Temporomandibular Joint
Editors: Berquist, Thomas H.
Title: Musculoskeletal Imaging Companion, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Chapter 2 – Temporomandibular Joint
Chapter 2
Temporomandibular Joint
Thomas H. Berquist
Anatomy
Key Facts
-
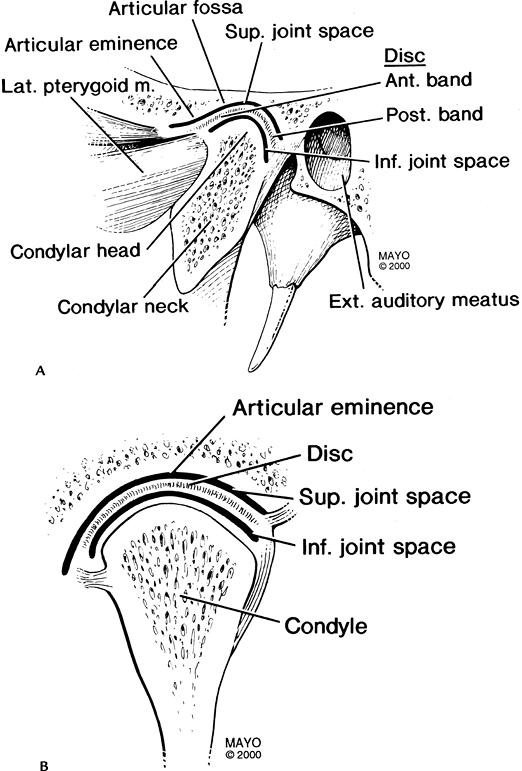
The temporomandibular joint (TMJ) is a synovial joint divided by a disc into superior and inferior compartments.
-
The normal disc is biconcave.
-
The posterior band is thicker and
separated from the anterior band by the thin intermediate zone, giving
the disc a “bow-tie” configuration. -
The posterior attachment (bilaminar zone) contains the neurovascular supply for the disc.
-
When the mouth is closed, the disc is at the apex of the mandibular condyle.
-
The normal disc remains centered over the condyle as the mouth opens.
P.16
 |
|
FIGURE 2-1 Normal TMJ in the sagittal (A) and coronal (B) planes.
|
P.17
Protocols
Imaging of the TMJ can be accomplished with multiple
methods. Routine radiographs, computed tomography, and magnetic
resonance imaging (MRI) are used most commonly in our practice.
methods. Routine radiographs, computed tomography, and magnetic
resonance imaging (MRI) are used most commonly in our practice.
Routine radiographs:
-
Anteroposterior
-
Towne
-
Oblique views of each TMJ
Computed tomography:
-
120 kVp, 270 mA, 25-cm field of view (FOV)
-
1- to 2-mm axial sections with bone and soft tissue windows
-
Reformatted sagittal and coronal images with 1.0-mm sections
MRI—basic approach:
-
3-inch dual-coupled coils
-
FOV: 10 to 12 cm 256 × 256 matrix, one excitation
-
Axial scout images (20/5, 40 degrees FA, 256 × 128 matrix, 4- to 5-mm–thick sections) through the TMJ
Technique 1:
-
Sagittal or oblique sagittal images in
the closed and open positions, 256 × 256 matrix, and three
acquisitions. T1-weighted (spin-echo 416/17) images (3 mm thick). Fast
spin-echo (turbo spin-echo 300/19) images (3 mm thick).Coronal fast spin-echo (turbo spin-echo 1500/19) images
optional if disc poorly visualized on sagittal images or medial or
lateral displacement is suspected.
Technique 2—motion studies:
-
Sagittal gradient-echo images (4-mm–thick
sections, 80/11, 30 degrees FA, 256 × 256 matrix, one acquisition, FOV
10–12 cm). Each image obtained as mouth is opened with incremental
device (3 mm per image). Images obtained from closed to open. Cine-loop
motion created. -
Optional coronal T1- or T2-weighted images.
Suggested Reading
Berquist TH, Helms CA. The temporomandibular joint. In: Berquist TH, ed. MRI of the musculoskeletal system, 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2006:98–120.
Gibbs SJ, Simmons C. A protocol for magnetic resonance imaging of the temporomandibular joints. Cranio 1998;16:236–241.
P.18
Internal Derangement
Key Facts
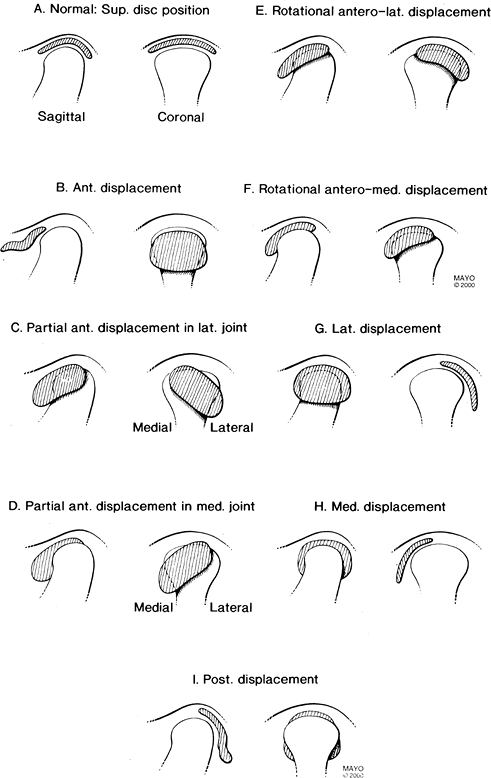
The disc is normally at the 12 o’clock position with the
mouth in the closed position. There is some degree of displacement in
up to 34% of asymptomatic patients.
mouth in the closed position. There is some degree of displacement in
up to 34% of asymptomatic patients.
-
Internal derangement is defined as an abnormal relationship or position of the disc to the condyle and articular eminence.
-
The cause is unknown, but trauma,
malocclusion, bruxism, hypermotility, ligament laxity, condylar
abnormalities, and stress are implicated. -
Females outnumber males 5:1.
-
Internal derangement is a progressive process.
-
Initially anterior, medial, or lateral displacement occurs when the mouth is closed, which reduces with opening.
-
The disc no longer reduces as elasticity decreases.
-
The disc becomes deformed with secondary bony changes.
-
Anterior displacement is most common, and
80% to 90% are bilateral. Stuck disc occurs in 4% to 11%, medial or
lateral displacement occurs in 5%, and posterior displacement occurs in
1%.
-
-
Clinical symptoms include pain, clicking, and reduced motion.
P.19
 |
|
FIGURE 2-2 Disc displacement categories: normal (A), anterior displacement (B), partial anterior displacement in lateral joint (C), partial anterior displacement in medial joint (D), rotational anterolateral displacement (E), rotational anteromedial displacement (F), lateral displacement (G), medial displacement (H), posterior displacement (I).
|
P.20
Suggested Reading
Aoyama
S, Kino K, Amagasa T, et al. Clinical and magnetic resonance imaging
study of unilateral sideways disc displacement of the temporomandibular
joint. J Med Dent Sci 2002;49:89–94.
S, Kino K, Amagasa T, et al. Clinical and magnetic resonance imaging
study of unilateral sideways disc displacement of the temporomandibular
joint. J Med Dent Sci 2002;49:89–94.
Milano
V, Desiate A, Bellin R, et al. Magnetic resonance imaging of
temporomandibular disorders: classification, prevalence, interpretation
of disc displacement and deformation. Dentomaxillofac Radiol 2000;29:353–361.
V, Desiate A, Bellin R, et al. Magnetic resonance imaging of
temporomandibular disorders: classification, prevalence, interpretation
of disc displacement and deformation. Dentomaxillofac Radiol 2000;29:353–361.
Tasaki
MM, Westesson PL, Isberg MA. Classification and prevalence of
temporomandibular joint disk replacement in patients and symptom-free
volunteers. Am J Orthod Dentofacial Orthop 1996;109:249–262.
MM, Westesson PL, Isberg MA. Classification and prevalence of
temporomandibular joint disk replacement in patients and symptom-free
volunteers. Am J Orthod Dentofacial Orthop 1996;109:249–262.
P.21
Anterior Disc Displacement
Key Facts
-
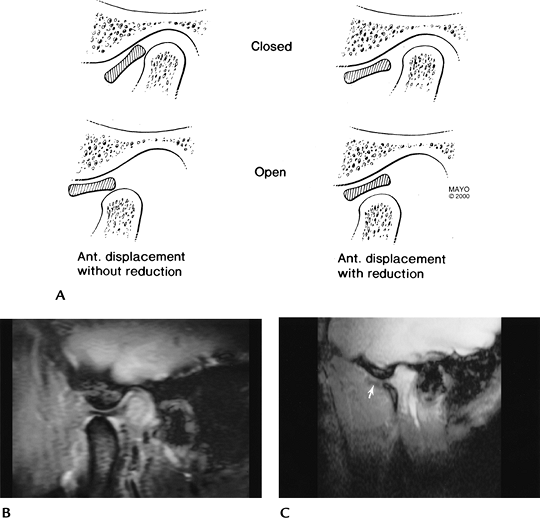
Anterior disc displacement occurs most commonly; 80% to 90% are bilateral.
-
Ninety percent of nondeformed anteriorly displaced discs reduce with opening.
-
Seventy-six percent of distorted discs do not reduce with opening.
-
Symptoms increase as disc deformity progresses.
-
Secondary signs of internal derangement.
-
Joint effusion
-
Joint space asymmetry
-
Marrow edema
-
Condylar erosion
-
Lateral pterygoid abnormalities
-
 |
|
FIGURE 2-3 (A) Anterior disc displacement without (left) and with (right) reduction. Sagittal gradient echo (80/11, 30 degrees FA) images demonstrate a normal disc in open-mouth position (B) and an anteriorly displaced disc (arrow) (C).
|
P.22
Suggested Reading
Foucart JM, Carpenter P, Pajoni D, et al. MR of 732 TMJs: Anterior, rotational, partial, and sideways disc displacements. Eur J Radiol 1998;28:86–94.
Kurita
H, Ohtsuka A, Kobayashi H, et al. Resorption of the lateral pole of the
mandibular condyle in temporomandibular disc displacement. Dentomaxillofac Radiol 2001;39:88–91.
H, Ohtsuka A, Kobayashi H, et al. Resorption of the lateral pole of the
mandibular condyle in temporomandibular disc displacement. Dentomaxillofac Radiol 2001;39:88–91.
Yang
X, Pernu H, Pyhtinen J, et al. MRI findings concerning the lateral
pterygoid muscle in patients with symptomatic TMJ hypermotility. Cranio 2001;19:260–268.
X, Pernu H, Pyhtinen J, et al. MRI findings concerning the lateral
pterygoid muscle in patients with symptomatic TMJ hypermotility. Cranio 2001;19:260–268.
P.23
LAteral Disc Displacement
Key Facts
-
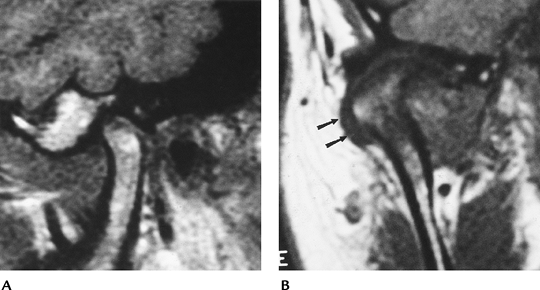
Anterior and anterolateral displacements account for 46% to 52% of disc displacements.
-
Rotational displacement was associated with 34% of displacements that did not reduce with opening and 53% of reducing discs.
-
Additional categories of internal
derangement include 11% with partial displacement, 4% with stuck discs
(disc does not move with condylar motion), and 1% with posterior
displacements. -
MRI is 95% accurate for disc position and classification and 93% accurate for osseous abnormalities.
 |
|
FIGURE 2-4 (A) Sagittal spin-echo 500/10 image does not clearly identify the disc. (B) Coronal spin-echo 500/10 image shows lateral displacement (arrows).
|
Suggested Reading
Foucart JM, Carpenter P, Pajoni D, et al. MR of 732 TMJs: Anterior, rotational, partial, and sideways disc displacements. Eur J Radiol 1998;28:86–94.
P.24
Trauma
Key Facts
-
Injury to the mandible and TMJ usually is secondary to a blow to the chin.
-
Injuries are most common in 15- to 30-year-old persons.
-
Multiple injuries to the mandible and TMJs are common.
-
TMJ injuries may involve soft tissues (subluxation, dislocation) or osseous and articular structures.
 |
|
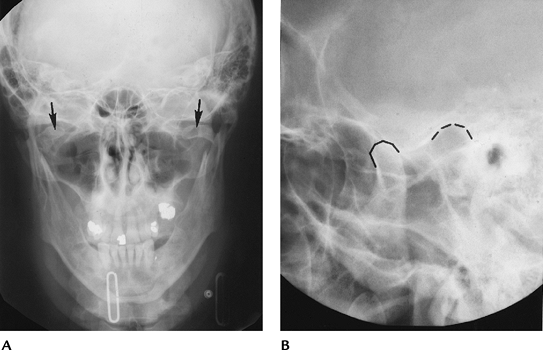
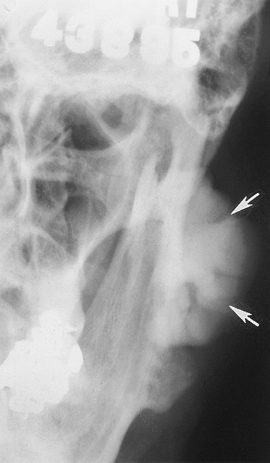
FIGURE 2-5 (A) Towne view demonstrating bilateral condylar neck fractures (arrows). (B) Coned-down lateral view demonstrating TMJ dislocation (broken lines define condyle and eminence).
|
Suggested Reading
Cascone
P, Leonardi R, Marino S, et al. Intracapsular fractures of the
mandibular condyle: Diagnosis, treatment, and anatomic and pathologic
evaluations. J Craniofacial Surg 2003;14(2):184–191.
P, Leonardi R, Marino S, et al. Intracapsular fractures of the
mandibular condyle: Diagnosis, treatment, and anatomic and pathologic
evaluations. J Craniofacial Surg 2003;14(2):184–191.
P.25
Osteoarthritis
Key Facts
-
Osteoarthritis is commonly associated with internal derangement.
-
The condition may be posttraumatic.
-
Computed tomography and MRI are most useful for evaluation.
 |
|
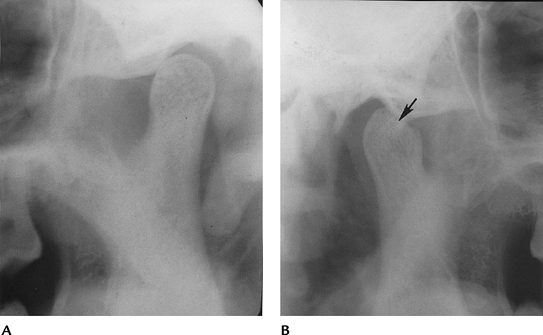
FIGURE 2-6 Posttraumatic arthritis with narrowing on the right (A) and an osteochondral defect (arrow) and subluxation on the left (B).
|
P.26
P.27
 |
|
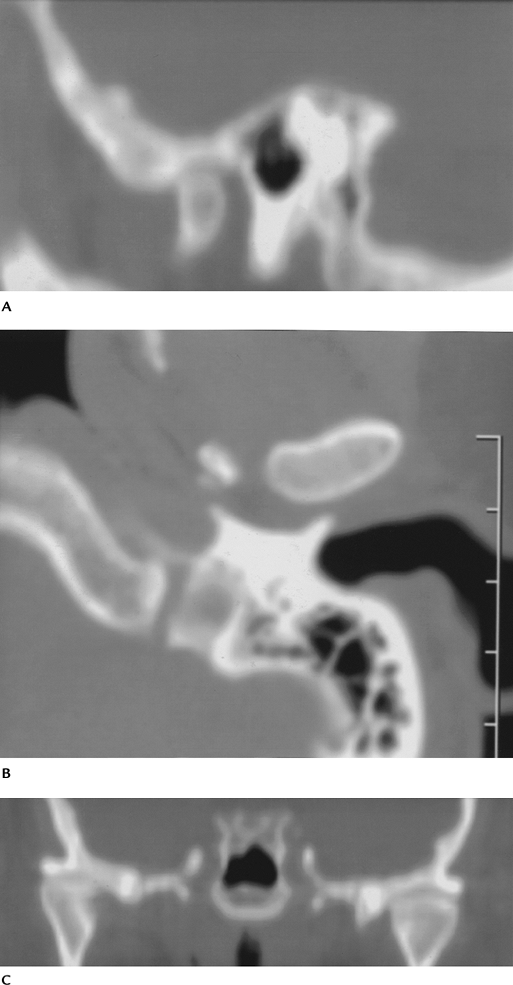
FIGURE 2-7 Osteoarthritis and internal derangement on sagittal (A), axial (B), and coronal (C) computed tomography images. There is joint space narrowing and asymmetry with osteophyte formation.
|
 |
|
FIGURE 2-8 Sagittal T1-weighted MR image with anterior disc displacement (arrow) and a condylar osteophyte (open arrow).
|
Suggested Reading
Westesson PL. Structural hard-tissue changes in temporomandibular joints with internal derangement. Oral Surg Med Oral Pathol 1985;59:220–224.
P.28
Miscellaneous Arthropathies
Key Facts
-
Multiple arthropathies can affect the
TMJ: rheumatoid arthritis (RA), juvenile chronic arthritis, psoriatic
arthritis, ankylosing spondylitis, systemic lupus erythematosus, gout,
and other crystal arthropathies. -
Some 28% to 63% of patients with juvenile chronic arthritis have TMJ involvement.
-
RA involving the TMJ is three times more common in females.
-
Up to 50% of patients with severe RA have TMJ involvement.
-
Patients may have joint erosions, laxity, and malocclusion.
-
MRI with contrast enhancement is most useful for complete evaluation of TMJ arthropathies.
 |
|
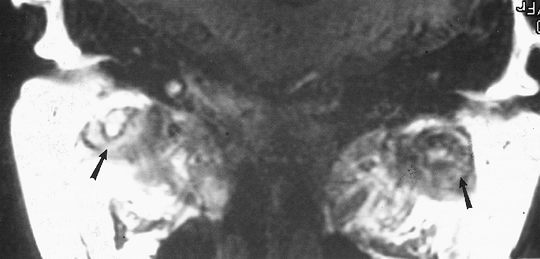
FIGURE 2-9 Coronal MRI in a patient with RA. There is extensive pannus formation bilaterally (arrows).
|
Suggested Reading
Kuseler
A, Pedersen TK, Herlin T, et al. Contrast-enhanced magnetic resonance
imaging as a method to diagnose early inflammatory changes in the
temporomandibular joint in children with juvenile rheumatoid arthritis.
J Rheumatol 1998;25:1406–1412.
A, Pedersen TK, Herlin T, et al. Contrast-enhanced magnetic resonance
imaging as a method to diagnose early inflammatory changes in the
temporomandibular joint in children with juvenile rheumatoid arthritis.
J Rheumatol 1998;25:1406–1412.
Ogus H. Rheumatoid arthritis of the temporomandibular joint. Br J Oral Surg 1975;12:275–284.
P.29
Tumors
Key Facts
-
Primary tumors in the TMJ region are rare.
-
Metastasis can occur, especially from breast carcinoma.
-
Fifteen of 1,907 (0.7%) benign tumors and 119 of 6,035 (1.9%) malignant tumors involve the mandible.
BENIGN AND MALIGNANT OSSEOUS TUMORS OF THE MANDIBLE
| Tumor | No. in mandible |
|---|---|
| Benign | |
| Giant cell tumor | 7 |
| Hemangioma | 4 |
| Neurolemmoma | 4 |
| Total | 15 |
| Malignant | |
| Lymphoma | 12 |
| Chondrosarcoma | 24 |
| Osteosarcoma | 39 |
| Fibrosarcoma | 17 |
| Total | 119 |
P.30
 |
|
FIGURE 2-10 A 65-year-old patient with jaw swelling. Anteroposterior radiograph demonstrates a large benign osteoma (arrows).
|
Suggested Reading
Unni KK. Dahlin’s bone tumors: General aspects and data on 11,087 cases. 5th ed. Philadelphia: Lippincott-Raven; 1996.
