STRESS FRACTURES
and military recruits. Runners, basketball and American football
players, dancers, and aerobic fitness enthusiasts are those at
significant risk for injury (6,13,16,17,25,27). The overwhelming majority of stress fractures occur in the lower extremity with 50% of cases involving the tibia and fibula (11,13,14,16,19). An increased incidence of stress fractures in women has been noted (3).
Although most of these injuries heal uneventfully with only rest from
the precipitating activity, certain stress fractures pose a challenge
to achieve and maintain union. Among these, fractures of the fifth
metatarsal proximal diaphysis, tarsal navicular, anterior tibial
diaphysis, and femoral neck frequently require surgical treatment.
injury. Of the numerous inciting factors that have been described, the
most common are rapid increases in the frequency, duration, or
intensity of an athletic activity. Anatomic and alignment factors such
as tibia vara, pronation, cavus, limited joint motion, and decreased
vascularity may be contributing factors in stress fractures of the
lower leg and foot (16,25,27) (See Chapter 10).
loads that exceed the remodeling capability of the involved bone.
Cyclic loading above the threshold level disrupts normal bone
remodeling, and osteoblastic activity becomes outpaced by osteoclastic
resorption. Li et al. have described the histologic changes in an
experimental model (15). Initially, vascular
congestion occurs, followed by osteoclast-mediated bone resorption in
the haversian canals and interstitial lamellae. Small cracks appear at
the cement lines of the haversian systems, which propagate into
microfractures. Simultaneously, new bone formation occurs as a result
of increased periosteal osteoblastic activity.
follow a recent increase in activity or a change in shoes or running
surface. Usually, symptoms subside with rest; without interruption of
activity, however, pain intensifies, performance is impaired, and overt
fracture can occur.
palpation. Pain often can be elicited by percussion over a distant site
of the involved bone. Especially in the foot, soft-tissue swelling can
be seen. A stress fracture of the tarsal bones or tibia should be
suspected in the foot with pronation just as a stress fracture of a
metatarsal should be considered in the cavus foot.
history and physical examination; confirmation requires radiographic
studies. Routine radiographs may be unremarkable for as long as 3 weeks
after the onset of symptoms and may never demonstrate an abnormality (20).
The technetium diphosphonate bone scan, although not specific for
diagnosis, is an extremely sensitive test for excluding a stress
fracture (22,23 and 24,29). Rarely, pain may antedate a positive scan, and if symptoms continue, a repeat scan is recommended (18).
If the bone scan demonstrates focal activity, tomography, computed
tomography, or MRI can be used to anatomically define the stress
fracture.
rest to surgical stabilization. Most stress fractures of the lower
extremity respond to avoidance of impact loading for a period of 4 to 8
weeks. During this time, aerobic conditioning can be maintained by
bicycling, swimming, or water running. A graduated return to impact
activity is started after resolution of pain. The most common fractures
involving the proximal and distal tibia, fibula, calcaneus, and central
metatarsals readily respond to this regimen.
from weight bearing is mandatory if nonoperative treatment is selected
for a stress fracture of the femoral neck. Immobilization and avoidance
of weight bearing are usually required for successful treatment of a
nondisplaced fracture of the tarsal navicular.
-
Femoral neck
-
Anterior tibia
-
Tarsal navicular
-
Fifth metatarsal (Jones)
A complaint of groin pain associated with activity requires
investigation and treatment without delay to avoid these potential
sequelae. Physical examination demonstrates pain with movement of the
hip and often a reduction in range of motion.
anteroposterior (AP) pelvis and frog lateral view of the hip, are
unremarkable, a bone scan is required. Evidence of a cortical
infraction or uptake along the superior aspect of the femoral neck
indicates a tensile-type fracture, which has a significant risk of
displacement (8). Internal fixation to prevent this is recommended as soon as possible (5,8). The method of internal fixation of the femoral neck is described in Chapter 19.
aspect of the femoral neck indicates a compression fracture that may be
amenable to conservative treatment (8). If,
however, a compression fracture is seen with a fracture line that
extends toward the superior cortex, immediate internal fixation is
advisable. Treatment of the stable compression-type femoral neck stress
fracture consists of avoiding weight bearing and serial radiographs to
ensure that displacement is not occurring and that healing is
progressing. Fracture healing may require up to 2 months from the time
of diagnosis. Return to activity requires resolution of pain, a full
range of motion of the hip, restoration of muscle strength and
endurance, and radiographic evidence of a healed fracture.
tibia are uncommon. First described in ballet dancers by Burrows, this
injury typically presents with localized pain associated with jumping (6).
On physical examination, there may be tenderness and palpable,
irregular thickening of the anterior cortex. Radiographs demonstrate
diffuse anterior cortical thickening containing one or more horizontal
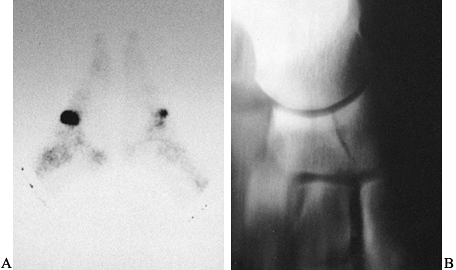
infractions (Fig. 96.1A, Fig. 96.1B).
 |
|
Figure 96.1.
Stress fracture of the anterior middiaphysis of the tibia. Notice the extensive cortical hypertrophy in addition to the transverse infraction (A) and the multiple horizontal translucencies (B). C: Immediately after IM nailing. D: Healed fractures with extensive anterior cortical thickening. |
nonunion or complete fracture despite rest and prolonged
immobilization, which are the initial recommended treatment (12).
Two factors may be responsible for this phenomenon: fracture
distraction as a result of tensile forces that are concentrated along
the anterior cortex and relative hypovascularity of the fracture area.
Electrical stimulation is combined with immobilization in a patellar
tendon-bearing (PTB) cast. The coils of the pulsed electromagnetic
field’s system are incorporated in the cast to overlie the fracture
site. The stimulator is used approximately 12 hours each day for 4 to 6
months (4). A bivalved,
removable cast facilitates nonimpact exercises of the lower extremity, including swimming.
symptomatic, surgical treatment is indicated. If a single fracture
exists, excision of the fracture site with cancellous bone grafting can
be used, but for multiple fracture lines, intramedullary nailing is
preferred (Fig. 96.1C, Fig. 96.1D) (2).
In the athlete, avoid the patella-splitting approach to minimize the
potential for patellar tendonitis. Intramedullary nailing is described
in Chapter 24.
-
Perform the procedure using a tourniquet and image intensifier.
-
Make a longitudinal incision centered
over the fracture, immediately lateral to the anterior tibial crest.
Longitudinally incise the crural fascia adjacent to the tibial crest,
and partially elevate the tibialis anterior to expose the fracture
area. Elevate periosteum medial and lateral to the crest. -
Using sharp osteotomes, remove the fracture and adjacent callus en bloc.
-
Use cancellous bone harvested from the iliac crest to fill the defect.
-
Reapproximate the periosteum with
interrupted stitches (0 absorbable). Position a 3-mm closed suction
drain superficial to the reapproximated periosteum and bring it out
through a separate proximal skin incision. Loosely reapproximate the
fascia and close the subcutaneous tissue and skin in an atraumatic
fashion using an Allgöwer stitch. Apply a well-padded splint to the
lower extremity, and admit the patient overnight for observation.
electrical stimulation unit to overlie the fracture area. Weight
bearing is allowed as tolerated. A PTB cast can be applied at 8 weeks.
Continue cast treatment until tenderness is absent and there is
radiographic evidence of healing. A return to vigorous jumping activity
or contact sports is not allowed until there is complete radiographic
union. This may require 6 to 9 months.
is frequently delayed because of the insidious onset, vague complaints
of pain on the dorsomedial aspect of the foot, and the frequency with
which routine radiographs do not demonstrate the injury (27,28).
Torg observed several factors associated with the injury, including
limited ankle dorsiflexion, limited motion of the subtalar joint,
shortening of the first metatarsal, metatarsus adductus, and
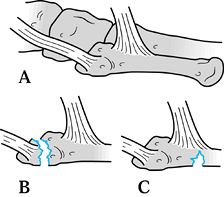
hypovascularity of the central one third of the navicular (27). Diagnosis is made with scintigraphy and tomograms in the AP plane (Fig. 96.2).
 |
|
Figure 96.2. A: Delayed bone scan indicating focal increased uptake in the region of the navicular bilaterally. B: Anteroposterior tomogram demonstrating navicular fracture.
|
fractures is avoidance of weight bearing and immobilization in a short
leg cast for 8 weeks. Surgical treatment is indicated for fractures
that are displaced at initial presentation or fail to heal with
immobilization. The preferred method of surgical treatment is open
reduction and internal fixation with lag screws.
-
Under tourniquet control, make a dorsal
incision centered over the navicular between the interval of the
tibialis anterior and extensor hallucis longus tendons. Retract the
deep peroneal nerve and dorsalis pedis artery laterally. -
With image intensification, approximate
the fracture edges, and from a medial or lateral approach, insert two
parallel 2-mm guide wires. -
Insert 4.0-mm cannulated lag screws of
appropriate length, making sure that no threads cross the fracture
site. If the fracture involves the extreme lateral third of the
navicular, it may be necessary to cut off excessive screw threads.
Occasionally, only one screw can be inserted. -
Cancellous grafting is not necessary unless the fracture edges are not compressed.
-
Perform routine closure of the wound, and immobilize the ankle with a well-padded posterior or U-splint.
in a non-weight-bearing short leg cast for 4 weeks. A controlled ankle
motion (CAM) walker allows protected weight bearing over the next 4
weeks. Eight weeks after surgery, remove the cast and begin
rehabilitative exercises for the foot and ankle, allowing progressive
weight bearing. Radiographic healing is required before resumption of
running or jumping. Tomography may be necessary to document
radiographic union. A return to full activity requires a minimum of 3
months (usually 4–6 months) following surgery.
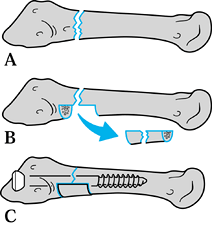
avulsion injuries of the tuberosity (dancer’s fracture) and fracture of
the proximal diaphysis (Jones fracture) (Fig. 96.3). Whereas avulsion injuries usually heal without the need for surgical treatment, fracture of the proximal diaphysis
often requires operative treatment, especially in the active patient.
Although stress fractures of the fifth metatarsal may present as an
acute injury, there is usually a history of discomfort antedating the
traumatic event.
 |
|
Figure 96.3. Patterns of proximal fifth metatarsal fractures. Peroneal brevis and tertius insetions (A), dancer’s avulsion fracture (B), and Jones fracture of the proximal diaphysis (C).
|
and tenderness over the lateral and plantar aspects of the proximal
diaphysis. This injury occurs frequently in basketball and American
football players and is not associated with any specific foot
configuration. At the time of presentation, routine radiographs can
demonstrate the fracture. As Torg described, intramedullary sclerosis
and widening of the fracture can be useful in diagnosing remote
injuries that have progressed to delayed union or nonunion (Fig. 96.4) (26). Successful treatment must take into account the activity level of the patient and the chronicity of the fracture.
 |
|
Figure 96.4. Nonunion of the fifth metatarsal with intramedullary sclerosis and fracture widening.
|
successful treatment can be achieved by cast immobilization combined
with strict avoidance of weight bearing for 6 to 8 weeks. In the
high-performance athlete, refracture after conservative treatment is
not unusual, and therefore, intramedullary screw fixation can achieve
early and persistent union with minimal morbidity and an early return
to activity (7). If a fracture has progressed
to delayed union or nonunion, intramedullary screw fixation or
medullary curettage and inlay bone grafting can be successful (26).
-
Select regional, epidural, or general
anesthesia, and position the patient on an operating table that allows
intraoperative use of the image intensifier. The lower extremity should
be internally rotated to provide access to the lateral border of the
affected foot. -
Under tourniquet control, palpate the
lateral base of the tuberosity of the fifth metatarsal, and make a
longitudinal incision from this point extending proximally for 3 cm.
Divide the subcutaneous tissue, protecting the branches of the sural
nerve and the insertions of the peroneus tertius and peroneal brevis at
the base of the tuberosity. Adduction of the forefoot increases
exposure of the metatarsal base. -
Under image intensification, introduce a
3.2-mm drill in line with the axis of the metatarsal. If necessary to
prevent penetrating the cortex of the shaft, reposition the drill.
Insert a 4.5-mm malleolar screw into the hole, making sure that the
screw remains intramedullary and that the threads completely pass
distal to the fracture site (Fig. 96.5). The
hole should not be countersunk to allow maximal compression. If the
canal is large, and adequate purchase is not obtained with the 4.5-mm
screw, redrill using a 4.5-mm drill bit and insert the appropriate
length 6.5-mm cancellous screw. If desired, a cannulated screw system
that allows insertion of an initial guide wire can be used. Figure 96.5. Jones fracture after insertion of a malleolar screw
Figure 96.5. Jones fracture after insertion of a malleolar screw -
Close the skin with interrupted sutures, and apply a well-padded splint to the foot and leg.
2 weeks, limiting weight bearing. After this period, remove the sutures
and fit the patient with a CAM walker, allowing progressive weight
bearing for an additional 3 to 4 weeks. Resistive exercises can be
started during this period. Resolution of pain and radiographic healing
usually occur by 8 weeks postoperatively. No further protection is
necessary after return to activity.
 |
|
Figure 96.6. Combined bone graft and internal fixation of a Jones fracture. Outlining the rectangular segment (A) and removing it (B). C: Insertion of a IM screw and placement of new corticocancellous graft from the iliac crest or distal tibia.
|
-
With the patient positioned as above,
make a straight 5-cm incision along the lateral border of the fifth
metarsal, centered over the tuberosity. -
Identify and protect sensory branches of
the sural nerve, and retract the peroneus brevis dorsally to expose the
inferior aspect of the tuberosity. Expose the fracture by incising the
periosteum. -
Use a curet and rongeur to trim the
sclerotic ends of the fracture. Outline and remove a small rectangular
cortical segment (2 × 1 cm) from the lateral and inferior area centered
over the fracture (Fig. 96.6A, Fig. 96.6B). -
Using a template, obtain a
corticocancellous block oversized by 2 mm in each direction from the
iliac crest along with cancellous graft. -
Pack the fracture area and intramedullary
canal with cancellous graft and press-fit the corticocancellous-block
into the trough bridging the fracture. -
If additional stability is desired,
insert an intramedullary screw as described above. This achieves a
“belt and suspenders” method of fixation (Fig. 96.6C). -
Close the skin and apply a well-padded splint as previously described.
walker for protected weight bearing for 6 to 8 weeks. Return to
activity usually takes 3 to 4 months.
scheme: 01, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
AC, Shelbourne KD, McCarroll JR, et al. The Natural History and
Treatment of Delayed Union Stress Fractures of the Anterior Cortex of
the Tibia. Am J Sports Med 1988;16:250.
JS, Balduini FC, Zelko RR, et al. Fractures of the Base of the Fifth
Metatarsal Distal to the Tuberosity: Classification and Guidelines for
Non-surgical and Surgical Management. J Bone Joint Surg 1984;66-A:209.
