulno-lunate and ulnotriquetral) ligament with (B) avulsed osseous insertions (curved arrow) of the ulnocarpal ligaments. There is also associated tearing of the dorsal radial aspect of the TFC. Isolated avulsion of the distal ulnolunate or ulnotriquetral ligaments as described in a class IC lesion is not common. H, hamate; T, triquetrum; tfc, triangular fibrocartilage; U, ulna; P, pisiform.
|
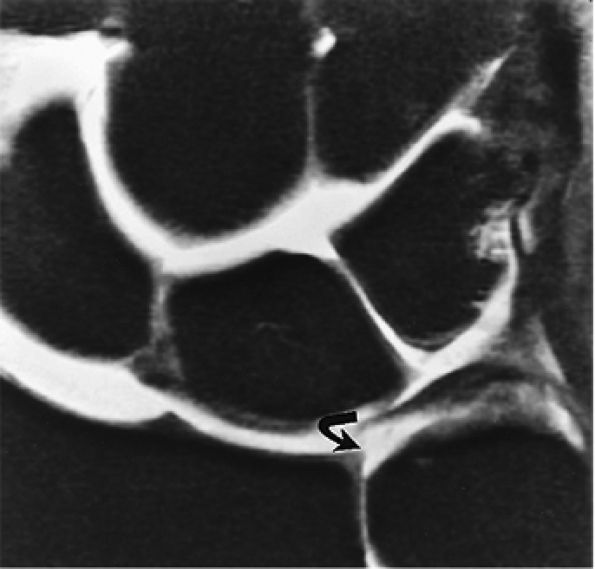 |
|
FIGURE 10.126 ● Traumatic avulsion of the radial attachment of the TFC as described in class ID lesions. Note the exposed articular cartilage at the radial sigmoid notch. Fluid communicates between the radiocarpal and distal radioulnar compartments (curved arrow) on this FS coronal T1-weighted arthrogram. The lunotriquetral ligament is absent.
|
 |
|
FIGURE 10.127 ● Class IIA lesion with degenerative thinning (arrows) of the TFC without perforation. No lunate chondromalacia is present and the lunotriquetral ligament is intact. U, ulna. FS coronal T1-weighted arthrogram.
|
 |
|
FIGURE 10.128 ● Class IIB lesion with degenerative fraying of the distal aspect of the TFC (straight arrow). There is chondromalacia of the lunate and triquetrum (curved arrow) without associated TFC perforation. The lunotriquetral and scapholunate ligaments are torn. FS coronal T1-weighted arthrogram.
|
 |
|
FIGURE 10.129 ● Class IIC lesion with a central TFC perforation (straight arrow) and lunate chondromalacia (curved arrow) on a FS PD FSE coronal image. No intra-articular contrast was required to facilitate the diagnosis. The lunotriquetral ligament is intact (open arrow). Tapering of the edges of the TFC is seen in degenerative (class II) lesions, whereas traumatic (class I) tears tend to have abrupt or straight margins.
|
Separation of the peripheral insertions of the TFC complex, especially at the fovea or radius, results in a loss of this suspensory trampoline effect.90
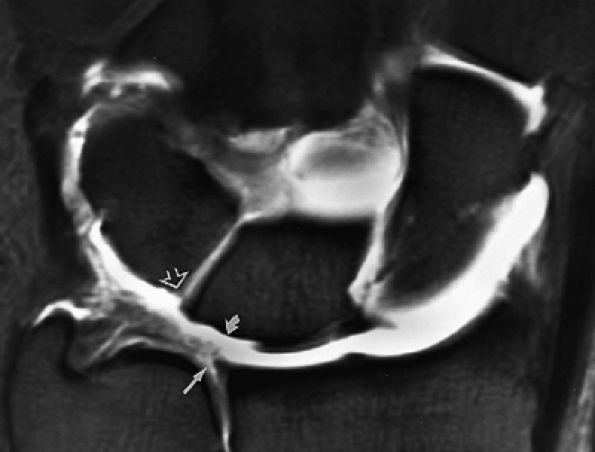 |
|
FIGURE 10.130 ● FS T1-weighted coronal arthrogram demonstrating class IID injury with perforation of the TFC (straight arrow), loss of lunate articular cartilage (curved arrow), and lunotriquetral ligament disruption (open arrow). Intrasubstance enhancement of the TFC is commonly seen in degenerative lesions.
|
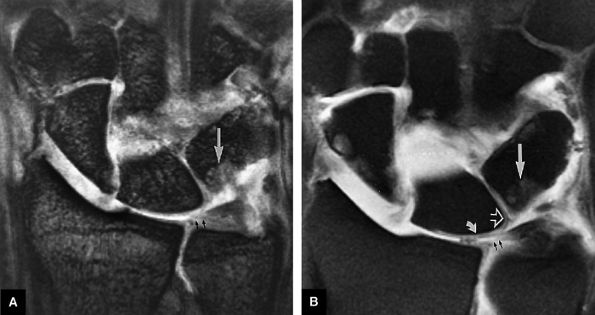 |
|
FIGURE 10.131 ● Class IIE lesion with ulnocarpal arthritis demonstrates a central TFC perforation (small straight arrows), lunate (curved arrow) and triquetral chondromalacia, lunotriquetral ligament tear (open arrow), and triquetral subchondral erosion (long straight arrow). (A) T2*-weighted coronal image. (B) FS T1-weighted coronal arthrogram.
|
dissections and may provide stability at the level of the pisotriquetral articulation.95 The prestyloid recess is defined as a high-signal-intensity area bordered by the meniscus homologue, the styloid attachment of the TFC complex, the central disc, the medial carpal capsule, and the extensor carpi ulnaris sheath (Fig. 10.136).
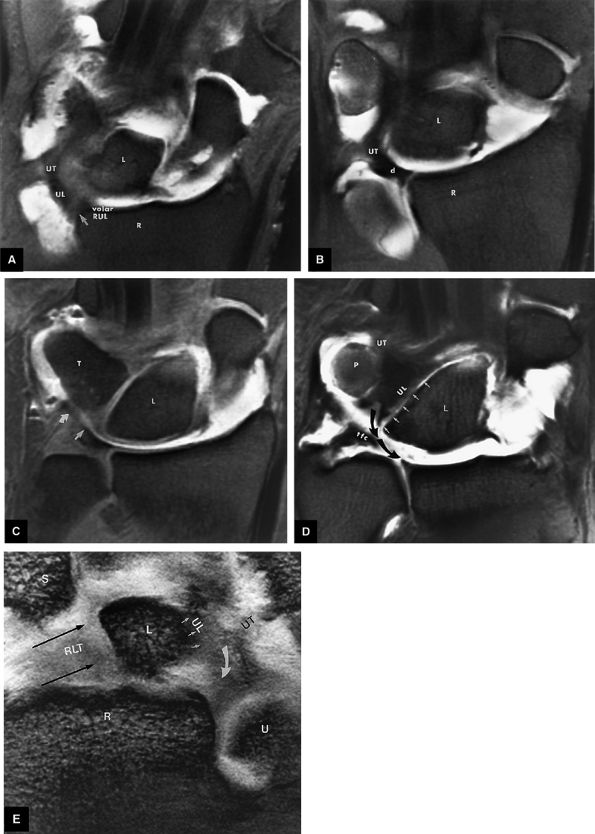 |
|
FIGURE 10.132 ● TFC complex, volar aspect. (A) Volar FS T1-weighted coronal arthrogram shows the radial attachment (arrow) of the volar radioulnar ligament (volar RUL). The ulnolunate (UL) and ulnotriquetral (UT) ligaments (components of the ulnocarpal ligament) originate and extend from the volar radioulnar ligament to attach to the volar-ulnar aspect of the lunate and triquetrum. (B) FS T1-weighted coronal arthrogram shows the ulnotriquetral ligament (UT) continuing in an ulnar distal course toward the triquetrum at the level of the volar aspect of the articular disc (d). (C) The ulnolunate (straight arrow) and ulnotriquetral (curved arrow) ligaments are visualized as a merged or confluent extension from the volar aspect of the radioulnar ligament. FS T1-weighted coronal arthrogram. (D) The lunate (L) insertion (arrows) and triquetrum insertion of the ulnolunate (UL) and ulnotriquetral (UT) ligaments, respectively, are shown. Note the broad-based common origin of these ligaments from the distal volar aspect of the volar radioulnar ligament (curved arrow). FS coronal T1-weighted arthrogram shows that the radial aspect of the TFC is torn in this patient. (E) A separate case demonstrates the continuity of the hypointense sheet of tissue representing the ulnolunate (UL) and ulnotriquetral (UT) ligaments extending from the volar aspect of the volar radioulnar ligament (curved arrow). RLT and straight arrow, radiolunotriquetral ligament; R, radius; L, lunate; U, ulna; T, triquetrum; P, pisiform; S, scaphoid.
|
 |
|
FIGURE 10.133 ● The dorsal radioulnar ligament (dorsal RUL; arrow) attachment to the dorsal distal radius. The dorsal portions of the intrinsic interosseous scapholunate and lunotriquetral ligaments are also seen at this level. FS coronal T1-weighted arthrogram.
|
 |
|
FIGURE 10.134 ● Insertion of the TFC complex into the ulnar styloid (s) process is accomplished by separate groups of fascicles directed to the styloid tip (white arrow) and base (black arrow). The ulnar collateral ligament (UCL), seen as a distinct structure of the TFC complex, extends from the outer aspect of the ulnar styloid to the triquetrum, hamate, and fifth metacarpal. The meniscus homologue (m) corresponds to thickening of the longitudinally oriented fibers of the ulnar collateral ligament distal to the TFC. FS coronal T1-weighted arthrogram.
|
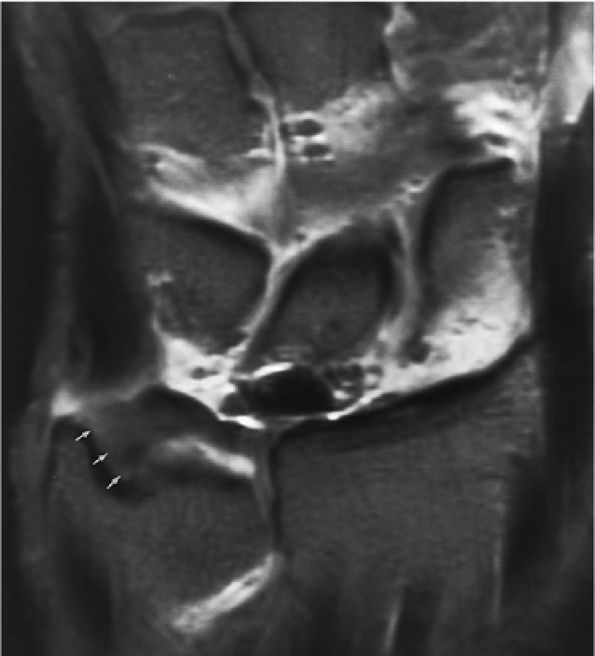 |
|
FIGURE 10.135 ● Single broad-based attachment of the TFC complex extending from the tip to the base of the ulnar styloid process (arrows). FS coronal T1-weighted coronal arthrogram.
|
intensity and should not be mistaken for fluid communication with the inferior radioulnar joint or detachment of the radial aspect of the TFC. Intrasubstance degeneration of the TFC is best depicted on T2*-weighted images and appears as regions of increased signal intensity without extension to the superior or inferior margins of the TFC. The meniscus homologue demonstrates greater signal intensity than the TFC on T2*-weighted images. Partial tears in this area may be more difficult to identify due to the increased signal intensity and inhomogeneity of the meniscal homologue and ulnar attachments. Tears of the TFC may occur either as an isolated injury or in association with subluxations of the distal radioulnar joint or perilunate dislocations. TFC tears, demonstrated by discontinuity or fragmentation, are most commonly located near or adjacent to the radial attachment.67 Contour irregularities, especially with associated regions of increased signal intensity, can be identified on T1-weighted, FS PD FSE, and T2*-weighted images. Tears on the radial aspect of the TFC frequently have a dorsal-to-volar orientation and extend to both its proximal and distal surfaces (Fig. 10.138).
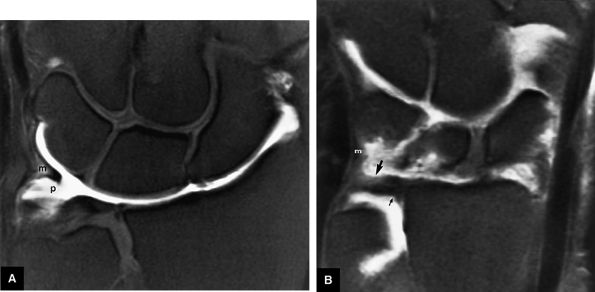 |
|
FIGURE 10.136 ● Meniscus homologue and prestyloid recess. (A) The triangular meniscus homologue (m) and prestyloid recess (p) are shown on an FS coronal T1-weighted arthrogram. The prestyloid recess is seen proximal to the meniscus homologue and distal to the ulnar styloid attachment of the TFC complex. The TFC, or central disc, is located radial to the prestyloid recess, whereas the medial capsule defines the ulnar aspect of the recess. The extensor carpi ulnaris tendon sheath courses dorsal to the prestyloid recess. (B) A more dorsal coronal image demonstrates the confluence of the meniscus homologue (m) and the radial origin of the dorsal radioulnar ligament (large arrow). A fold from the dorsal radioulnar ligament forms the proximal attachment of the TFC complex (small arrow). FS coronal T1-weighted arthrogram.
|
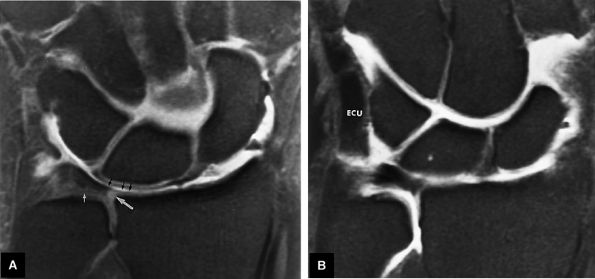 |
|
FIGURE 10.137 ● The TFC. (A) The distal aspect of the TFC or central disc is shown to be contiguous with the articular cartilage of the distal surface of the lunate fossa (small black arrows). The volar and dorsal radioulnar ligaments contribute to the striated tissue between the ulnar styloid and the central disc. High-signal-intensity articular cartilage (large white arrow) is present at the radial attachment of the central disc to the sigmoid notch of the radius. The central disc is in direct contact with the articular cartilage of the ulnar head in the absence of distal radioulnar joint fluid distention (small white arrow). FS coronal T1-weighted arthrogram. (B) The extensor carpi ulnaris tendon and sheath (extensor carpi ulnaris) are identified on a more dorsal coronal image in the plane of the TFC. The TFC attaches to the sheath of the extensor carpi ulnaris tendon dorsomedially. FS coronal T1-weighted arthrogram.
|
-
Intrasubstance degeneration, best visualized on T1-, PD-, or T2*-weighted gradient-echo images
-
Volar margin tears associated with dorsal subluxation of the ulna relative to the radius
-
Dorsal tears associated with volar subluxation of the ulna
-
Volar instability seen on supination in the axial plane
-
Dorsal instability seen on pronation in the axial plane
-
Radial-sided tears with a dorsal-to-volar orientation
-
Ulnar avulsion with or without an ulnar styloid fracture
-
Radial avulsion with or without a sigmoid notch fracture
-
Chondromalacia and sclerosis of the lunate, triquetrum, and distal ulna in ulnocarpal (ulnolunate) abutment syndrome with loss of the normal signal intensity of articular cartilage
-
Contour irregularity of the proximal (undersurface) or distal surfaces in partial tears
-
Fluid extension across the articular disc or discontinuity
-
Synovitis
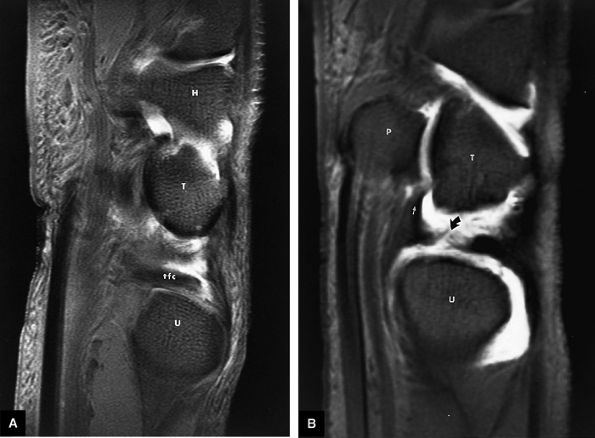 |
|
FIGURE 10.138 ● Comparison of (A) an intact TFC with (B) a TFC tear on FS sagittal T1-weighted arthrograms. The TFC tear (curved arrow) involves the radial aspect of the disc without disruption of the volar ulnocarpal ligaments (straight arrow). H, hamate; T, triquetrum; tfc, triangular fibrocartilage; P, pisiform; U, ulna.
|
better long-term results than resection. In triquetral impingement of the ulnar styloid, limited ulnar styloidectomy may provide symptom relief.
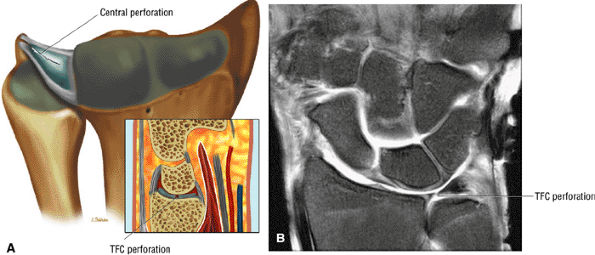 |
|
FIGURE 10.139 ● (A) Central perforation of the TFC on a coronal color illustration with a sagittal inset. (B) Central TFC perforation on an FS PD FSE image.
|
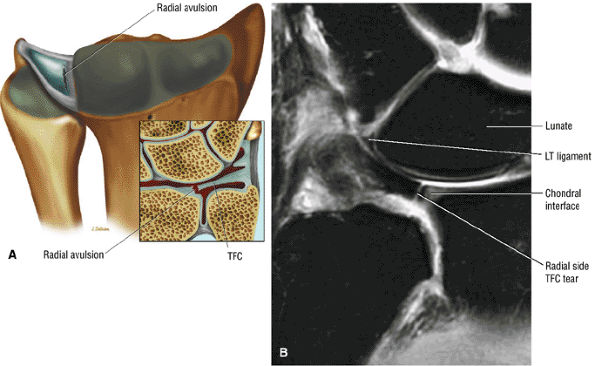 |
|
FIGURE 10.140 ● (A) Radial avulsion of the TFC on coronal color illustration. (B) Vertical radial-sided TFC tear parallel to the normal radial chondral junction. Coronal FS PD FSE image.
|
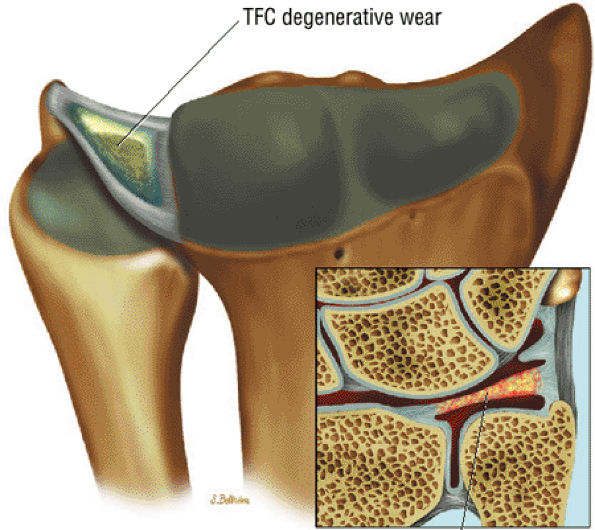 |
|
FIGURE 10.141 ● Palmer class II degenerative wear as the initial stage of ulnocarpal (ulnolunate) abutment syndrome. Color coronal illustration.
|
radius. Trispiral tomography depends on correct planar positioning, or carpal fractures may be underdiagnosed. Results from early bone scintigraphy, performed within 72 hours of an acute fracture, may be negative or equivocal. CT using thin (1.5-mm) sections in either direct coronal or axial planes with reformatting and 3D rendering is the most accurate modality for identifying fractures and for characterizing morphology and associated comminution or displacement. Chip fractures can be detected by CT in patients with negative findings on MR studies. Fracture extent and adjacent marrow hyperemia are clearly demonstrated on MR images. In subacute and chronic fractures, sclerosis demonstrates low signal intensity on T1-weighted images. The temporal stage of a fracture (e.g., acute, subacute, chronic) and its location determine the optimal diagnostic imaging plane (e.g., coronal, axial, or sagittal). MR imaging shows associated ligamentous injury in isolated or multiple carpal bone trauma. If initial imaging is inadequate, delayed diagnosis and treatment may lead to poor anatomic reduction and loss of function.
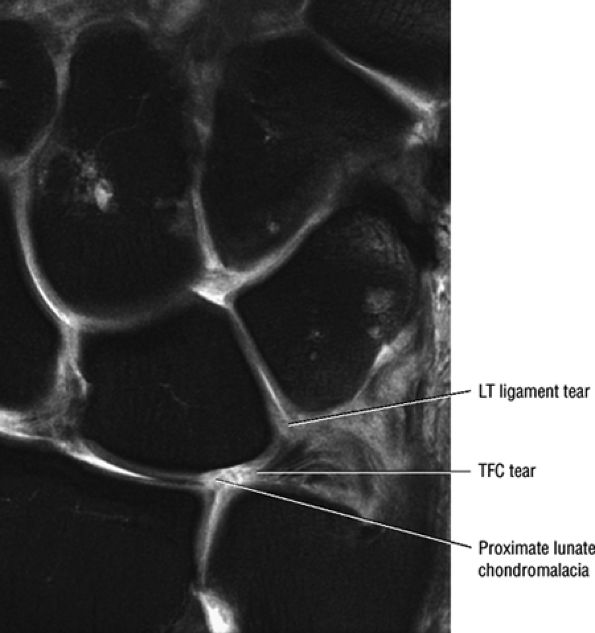 |
|
FIGURE 10.142 ● Palmer class II degenerative TFC tear in association with proximal lunate chondral erosion and lunotriquetral (LT) ligament tear. Coronal FS PD FSE image.
|
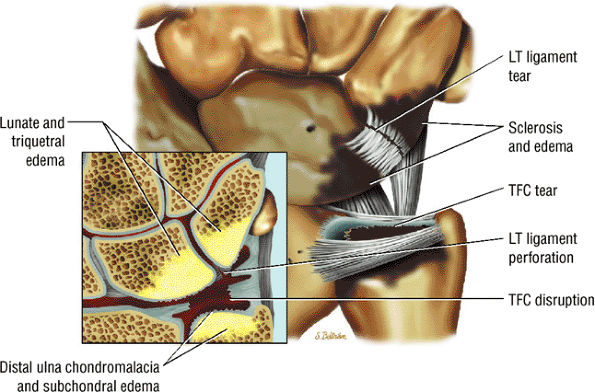 |
|
FIGURE 10.143 ● Advanced changes of ulnocarpal (ulnolunate) abutment (Palmer class II) with TFC tear, lunate, triquetral and ulnar chondromalacia, and lunotriquetral ligament tear. Coronal color illustration.
|
-
Associated radial styloid and ulnar styloid fractures should be identified.
-
Lunate fossa involvement in distal radius fractures is divided into dorsal and palmar (volar) medial components, characterized on sagittal images.
-
The Melone classification divides intra-articular fractures into four components: the radial shaft, the radial styloid, and dorsal medial, and volar medial segments.
-
Intra- and extraarticular fractures of the distal radius, including Barton's fracture, an intra-articular fracture-dislocation or subluxation (a palmar or dorsal fracture) with displacement of the carpus
-
Colles' fracture, a fracture of the distal metaphysis with dorsal displacement, angulation (silver fork deformity), radial angulation, and radial shortening
-
Smith's fracture (reverse Colles'), a palmarly angulated fracture (the garden spade deformity)
-
The Frykman classification102 (Fig. 10.144) has received the most attention. This system differentiates among fractures based on whether they are intraarticular or extra-articular and on the degree to which they involve the distal radioulnar joint.
-
In another system, developed by Melone,103 articular fractures of the distal radius are classified into five fracture types based on the degree and direction of displacement of the articular fragments (Fig. 10.145) and indications
P.1755
for open reduction. The four basic components of articular fractures in this classification are divided into metaphyseal or shaft, radial styloid, dorsal medial, and palmar medial sections. This system is clinically useful because it indicates when open reduction is necessary to achieve accurate anatomic reduction. On routine lateral radiographs, the normal palmar tilt of the articular surface of the distal radius is 10° to 14°. On PA radiographs, the inclination of the radial articular surface forms an angle of 23° with the long axis of the forearm. These angles must be accurately restored with fracture reduction. If the palmar tilt is not anatomically correct, the range of motion in flexion will be limited and an intercalated instability pattern of the carpus may develop. Loss of the angle of inclination leads to increased loading of the radial articular surface and arthritic degeneration.104 -
A universal classification that has replaced the Frykman classification, including the treatment algorithm. This classification is based on location, displacement, stability, and reducibility. Extra-articular and intra-articular fractures are subdivided into nondisplaced and displaced fractures.
-
The Mayo classification, which considers the scaphoid, lunate, and sigmoid notch as separate articulations with involvement of one or more articular fossae
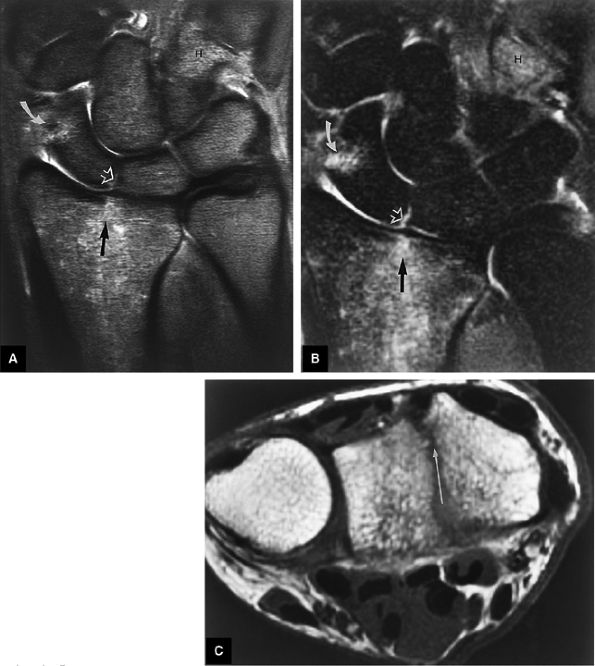 |
|
FIGURE 10.144 ● Nondisplaced intraarticular distal radius fracture (Frykman type III) associated with scapholunate ligament tear, hook of the hamate fracture, and nondisplaced fracture of the distal scaphoid pole. Fracture-related marrow edema is hyperintense on both FS PD FSE (A) and fast STIR (B) coronal images. The dorsal-to-volar extension of the fracture is shown on a T1-weighted axial image (C). In the Frykman classification of distal radius fractures, intra-articular fractures are classified as class III or higher, based on radiocarpal, distal radioulnar joint, and distal ulnar involvement. Complex intra-articular fractures have a poor prognosis.
|
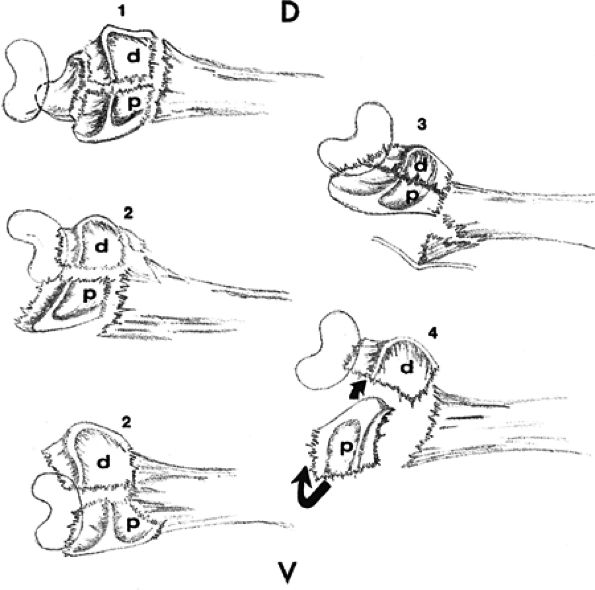 |
|
FIGURE 10.145 ● The Melone classification of distal radius articular fractures. The displacement of the medial complex (which consists of medial fragments and ligamentous attachments to the ulnar styloid and carpus) is the basis for classifying four types of articular fractures. (1) In a type I fracture, the medial complex may be displaced or not, with stable reduction and congruity of the joint surface. (2) In a type II fracture, there is comminution and the fracture is unstable. The medial complex is posteriorly or anteriorly displaced. (3) In a type III fracture, the medial complex is displaced and there is a spike fragment from the comminuted radial shaft. (4) In a type IV fracture, separation or rotation of the dorsal and palmar medial fragments occurs, with severe disruption of the distal radial articular surface. Small and large curved arrows indicate rotation of distal and palmar medial fragments; D, dorsal; d, dorsal medial fragment; p, palmar medial fragment; V, volar.
|
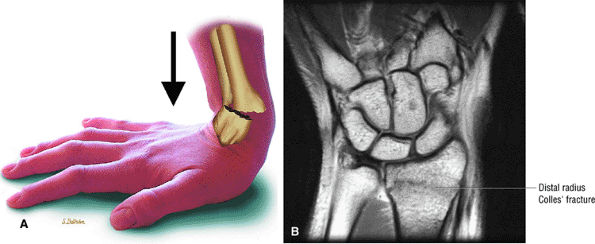 |
|
FIGURE 10.146 ● (A) Dorsal displacement of the distal radius in a Colles' fracture resulting from a fall on an outstretched hand. Lateral view color illustration. (B) Nondisplaced transverse Colles' fracture proximal to the distal articular surface of the radius. Coronal T1-weighted image.
|
-
Type I: Minimally displaced (Fig. 10.147)
-
Type II fractures. Type II, or die-punch, fractures are subdivided into two groups:
-
Type IIA: Dorsally displaced (most common) or volarly displaced (Figs. 10.148 and 10.149)
-
Type IIB: Die-punch fractures with lunate impaction, most commonly on the dorsal medial component. There is greater communication and displacement of the medial fragments, usually in a dorsal direction. A double die-punch fracture occurs when both the scaphoid and lunate impact the articular surface of the distal radius. Articular offset of the radiocarpal joint may exceed 2 mm.
-
Type III: Addition of a spike fragment from the volar metaphysis (Fig. 10.150)
-
Type IV: Separation or rotation of the dorsal and palmar medial fragments and disruption of the distal radius articulation (Fig. 10.151)
-
Type V: Explosion fracture with comminution from the articular surfaces to the diaphysis (Fig. 10.152)
-
Fracture diastasis can be directly measured on coronal, axial, or sagittal images.
-
Involvement of scaphoid plus lunate fossa can be evaluated on coronal images.
-
Fracture line(s) with extension to the volar or dorsal distal radius
-
Articular involvement should be correlated with offset of the chondral surface and subchondral plate.
-
Associated injury of the radial shaft and styloid
-
Marrow edema associated with carpal fractures or radial impaction and joint effusion
-
Synovitis and subcutaneous edema
-
Associated partial or complete ligament tears
arthrosis (associated with articular surface incongruity of more than 2 mm). Conservative treatment is appropriate for stable (Melone type I) injuries. Surgery is necessary for more complex injuries, and treatment considerations include the following:
-
Melone type IIA (unstable dorsal or volar displacement): treatment with reduction and external fixation
-
Melone type IIB: not reducible by closed techniques, treatment with open reduction and internal fixation (ORIF)
-
Melone type III: treatment with ORIF; volar spike fragment from metaphysis places adjacent nerves and tendons at risk
-
Melone type IV: arthroscopic percutaneous reduction and pinning or ORIF
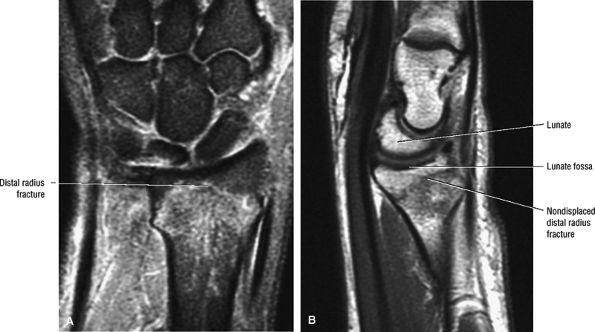 |
|
FIGURE 10.147 ● (A) Intra-articular nondisplaced radius fracture without separation of the medial complex (lunate fossa and related soft-tissue components). Coronal FS PD FSE image. (B) Intact lunate fossa is demonstrated on this sagittal T1-weighted image.
|
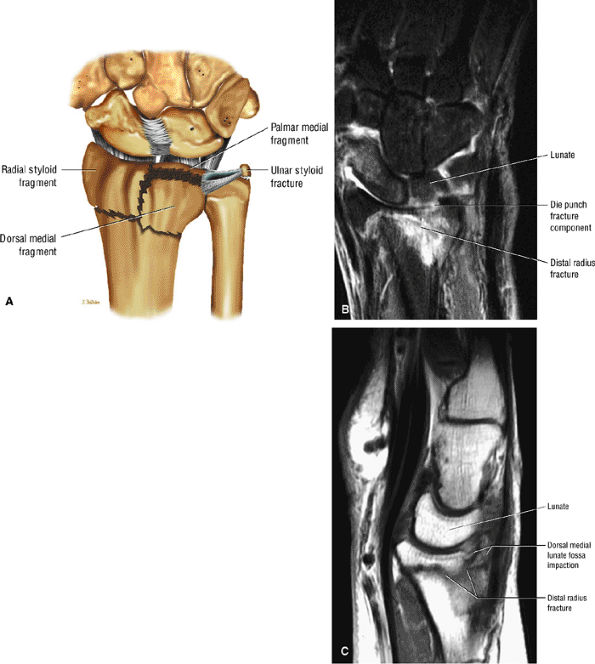 |
|
FIGURE 10.148 ● (A) A type II articular fracture with die-punch impaction of the dorsal medial component. Color coronal illustration. (B) Dorsal coronal FS PD FSE image demonstrating selective fracture extension of the dorsal lip of the lunate fossa on this coronal FS PD FSE image. (C) Dorsal die-punch involvement of the lunate fossa on a T1-weighted sagittal image.
|
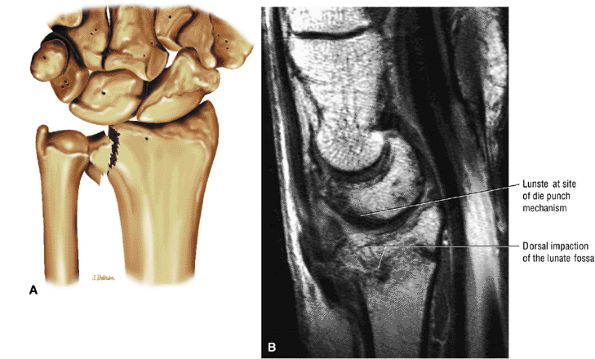 |
|
FIGURE 10.149 ● (A) Displaced die-punch fracture of the lunate fossa. Coronal color illustration. (B) Greater comminution of the dorsal metaphysis with dorsal tilting and shortening of the radius. T1-weighted sagittal image.
|
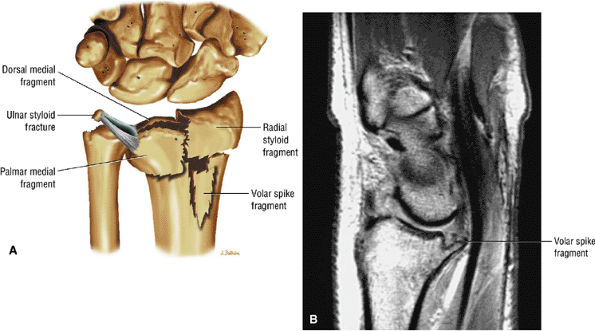 |
|
FIGURE 10.150 ● (A) Type III spike fractures include the articular disruption seen in a type II injury with the addition of a volar metaphyseal spike fragment. Displacement of the volar spike fragment may result in injury to adjacent nerves and tendons. Coronal color illustration. (B) Volar spike fragment on sagittal T1-weighted image.
|
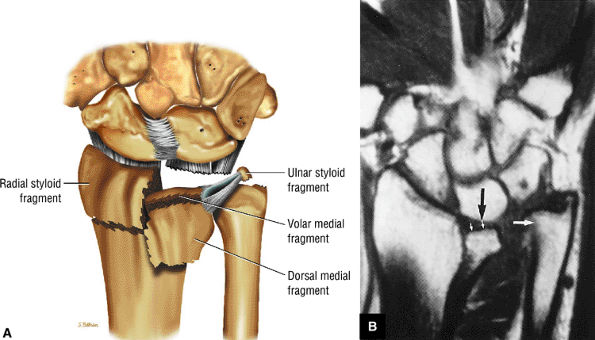 |
|
FIGURE 10.151 ● (A) Type IV fracture pattern with wide separation on rotation of the dorsal and palmar medial fragments. Coronal color illustration. (B) Coronal T1-weighted image shows splitting and depression of the lunate fossa (small white arrows) of the distal radius, with proximal migration of the lunate (black arrow). Associated diastasis (large white arrow) of the distal radioulnar joint is present, with complete disruption of the TFC complex.
|
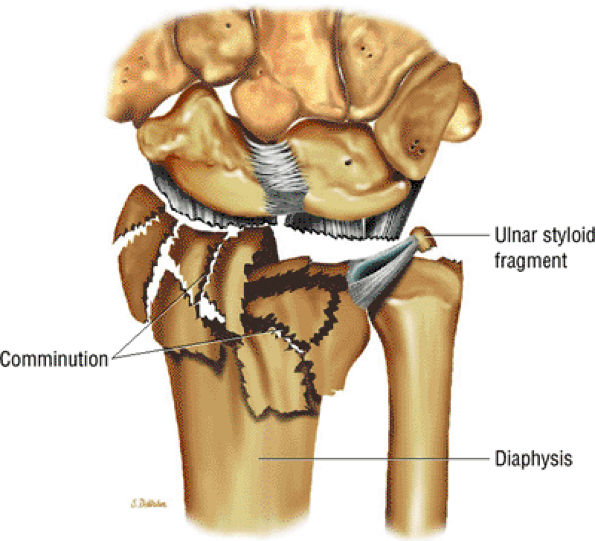 |
|
FIGURE 10.152 ● Type V explosion fraction with comminution extending from the distal radius articular surfaces to the diaphysis. This injury pattern is associated with massive soft-tissue trauma. Coronal color illustration.
|
-
In addition to identification of base or distal ulnar styloid fractures, TFC complex attachments should be evaluated.
-
Associated with distal radial fractures
-
Type 2 ulnar styloid fractures are associated with both nonunion and an unstable distal radioulnar joint.
-
Hypointense or hyperintense fracture line
-
Marrow edema proximal and distal to the fracture site
-
Displacement of fragments
-
Associated traumatic avulsion of the TFC at its insertion at the base of the ulnar styloid
-
Distal radioulnar joint instability, most likely to be seen with base fractures, with interosseous membrane tears and fluid interposed between the TFC and the attachment to the styloid base
-
Associated distal radius articular fractures (the ulnar styloid is part of the medial complex)
-
Associated soft-tissue injury, including the ulnar collateral ligament of the wrist, the TFC complex, and tendon injuries (e.g., extensor carpi ulnaris)
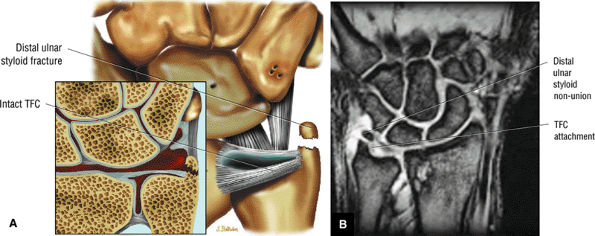 |
|
FIGURE 10.153 ● (A) Type 1 ulnar styloid fracture nonunion with intact TFC complex. (B) Ulnar styloid nonunion distal to the attachment of the TFC. Coronal T2* gradient-echo image.
|
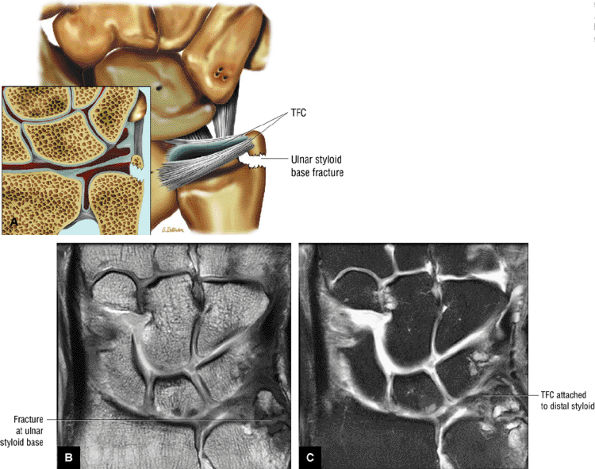 |
|
FIGURE 10.154 ● (A) Ulnar styloid fracture at the base of the styloid associated with an unstable distal radioulnar joint. Nonunion of ulnar styloid base on coronal T1-weighted (B) and coronal FS PD FSE (C) images. The TFC and ulnocarpal ligaments are attached to the styloid fragment.
|
-
A trabecular fracture line may persist with intact radial and ulnar cortices in the healing phase.
-
The wrist should be assessed for associated scaphoid flexion deformity and dorsiflexion instability of the lunate.
-
Displaced scaphoid fractures are usually the result of an incomplete or spontaneously reduced perilunate dislocation.
the attachment site for the dorsal radiocarpal and radial collateral ligaments. There is a palmar (volar) surface concavity which contains the radioscaphocapitate ligament. The flexor retinaculum attaches to the scaphoid tubercle, and the medial surface has two facets, a semilunar surface for lunate articulation and a large concavity for capitate articulation. The vascular supply is provided by the radial artery. Dorsal ridge vessels supply the proximal 70% to 80% of the scaphoid and scaphoid tubercle branches supply the distal 20% to 30%. The absence of a separate proximal pole blood supply leads to a propensity for delayed healing and AVN of the proximal pole (see the discussion of AVN and nonunion of the scaphoid, below).
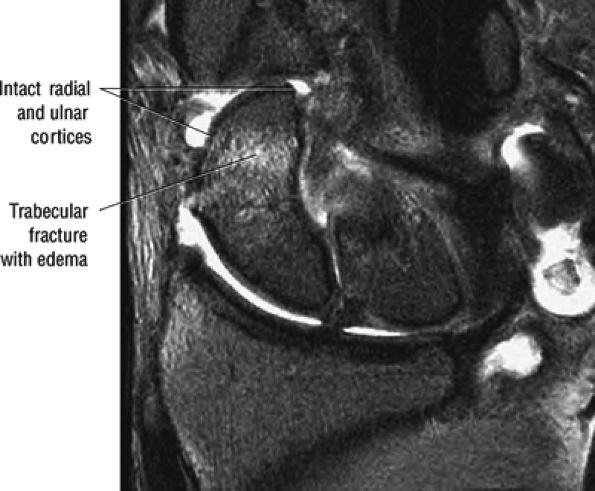 |
|
FIGURE 10.155 ● Initial presentation of transverse scaphoid fracture without interruption of the scaphoid cortex. Coronal FS PD FSE image.
|
-
Fracture line, in 80% of cases in the scaphoid waist (middle third) (Fig. 10.158), in 10% of cases in the proximal pole, and in 10% of cases in the tuberosity or distal pole (Fig. 10.159)
-
Scaphoid flexion (humpback deformity) on sagittal images (Fig. 10.160)
-
Intercarpal instability (ISI), especially if there is a scaphoid flexion deformity without injury to the scapholunate ligament (Fig. 10.161) with resultant wrist shortening
-
Fracture extension to the cortex differentiates acute from chronic fractures (intact cortex implies a chronic process) (Fig. 10.162).
-
Scaphoid angulation (the scaphoid is hinged open dorsally on the intact volar radioscaphocapitate ligament in association with dorsiflexion instability of the lunate)
-
Subchondral marrow edema adjacent to or on both sides of the fracture (see Fig. 10.160)
-
Diffuse marrow edema within scaphoid (less common)
-
Proximal pole edema or edema on either side of the fracture site
-
Associated injury to the scapholunate ligament and volar capsule (radioscaphocapitate and radiolunotriquetral ligaments)
-
Displaced and unstable fractures have a greater-than-1-mm step-off or an increased capitolunate angle (more than 30°).
-
Instability from uncorrected displacement is associated with pseudarthrosis.
-
AVN in the proximal pole as a complication of scaphoid fracture
-
Early SLAC with chondral loss between the distal pole of the scaphoid and the distal radius (styloid).
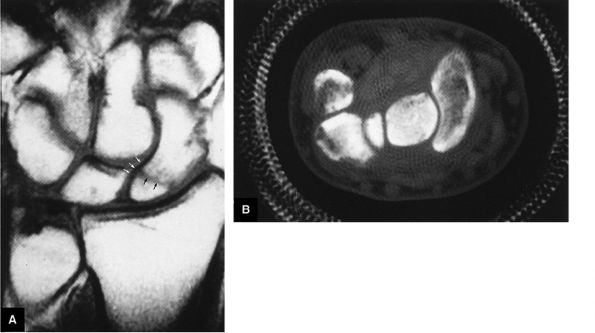 |
|
FIGURE 10.156 ● (A) T1-weighted coronal image shows a hypointense healing fracture line located across the proximal pole of the scaphoid (black arrows), with intact cortical margins (white arrows). Normal fatty marrow is present in the proximal pole. (B) Corresponding axial CT does not show cortical or trabecular fracture. This is consistent with the continuity of the cortex seen on corresponding MR images, which are more sensitive in the initial and healing stages of scaphoid fractures. Small chip fractures of other carpal bones, however, are still best evaluated with thin-section CT.
|
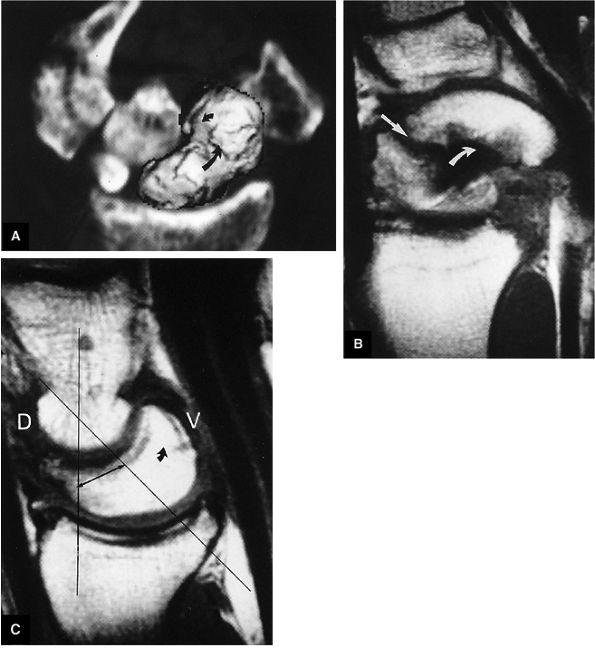 |
|
FIGURE 10.157 ● Scaphoid fracture with DISI. (A) A 3D CT rendering of the foreshortened scaphoid (curved arrows) is displayed on a 2D CT reformatted background. (B) A T1-weighted sagittal image illustrates the humpback scaphoid deformity characterized by flexion of the distal pole (curved arrow) relative to the fracture line (straight arrow) and proximal pole. The radioscaphocapitate ligament is not seen, and there is localized synovitis in its expected location. (C) A T1-weighted sagittal image demonstrates DISI secondary to the humpback deformity, and wrist shortening without scapholunate interosseous ligament tear. The dorsal tilt of the lunate (curved arrow) and increased capitolunate angle (double-headed arrow) are indicated. The capitate is dorsally displaced relative to the radius, as is characteristically seen in DISI instabilities. D, dorsal; V, volar.
|
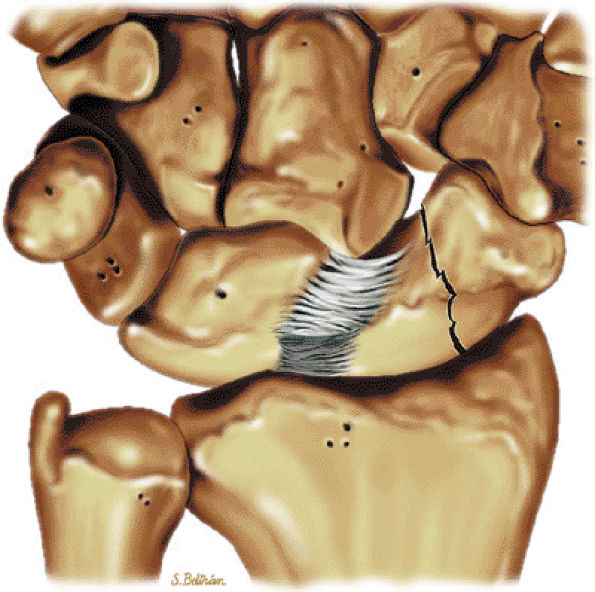 |
|
FIGURE 10.158 ● Middle-third scaphoid waist fracture. The scaphoid is unique in its relationship to the distal radius, distal carpal row, and volar carpal ligaments and is more susceptible to injury than the other carpal bones. Coronal color illustration.
|
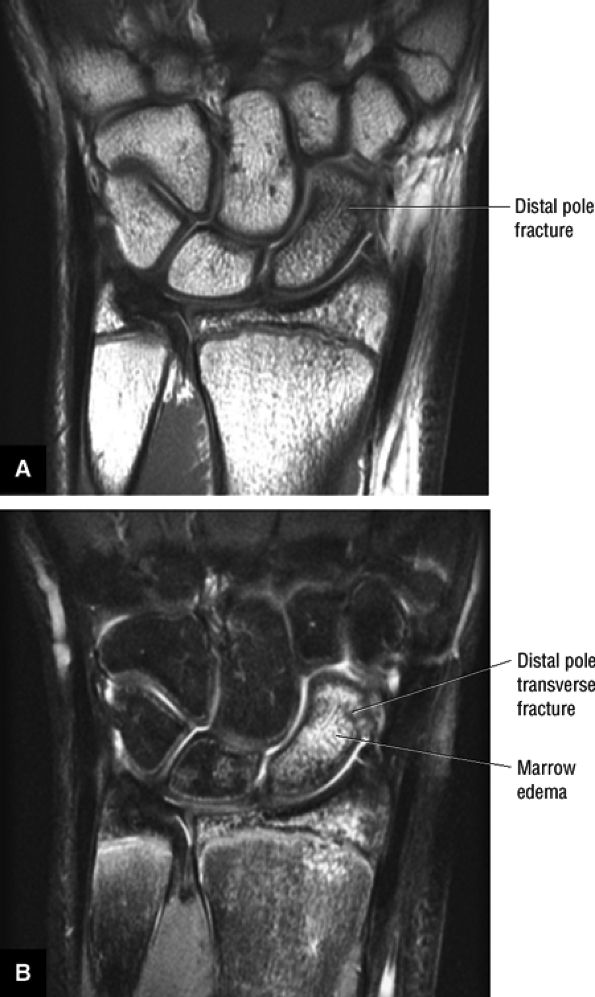 |
|
FIGURE 10.159 ● Distal-pole scaphoid fracture. Distal-pole scaphoid fractures are more commonly seen in children. (A) Coronal T1-weighted image. (B) Coronal FS PD FSE image.
|
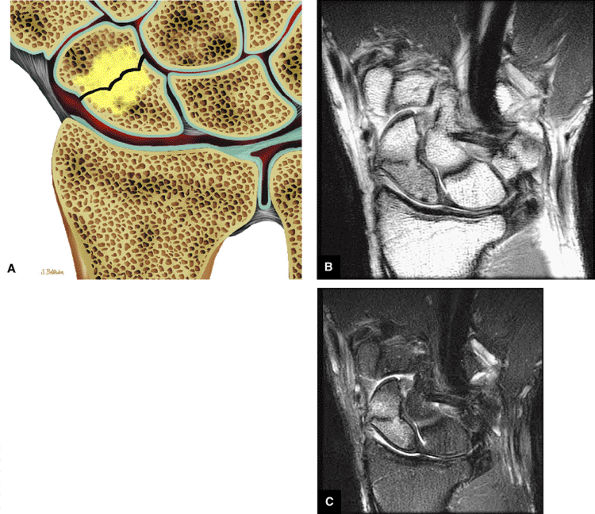 |
|
FIGURE 10.160 ● (A) Marrow edema on both proximal and distal sides of a scaphoid fracture. Coronal color illustration. Coronal T1-weighted (B) and FS PD FSE (C) images with hypointense fracture line associated with adjacent marrow edema, which is hypointense on the T1-weighted image and hyperintense on the FS PD FSE image.
|
via the dorsal ridge from branches of the radial artery. Thus, with fractures through the waist of the scaphoid, blood supply to the proximal pole is poor, accounting for the high rate of AVN and delayed healing (see more detailed discussion on AVN and nonunion of the scaphoid below). Associated injuries such as scapholunate dissociation and capitate head shear fracture and triquetral fracture also affect healing. Other complications of scaphoid fractures include deformity (including the humpback deformity), carpal instability (DISI), secondary osteoarthritis and other degenerative changes, carpal tunnel syndrome, sympathetic dystrophy, and pseudoarthrosis at the fracture site.
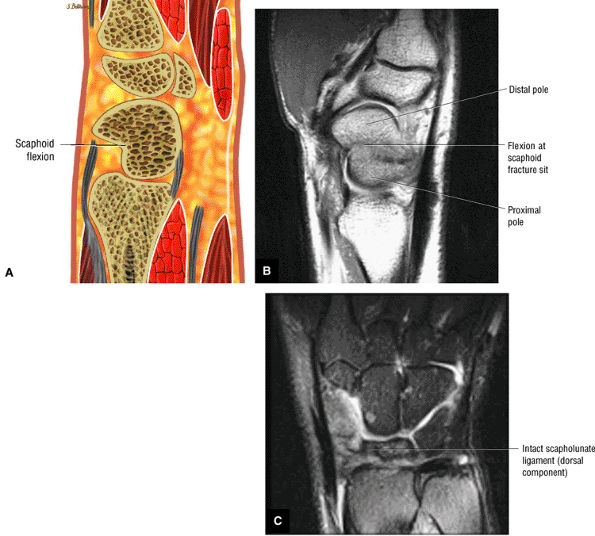 |
|
FIGURE 10.161 ● Scaphoid flexion on color sagittal illustration (A) and T1-weighted sagittal image (B). (C) The dorsal fibers of the scapholunate ligament are intact, as shown on this coronal FS PD FSE image.
|
-
Stage I: Scaphoid dislocation or instability with scapholunate interosseous and radioscaphoid ligament injury
-
Stage II: Capitate dislocation and opening of the space of Poirier
-
Stage III: Triquetral dislocation and radiotriquetral ligament failure
-
Stage IV: Radiocapitate, radiotriquetral, and dorsal radiocarpal ligament failure with lunate dislocation
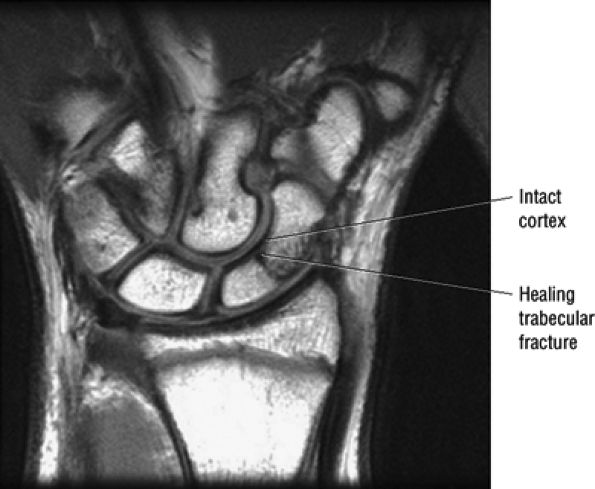 |
|
FIGURE 10.162 ● Subacute scaphoid fracture without discontinuity of cortical margins. Coronal T1-weighted image.
|
 |
|
FIGURE 10.163 ● Internal fixation of proximal pole scaphoid fracture. Smooth Kirschner (K) wire fixation or Herbert's screw techniques have been used. Bone grafting is used for nonunions and comminuted fractures. (A) Coronal T1-weighted image. (B) Sagittal FS PD FSE image.
|
 |
|
FIGURE 10.164 ● Silastic implant of the proximal pole of the scaphoid. Silicone synovitis may complicate this type of implant replacement arthroplasty. Coronal T2* gradient-echo image.
|
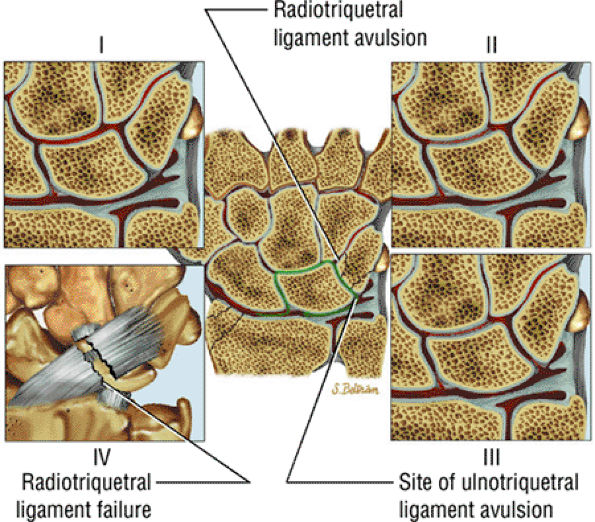 |
|
FIGURE 10.165 ● Perilunate patterns of instability. Stage I is scapholunate failure, stage II is capitolunate failure, stage III is triquetrolunate failure (with triquetral dislocation and radiotriquetral ligament failure), and stage IV is dorsal radiocarpal ligament failure resulting in volar rotation of the lunate. Color coronal color illustrations.
|
this intermediate stage of injury carpal displacements are halfway between a perilunate and lunate dislocation. The capitate is partially dorsal to the longitudinal axis of the radius and the lunate is angulated volarly but not completely dislocated. In dorsal transscaphoid perilunate dislocation there is an associated fracture of the waist of the scaphoid. In the less common volar perilunate and volar transscaphoid perilunate dislocation, the lunate is palmarly flexed and the capitate is displaced volarly (Fig. 10.168). Volar transscaphoid perilunate dislocation is usually widely displaced and is typically more unstable than its dorsal counterpart.
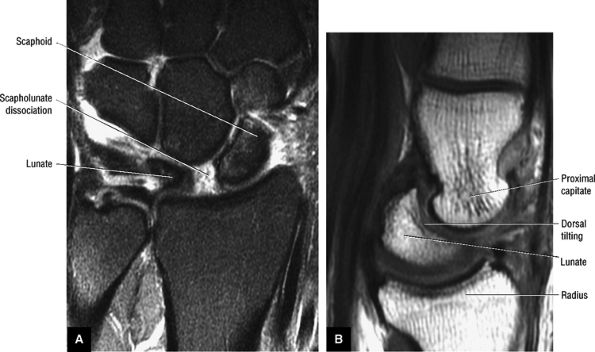 |
|
FIGURE 10.166 ● Scapholunate dissociation (A) associated with dorsal tilting of the lunate in a DISI deformity (B). (A) Coronal FS PD FSE image. (B) Sagittal T1-weighted image.
|
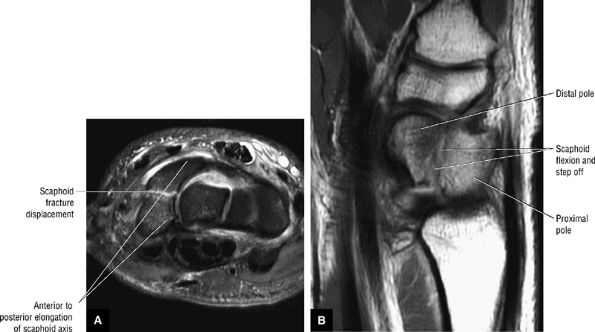 |
|
FIGURE 10.167 ● Unstable scaphoid fracture with greater than 1 mm of step-off at the fracture site. The scaphoid is elongated in the axial plane secondary to flexion. Scaphoid displacement indicates instability, usually from an incomplete or spontaneously reduced perilunate dislocation.
|
T1-weighted images display a larger surface area of the pisiform bone, minimizing the partial volume effect that may complicate coronal images.
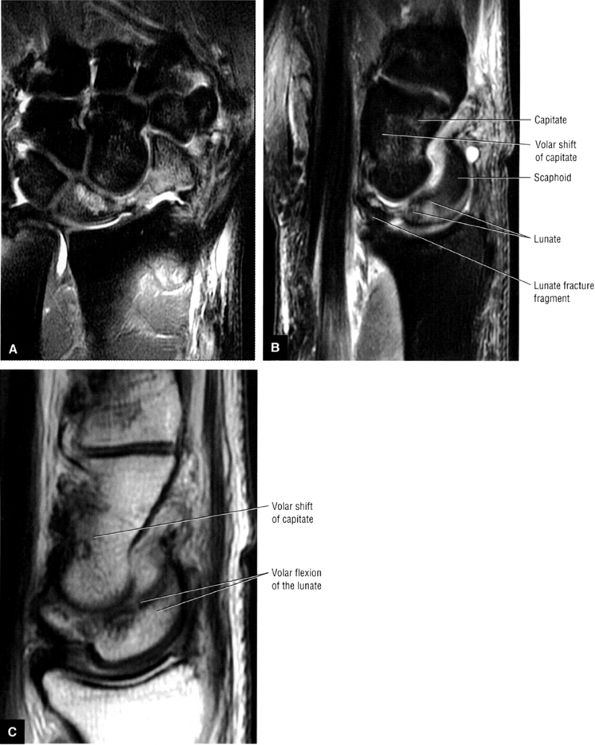 |
|
FIGURE 10.168 ● Volar transscaphoid perilunate dislocation associated with a scaphoid fracture, scapholunate dissociation, lunate volar flexion, and a volar shift of the capitate. This injury pattern is less common than dorsal transscaphoid perilunate dislocation. (A) Corcnal FS PD FSE image. (B) Sagittal FS PD FSE image. (c) Sagittal T1-weighted image.
|
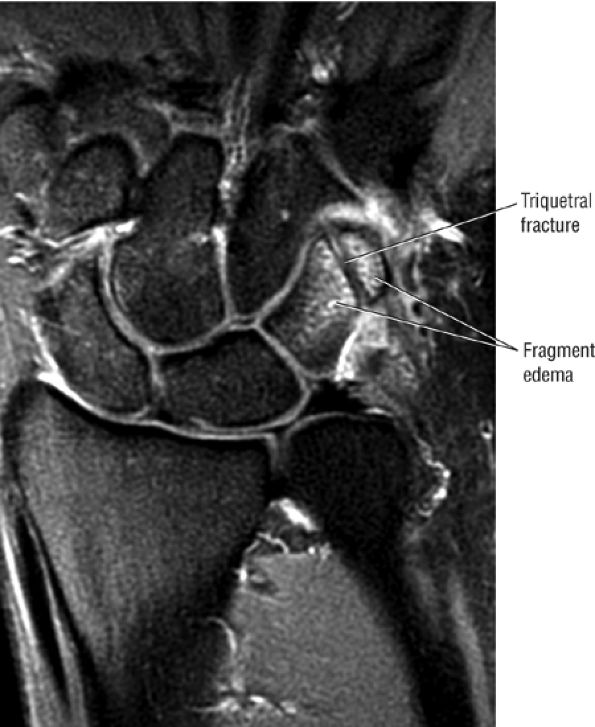 |
|
FIGURE 10.169 ● Triquetral fracture of the distal pole on a coronal FS PD FSE image.
|
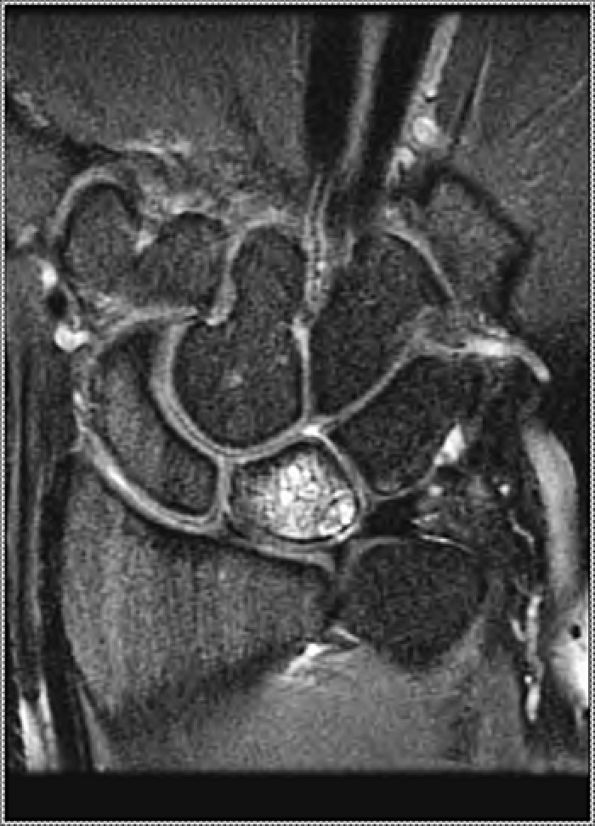 |
|
FIGURE 10.170 ● Eccentric volar ulnar-sided lunate fracture unrelated to Kienböck's disease. Volar-pole fractures of the lunate represent the most common non-Kienböck's related fracture pattern. Coronal FS PD FSE image.
|
-
A bipartite hook or os hamuli proprium (incomplete fusion of ossification center of hook) may mimic a fracture.
-
Both axial and sagittal images should be obtained before excluding a fracture.
-
Other causes of ulnar-sided pain should be evaluated, including the lunotriquetral ligament in cases of chronic or healing hamate fractures.
sports-related injuries; the nondominant hand may be involved with other causes.
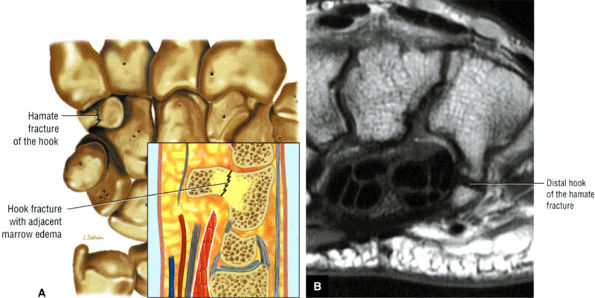 |
|
FIGURE 10.171 ● Fracture of the hook of the hamate on (A) a coronal illustration with sagittal inset and (B) an axial T1-weighted image. Hamate fractures may involve either the body or the hook.
|
-
Hypoimense or hyperintense fracture line (Fig. 10.173)
-
A transverse fracture line of trie hook on axial images and a vertical line on sagittal images
-
Marrow edema of the hook or body in acute injury
-
Displacement of hook fractures (seen on axial or sagittal plane images)
-
Displacement of articular fractures
-
Associated osteochondral fractures
-
Effacement of the ulnar aspect of the carpal tunnel at the level of the ulnar-sided flexor digitorum profundus tendons
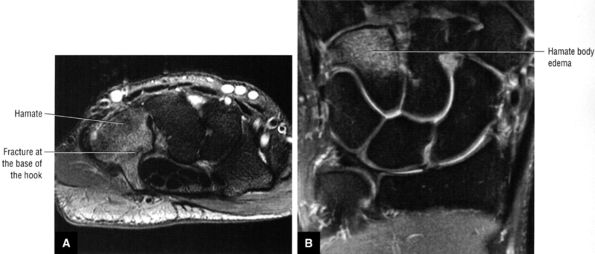 |
|
FIGURE 10.172 ● Marrow edema is hyperintense on FS PD FSE axial (A) and coronal (B) images of a hamate hook fracture at the junction of the hook and body of the hamate.
|
-
Associated marrow edema is best seen on coronal FS PD FSE or STIR images.
-
There may be displacement at the fracture site or DISI deformity
-
The triquetrum, lunate, and proximal scaphoid fragments slide volarly into extension in stage I perilunar instability.
-
SLAC plus scaphoid nonunion presents as a scaphoid nonunion advanced collapse, or SNAC lesion.
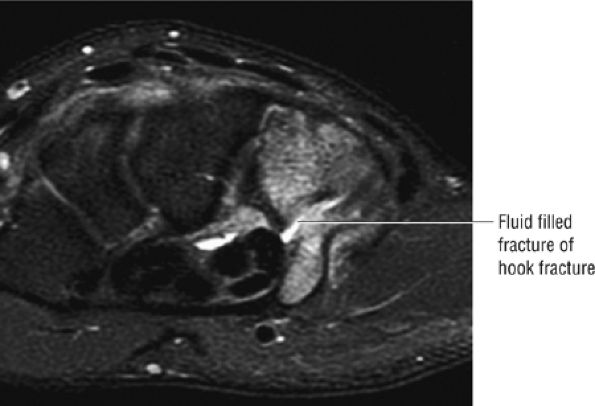 |
|
FIGURE 10.173 ● Hyperintense fluid in the hook of the hamate fracture site. Hook fractures are associated with falls, direct trauma, and striking a ball with a club (golf) or racquet (tennis). Axial FS PD FSE image.
|
 |
|
FIGURE 10.174 ● Transverse fracture through the body of the capitate. These fractures may be isolated or occur in association with perilunate dislocation (A) Coronal T1-weighted image. (B) Coronal FS PD FSE image.
|
-
Hypointensily in the proximal pole on both T1-weighted and FS PD FSE images (Figs. 10.177 and 10.178). In diffuse marrow necrosis, low-signal-imensity marrow may not be restricted to the proximal pole.
-
Localized fluid accumulation and limited marrow edema of the proximal pole
-
Reactive marrow hyperemia of the distal pole, which should not be confused with diffuse changes of necrosis
-
Fluid separating fracture fragments
-
Nonunion is characterized by persistent hypointensity on T1, FS PD FSE, and post-contrast FS T1-weighted images (see more detailed discussion below on nonunion of the scaphoid).
-
Fracture healing demonstrates hyperemia at the fracture site and adjacent marrow.
-
Callus or fibrous union may also demonstrate hypointensity on T1-weighted or FS PD FSE images.
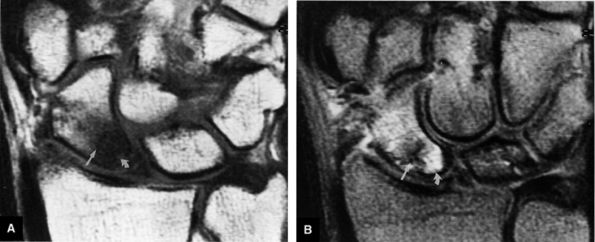 |
|
FIGURE 10.175 ● A scaphoid fracture with AVN (curved arrow) of the proximal pole is hypointense on a T1-weighted coronal image (A) and hyperintense in hyperemic viable bone on a FS PD FSE coronal image (B). The fracture line (straight arrow) remains hypointense on both pulse sequences. The FS PD FSE image is also more sensitive than the T1 -weighted image in detecting distal-pole marrow edema.
|
-
Type 1: Simple nonunion; it is nondisplaced and there are no degenerative changes
-
Type 2: Unstable nonunion (see Fig. 10.179), with displacement (more than 1 mm) or DISI (SL angle greater 70°), but no degenerative changes
-
Type 3: Early arthritic nonunion with radioscaphoid arthritis
-
Type 4: SNAC wrist (Fig. 10.180)
-
Type 5: Scaphoid nonunion advanced collapse-plus (SNAC plus), and there is arthritis throughout the wrist.
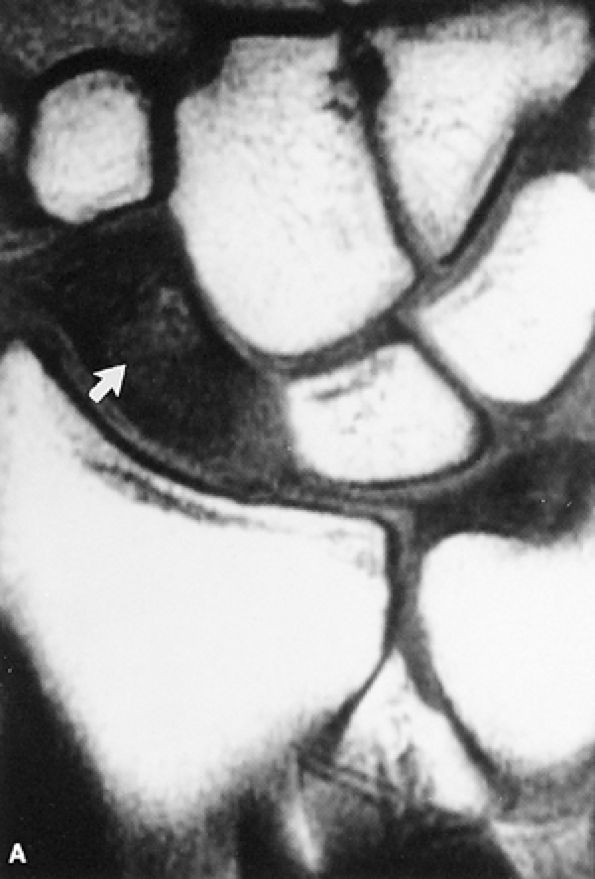 |
|
FIGURE 10.176 ● Preiser's disease. A T1-weighted coronal image shows a low-signal-intensity sclerotic scaphoid (arrow) without an identifiable fracture site.
|
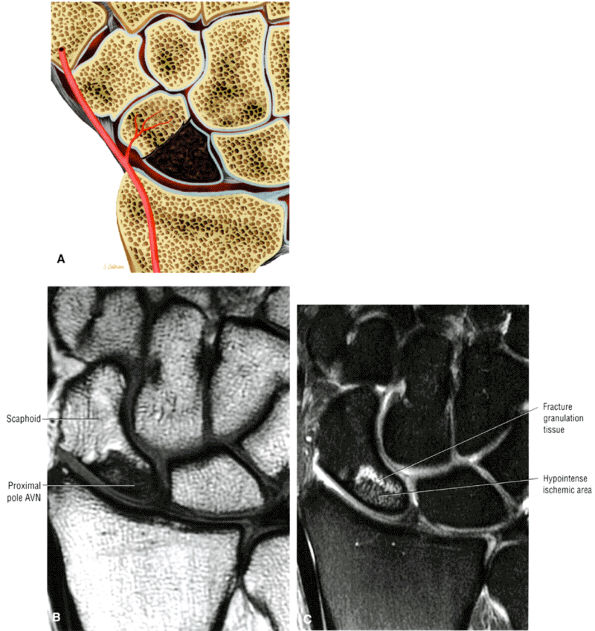 |
|
FIGURE 10.177 ● (A) Coronal illustration shows a fracture of the waist of the scaphoid with AVN of the proximal pole. The vascular supply to the proximal pole occurs via the radial artery from the distal pole. Chronic proximal-pole AVN with hypointense marrow is shown on coronal T1-weighted (B) and FS PD FSE (C) images.
|
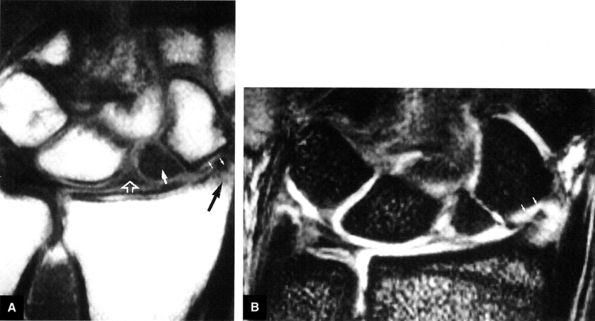 |
|
FIGURE 10.178 ● AVN of the scaphoid, with early SLAC wrist (A) A low-signal-intensity “corner sign” of radial styloid subchondral sclerosis (black arrow) is seen in the presence of scaphoid nonunion and AVN of the proximal pole (large white arrow) on a T1-weighted coronal image. There is mild narrowing of the radioscaphoid articulation with respect to the distal pole (small white arrows). The scapholunate interosseous ligament is intact (open arrow). (B) Attenuated articular cartilage is seen in the proximal aspect of the distal pole of the scaphoid in early SLAC degeneration (arrows) on a T2*-weighted coronal image. The radiolunate joint is characteristically unaffected.
|
-
Hypointensity across the fracture site on T1- or PD-weighted images
-
Displacement with a cortical offset of 1 mm or more
-
DISI on sagittal images
-
Dorsal gap on sagittal images through the scaphoid
-
Loss of coaptation of scaphoid fracture fragments
-
Instability between proximal and distal carpal rows
-
Increased scapholunate and capitolunate angles on sagittal images
-
Trabecular erosion with a volar defect at the fracture site associated with scaphoid angulation
-
Proximal-pole AVN
-
Pseudoarthrosis
-
Degenerative loss of joint space (chondral loss) in the radioscaphoid, scaphocapitate, and capitolunate joints
-
SNAC
-
Viable marrow in the acute/subacute phase; nonviable marrow in chronic nonunion
-
Diffuse marrow hyperintensity on FS PD FSE images, possibly representing proximal-pole ischemia and reactive edema of the distal pole
is necessary. The specific procedure depends on the classification of nonunion:
-
Type 1 simple nonunion may be treated with an inlay bone graft.
-
Type 2 unstable nonunion requires a volar wedge graft.
-
Type 3 nonunion is treated with a wedge graft, ORIF, and styloidectomy.
-
Type 4 (SNAC wrist) is treated with midcarpal fusion and scaphoid excision.
-
Type 5 (SNAC-plus) is treated with arthrodesis.
 |
|
FIGURE 10.179 ● Scaphoid nonunion with persistent hyperintense fracture gap on coronal T1-weighted (A) and FS PD FSE (B) images.
|
-
Lunate sclerosis or marrow edema is centrally located and not ulnar-sided or eccentric
-
Kienbock's disease frequently presents without a defined transverse fracture in the initial stages.
-
FS PD FSE or STIR sequences should be routinely performed to identify marrow edema.
-
Anteroposterior elongation of the lunate is evaluated in the sagittal plane in stage III Kienböck's disease.
-
Y pattern, present in approximately 60% of individuals
-
I pattern, present in approximately 30%
-
X pattern, present in approximately 10%
techniques and measurement methods, this correlation has withstood the test of time. The association between a short ulna and Kienböck's disease is not absolute. Although exceedingly uncommon, Kienböck's disease may also occur in patients with neutral or positive ulnar variance. The significance of negative ulnar variance is that it subjects the lunate to an increased mechanical load compared with that associated with neutral or positive ulnar variance.
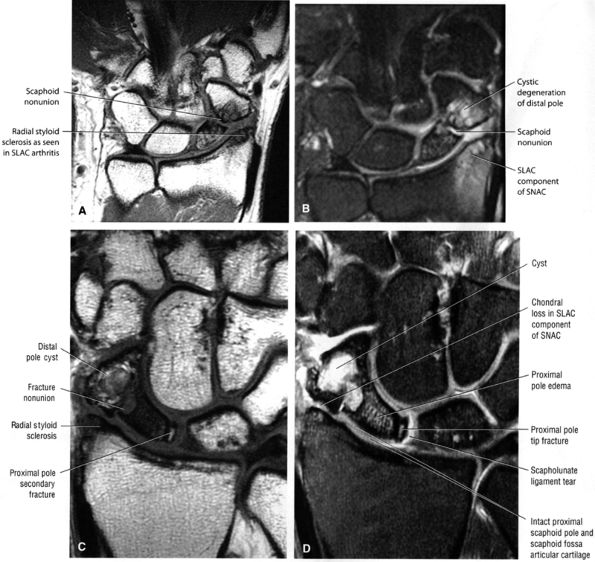 |
|
FIGURE 10.180 ● Scaphoid nonunion advanced collapse (SNAC), with components of both a scaphoid nonunion and SLAC arthntis. SNAC is considered a greater arc injury. (A) Coronal T1-weighted image. (B) Coronal FS PD FSE image. (C, D) In a separate case. SNAC wrist demonstrates features of early SLAC arthritis (stage I) with distal-pole scaphoid-radial styloid arthrosis, fracture nonunion, and AVN of the scaphoid proximal pole. The smaller proximal-pole scaphoid fragment adjacent to the scapholunate interval is a secondary sign of scaphoid instability. (C) Coronal T1- weighted image. (D) Coronal FS PD FSE image.
|
 |
|
FIGURE 10.181 ● Kienböck's disease. (A) An AP radiograph displays sclerosis and collapse of the lunate (arrows) associated with negative ulnar variance. (B) The corresponding T1 -weighted coronal image shows a low-signal-intensity necrotk lunate (open arrow), a disrupted scapholunate ligament (large solid arrow), and an intact TFC (small solid arrows).
|
unilateral, although there are incidences of bilateral disease. Kienböck's disease is a great dissembler, and a number of other conditions should be considered. Any history of trauma should be carefully elicited.
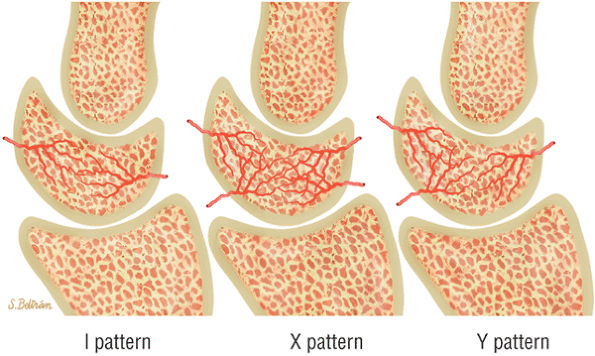 |
|
FIGURE 10.182 ● Three patterns of the interosseous vascular supply of the lunate. Acute trauma or repeated microtrauma with excessive shear force results in interruption of the blood supply to a lunate susceptible to or at risk for Kienböck's disease. A single nutrient vessel or compromised intraosseous blood supply places the lunate at risk. Sagittal color illustrations.
|
-
Stahl's classification, based on clinical and radiographic criteria
-
Decoulx's modification of Stahl's system, in which the presence of a fracture is not required in early stages
-
Lichtman's staging classification, which involves three stages described in detail below
-
An MR classification based on Lichtman stage II (discussed later under MR appearance)
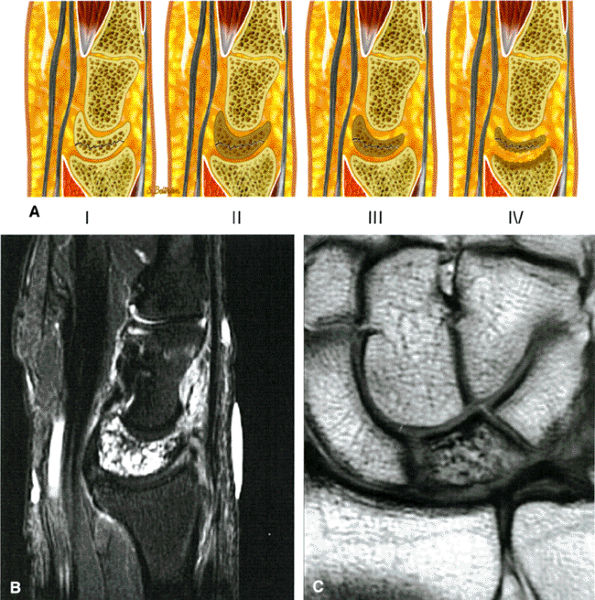 |
|
FIGURE 10.183 ● The four stages of Kienböck's disease. In contrast to stages I and II, stages III and IV are characterized by lunate collapse in the coronal plane and elongation of the lunate in the sagittal plane. Associated findings (in stage III and IV) include proximal migration of the capitate, scapholunate dissociation, scaphoid flexion, and ulnar migration of the triquetrum. Stage IV has generalized degenerative changes of the carpus. Extensive lunate marrow edema is associated with stage I Kienböck's disease. (A) Sagittal color illustration. (B) Sagittal FS PD FSE image. (C) Coronal T1-weighted image.
|
-
Stage IIA: A focal area of central hypointnsity on T1- weighted images that increases on T2-weighted images
-
Stage IIB: A focal area of central hypointnsity on both T1- and T2-weighted sequences
-
Stage IIC: Generalized hypointensity on T1-weighted images that increases on T2- weighted images
-
Stage IID; Generalized hypointensity on T1- and T2-weighted images
the capitate. The absence or presence of scapholunate dissociation with rotatory subluxation of the scaphoid divides patients into stage IIIA and IIIB, respectively. Rotation of the scaphoid may be accompanied by ulnar deviation of the triquetrum. With scaphoid rotation, the inability to see the entire long axis of the scaphoid in a single coronal image is the MR equivalent of the radiographic “ring” sign on conventional AP radiographic projections. Articular cartilage degeneration can be identified in this stage.123
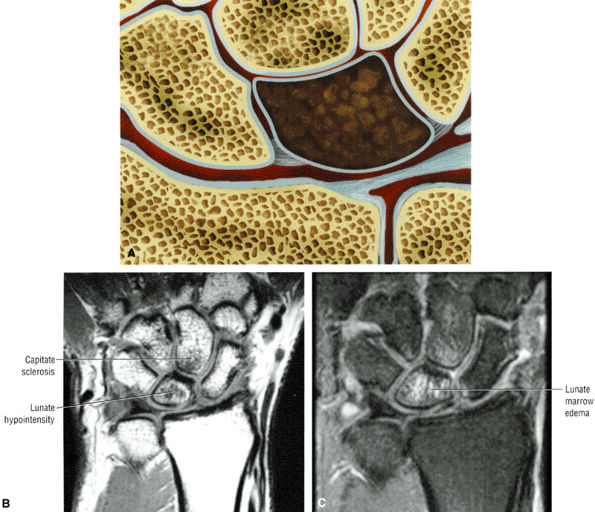 |
|
FIGURE 10.184 ● Stage I Kienböck's disease without visible fracture line. (A) Color coronal illustration. (B) Coronal T1-weighted image. (C) Coronal FS PD FSE image.
|
distends synovial recesses. Pannus tissue is low to intermediate in signal intensity on T1- weighted and FS PD FSE images and enhances with gadolinium intravenous contrast.
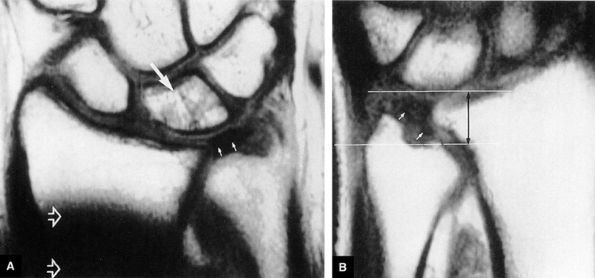 |
|
FIGURE 10.185 ● (A) Recovering fatty marrow signal intensity (large arrow) is present after treatment of stage I Kienböck's disease of the right wrist. The lunate and TFC (small arrows) are normal. A low-signal-intensity postoperative artifact secondary to radial shortening is present (open arrows). (B) The untreated left wrist shows severe negative ulnar variance (black double-headed arrow) and a deformed but intact TFC (white arrows). The lunate marrow is unaffected.
|
-
Stage I
-
A hypointense to hyperintense transverse fracture line (Fig. 10.189)
-
Microtrabecular compression fractures, more common than well-defined transverse fracture
-
Marrow hyperintensity on FS PD FSE images (see Fig. 10.184)
-
Intermediate-signal-intensity synovitis on FS PD FSE images
-
-
Stage II
-
Centralized to diffuse marrow hypointensity on T1- and PD-weighted images (see Fig. 10.181)
-
Intact shape of lunate
-
Subtle collapse (stage II) of lunate on radial border on coronal images
-
Hypointense to hyperintense fracture lines, if present
-
Viable marrow hyperintense on FS PD FSE or STIR images
-
Decreased height of the radial aspect of the lunate on coronal and sagittal images
-
-
Stage III
-
Lunate collapse plus proximal migration of capitate
-
Anteroposterior elongation of lunate in sagittal plane
-
Proximal migration of capitate on coronal images
-
Associated scapholunate dissociation with hyperintensity of the scapholunate ligament on FS PD FSE images
-
-
Stage IV
-
Sclerosis plus osteophyte formation and areas of reactive marrow degeneration
-
Loss of articular cartilage in radiocarpal and midcarpal articulations
-
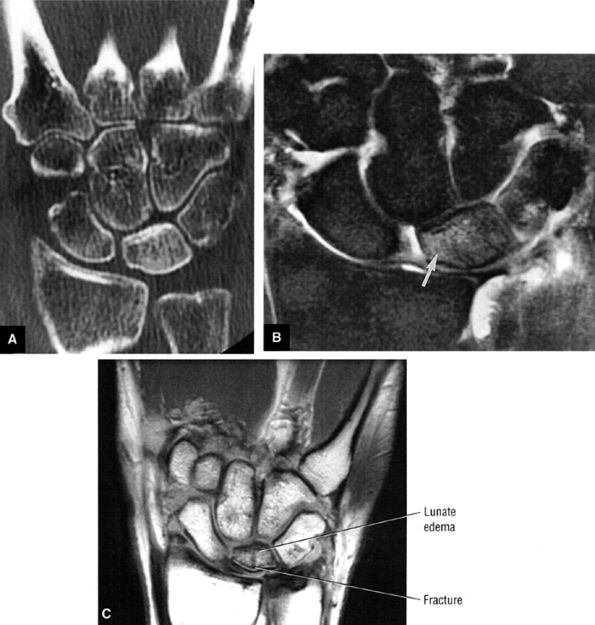 |
|
FIGURE 10.186 ● Stage II Kienböck's disease with (A) increased lunate density (sclerosis) on coronal reformatted CT scan and (B) corresponding marrow hyperintensity on fast STIR coronal image. (C) A separate case of stage II Kienböck's disease with visible proximal subchondral fracture line
|
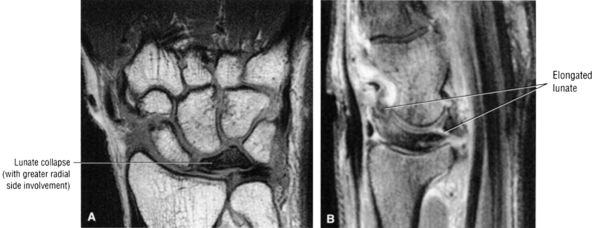 |
|
FIGURE 10.187 ● Stage III Kienböck's with lunate collapse identified in both coronal and sagittal planes. (A) Coronal T1-weighted image. (B) Sagittal FS PD FSE image.
|
shortening, with or without revascularization with a vascular pedicle, can be used to unload and revascularize the lunate. Radial shortening is substituted for capitate shortening in the patient with negative ulnar variance. During revascularization. every attempt should be made to reconstruct the lunate. When the dorsal cortex is entered, the collapsed articular surface can be elevated and buttressed with a bone graft. The vascular pedicle is then inserted.
 |
|
FIGURE 10.188 ● Stage IV Kienböck's disease with lunate collapse and associated degenerative changes. (A) Coronal T1-weighted image. (B) Coronal T2*-weighted image.
|
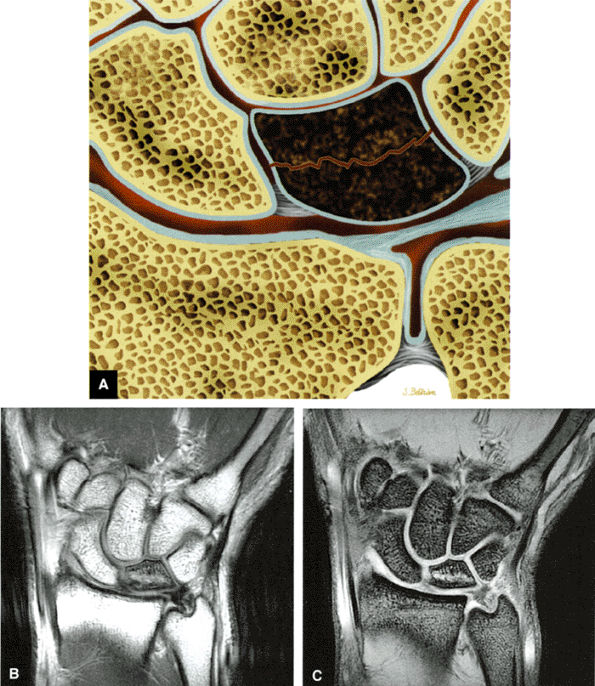 |
|
FIGURE 10.189 ● Discrete transverse fracture line associated with stage I Kienböck's disease. (A) Coronal color illustration. (B) Coronal T1-weighted image. (C) Coronal T2* gradient-echo image.
|
carpectomy can be performed. Because of the tenuous vascular supply of the lunate, there is usually degeneration in the lunate fossa, although occasionally the distal articular surface of the lunate remains serviceable. In these cases, a radioscapholunate fusion may preserve motion at the intercarpal joint. This is not common, however, and arthritic degeneration is usually so advanced throughout the carpus that there is no choice but to perform a panarthrodesis of the wrist. Although there is a total loss of wrist motion, the patient is usually quite happy because of the pain relief.
-
Thenar muscle hyperintensity (atrophy or denervation) is seen in assoication with positive median nerve findings.
-
There may be partial to complete involvement of median nerve fascicles.
-
Triscaphe volar ganglions may compress the deep surface of the carpal tunnel.
-
The carpus has a concave bony contour on its flexor surface and is covered by the flexor retinaculum (Fig. 10.190).
-
The bony carpus forms the floor and walls of the carpal tunnel, with the rigid flexor retinaculum as its roof (Fig. 10.191).
-
The flexor retinaculum, or transverse carpal ligament, attaches to the tubercle of the scaphoid, the ridge of the trapezium, and the ulnar aspect of the hook of the hamate and pisiform.
-
The long flexors of the fingers and thumb pass through the carpal tunnel (Fig. 10.192). The separate flexor digitorum superficialis tendons are arranged in two rows, with the tendons to the middle and ring finger volar to the tendons to the index and little finger. The flexor digitorum profundus tendons are arranged in the same coronal plane, and the tendon to the index finger is separated from the adjacent three profundus tendons. All eight flexor tendons are invested in a common synovial sheath. The flexor pollicis longus tendon, invested in its own synovial sheath, is located on the radial aspect of the flexor tendons within the carpal tunnel.
-
The median nerve is deep to the flexor retinaculum and is seen on the lateral side of the flexor digitorum superficialis between the flexor tendon of the middle finger and the flexor carpi radialis.
-
The proximal fibers of the volar carpal ligament contribute to the roof of the carpal tunnel, although this contribution is not as significant as that of the thicker flexor retinaculum.
-
In dorsiflexion and palmarflexion of the wrist, the median nerve is forced against the transverse carpal ligament. This is compounded by friction forces between the median nerve tendons and the transverse carpal ligament during flexion and extension, with up to 20 mm of excursion of the median nerve.
 |
|
FIGURE 10.190 ● The flexor retinaculum (transverse carpal ligament) completes the boundary of the carpal tunnel on the palmar side.
|
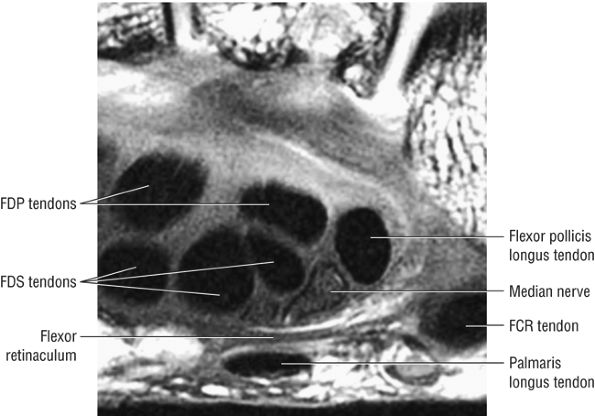 |
|
FIGURE 10.191 ● Flexor retinaculum at the level of the pisiform. The flexor retinaculum holds the flexor tendons in place during wrist flexion to prevent bowstringing and loss of power. FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis; FCR, flexor carpi radialis. Axial T1-weighted image.
|
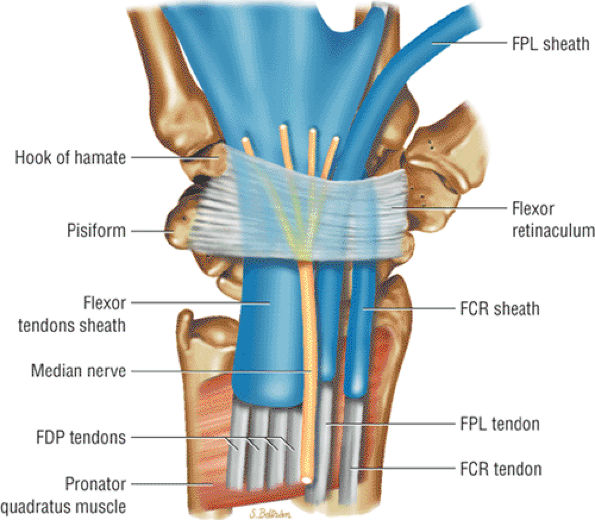 |
|
FIGURE 10.192 ● The relationship of the flexor tendons, median nerve, and flexor retinaculum shown on a coronal color illustration. The flexor retinaculum is under constant tension and helps maintain the contour of the carpal arch. FDP, flexor digitorum profundus; FCR, flexor carpi radialis; FPL, flexor pollicis longus.
|
flexor digitorum superficialis tendon of the index finger. In wrist flexion, the median nerve can be found anterior to the flexor retinaculum or between the flexor digitorum superficialis tendons of the index finger and thumb or middle and ring fingers. In the flexed position, there is flattening of the elliptical shape of the median nerve. Alteration of morphology is less significant in wrist extension. The morphology of the median nerve may also change with involvement by benign peripheral nerve sheath tumors. These lesions may present extrinsic to the median nerve (schwannoma) or may not be separate from the median nerve fascicles (neurofibroma) (Fig. 10.194).
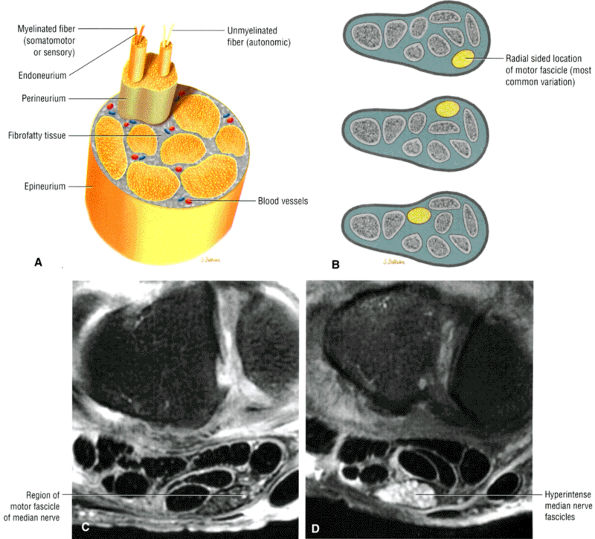 |
|
FIGURE 10.193 ● (A) Anatomy of a peripheral nerve demonstrating myelinated and unmyelinated axons. The perineurium binds the separate nerve fascicles together. Axial color cross-section. (B) Variation in the position of the motor fascicle within the cross-section of the median nerve. Axial color cross-section. (C) Normal fascicles of the median nerve on an axial FS PD FSE image. (D) Hyperintense fascicles of the median nerve on an axial FS PD FSE image.
|
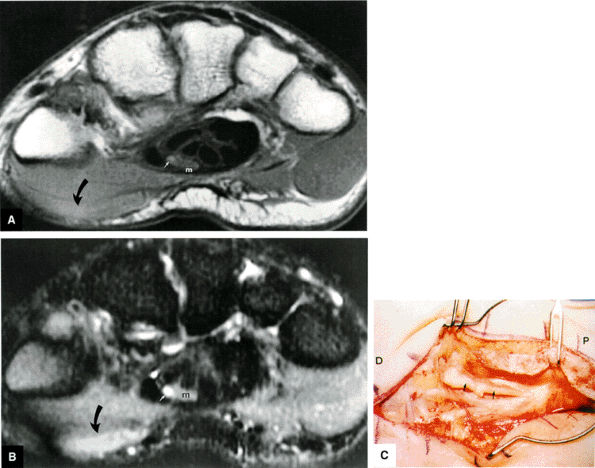 |
|
FIGURE 10.194 ● Neurofibroma (small straight arrow) of the motor branch of the median nerve (m) demonstrates intermediate signal intensity on T1-weighted axial image (A) and hyperintensity on (curved arrow) (corresponding to the affected motor branch of the median nerve) demonstrates increased signal intensity on T1-weighted and STIR axial images. (B). Thenar muscle denervation (curved arrow) (corresponding to the affected motor branch of the median nerve) demonstrates increased signal intensity on T1-weighted and STIR axial images. Surgical photograph (C) shows the tumor (arrow) in situ. D, distal; P, proximal.
|
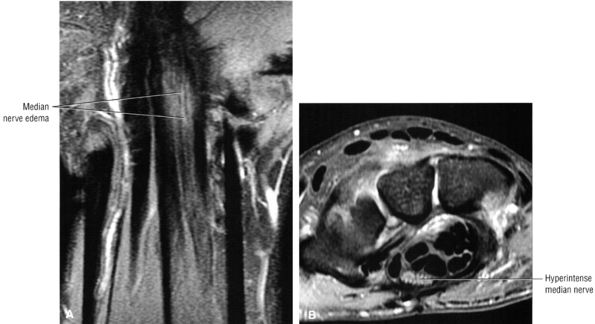 |
|
FIGURE 10.195 ● Carpal tunnel syndrome with hyperintense median nerve at the level of the distal carpal row. (A) Coronal FS PD FSE image. (B) Axial FS PD FSE image.
|
-
Fractures and dislocation about the wrist (e.g., Colles' fracture), which result in decreased volume of the carpal tunnel or direct nerve trauma
-
Inflammatory processes (Fig. 10.196), such as rheumatoid arthritis, gout and pseudogout, and amyloidosis
-
Median nerve tumors131 including neurilemmomas (schwannomas) (Fig. 10.197), fibromas, and hamartomas (Fig. 10.198)
-
Tumors (space-occupying), including ganglions (Fig. 10.199), lipomas (Fig. 10.200), and hemangiomas
-
Intraneural hemorrhage
-
Infection
-
Infiltrative disease
-
Soft-tissue injuries
-
Anomalous muscles,132 which act as a space-occupying mass (Fig. 10.201)
-
Pain and numbness or tingling in the median nerve distribution with increased nocturnal pain and/or burning (can be classified as mild, moderate, or severe based on electrodiagnostic data or by severity of clinical symptoms)
-
Involvement of the thumb, index, middle fingers, and radial half of the ring finger is most common.
-
Sensory findings ranging from minimal hypesthesia to complete anesthesia
-
Muscle atrophy and loss of function are usually late findings, although abductor pollicis brevis involvement and opponens weakness may be seen earlier (opponens atrophy is a late finding).
-
Positive clinical tests for nerve entrapment:
-
Tinel's sign (i.e., paresthesias reproduced by tapping over the median nerve), indicating nerve entrapment
-
Phalen's test (i.e., symptoms produced after 30 seconds with the wrist in forced palmarflexion)
-
Carpal tunnel compression tests (i.e., symptoms produced by manual compression with the wrist in flexion, most accurate)
-
Prolonged sensory conduction or distal motor latency tests (electrodiagnostic tests in patients with carpal tunnel syndrome are reported to be 85% to 90% accurate, with a false-negative rate of 10% to 15%)
-
Semmes-Weinstein monofilament test with the wrist in both neutral and flexed positions
-
Kimura inching technique
-
Ring finger differential measurements
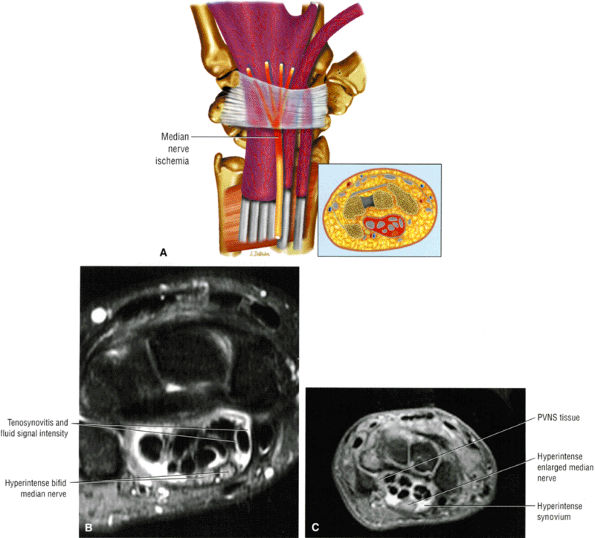 |
|
FIGURE 10.196 ● Tenosynovitis (fibrosynovial) with symptoms of carpal tunnel syndrome. (A) Coronal color illustration. (B) Axial FS PD FSE image. (C) Axial FS PD FSE in a separate case of pigmented villonodular synovitis. Connective tissue degeneration, edema, and vascular sclerosis occur with a fibrosynovial noninflammatory synovium. True tenosynovitis is less common.
|
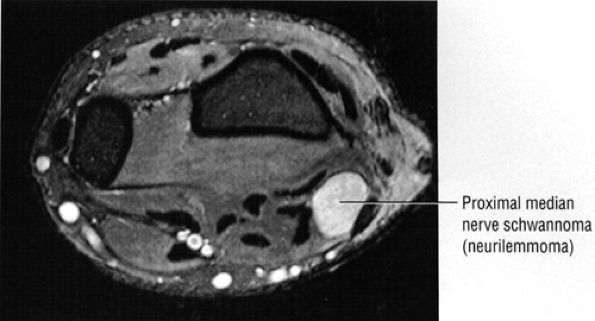 |
|
FIGURE 10.197 ● Benign peripheral nerve sheath tumor of the median nerve proximal to the carpal tunnel on an axial FS PD FSE image.
|
-
Cross-sectional enlargement and hyperintensity of the median nerve on FS PD FSE or STIR images, located deep to the flexor retinaculum
-
Swelling or segmental enlargement of the median nerve, best evaluated at the level of the pisiform
-
Flattening of the median nerve, best demonstrated at the level of the hamate
-
Palmar bowing of the flexor retinaculum, assessed at the level of the hamate.136
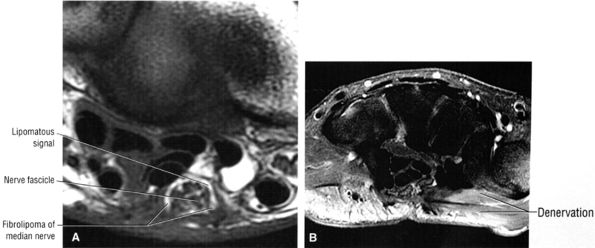 |
|
FIGURE 10.198 ● Fibrolipoma of the median nerve with mixed fat, fibrous, and nerve fascicle signal intensity. Distal thenar muscle denervation is shown. (A) Axial T1-weighted image. (B) Axial FS PD FSE image.
|
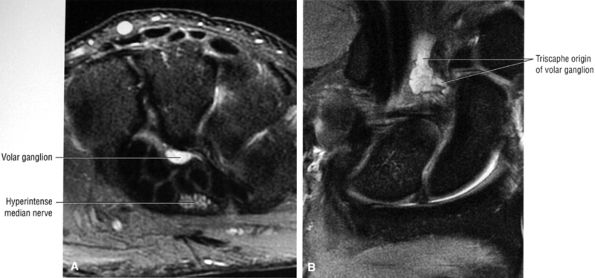 |
|
FIGURE 10.199 ● Volar ganglion extending from the triscaphe articulation deforms the deep carpal tunnel and results in median nerve compromise. (A) Axial FS PD FSE image. (B) Coronal FS PD FSE image.
|
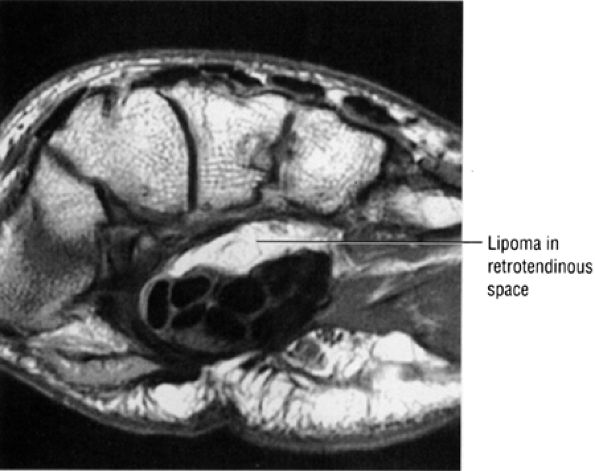 |
|
FIGURE 10.200 ● Lipoma as a space-occupying lesion deep to the carpal tunnel on a T1-weighted axial image.
|
be associated with constriction of the median nerve within the carpal tunnel, distal to the point of swelling.
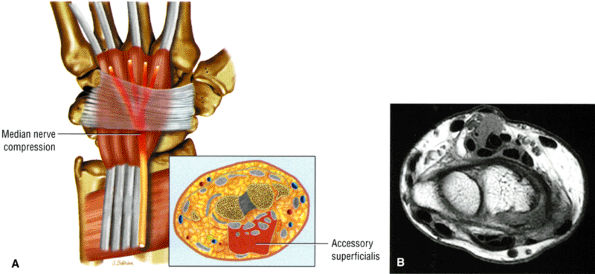 |
|
FIGURE 10.201 ● Accessory flexor digitorum superficialis muscle resulting in median nerve compression on (A) coronal color illustration and (B) axial T1-weighted MR image.
|
-
Swelling or segmental enlargement of the median nerve at the level of the pisiform, intermediate on T1- or PD-weighted images and hyperintense on FS PD FSE images (Fig. 10.202)
-
Flattening of the median nerve at the level of the hamate
-
Palmar bowing of the flexor retinaculum at the level of the hamate
-
Displaced proximal half of a capitate fracture
-
Impingement in perilunar dislocation
-
Fracture of the radius (Colles' or Smith's)
-
Pseudoneuroma (swelling of the median nerve proximal to the carpal tunnel)
-
Ganglions (of triscaphe origin) that project deep to the carpal tunnel and compress the canal (see Fig. 10.199)
-
Thickening of the tenosynovium of the flexor tendons
-
Thenar muscle denervation (Figs. 10.203 and 10.204)
-
Incomplete release of the flexor retinaculum is associated with residual nerve hyperintensity on FS PD FSE images.
volar carpal ligament, with an epineurotomy for thickened or scarred epineurium. Surgical treatment of carpal tunnel syndrome may be complicated by complex regional pain syndrome (reflex sympathetic dystrophy), scar formation, damage to the branches of the median ulnar nerve, tenosynovitis, flexor tendon adhesions, or bowstringing of tendons.
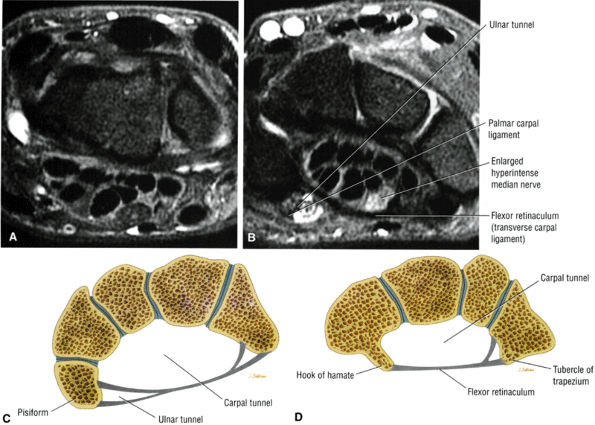 |
|
FIGURE 10.202 ● (A) Normal median nerve signal proximal to the carpal tunnel. Axial FS PD FSE image. (B) Hyperintense enlarged median nerve within the carpal tunnel between the proximal and distal carpal rows. Axial FS PD FSE image. Progressive narrowing of the carpal tunnel from proximal (C) to distal (D). Axial color cross-sections.
|
-
Compression of the ulnar nerve may occur at the entrance to the ulnar tunnel, affecting the superficial branch (sensory) or the deep branch (motor).
-
The deep ulnar nerve supplies motor innervation to the hypothenar, interosseus, third and fourth lumbricals, and adductor pollicis muscles.
-
The superficial ulnar nerve provides sensory innervation to the skin of the hypothenar eminence and the fourth and fifth digits and motor innervation to the palmaris brevis.
tingling of the fifth (little) finger, the ulnar side of the fourth (ring) finger, and the palmar surface from irritation of the ulnar nerve in Guyon's canal. It is seen most frequently in young to middle-aged adults and is less common than median nerve compression or ulnar nerve entrapment at the elbow. It may be associated with sports injuries, and cyclists, golfers, and baseball players are at risk. Ulnar tunnel syndrome is also discussed in Chapter 12.
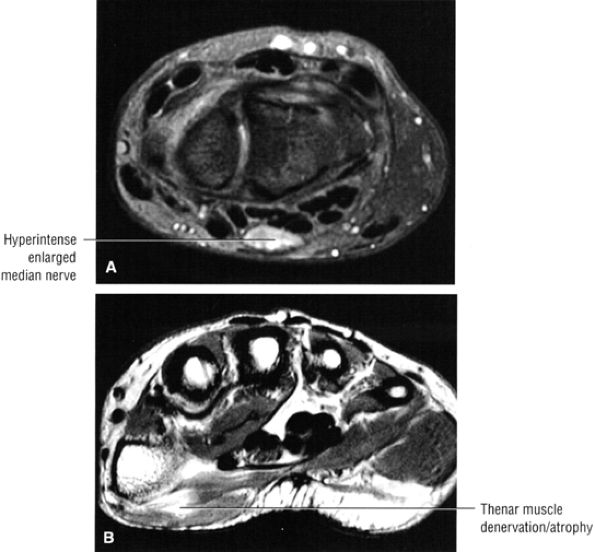 |
|
FIGURE 10.203 ● Carpal tunnel syndrome with enlarged hyperitense median nerve and thenar muscle denervation and atrophy. (A) Axial FS PD FSE image. (B) Axial PD FSE image.
|
-
Sports activities (bicycling, baseball, and golf) that cause intermittent impaction or repetitive flexion/extension of the wrist
-
Soft-tissue tumors such as lipomas142 (Fig. 10.208)
-
Ganglion cysts (Fig. 10.209)
-
Scar tissue
-
Ulnar artery thrombosis or aneurysm (Fig. 10.210) from chronic repetitive trauma (hand tools that vibrate against the hypothenar eminence/the hypothenar hammer syndrome)
-
Carpal fractures (fractures of the hook of the hamate are most common) or distal radius fractures
-
Synovitis
-
Anomalous muscle belly
-
Arthritic changes
present in 15% of the population) may produce anomalous motor and sensory findings, as may a Riche-Cannieu anastomosis, anastomosis between the deep branch of the ulnar nerve and the median nerve in the hand. Histologically there is evidence of increased pressure, impairment of the intraneural microcirculation, and ischemia.
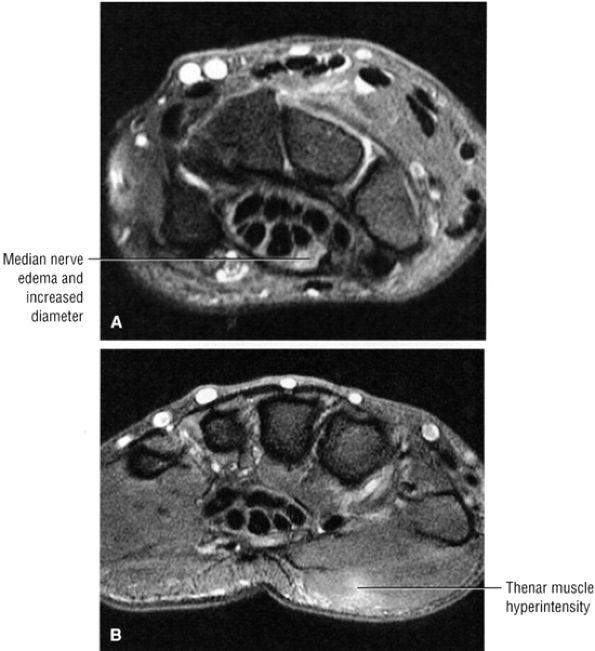 |
|
FIGURE 10.204 ● Median nerve hyperintensity associated with acute thenar muscle denervation prior to fatty atrophy. Axial FS PD FSE images.
|
-
Paresthesias followed by decreased sensation at the fourth and fifth fingers
-
Hand weakness
-
Sensory and/or motor changes depending on the pressure point
-
Positive Tinel's sign over the ulnar nerve
-
Positive Phalen's test with paresthesias in the fourth and fifth fingers
-
Electromyographic and electrodiagnostic testing may show denervation potentials in the interosseus muscle and motor nerve latency prolongation to the first dorsal interossei.
-
Zone I: Proximal to the bifurcation of the deep (motor) branch and the superficial (sensory) branch of the ulnar nerve. Compression in zone I produces motor and sensory deficits and is commonly caused by ganglion cysts or hamate hook fracture.
-
Zone 2: The deep branch; compression produces motor deficits. Compression in zone 2 is also caused by ganglion cysts or fracture of the hook of the hamate.
-
Zone 3: The superficial branch; compression produces sensory deficits. Compression in zone 3 is related to ulnar artery aneurysm or thrombosis.
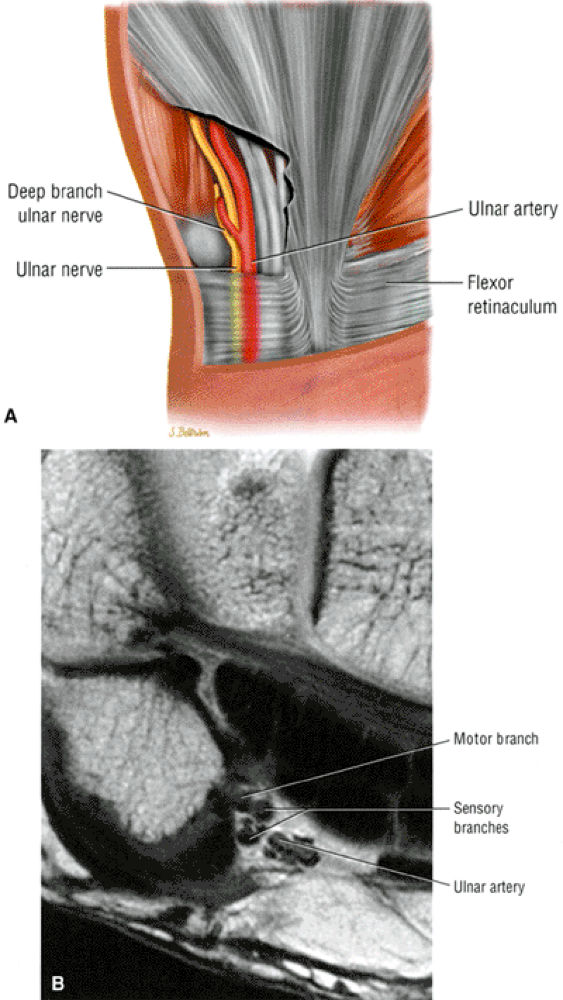 |
|
FIGURE 10.205 ● (A) Coronal color illustration showing ulnar tunnel or Guyon's canal and the relationship of the ulnar nerve. (B) T1-weighted axial image of Guyon's canal containing the ulnar nerve and artery at the level of the distal carpal row. Guyon's canal is formed by the pisiform bone, the flexor retinaculum, and a volar carpal ligament. The separate motor and sensory branches of the ulnar nerve are seen in zone I, deep to the volar carpal ligament. Division into the deep motor branch constitutes zone ll, and the superficial sensory branch constitutes zone lll. Compression of the ulnar nerve in zones I and III produces sensory findings, whereas compression in zones I and II produces motor findings.
|
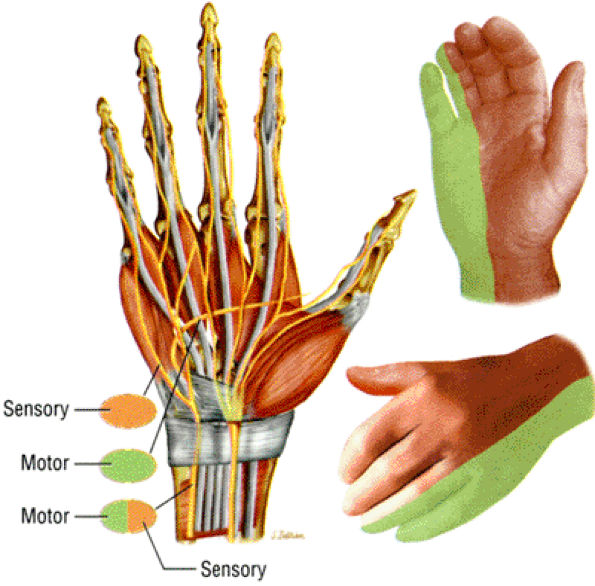 |
|
FIGURE 10.206 ● Potential sites of ulnar nerve injury. Orange represents sensory fibers, green represents motor fibers, and mixed orange-green represents both. Corresponding ulnar-side palmar and dorsal cutaneous innervation is shown. Coronal and oblique color illustrations.
|
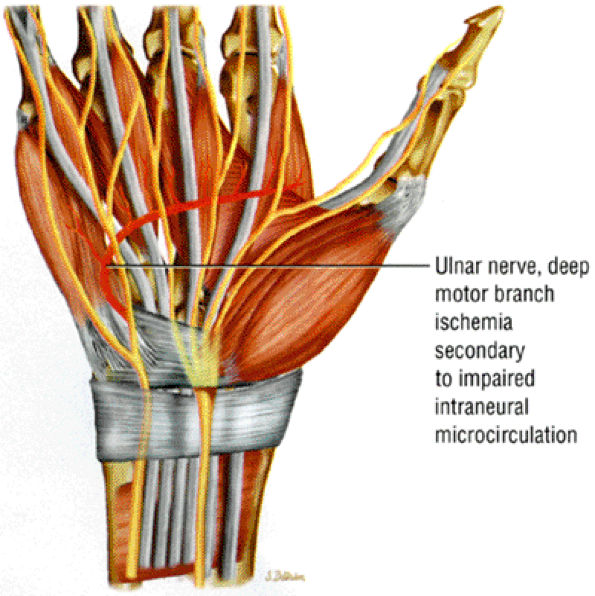 |
|
FIGURE 10.207 ● Ulnar tunnel syndrome with ischemia of the deep motor branch of the ulnar nerve. Coronal color illustration.
|
-
Diffuse swelling
-
Enlargement of the ulnar nerve
-
Hyperintense signal within the ulnar nerve, best demonstrated on axial FS PD FSE or STIR images (see Fig. 10.208)
-
A round to ovoid mass (usually with hyperintense signal on FS PD FSE images)
-
A ganglion cyst
-
An aneurysm
-
Associated fracture
-
Anomalous muscle
-
SLAC wrist, the most common pattern of degenerative arthritis of the wrist, develops in response to scaphoid rotation.
-
Initial changes of SLAC arthritis occur with degeneration of the proximal scaphoradial articulation, with subsequent development of capitolunate articular destruction.
-
Advanced SLAC represents complete destruction of the scaphoradial, capitotunate, and scaphocapitate joints. There is capitate impingement on the distal radius and narrowing of the hamate-lunate joint space. The radiolunate joint is not affected since it maintains smooth articular contact.
-
Triscaphe arthritis is the second most common form of degenerative arthritis of the carpus.
-
A combination of SLAC and triscaphe arthritis represents the third most common form of degenerative arthritis.
-
Less common degenerative disorders include ulnolunate and lunotriquetral arthritis.
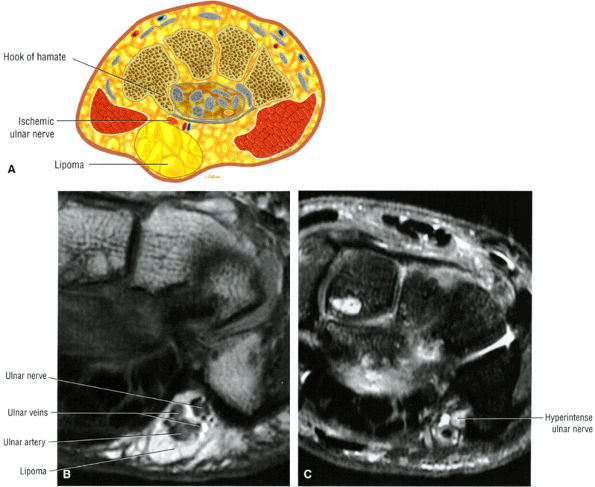 |
|
FIGURE 10.208 ● (A) Ulnar tunnel syndrome caused by extrinsic compression by a lipoma. Color axial section. (B) Axial T1-weighted image of lipoma within Guyon's canal encasing the ulnar nerve and vessels. (C) Hyperintense ulnar nerve on corresponding axial FS PD FSE image.
|
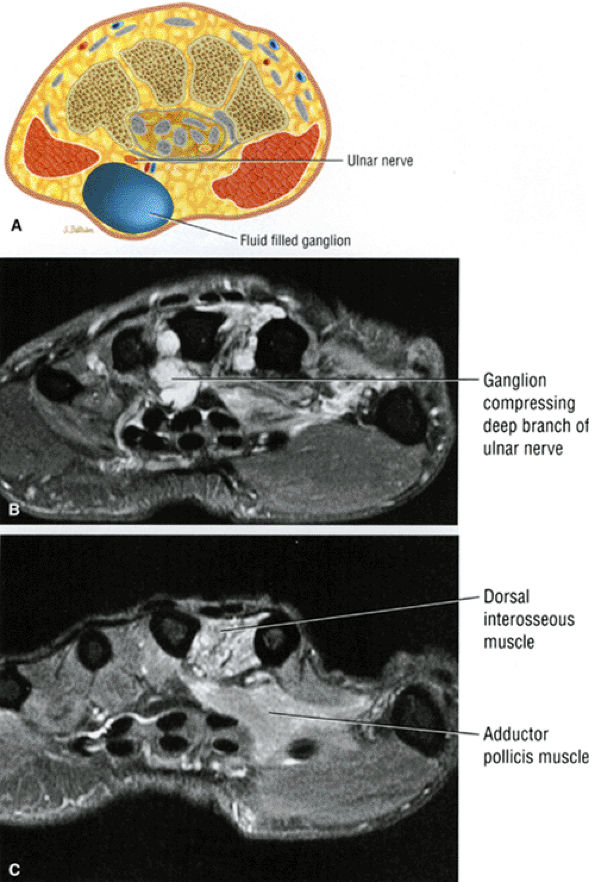 |
|
FIGURE 10.209 ● (A) Axial color illustration showing a ganglion compressing the ulnar nerve. (B, C) Axial FS PD FSE images showing dorsal interosseus and adductor pollicis denervation secondary to a motor deficit of the deep branch of the ulnar nerve.
|
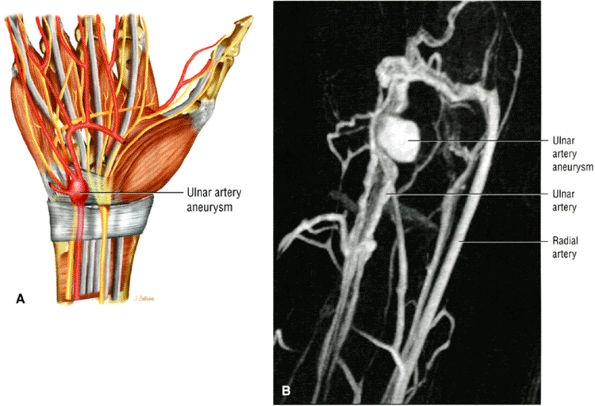 |
|
FIGURE 10.210 ● (A) Coronal color illustration (volar perspective) of ulnar artery aneurysm as an etiology of ulnar tunnel syndrome. (B) Maximum intensity projection MR image acquired post-contrast administration demonstrating a posttraumatic ulnar artery aneurysm. There is also an associated arteriovenous fistula resulting in local venous engorgement.
|
-
Stage 1 (Fig. 10.212): arthrosis limited to the radial styloid-scaphoid articulation
-
Stage II: arthrosis of the entire radioscaphoid articulation
-
Stage III (Fig. 10.213): capitolunate arthrosis
-
Sclerosis and narrowing with chondral loss between the radial styloid and scaphoid articulation
-
Sclerosis and narrowing involving the entire radioscaphoid articulation
-
Sclerosis and narrowing of the capitolunate joint
-
Loss of articular cartilage between the radial styloid and the dorsal pole of the scaphoid (in the setting of scaphoid nonunion)
-
Sclerosis or subchondral degenerative edema across the entire radioscaphoid articulation
-
Chondral loss in the capitolunate joint
-
Sparing of the radiolunate articulation, which can accommodate changes in scaphoid rotation and alignment
-
A fluid-filled gap between the scaphoid and lunate
-
Discontinuity of the scapholunate ligament
-
Degenerative cyst within the scaphoid, capitate, or distal radius.
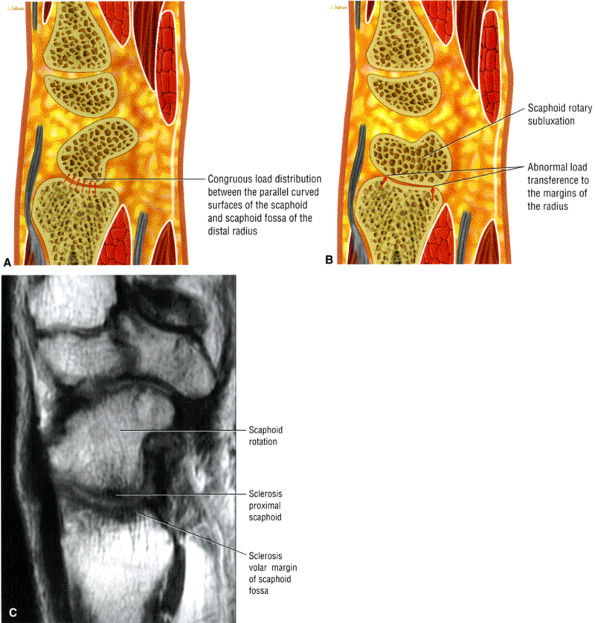 |
|
FIGURE 10.211 ● (A) Normal radioscaphoid congruous joint surfaces. (B) The congruous joint surface contact between the scaphoid and radius is lost with rotational instability secondary to rotary subluxation of the scaphoid. There is an abnormal load transferred to the volar and dorsal margins of the radius and the center of the scaphoid. The rotation of the scaphoid thus accelerates the process of radioscaphoid joint degeneration. (C) Corresponding T1-weighted sagittal image of scaphoid rotation with secondary pattern of sclerosis between the distal radius and scaphoid.
|
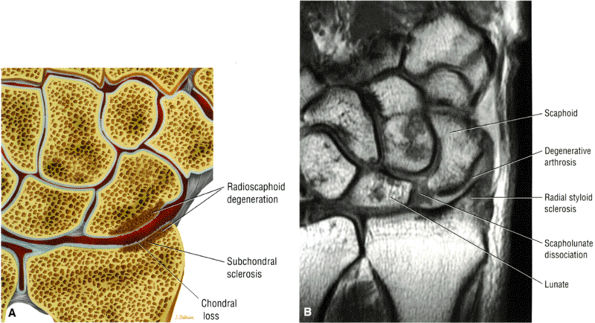 |
|
FIGURE 10.212 ● Stage I SLAC with arthrosis of the radial styloid-scaphoid articulation. (A) Coronal color graphic. (B) Coronal T1-weighted image.
|
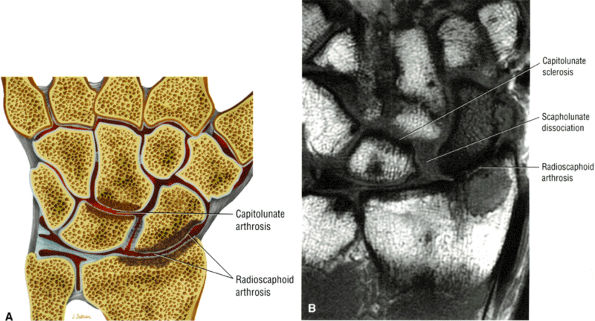 |
|
FIGURE 10.213 ● Stage III SLAC with arthrosis of the radioscaphoid articulation and capitolunate joint. (A) Color coronal graphic. (B) Coronal T1-weighted image.
|
 |
|
FIGURE 10.214 ● Calcium pyrophosphate arthropathy of the wrist with findings of scapholunate dissociation, SLAC wrist with proximal migration of the capitate, ulnar translocation of the lunate, synovitis, and marrow edema involving the capitate and lunate on T1-weighted (A) and FS PD FSE (B) coronal images. Corresponding AP radiograph (C) demonstrates chondrocalcinosis (arrows) in the TFC complex and scapholunate ligament.
|
-
Subchondral sclerosis (scaphotrapeziotrapezoid arthrosis)
-
Sclerosis with chondral loss
-
Degenerative marrow edema (a late finding)
-
Proximal migration of the trapezium and trapezoid
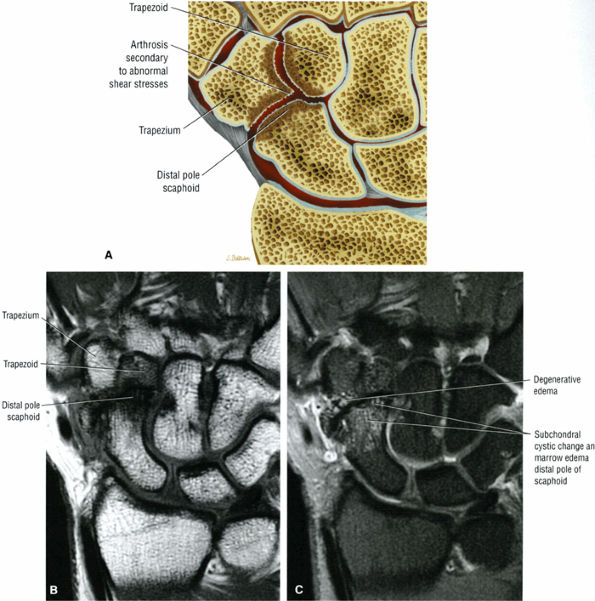 |
|
FIGURE 10.215 ● Triscaphe arthritis with arthrosis and destruction of the trapezioscaphoid and trapezoidoscaphoid joints. There is disruption in the ligamentous support of the scaphoid distally. (A) Coronal color graphic. (B) Coronal T1-weighted image. (C) Coronal FS PD FSE image.
|
-
The type ll lunate has an extra facet on its ulnar aspect, which is at risk for arthrosis at its articulation with the proximal pole of the hamate.
-
Coronal FS PD FSE images are used to identify early chondral erosions.
-
T1-weighted images are sensitive to hamato-lunate subchondral sclerosis.
-
Located between the scaphoid radially and the triquetrum medially (ulnarly)
-
The deep concave distal surface articulates with the head of the capitate.
-
The convex proximal surface represents the lunate facet of the distal radius and the triangular fibrocartilage.
-
The medial surface is a large flattened facet for articulation with the triquetrum.
-
There is an extra medial lunate facet seen in type II lunate, which articulates with the hamate.
-
Radially there is a flattened facet for articulation with the proximal (medial) end of the scaphoid.
-
The distal articular surface is narrower than the proximal surface (i.e., the lunate is wedge-shaped).
-
The lunate is narrower dorsally.
-
Articular cartilage covers most of the lunate.
-
The lunate articulates with the radius, the capitate, the hamate, the scaphoid, and the triquetrum.
![]() FIGURE 10.216 ● Type ll lunate (medial lunate facet) with sub-chondral erosion of the proximal pole of the hamate and accessory lunate facet. Coronal color illustration.Relevant information on the hamate includes:
FIGURE 10.216 ● Type ll lunate (medial lunate facet) with sub-chondral erosion of the proximal pole of the hamate and accessory lunate facet. Coronal color illustration.Relevant information on the hamate includes: -
It is the most medial bone in the distal row.
-
The proximal surface is narrow and convex for the lunate articulation.
-
The distal surface articulates with the forth and fifth metacarpals via two facets.
-
The dorsal surface is triangular.
-
The palmar surface is the hook.
-
The lateral surface is the concavity of the body and the hook.
-
The ulnar surface articulates with the triquetrum.
-
The spiral orientation of the triquetrohamate joint facilitates motion between the proximal and distal carpal rows.
-
An extra medial lunate facet
-
Subchondral sclerosis of the proximal hamate or medial lunate facet (in advanced disease)
-
Associated capitolunate arthrosis
-
Subchondral edema of the hamate (an uncommon finding)
-
Narrowing of the hamate-lunate joint space
-
Inhomogeneous signal intensity in the chondral surfaces of the medial lunate facet and the proximal hamate
-
Surface fibrillation, fraying, or full-thickness chondral defects (Fig. 10.217)
-
Four-corner arthritis (chondral degeneration in the proximal hamate, proximal capitate, radial distal triquetrum, and medial lunate facet)
-
Hamate or lunate marrow edema (unusual finding)
-
Small subchondral cystic changes in the proximal pole of the hamate
-
Subchondral bone loss in the proximal pole of the hamate and the medial lunate facet
-
Associated lunotriquetral ligament tear
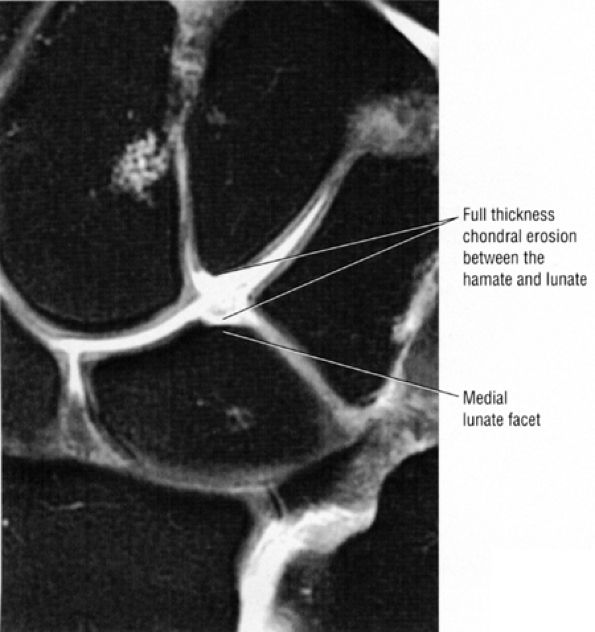 |
|
FIGURE 10.217 ● Medial lunate facet with chondromalacia between the medial facet and the proximal pole. The accessory facet may range in size from 10% to 50% of the length of the distal aspect of the lunate.
|
-
FS PD FSE or intravenous contrast is used to identify pannus tissue.
-
Chronic synovitis and inflammation are associated with capsulitis and ligamentous laxity and TFC complex tears.
-
Findings in the caput ulnar syndrome include dorsal subluxation.
-
Distal radioulnar joint
-
Ulnar and radial styloid
-
Carpus (the scaphoid, triquetrum, and pisiform)
-
Radiocarpal, midcarpal, and carpometacarpal articulations
-
Metacarpophalangeal and proximal interphalangeal joints
 |
|
FIGURE 10.218 ● Juxta-articular osteopenia with patchy marrow edema as shown on a coronal color graphic.
|
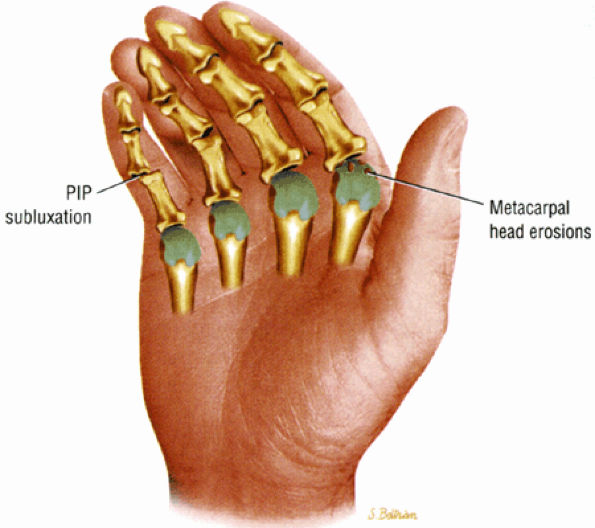 |
|
FIGURE 10.219 ● Ulnar deviation at the metacarpophalangeal joints is associated with radial deviation at the radiocarpal joint. Metacarpal head erosions are demonstrated. Soft-tissue swelling, marginal erosions (bare areas including the radial aspect of the second and third metacarpal heads), and joint deformities are common.
|
-
Morning stiffness lasting more than 1 hour
-
Arthritis of three or more joints
-
Arthritis of hand joints
-
Symmetric arthritis
-
Positive serum rheumatoid factor
-
Rheumatoid nodules
-
Radiographic changes
and MR studies document the subluxations and erosions affecting the phalanges, carpals, metacarpals, and ulnar styloid. Radiographic findings are usually negative in the early stages of disease, although early soft-tissue swelling may be visible. Erosion of the ulnar styloid tip is often the first radiographic evidence of disease; other findings include:
-
Erosions at the distal radius and ulna (common)
-
Triquetrum and pisiform erosions
-
Marginal erosion at the radial aspect of the trapezium (common)
-
Juxta-articular osteopenia
-
Pancarpal progressive chondral loss, seen as gradual joint space narrowing or joint obliteration
-
Bony ankylosis, most common in the midcarpal compartment in late stages
-
The zig-zag deformity (radial deviation at the radiocarpal joint and ulnar deviation at the metacarpophalangeal joints)
-
Dorsal subluxation of the ulna (common)
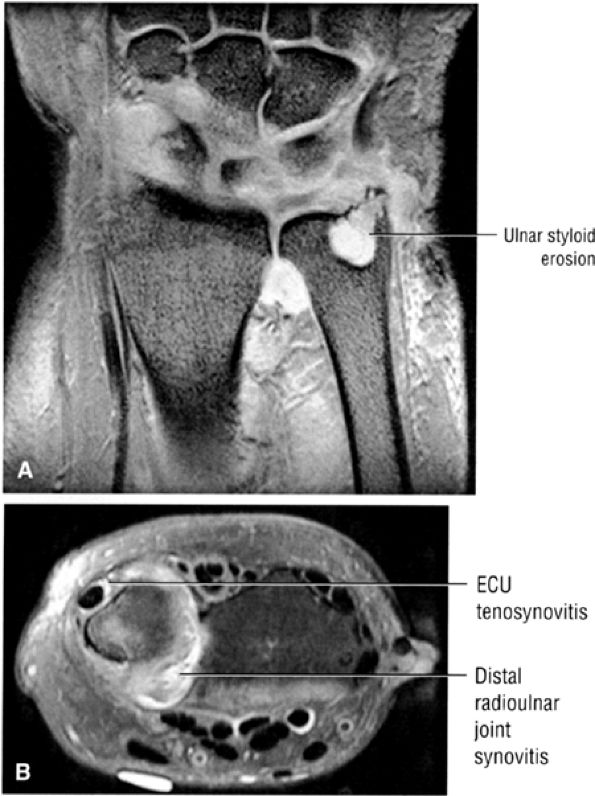 |
|
FIGURE 10.220 ● Erosion of the ulnar styloid secondary to synovial inflammation of the prestyloid recess. (A) Coronal T2* gradient-echo image. (B) Axial FS PD FSE image.
|
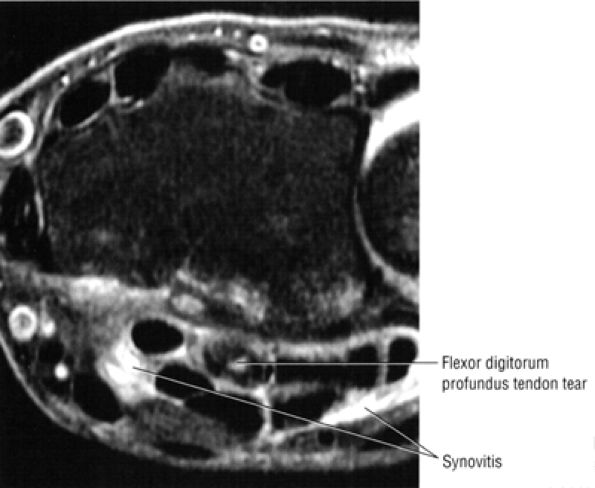 |
|
FIGURE 10.221 ● Flexor digitorum profundus tendon rupture and associated synovitis of the flexor tendons are shown on a axial FS PD FSE image.
|
-
Subchondral sclerosis, best appreciated on T1-weighted images
-
Early erosions with reactive marrow edema (Fig. 10.222)
-
Early joint effusions
-
Joint debris, visualized as signal inhomogeneity
-
Hypertrophied synovium, most frequently identified as intermediate signal intensity on FS PD FSE images
-
Tenosynovitis, hyperintense on FS PD FSE images
-
Partial tendon tears
-
Pannus (Fig. 10.223), which enhances vigorously after contrast administration
(seen as an area of low signal intensity without artifact) can be assessed on coronal images. The site of fusion of the interphalangeal articulation of the thumb may be degraded by residual metallic artifact, despite prior surgical removal of fixation pins. In diffuse soft-tissue swelling of a single digit secondary to psoriatic arthritis, MR imaging may be successful in excluding the diagnosis of osteomyelitis.
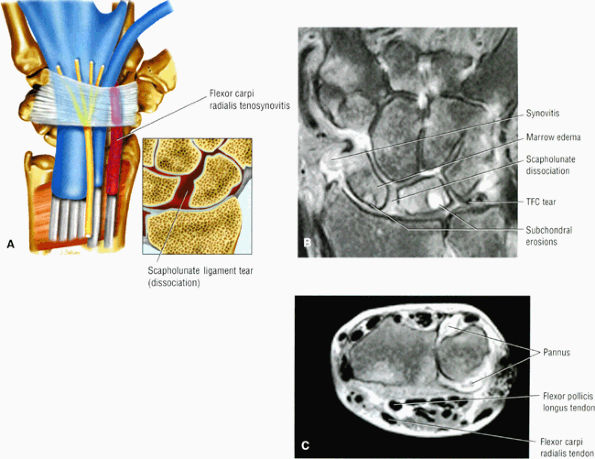 |
|
FIGURE 10.222 ● (A) Flexor tendon tenosynovitis in association with rheumatoid disease on a coronal color illustration with inset. (B) A coronal FS PD FSE image demonstrating intermediate-signal-intensity pannus, carpal edema and erosions, TFC disruption, and scapholunate dissociation. (C) Axial FS PD FSE image showing tenosynovitis of the flexor pollicis longus tendon and distal radioulnar joint synovial inflammation.
|
In patients with calcium pyrophosphate deposition disease (see Fig. 10.214) the areas of intra-articular calcification are not satisfactorily demonstrated on T1-weighted images when compared with high-quality magnification radiographs. FS PD FSE and T2*-weighted images viewed at high contrast settings are useful in identifying areas of calcified crystalline depositions. The MR changes in calcium pyrophosphate deposition disease arthropathy include marrow hyperemia. widening of
the scapholunate interval, proximal migration of the capitate, and joint space narrowing in the radiocarpal and metacar-pophalangeal joints. There is trapezioscaphoid involvement, with sparing of the distal radioulnar joint.154 Calcium pyrophosphate deposition may also occur in the TFC complex and interosseous ligaments. Crystal deposition in ligaments can lead to their rupture. Thus, degenerative changes and SLAC wrist deformity can be seen in calcium pyrophosphate deposition disease.
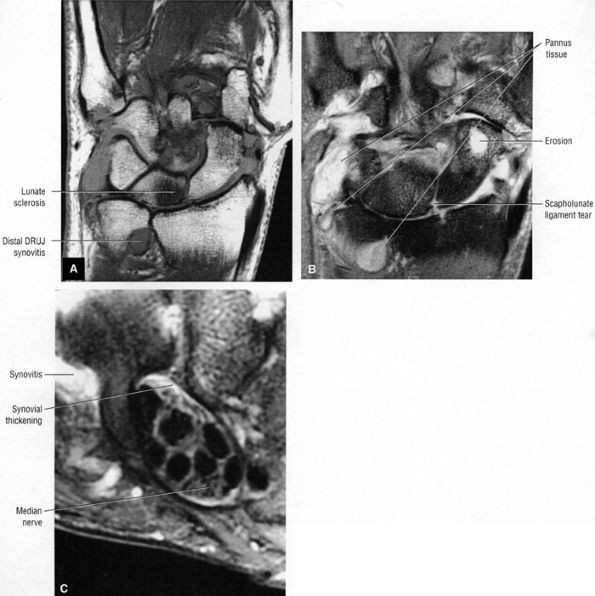 |
|
FIGURE 10.223 ● Intermediate-signal-intensity pannus adjacent to synovial fluid in a rheumatoid wrist on a coronal T1-weighted image (A) and a coronal FS PD FSE image (B). (C) Axial FS PD FSE image demonstrates synovial thickening within the carpal tunnel and adjacent to the hamate.
|
dense collagen. Subcutaneous nodules demonstrate an inhomogeneous intermediate signal intensity on T1-weighted and FS PD FSE images. Less common hypocellular nodules demonstrate low signal intensity on both T1-weighted and FS PD FSE images. Dupuytren's contracture is also described in Chapter 11.
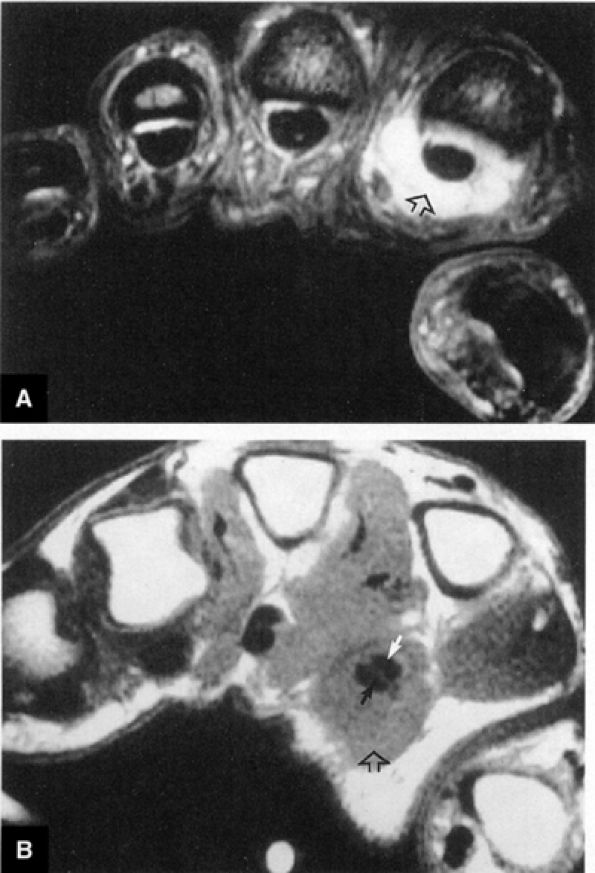 |
|
FIGURE 10.224 ● Psoriatic arthritis is classified into five subgroups based on the presence of acro-osteolysis of the distal interphalangeal joints, arthritis mutilans, symmetric polyarthritis, oligoarticular arthritis, and spondyloarthropathy. The subgroup with oligoarticular disease includes presentations of sausage-like tenosynovitis of the digits, as shown in this case. (A) Axial T1-weighted image. (B) T2*-weighted image.
|
-
The distal radial epiphysis is triangular and medially tilted.
-
Subtypes include Madelung's, reverse Madelung's, and chevron carpus.
-
Loss of motion
-
Weakness
-
Ligamentous stretching and carpal translation
-
Derangement of the distal radioulnar joint
-
Extensor tendon attrition over the deformed ulnar head in adults
-
Marked obliquity of the carpal tunnel associated with a susceptibility to median neuropathy in trauma
-
Midcarpal joint involvement secondary to the triangular morphology of the carpus
-
Loss of supination and restriction of dorsiflexion and radial deviation
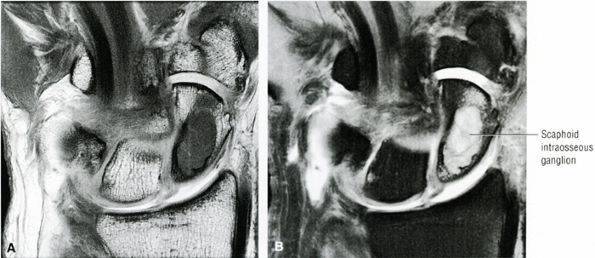 |
|
FIGURE 10.225 ● Large intraosseous ganglion of the scaphoid. There is a high association of intraosseous ganglions and soft-tissue ganglion cysts. Intraosseous ganglions are most common in the lunate. (A) Coronal T1-weighted image. (B) Coronal FS PD FSE image.
|
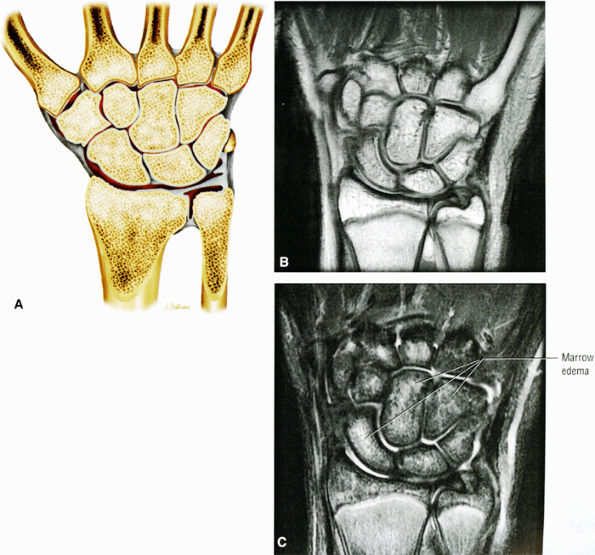 |
|
FIGURE 10.226 ● Patchy carpal marrow edema in response to injury with early clinical findings of complex regional pain syndrome on coronal color graphic (A), coronal T1-weighted (B), and corresponding FS PD FSE (C) images. Complex regional pain syndrome (CRPS; formerly known as reflex sympathetic dystrophy) may result from trauma or from neurologic or vascular insults. MR detects patchy osteoporosis as regions of nonspecific marrow edema. Diffuse osteopenia may have similar MR findings. CRPS type 1 occurs in response to an initiating noxious event, and there is no known nerve injury. CRPS type 2 or causalgia is related to a nerve injury but not necessarily limited to the distribution of the injured nerve.
|
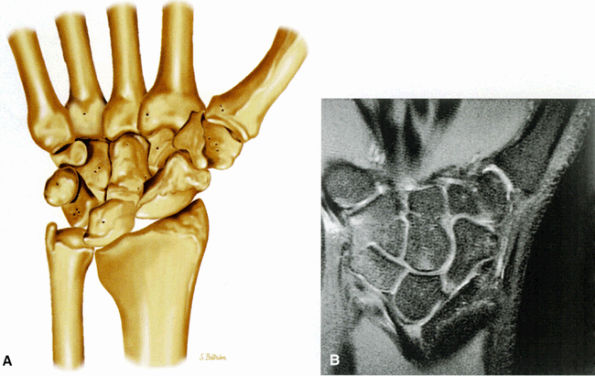 |
|
FIGURE 10.227 ● (A) Madelung's deformity with medial angulation of the distal radial articular surface and triangulation of the carpus. Coronal color illustration. FS PD FSE (B) images of Madelung's deformity with proximal migration of the lunate (triangulation of the carpus), medial angulation of the distal radius, and oblique orientation of the TFC.
|
-
Ulnar angulation of the distal radial articular surface
-
A dorsoulnar configuration of the ulnar head (dorsally prominent ulnar head)
-
Bowing of the radius
-
A physeal lesion at the palmar ulnar aspect of the distal radial physis
-
A thickened radiolunate ligament attached to the distal radial physis
-
Development of a groove and osseous spike at the ulnar aspect of the metaphyseal-diaphyseal junction from the tethering effect of the radiolunate ligament
-
Oblique radial TFC attachment
-
Lunate ischemia is sometimes seen.
-
Chevron carpus (mid-ulnar zone dyschondrosteosis)
-
Advanced dyschondrosteosis with lack of proximal lunate support by the radius
-
The typical origin of a ganglion is dorsal to the scapholunate joint.
-
Intravenous contrast is required for diagnosis when there is inhomogeneity of the ganglion signal intensity on FS PD FSE or STIR images.
-
Dorsal extension of the ganglion occurs in proximity to the dorsal interosseous nerve subjacent to the capsule.
-
Dorsal scapholunate interval (Fig. 10.228)
-
Volar (palmar) radiocarpal joint
-
Dorsal retinaculum of the first extensor component
-
Carpal tunnel
-
Guyon's canal
-
Triscaphe joint
-
Ulnocarpal joint
-
Second metacarpal-trapezial joint
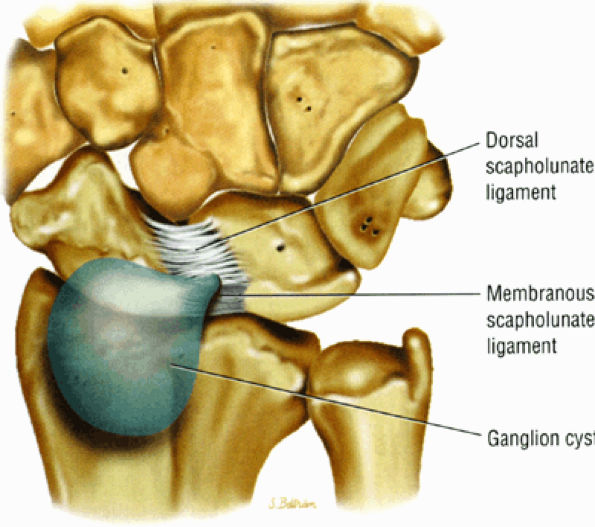 |
|
FIGURE 10.228 ● Common location of a ganglion cyst relative to the dorsal scapholunate interval. Coronal color illustration.
|
-
Soft-tissue cystic mass (Fig. 10.230), which may be unilocular or multiloculated (Fig. 10.231)
-
Subcutaneous tissue adjacent to the mass is normal.
-
Arthrosis of the scaphotrapezial or radioscaphoid articulations
-
Scapholunate diastasis on coronal images
-
Narrow stalk in communication with the main cyst, which may be difficult to visualize on T1-weighted images but is conspicuous and hyperintense on FS PD FSE or STIR images
-
Stalk extension through the joint capsule with an elongated pedicle allows cyst presentation away from its point of origin (e.g., cysts originating from the scapholunate interval may be ulnar to the extensor tendons).
-
Hypointense capsule may be seen on FS PD FSE images.
-
Inhomogeneity of cyst related to mucin content as appreciated on FS PD FSE images
-
Small carpal tunnel ganglions are frequently traced to the scaphotrapeziotrapezoid joint.
-
Secondary compression of the median nerve
-
Cyst communication with its adjacent tendon sheath
-
Intraosseous carpal ganglions
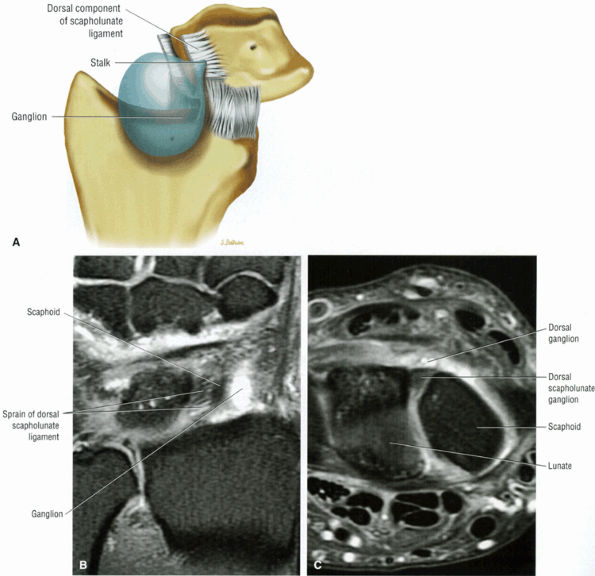 |
|
FIGURE 10.229 ● (A) A dorsal ganglion may be associated with a sprain or tear of the dorsal and/or membranous fibers of the scapholunate ligament complex. Coronal color graphic. (B, C) A scapholunate ligament dorsal component sprain associated with radial extension of an associated dorsal ganglion. (B) Coronal FS PD FSE image. (C) Axial FS PD FSE image.
|
ganglions. Surgical treatment consists of excision of the ganglion, including the stalk.
 |
|
FIGURE 10.230 ● Direct extension of dorsal ganglions through the dorsal fibers of the scapholunate ligament. Synovial fluid is pumped between collagen bundles in weak areas in the dorsal capsule. (A) Coronal T1-weighted image. (B) Coronal FS PD FSE image.
|
-
True osseous invasion is not typical and is suggestive of a more aggressive process.
-
Reactive soft-tissue edema is atypical.
-
T2* gradient-echo images are useful to document hemosiderin content.
-
Enhancement with contrast is typical.
-
Fibrous septations and lobulations
-
Convex bowing or bulge toward the skin from the tendon sheath
-
Flexor or extensor tendon-related location
-
Extension in the transverse and longitudinal planes
-
Origin may be deep to the tendon (between the tendon bone).
-
Foci of hemosiderin (hypointense on T1-, PD-, or FS PD FSE images) may be peripheral (sometimes clumped) or found throughout the lesion.
-
A sharply defined interface without reactive edema of the adjacent subcutaneous tissue
-
Adjacent osseous erosion (unusual but can occur)
-
Greater long-axis growth is characteristic.
-
Minimal associated fluid is observed adjacent to the lesion.
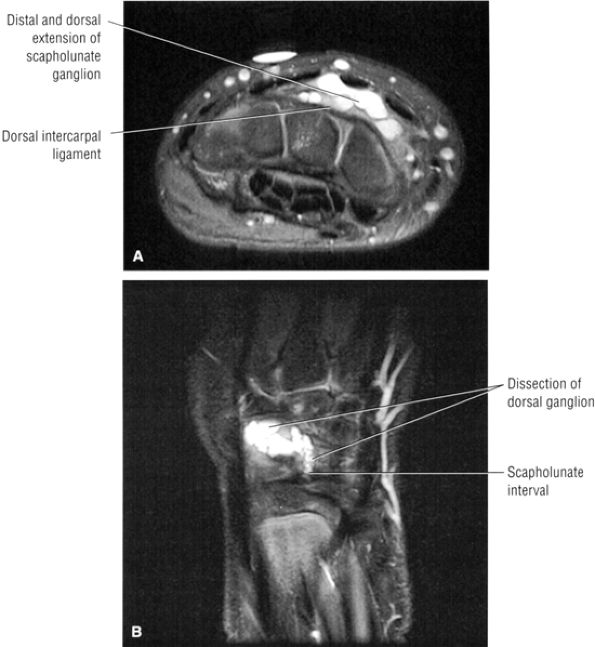 |
|
FIGURE 10.231 ● Distal and dorsal extension of a multiloculated and multilobular scapholunate ligament ganglion, which has protruded through the dorsal wrist capsule. The ganglion connects to the joint capsule through a narrow stalk. These ganglions have a nonsynovial capsular lining of compressed collagen fibers and flat nonendothelial cells. (A) Axial FS PD FSE image. (B) Coronal FS PD FSE image.
|
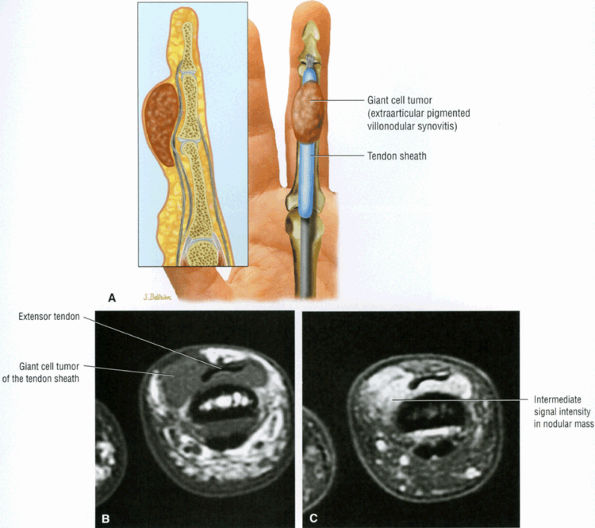 |
|
FIGURE 10.232 ● (A) Coronal graphic and sagittal inset of a giant cell tumor of the flexor tendon sheath. Characteristic lobulations and well-circumscribed fibrous morphology are shown. (B, C) Localized form of giant cell tumor, or extra-articular pigmented villonodular synovitis, involving the radial dorsal aspect of the third digit (long finger) proximal to the distal interphalangeal joint. The majority (up to two thirds) of giant cell tumors are located in the volar aspects of the fingers and usually involve the index and long fingers. (B) Axial T1-weighted image. (C) Axial FS PD FSE image.
|
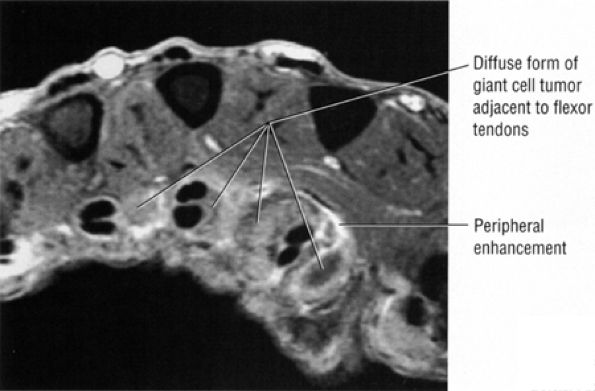 |
|
FIGURE 10.233 ● Rare diffuse form of extra-articular giant cell tumor of the tendon sheath similar to pigmented villonodular synovitis. Axial FS T1-weighted contrast-enhanced MR image.
|
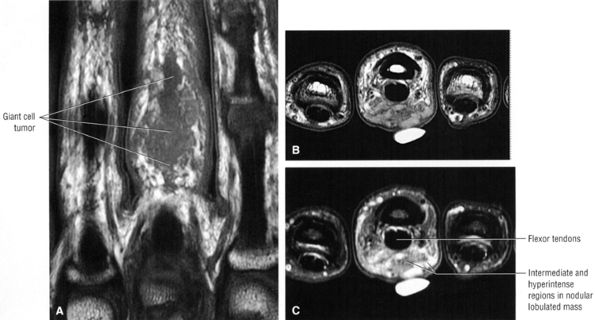 |
|
FIGURE 10.234 ● Volar presentation of characteristic MR findings of giant cell tumor of the tendon sheath with intermediate and hyperintense regions within the lesion. Corresponding histology demonstrates histiocytes and multinucleated giant cells. Hemosiderin-containing xanthoma cells occur in the periphery of the lesion and are best appreciated using T2* gradient-echo techniques. (A) Coronal T1-weighted image. (B) Axial T1-weighted image. (C) FS PD FSE image.
|
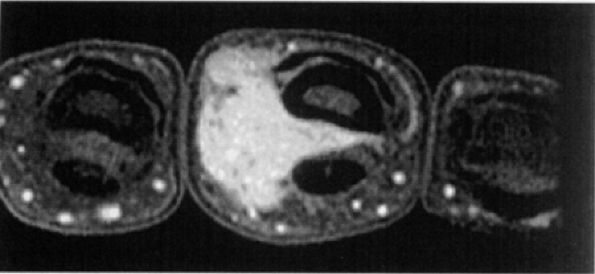 |
|
FIGURE 10.235 ● Typical intense contrast enhancement of a giant cell tumor shown between the flexor tendons and phalanx. Axial FS T1-weighted image.
|
-
Tendinosis and tenosynovitis of the abductor pollicis longus and extensor pollicis brevis are assessed at the level of the radial styloid on axial MR images.
-
The striated appearance of the abductor pollicis longus is related to enlargement of tendinous slips. Longitudinal splitting is more common in the abductor pollicis longus.
-
A longitudinal septum may divide the abductor pollicis longus and extensor pollicis brevis, creating a subcompartment for the extensor pollicis brevis.
styloid and point tenderness over first dorsal compartment. Triggering or crepitus may also occur.
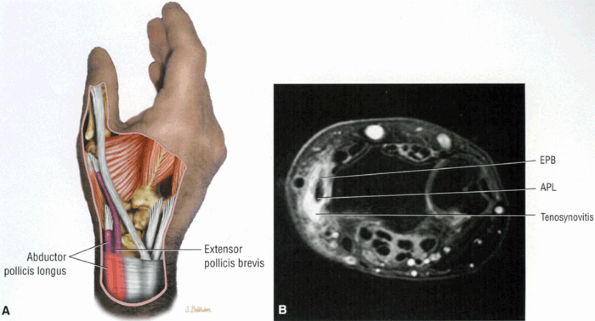 |
|
FIGURE 10.236 ● De Quervain's tenosynovitis involving the abductor pollicis longus and extensor pollicis brevis at the level of the radial styloid. (A) Oblique color graphic. (B) Axial FS PD FSE image.
|
-
Fluid signal intensity in the distended tendon sheath and surrounding extensor pollicis brevis and abductor pollicis brevis
-
Debris within the sheath
-
Effacement of subcutaneous fat radial to the extensor pollicis brevis and abductor pollicis brevis
-
Hyperintense adjacent subcutaneous fat on FS PD FSE images
-
Intermediate signal in chronic changes on FS PD FSE images
-
Central or eccentric intermediate signal in the grossly enlarged extensor pollicis brevis and abductor pollicis brevis tendons on T1- and PD-weighted images (Fig. 10.237)
-
Tendon degeneration (displays intermediate signal intensity on FS PD FSE images unless associated with a hyperintense longitudinal split)
-
Enlargement of the first extensor compartment tendons from medial to lateral on coronal images and in cross-sectional diameter on axial images
-
Maximum tendon enlargement is at and immediately distal to the radial styloid.
-
Longitudinal splitting of the tendon is more common in the abductor pollicis brevis tendon.
-
A septum between the tendons (forming a subcompartment for the extensor pollicis brevis)
-
Striation of abductor pollicis brevis related to enlargement of multiple slips
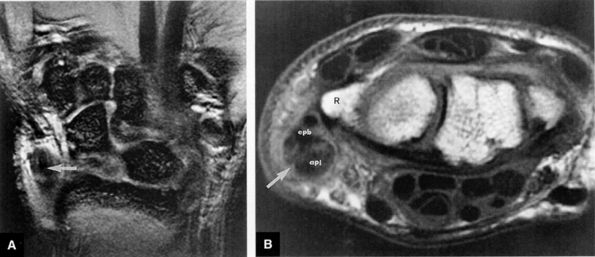 |
|
FIGURE 10.237 ● De Quervain's stenosing tenosynovitis (arrow) with inflammation of the abductor pollicis longus (apl) and extensor pollicis brevis (epb) tendons of the first extensor compartment. Inflammation is associated with these enlarged tendons in the fibro-osseous tunnel at the level of the radial styloid (R). Increased signal intensity in the tendon sheath (tenosynovitis) and tendon (tendinitis) coexist in this case. (A) T2*-weighted coronal image.(B) T1-weighted axial image.
|
-
The subsheath of the extensor carpi ulnaris forms the fibro-osseous tunnel, attaches to the ulnar styloid and ulnar head, and merges with the capsule of the distal radioulnar joint and the TFC complex.
-
The position of supination and ulnar deviation reproduces extensor carpi ulnaris instability. Extensor carpi ulnaris relocation occurs with pronation and radial deviation.
-
Longitudinal splitting of the extensor carpi ulnaris tendon is characterized by hyperintense signal intensity and is associated with tenosynovitis.
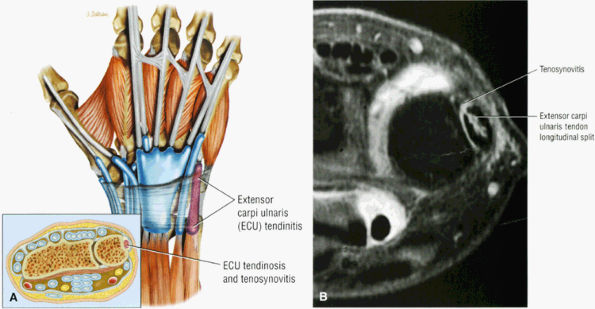 |
|
FIGURE 10.238 ● (A) Extensor carpi ulnaris tendinitis represents an inflammation of the synovial lining of the extensor carpi ulnaris and is frequently associated with intrinsic tendon degeneration. Color coronal illustration and axial inset. (B) Longitudinal split of extensor carpi ulnaris tendon occurs as the extensor carpi ulnaris tendon becomes stiff and has a decreased resistance to shear forces. Axial FS PD FSE image.
|
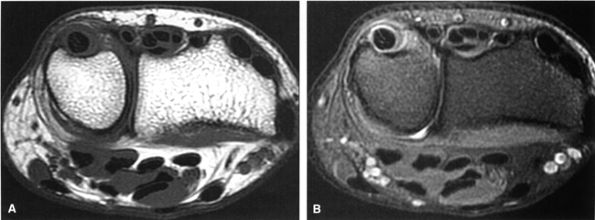 |
|
FIGURE 10.239 ● Extensor carpi ulnaris tenosynovitis and tendinosis. Tendon degeneration is associated with a decrease in collagen content. (A) Axial T1-weighted image. (B) Axial FS PD FSE image.
|
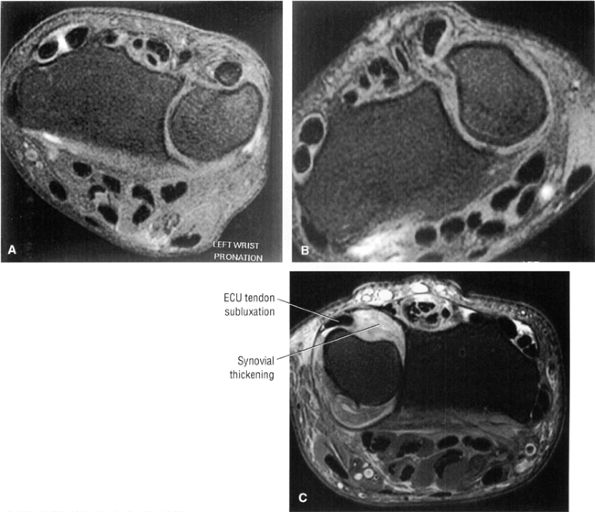 |
|
FIGURE 10.240 ● (A) Normal position of the extensor carpi ulnaris tendon in partial supination. (B) Dislocation of the extensor carpi ulnaris in the position of maximal supination. Supination and ulnar deviation reproduce extensor carpi ulnaris instability, and extensor carpi ulnaris relocation occurs with pronation and radial deviation. (C) Extensor carpi ulnaris subluxation secondary to chronic synovial inflammation displacing the extensor carpi ulnaris in an ulnar direction in the neutral position of the ulna (partial supination). Rupture of the extensor carpi ulnaris subsheath results in a painful subluxation syndrome. (A, B) Axial FS PD FSE images. (C) Axial FS PD FSE image.
|
-
Fluid within the extensor carpi ulnaris tendon sheath (see Figs. 10.238, 10.239, and 10.241)
-
Thickening of the tendon sheath
-
Increased cross-sectional diameter of the extensor carpi ulnaris tendon
-
Fraying of the tendon margins
-
Tendon degeneration
-
Extensor carpi ulnaris subluxation or dislocation
-
Intermediate-signal-intensity fluid on FS PD FSE images in chronic tenosynovitis
-
Intermediate signal on FS PD FSE images in tendinosis/degeneration
-
Longitudinal splitting
-
Replacement of tendon by fluid signal in complete extensor carpi ulnaris rupture
-
Foci of calcification
-
Inflamed synovium, which enhances after administration of intravenous contrast
tendinitis includes diagnostic and therapeutic injection of lidocaine and cortisone, splinting, nonsteroidal anti-inflammatory agents, and the RICE protocol (rest, ice, compression, and elevation). Conservative treatment for acute extensor carpi ulnaris rupture is application of a long-arm cast in full supination and neutral wrist flexion/extension. Surgery is necessary for chronic or nonresponsive conditions. Extensor carpi ulnaris tendinitis with progressive fibrosis of the sixth compartment requires surgical release, and traumatic rupture of the extensor carpi ulnaris is treated with reconstruction of the retinaculum.
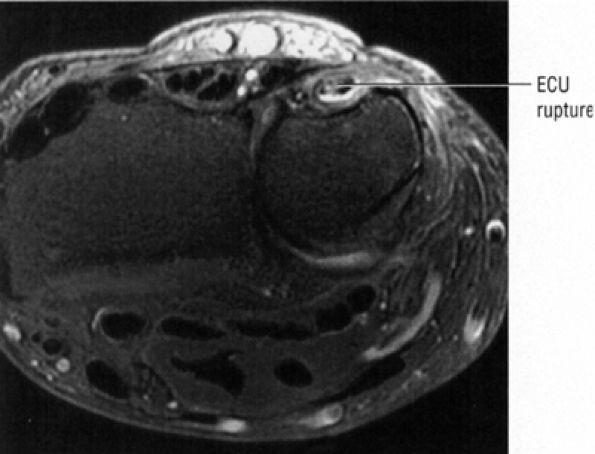 |
|
FIGURE 10.241 ● Extensor carpi ulnaris rupture as an endstage in the process of tenosynovitis, tendinosis, and longitudinal splitting. Axial FS PD FSE image.
|
-
Evaluation of ulnar collateral ligament tears and Stener's lesions requires coronal images through the first metacarpophalangeal joint acquired parallel to the plane of the collateral ligaments.
-
The retracted ulnar collateral ligament is seen with folded or horizontally directed fibers in Stener's lesions.
-
Stener's lesion must demonstrate entrapment of the ulnar collateral ligament by adductor pollicis aponeurosis.
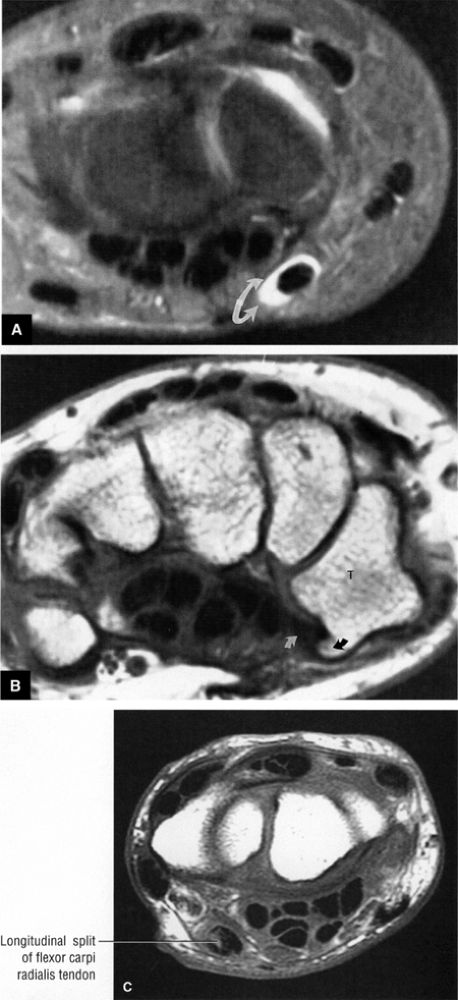 |
|
FIGURE 10.242 ● (A) Flexor carpi radialis tenosynovitis (arrows) is hyperintense on an FS PD FSE axial image at the level of the proximal carpal row. (B) The vulnerable area of fibro-osseous tunnel narrowing (white arrow) occurs beneath the prominent trapezial crest (black arrow). Since the tendon sheath forming the rigid fibro-osseous canal narrows and ends at the level of the trapezium (T), MR findings of tendinitis or tenosynovitis are seen proximal to this location. Axial T1-weighted image. (C) Flexor carpi radialis partial tear with tendon cross-sectional enlargement visualized proximal to the trapezium. Axial T1-weighted image.
|
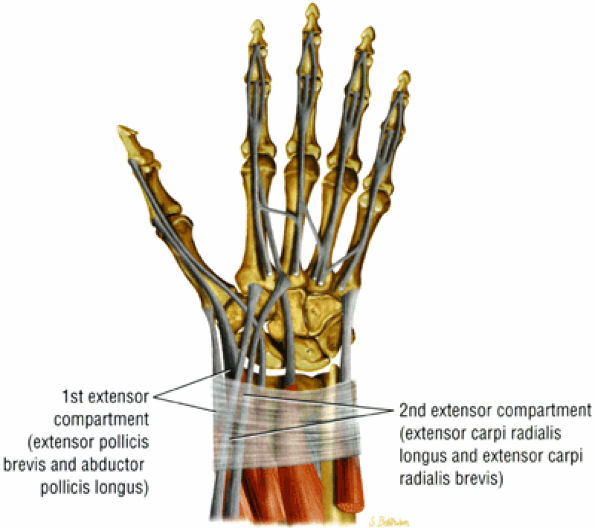 |
|
FIGURE 10.243 ● Area where tenosynovitis of the second dorsal compartment occurs in intersection syndrome. Pain and swelling usually occur proximal to the wrist as inflammation occurs where the muscle belly of the abductor pollicis longus and extensor pollicis brevis cross the common wrist extensors of the second dorsal compartment. Coronal color graphic.
|
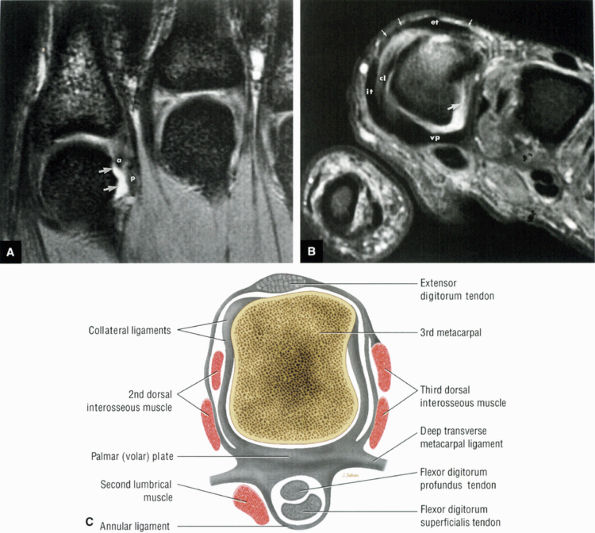 |
|
FIGURE 10.244 ● (A) Index metacarpophalangeal joint with direct extension of hyperintense joint fluid across a torn proximal attachment of the ulnar collateral ligament (arrows). There is disruption of both the proper (p) and accessory (a) components of the collateral ligament. T2*-weighted coronal image. (B) Correspond-ing T2*-weighted axial image shows the normal insertion of the collateral ligament (cl) into the lateral aspect of the volar plate (vp). The torn and retracted accessory component of the ulnar collateral ligament (large arrow) is not seen in continuity with the periphery of the volar plate. The volar plate represents a normal capsular thickening forming the floor of the metacarpophalangeal joint. Also shown are the common extensor tendon (et) and sagittal bands (small arrows). The sagittal bands of the extensor hood extend from the common extensor tendon to the volar plate and course in the plane between the interosseous tendon (it) and collateral ligament (ct). (C) Normal anatomy of the third metacarpal at the level of the metacarpophalangeal joint. Axial color graphic.
|
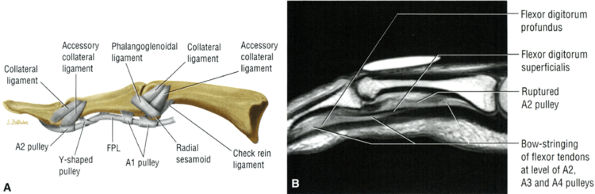 |
|
FIGURE 10.245 ● (A) Thumb capsular ligaments of the metacarpophalangeal and interphalangeal joints. Lateral color graphic. (B) Sagittal FS PD FSE image with a torn checkrein ligament. The accessory collateral ligament was also injured in this patient, who sustained a thumb dislocation.
|
-
Swelling
-
Reduced pinch strength
-
A mass caused by the displaced ulnar collateral ligament stump on the ulnar side of the metacarpophalangeal joint or proximal to the metacarpophalangeal joint
-
Abnormal thumb rotation (rotation of the proximal phalanx on the intact axis of the radial collateral ligament)
-
Absent endpoint on joint stress test in complete tears
-
Instability in metacarpophalangeal flexion in proper collateral ligament tears with intact accessory collateral ligament and volar plate
-
Instability in flexion and extension in complete ulnar complex disruption
-
Stability less than or equal to 10° of joint space opening
-
Instability greater than or equal to a 30° abduction arc on stress relative to the contralateral side
 |
|
FIGURE 10.246 ● Gamekeeper's thumb with rupture of the distal attachment (curved arrow) of the ulnar collateral ligament (u). The torn ulnar collateral ligament remains deep to the overlying adductor aponeurosis (small arrows). In Stener's lesion (not present in this case), the torn ulnar collateral ligament relocates superficial to the adductor pollicis aponeurosis after the abduction injury occurs. (A) T1-weighted coronal image. (B) STIR coronal image.
|
-
Grade I: Stretching of the ligament
-
Grade II: Incomplete but discrete tears
-
Grade III: Complete ruptures with or without Stener's lesion
-
Ulnar collateral ligament remains deep to the overlying adductor aponeurosis.
-
Ulnar collateral ligament thickening
-
Discontinuity at the ulnar collateral ligament attachment to the proximal aspect of the proximal phalanx (thumb)
-
Edema and fluid superficial and deep to the ulnar collateral ligament
-
Subchondral edema with or without osseous avulsion at the ulnar collateral ligament distal attachment to the proximal phalanx
-
Soft-tissue edema superficial to the adductor aponeurosis
-
Ulnar displacement of the ulnar collateral ligament and adductor aponeurosis
-
Ulnar collateral ligament orientation along the long axis of the first ray (thumb)
-
Thickened ulnar collateral ligament with central signal inhomogeneity (focal areas of edema)
-
Fluid interposed between the base of the proximal phalanx and the retracted ligament
-
Fluid plane between the distal ulnar aspect of the first metacarpal and the ulnar collateral ligament and between the ulnar collateral ligament and the adductor aponeurosis
-
Retracted mass of ulnar collateral ligament
-
Ulnar collateral ligament trapped either completely superficial to or intersecting the overlying adductor aponeurosis
-
Gross displacement of the ulnar collateral ligament medial to the adductor aponeurosis
-
Ulnar collateral ligament directional vector with increased horizontal orientation (no longer parallel to long axis of first digit) (see Fig. 10.247)
-
Displacement of the retracted ulnar collateral ligament varies from 90° to as much as 180° of pronation (Fig. 10.248).
-
“Yo-yo on a string” appearance of Stener's lesion caused by a retracted and balled-up ulnar collateral ligament (the yo-yo) with the more proximal linear adductor aponeurosis (the string)
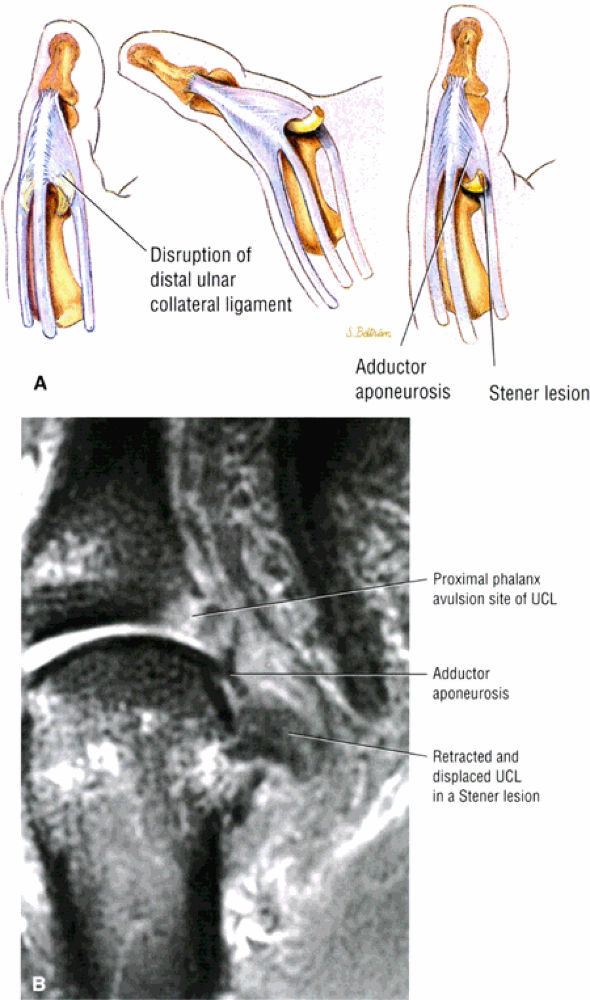 |
|
FIGURE 10.247 ● (A) Progression of a displaced ulnar collateral ligament (UCL) forming Stener's lesion with the proximal margin of the abductor aponeurosis intersecting and entrapping the folded UCL. (B) Stener's lesion with the thickened mass-like morphology of the retracted UCL oriented in a horizontal direction. The UCL is perpendicular to the long axis of the thumb and to the course of the adductor aponeurosis.
|
 |
|
FIGURE 10.248 ● Stener's lesion with complete 180° rotation of the torn ulnar collateral ligament (UCL). The flipped UCL is visualized proximal to the metacarpophalangeal joint on the axial image. (A) Coronal FS PD FSE image. (B) Axial FS PD FSE image.
|
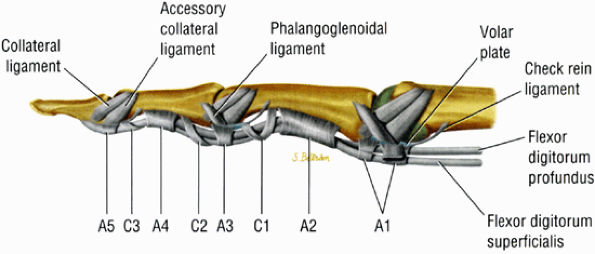 |
|
FIGURE 10.249 ● Normal anatomy of the ligaments reinforcing the digital tendon sheath. A1 through A5 represent the annular ligaments and C1 through C3 represent the cruciform ligaments. The longest annular ligament, the A2 pulley, is located on the proximal diaphysis of the proximal phalanx. Sagittal color graphic.
|
-
There are five digital annular pulleys, which are condensations of transversely oriented fibrous bands.
-
The digital annular pulleys stabilize the flexor tendons during flexion and resist ulnar/radial displacement as well as palmar bowing.
-
The A2 pulley (located at the proximal aspect of the proximal phalanx) and the A4 pulley (located at the midaspect of the middle phalanx) are the key stabilizing digital annular pulleys.
-
Bowstringing from the proximal interphalangeal joint to the base of the proximal phalanx on sagittal images in complete rupture of the A2 pulley
-
Bowstringing from the proximal interphalangeal but not reaching the base of the proximal phalanx in incomplete rupture of A2 pulley
-
Bowstringing at the level of the proximal phalanx to a region distal to the proximal interphalangeal joint in rupture of both the A2 and A3 pulleys
-
Bowstringing at the level of the middle phalanx in A4 rupture
-
Fluid signal associated with the affected pulley
-
Tendon sheath cysts
-
Fibrous tissue
-
Tendon displacement
-
Anterior displacement relative to the proximal aspect of the proximal phalanx in the A2 pulley area
-
Anterior displacement relative to the middle phalanx in the A4 pulley area
-
Medial or lateral subluxation
-
-
Fibrous scar tissue
-
Proximal or distal interphalangeal joint fluid
-
Tenosynovitis
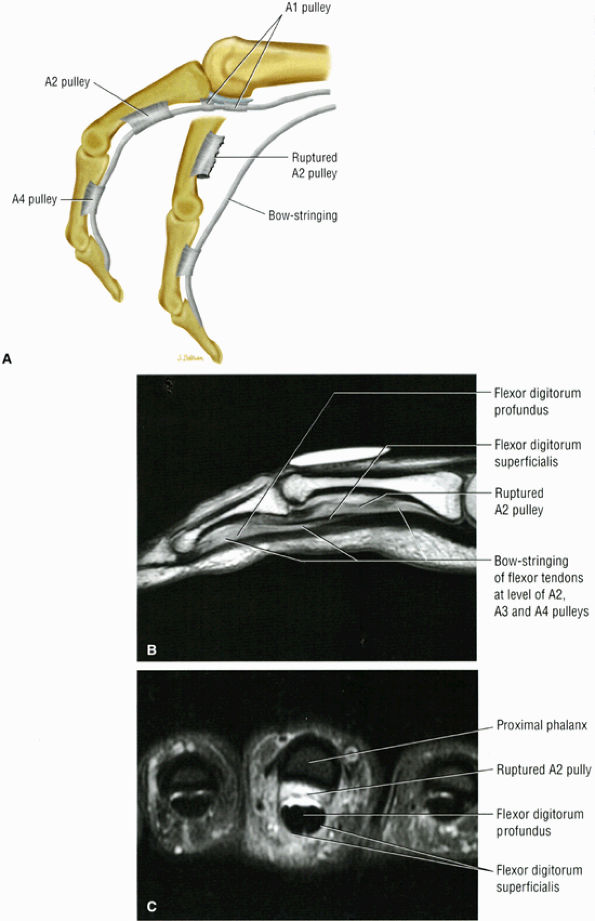 |
|
FIGURE 10.250 ● (A) Bowstringing of flexor tendons secondary to rupture of the A1 and A2 pulleys. Bowstringing of the flexor tendons is associated with rock-climbing pulley injuries. Ruptures may occur at the A3, A2, A4, or A1 pulleys. Sagittal color graphic. (B) T1-weighted sagittal image with bowstringing of the flexor tendons at the level of the A2, A3, and A4 pulleys in a rock climber. Ruptures occur frequently in the A3, A2, and A4 pulleys. The pulleys of the middle or long finger are stronger than the pulleys in the index, ring, and little fingers. FDS, flexor digitorum superficialis; FDP, flexor digitorum profundus. (C) Rupture of the A2 pulley of the third finger. There is volar displacement of the flexor tendons, with the torn A2 pulley identified between the proximal phalanx and the flexor tendons.
|
-
There are three types of flexor digitorum profundus avulsion injuries: tendon retraction into the palm, retraction to the proximal interphalangeal joint, and an osseous avulsion lodged at the distal edge of the A4 pulley.
-
Evaluation of the tendon course on sagittal images should be correlated with axial images. T2* gradient-echo images may be used to improve tendon contrast discrimination.
-
A2 and A4 pulleys, critical for maximal finger flexion, which originate from bone
-
Five annular pulleys (A1 to A5), which are thick and well defined
-
Three cruciate pulleys (C1 to C3), which are thin and collapse in flexion
-
Palmar aponeurosis
-
Short and long vincula, a dorsal mesotenon that carries blood supply
-
Type I: Tendon retraction into the palm, blood supply disruption, and a tendon sheath scar
-
Type II: Tendon retracts to the proximal interphalangeal joint and the flexor digitorum profundus is caught at the chiasm of the flexor digitorum superficialis.
-
Type III: Flexor digitorum profundus avulsion plus a large osseous fragment. The bony fragment is lodged at the distal edge of the A4 pulley.
-
Zone 1: from the fingertip to the midportion of middle phalanx
-
Zone 2: from the midportion of the middle phalanx to the distal palmar crease
-
Zone 3: from the distal palmar crease to the distal edge of the carpal tunnel
-
Zone 4: in the carpal tunnel
-
Zone 5: proximal to the carpal tunnel
-
Type I: Flexor digitorum profundus retracts to the palm.
-
Type II: Vincula vessels are intact and there is a tether retracting the flexor digitorum profundus.
-
Type III: A large fragment of bone catches on the A4 or A5 pulley.
-
Type IV: Fractures at the flexor digitorum profundus insertion; retraction is permitted by separation of tendon from bone.
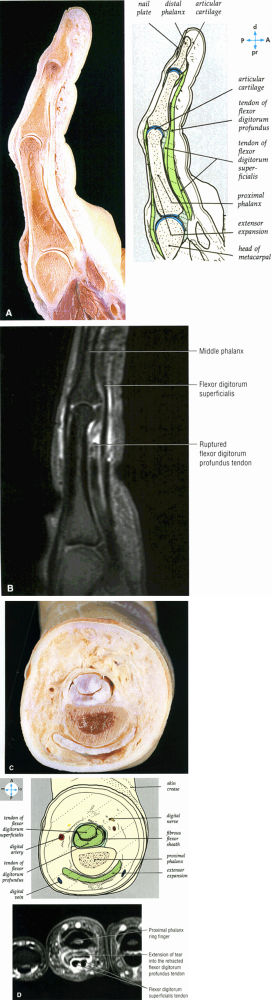 |
|
FIGURE 10.251 ● (A) A sagittal section of a finger shows the capsules and the relations of the joints. (B) Complete rupture of the flexor digitorum profundus of the ring finger (fourth digit) at the level of the mid-aspect of the proximal phalanx. Sagittal FS PD FSE image. (C) A transverse section through the index finger at the level of the proximal phalanx. (D) Axial FS PD FSE image of a flexor digitorum profundus (FDP) tear with rupture at the mid-aspect of the proximal phalanx of the ring finger. The ring finger is most frequently involved in FDP avulsions. In a type II avulsion, the FDP is caught at the chiasm of the flexor digitorum superficialis.
|
-
Discontinuity indicates complete disruption.
-
Tendon retraction, most easily visualized on sagittal images
-
Marrow edema at the site of the avulsion fracture
-
Profundus tendon in the area between the divisions of the flexor digitorum superficialis tendon
-
Fluid signal intensity along the course of the retracted flexor digitorum profundus
-
Associated tendinosis and tenosynovitis
-
Partial tendon tear
-
Fluid surrounding the flexor digitorum superficialis slips (divisions) and centrally (within the flexor digitorum profundus tendon gap) on axial images
-
Normal tendons demonstrate homogeneous hypointensity on both T1-weighted and FS PD FSE images.