ANKLE LIGAMENT INJURIES
Injuries of the distal tibiofibular ligaments (syndesmosis sprains) are
often associated with a protracted course of recovery and, in the case
of extensive injury, can cause diastasis of the ankle mortise leading
to subsequent arthritis (18).
tibiotalar capsule, the anterior talofibular (ATaF) and calcaneofibular
(CF) ligaments are the most clinically significant (8), functioning in reciprocal fashion to resist inversion loads applied to the ankle (33).
The ATaF progressively tightens as the ankle is moved from dorsiflexion
through plantarflexion, with the CF developing maximal tautness in
dorsiflexion (13,48).
excessive inversion force is applied to the plantarflexed ankle during
loading or unloading of the foot. Sequentially, the ATaF is torn,
followed by the CF and, ultimately, the posterior talofibular ligament
(PTaF) (1,6,17,47).
The spectrum of injury ranges from a mild sprain of one ligament to
frank rupture of both. Rarely, the PTaF is the ultimate ligament to
fail, an event that can cause frank dislocation of the ankle. Although
isolated injury of the ATaF is common, isolated rupture of the CF is
clinically unlikely (7,47).
tibiofibular ligaments (ATF and PTF), the inferior transverse ligament,
and the interosseous ligament. The ATF develops increasing strain with
external rotation of the talus, and both tibiofibular ligaments undergo
elongation with ankle dorsiflexion (13,14). The spectrum of injury to the syndesmosis can include latent or frank diastasis of the ankle mortise.
and is paramount to avoid missing adjacent injuries such as Achilles
tendon rupture, peroneal tendon dislocation, or severe midfoot injury (Table 95.1).
The mechanism may provide a clue to the type of injury: an inversion
mechanism suggests a lateral ligament sprain, whereas a dorsiflexion or
external rotation injury points to the possibility of a syndesmosis
injury. A “pop” or tearing sensation combined with pain that precludes
weight bearing as well as rapid swelling usually indicates a more
severe injury.
 |
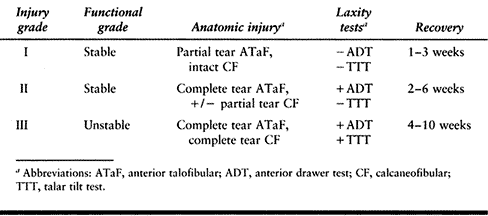
|
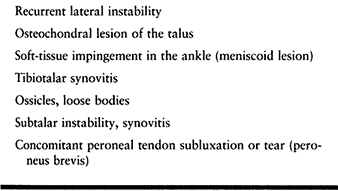
Table 95.1. Differential Diagnosis of Lateral Ankle Injuries
|
first few hours swelling remains localized and can aid in diagnosis.
Swelling confined to the inframalleolar area that occurs with a lateral
ligament sprain can be differentiated from the supramalleolar swelling
seen in a syndesmosis injury as well as the more distal swelling seen
over the sinus tarsi and midfoot that accompanies a subtalar or midfoot
sprain. Localized tenderness is suggestive of but not specific to
individual ligament injury. Palpate the malleoli, the entire fibula,
joint margins, and tendons about the ankle, confirming structural
integrity and eliciting any tenderness and crepitus. Tenderness
proximal to the ankle joint is characteristic of a syndesmosis injury.
Active and passive motion of the ankle is painful and decreased in both
types of sprains. Measurement of motion does not aid in diagnosis or
determination of severity. In addition to ascertaining the integrity of
the Achilles by squeezing the calf muscles and looking for plantar
flexion (31), assess the function of the
peroneal tendons by active dorsiflexion and eversion. An important part
of the exam is assessment of pedal pulses and the motor and sensory
function of the ankle and foot. Peroneal compartment syndrome as well
as traction injuries of the posterior tibial and peroneal nerves have
been described in severe sprains (44,50).
ligaments include the anterior drawer test (ADT), which measures
displacement of the talus in relation to the tibia (1,16).
The primary restraint to the ADT is the anterior talofibular ligament.
Injury of the calcaneofibular ligament does not affect the ADT (37). The preferred testing position is 10° of ankle plantarflexion, which allows maximum anterior talar translation (27).
This test usually can be performed in the presence of swelling without
inducing significant discomfort, as can Lachman’s test for rupture of
the anterior cruciate ligament of the knee. Stabilizing the distal leg
with one hand, apply an anterior force to the heel using the fingers
while the thumb rests along the anterior aspect of the ankle over the
talus. An increase of 3 to 5 mm side-to-side difference (STSD) on the
ADT indicates rupture of the anterior talofibular ligament (1,25,26).
talofibular (primary restraint) and calcaneofibular (secondary
restraint) ligaments. Performed in 10° of plantarflexion, the test also
measures inversion of both the tibiotalar and subtalar joints.
Palpating with the thumb along the tibiotalar joint allows an
estimation of talar tilt to be made. A STSD of at least 5° on the TTT
indicates rupture of both the anterior talofibular and calcaneofibular
ligaments (9,10,15).
Unlike the ADT, the TTT is often difficult to perform in the acute
injury because of pain and swelling. In addition, in the chronic
injury, it may prove difficult to differentiate subtalar motion. If
abnormal laxity is suspected, the talar tilt test should be assessed
using stress radiographs.
ankle ligaments. These radiographs may reveal associated osteochondral
injuries, avulsion fractures of the collateral ligaments from the
distal fibula, unsuspected widening of the mortise, as well as
unsuspected fractures of the malleoli. Occasionally, additional
radiographic views are necessary. If swelling and tenderness appear
distal to the lateral malleolus along the lateral foot, include a
medial oblique and an AP view of the foot to exclude fractures of the
anterior process of the calcaneus or base of the fifth metatarsal.
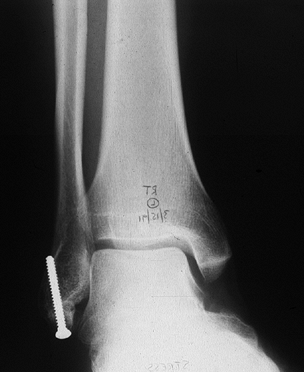
anterior drawer and talar tilt tests are negative on physical
examination, then stress radiographs are unnecessary. If clinical
laxity is apparent, the specific degree of abnormal translation can be
documented by obtaining both anterior drawer and talar tilt stress
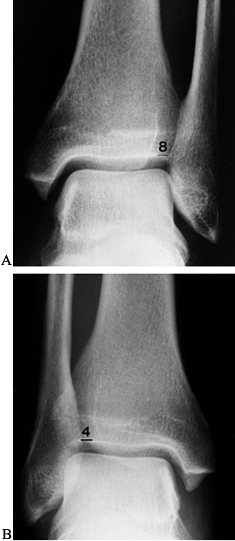
radiographs (Fig. 95.1 and Fig. 95.2).
If desired, 15 ml of 1% lidocaine can be injected into the ankle for
pain relief. The amount of anterior talar translation is measured as
the distance from a constant point on the posterior aspect of the talus
to the posterior lip of the tibia. Talar tilt is measured as the degree
of angulation of the superior aspect of the talus as referenced against
the neutral position of tibial plafond.
 |
|
Figure 95.1. Stress radiograph of a positive anterior drawer test (ADT).
|
 |
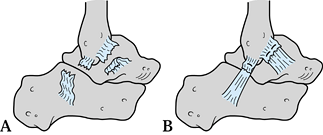
|
Figure 95.2. Abnormal stress radiographic talar tilt test (TTT) with more than 10° STSD: (A) injured ankle; (B) uninjured.
|
tonography were utilized to diagnose lateral ankle ligament tears.
Because so few acute lateral ligament injuries require early surgery,
these studies are now rarely performed. Magnetic resonance imaging
(MRI), although capable of demonstrating the anatomy of the injury, is
best used for diagnosing suspected osteochondral lesions of the talus
and peroneal tendon tears.
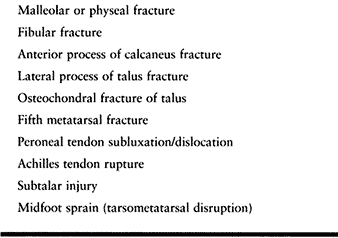
Grading is more difficult in the ankle than in other structures because
injuries can involve combinations of capsular rupture as well as
partial or complete tearing of one or more ligaments. Black (3) introduced the concept of single-and double-ligament injuries, and Singer and Jones (50) popularized the concept of stable and unstable injuries. Table 95.2 is a compilation of various classification criteria to provide a useful system for characterizing these injuries (29,45,50).
Stable injuries consist of a partial or complete tear of the anterior
talofibular ligament alone or with at most a partial tear of the
calcaneofibular ligament. Unstable injuries involve complete tears of
both ligaments. In a stable injury the ADT alone may be slightly
positive (3–5 mm STSD); in an unstable injury, however, the ADT will be
markedly positive (>5 mm STSD), and the TTT will show more than 5°
to 10° of STSD.
 |
|
Table 95.2. Classification of Lateral Ankle Sprains
|
differentiate stable from unstable sprains as well as to identify those
patients with one of the following factors: (a) bony avulsion or
osteochondral fragment or (b) acute injury superimposed on chronic,
recurrent lateral instability.
ankle with normal motion and to minimize the time lost from activity.
Although operative repair of significant ligament injuries has been the
standard previously, control studies have shown no difference between
the results of surgery and of nonoperative methods (20,22,34,43).
sprains. Initially use splinting and crutches until weight bearing is
nonpainful and there is no limp. Prescribe range-of-motion (ROM)
exercises and such modalities as ice, whirlpool, and electrical
stimulation, as pain allows. Start dorsiflexion and peroneal
strengthening exercises. Most patients can return to activity within 2
to 4 weeks.
unlikely to cooperate with the treatment schedule, then initial
splinting and elevation followed by immobilization by a short-leg
weight-bearing cast or a controlled ankle motion (CAM) walker is used
to treat all unstable injuries for a period of 3 to 4 weeks. If access
to therapy exists, prescribe an early functional rehabilitation program
similar to that advocated by Garrick (24).
Initial treatment utilizes intermittent cryotherapy and mechanical
compression, splinting with a removable compression splint
incorporating a felt horseshoe pad around the lateral malleolus or a
U-shaped splint, and avoiding weight bearing until ambulation is
nonpainful and there is no limp. Begin a program of ankle range of
motion, peroneal and dorsiflexion muscle strengthening, followed by
functional exercises (tilt board, jump rope, hopping). Depending on
severity of injury, return to activity can take 4 to 10 weeks. Use of
taping, an orthosis, and even high-top shoes may help decrease the
likelihood of future sprains (28,39,46).
Protect the ankle in a splint for 1 week and have the patient use a CAM
walker until clinical and radiographic evidence of union are seen
(usually 6–8 weeks).
 |
|
Figure 95.3. ORIF of avulsion injury of the lateral malleolus.
|
severe sprain occurs superimposed on a pattern of chronic recurrent
instability, acute surgery may be necessary. For repair of these
injuries, use the approach described for delayed repair (modified
Brostrom) (6,7).
Common postsprain complications include ankle pain secondary to
osteochondral lesions, ossicles, or the development of soft-tissue
impingement syndrome at the anterolateral corner of the tibiotalar
articulation (2,21,42). The most frequent problem, however, is recurrent instability.
 |
|
Table 95.3. Causes of Continuing Symptoms after Lateral Ankle Sprains
|
may note continuing pain, swelling, giving way, or functional
instability associated with pivoting and twisting on the affected ankle
and foot. Physical examination demonstrates peroneal weakness and calf
atrophy, tenderness to palpation over the lateral ligaments with
chronic soft-tissue swelling, and, most significantly, abnormal laxity
during the anterior drawer and the talar tilt tests. Routine
radiographs may demonstrate ossicles about the tip of the lateral
malleolus. The key to establishing the diagnosis is demonstration of
abnormal laxity using stress radiographs, as previously described.
diagnosis. Peroneal subluxation can be diagnosed by observing
retromalleolar tenderness and crepitus, with the ability to displace
the tendons on examination or spontaneous subluxation of the tendons
from the peroneal groove on active dorsiflexion and eversion of the
foot and ankle. Suspect subtalar instability, which can mimic or
coexist with lateral ankle instability, if total subtalar inversion
exceeds that of the normal side. Subtalar instability, however, may go
undetected unless stress radiographs are obtained or stress tomography
of the subtalar joint is performed (38). In the
absence of mechanical instability, loose bodies or ossicles of the tip
of the lateral malleolus can produce symptoms of instability.
Functional instability, as popularized by Freeman et al. (22),
occurs from loss of proprioception after lateral ligament injury and is
ameliorated by the same nonoperative exercise program utilized for
mechanical instability.
instability of the ankle respond to a program of peroneal
strengthening, proprioceptive training, and use of an ankle orthosis or
brace or taping. A tilt board is especially helpful to recondition the
ankle and lower leg and facilitates the transition back to sports.
In most instances, delayed primary repair of the anterior talofibular
and calcaneofibular ligaments is possible and, as such, is the
procedure of choice. Potential disadvantages of reconstructive
procedures include limitation of ankle and subtalar motion by the
nonanatomic location of the tendon graft and local morbidity from graft
harvest (8,12).
Indications for reconstruction as opposed to delayed primary repair
include severe lateral ankle instability of long duration, evidence of
subtalar hypermobility, or failure of a previous repair or
reconstruction.
-
Arthroscopy as described in Chapter 93
is useful as the initial procedure because a number of patients may
have chondral lesions of the medial talar dome. Before performing
arthroscopy, mark the lateral branches of the superficial peroneal
nerve as they cross the ankle to the foot. Plantarflexion of the ankle
facilitates this procedure. -
Place a bump underneath the ipsilateral
hip of the supine patient to allow internal rotation of the foot and
ankle, exposing the lateral malleolus. Prepare the skin and drape the
extremity free. -
Under tourniquet control, incise the skin (Fig. 95.4)
using an oblique incision, starting along the anterior border of the
lateral malleolus 2 to 3 cm proximal to the tip, passing inferiorly to
end proximal to the visible and palpable peroneal tendons.
Alternatively, with the ankle in maximum equinus, make the skin
incision immediately posterior to the prominence of the lateral
malleolus starting 3 cm proximal to the tip and following the peroneal
tendons distally (Fig. 95.5). This incision
completely avoids the lateral branches of the superficial peroneal
nerve and the sural nerve, provides better access to the
calcaneofibular ligament, and can be extended to perform an anatomic
reconstruction with split peroneus brevis tendon, if necessary.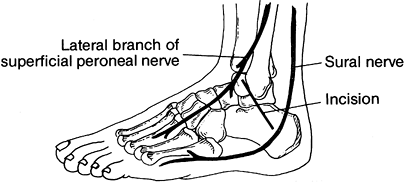 Figure 95.4.
Figure 95.4.
Oblique skin incision for modified Brostrom repair. Note proximity of
branches of superficial peroneal and sural nerves to ends of incision.
(From Mann RA, Coughlin MC. Video Textbook of Foot and Ankle Surgery. St. Louis: Medical Video Productions, 1991.)![]() Figure 95.5.
Figure 95.5.
With ankle plantarflexed, a longitudinal incision centered over the
posterior aspect of the lateral malleolus allows access to lateral
ankle ligaments. Proximal and distal extension (dotted lines) of the incision enables reconstruction using peroneus brevis tendon graft. -
Protect the lateral branches of the
superficial peroneal nerve along the anterior extent of the incision
and the sural nerve inferiorly and posteriorly as the subcutaneous
tissue is incised. Palpate the talus and the tip of the fibula while
passively moving the ankle to avoid inadvertently opening the subtalar
joint. -
Starting anteriorly, incise the capsule
and the normally attenuated anterior talofibular and calcaneofibular
ligaments 5 mm from their insertion on the fibula (Fig. 95.6). Do not transect the ligaments more than midway from their fibular attachment points to avoid overtightening.
P.2479
For better exposure of the calcaneofibular ligament, open the sheath and posteriorly retract the peroneal tendons.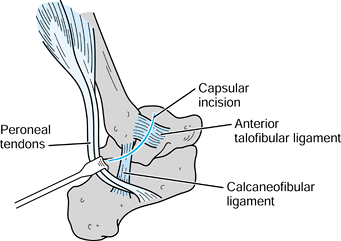 Figure 95.6. Capsular incision for ATaF and CF ligament repair.
Figure 95.6. Capsular incision for ATaF and CF ligament repair. -
Inspect the joint if it has not already
been examined arthroscopically, debride chondral lesions, and remove
loose bodies, as necessary. -
Preserving the proximal attachments of
the anterior talofibular and calcaneofibular ligaments, perform gentle
subperiosteal dissection of their fibular attachments in order to
roughen the fibular surface for improved healing. -
Place two 1-0 nonabsorbable sutures in
each distal ligament using a horizontal mattress-weaving configuration
and advance the distal ligaments under the tips of their respective
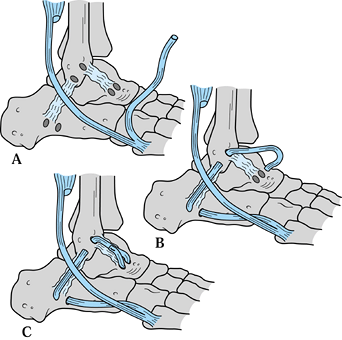
proximal attachments (Fig. 95.7). Tie the
sutures on the anterior aspect while the ankle and foot are maintained
in neutral flexion and slight eversion. Next, imbricate the proximal
end of each ligament over its distal end in a vest-over-pants manner.![]() Figure 95.7. A: Isolate and transect the ATaF and CF ligaments. B: Overlap and imbricate the ligaments.
Figure 95.7. A: Isolate and transect the ATaF and CF ligaments. B: Overlap and imbricate the ligaments. -
Repair the peroneal tendon sheath and the
joint capsule with 2-0 absorbable suture. If additional support for the
repair is desired, mobilize the inferior extensor retinaculum from the
sinus tarsi and imbricate it to the fibular periosteum proximal to the
ligament repair (26). This maneuver requires placing the foot in maximum eversion. -
Close the skin with interrupted 4-0 nylon
sutures and apply a short-leg, well-padded U-shaped splint to maintain
the ankle and foot in neutral position.
postoperatively, at which time remove the splint and sutures. Apply a
short-leg walking cast or have the patient use a CAM walker for an
additional 5 weeks. Start rehabilitation to regain active ankle and
subtalar motion. As motion is regained, add resistive exercises for the
peroneals and dorsiflexors of the ankle together with a tilt board for
proprioceptive conditioning. Once motion is restored and strength is
90% that of the normal ankle, begin functional exercises including
running and pivoting. The patient usually returns to activity by 3 to 4
months. Taping or use of an ankle orthosis is recommended during the
first year after surgery.
precise placement of the tendon graft to replicate normal anatomy,
thereby avoiding the limitation of subtalar motion that occurs with the
traditional Watson Jones and Chrisman Snook procedures (14). Anatomic reconstruction yields similar success in stabilizing the ankle (85%) without limiting subtalar motion (14) (refer to Fig. 95.8).
 |
|
Figure 95.8. Anatomic reconstruction for chronic lateral ligament laxity. A:
Anterior half of peroneus brevis is harvested, leaving distal insertion intact. Drill holes are made in the calcaneus, fibula, and talar neck as described in the text. B: Split tendon is passed through the drill holes in the calcaneus and fibula. C: Tendon graft is passed through talar neck drill holes and sutured to itself. |
-
Position the patient supine with a bump
beneath the ipsilateral hip. With the ankle in plantarflexion, make a
15-cm longitudinal incision centered over the prominence of the lateral
malleolus and extending toward the base of the fifth metatarsal. -
Protect the sural nerve, which lies in
the posterior portion of the incision. Open the peroneal tendon sheath
and identify the peroneus brevis tendon running anterior to the
peroneus longus at the ankle. Traction on the peroneus longus causes
the hallux metatarsal to flex in a plantar direction. Dissect the
muscle of the peroneus brevis from the anterior two thirds of the
peroneus brevis tendon, splitting the tendon longitudinally to its
P.2480
attachment to the base of the fifth metatarsal (Fig. 95.8A). Place a whipstitch (#2 nonabsorbable suture) tapering the free end of the graft to ease passage through the bony tunnels. -
Make bony tunnels in the calcaneus,
fibula, and talus with a 4.5-mm drill bit. Make a transverse tunnel at
the calcaneal insertion of the CF ligament. Maintaining a 1-cm bony
bridge, start both tunnels at 45° angles to converge beneath the
cortical bridge. Connect and enlarge the drill holes with a curette.
Now, at the fibular origin of the calcaneofibular ligament, drill a
tunnel from posterior to anterior that exits at the origin of the
anterior talofibular ligament. Next, drill a vertical tunnel on the
neck of the talus at the insertion of the anterior talofibular ligament. -
Before passing the tendon graft,
imbricate the anterior talofibular and calcaneofibular ligaments as
described in the section on delayed primary repair. Pass the tendon graft sequentially through the calcaneal, fibular, and talar tunnels (Fig. 95.8B). Coating the tendon with mineral oil and using a commercially available curved suture passer are helpful in passing the graft. -
Position the ankle in neutral and the
foot in near maximum eversion. Tighten the peroneal tendon graft.
First, suture the graft (#0 absorbable suture) to the calcaneofibular
ligament origin and insertion. Tighten the graft again and suture the
free end of the graft to the anterior talofibular limb (Fig. 95.8C). -
Check that ankle and subtalar motion are
preserved. Repair the peroneal tendon sheath at the level of the
lateral malleolus (2-0 absorbable suture). Release the tourniquet,
obtain hemostasis, and close the subcutaneous layer. Close the skin
with interrupted 3-0 nylon mattress sutures. Apply a well-padded
posterior splint.
and foot in a short leg cast, allowing weight bearing as tolerated. At
6 weeks discontinue immobilization and start rehabilitation using the
same schedule as for delayed primary repair. Patients can return to
sports at 6 months. An ankle brace or orthosis is used for the first
year of activity.
injury to the syndesmosis can have significant ramifications including
prolonged recovery from injury, ossification of the syndesmosis, and
diastasis of the ankle mortise if complete ligament rupture occurs (5).
Diastasis, latent or frank, can cause symptoms of instability, loss of
power with push-off, and eventually arthrosis of the ankle joint (18).
spreads to involve the entire ankle. Tenderness is present over the
anterior inferior tibiofibular ligament just above the ankle joint
margin and may extend to the posterior aspect of the distal
tibiofibular joint but does not extend to the inframalleolar region
laterally. Tenderness along the deltoid ligament medially in the
absence of tenderness of the lateral ankle ligaments should raise
suspicion of a syndesmosis injury. Compression of the malleoli and
squeezing of the midcalf (31), compressing hematoma within the injured syndesmosis, are quite painful. The usual ankle laxity tests are negative.
tenderness is present, include the entire tibia and fibula to avoid
missing an extensive syndesmosis rupture with associated proximal
fibula fracture. On the AP view, the fibula should overlap the tibia by
42% of the width of the fibula, and on the mortise view the separation
of the tibia and fibula should not exceed 5 mm (30). A comparison view is helpful (Fig. 95.9).
Radiographic evidence of lateral talar shift in the absence of a fibula
fracture confirms combined rupture of the deltoid ligament and
syndesmosis (Fig. 95.10). If latent diastasis is suspected, obtain a stress AP or mortise view by applying external rotation to the foot and ankle.
 |
|
Figure 95.9. Syndesmosis disruption (A) compared to normal mortise (B).
|
 |
|
Figure 95.10. Lateral talar shift confirming deltoid ligament tear associated with syndesmosis rupture.
|
successful early resolution are to keep the limb immobilized and have
the patient keep weight off it. Between sessions for range-of-motion
exercises and therapeutic modalities, immobilize the injury in either a
bivalved short leg cast or a CAM walker. Do not allow weight bearing
until the ankle is nonpainful and the patient is able to walk
unprotected without a limp—usually 3 to 4 weeks but possibly up to 6
weeks. Thereafter, treatment is similar to that of a lateral ankle
sprain.
-
If diastasis is present, either frank or latent, surgery is necessary.
-
Anatomic reduction of the fibula into the
sulcus on the tibia in both the medial–lateral and anteroposterior
planes is essential. Fixation can be done using closed percutaneous
technique, or the syndesmosis can be opened if reduction is uncertain
or the injury is old and interposed scar tissue prevents reduction.
Maintain closed reduction of the syndesmosis by a positional,
P.2481
nonlagged
3.5-mm cortical screw. In large men, a 4 to 5-mm cortical screw may be
necessary to prevent breakage. Placed 2 to 3 cm above the tibiotalar
joint, the screw should engage both fibular and tibial cortices. -
Postoperatively, use a well-padded
U-splint for 1 week and then start ROM exercises and peroneal and
dorsiflexor strengthening. Allow protected weight bearing for 3 to 4
weeks. If desired, remove the screw before return to sports at 2 to 3
months, although breakage is not likely (36).
weakness with push-off during running and jumping are not uncommon.
These symptoms may last for more than a year in the high-performance
athlete. Stiffness of the ankle may develop as a result of ossification
of the syndesmosis ligaments (Fig. 95.11). After ossification, patients experience a greater incidence of inversion sprains of the ankle (52). Excision of the ossification is usually not necessary, however.
 |
|
Figure 95.11. Posttraumatic syndesmosis ossification.
|
side of the ankle are much less common than lateral injuries. Rupture
of the deltoid ligament commonly accompanies fractures of the lateral
malleolus because of external rotation-eversion or abduction injuries.
These fractures are usually treated with internal fixation. Exploration
and repair of the deltoid ligament is rarely required unless
interposition prevents reduction or an osteochondral fracture is
suspected.
rotation or ankle eversion injury with medial ankle pain. Physical
examination usually provides the diagnosis, as there is localized
tenderness and swelling directly over the ligament. Grade I tears are
anterior and progress posteriorly as the tear increases in severity.
There may be instability on eversion stress. Radiographs may be
necessary to rule out a fracture. Other conditions that may mimic a
deltoid ligament tear include injuries to the posterior tibial tendon
or spring ligament.
nonoperatively. Stable injuries can be treated as described for lateral
ligament sprains. More severe sprains that are very painful or are
unstable may require use of a short leg walking cast or CAM walker for
3 to 4 weeks.
scheme: *, classic article; #, review article; !, basic article; and +,
clinical results/outcome study.
KJ, Lecocq JF, Lecocq EA. Recurrent Anterior Subluxation of the Ankle
Joint: A Preliminary Report of Two Cases and an Experimental Study. J Bone Joint Surg [Am] 1952;34:853.
OD, Snook GA. Reconstruction of the Lateral Ligament Tears of the
Ankle: An Experimental Study and Clinical Evaluation of Seven Patients
Treated by a New Modification of the Elmslie procedure. J Bone Joint Surg [Am] 1969;51:904.
TA, Hillman SK. Comparison of Support Provided by a Semirigid Orthosis
and Adhesive Ankle Taping Before, During, and After Exercise. Am J Sports Med 1990;18:498.
P, Renstrom P. Current Concepts Review; Treatment for Acute Tears of
the Lateral Ligaments of the Ankle: Operation, Cast, or Early
Controlled Mobilization. J Bone Joint Surg [Am] 1991;73:305.
J, Bergsten T, Lansinger O, et al. Reconstruction of the Lateral
Ligaments of the Ankle for Chronic Lateral Instability. J Bone Joint Surg 1988;70A:581.
RA, Ashton-Miller JA, Kothari SU, et al. Basketball Shoe Height and the
Maximal Muscular Resistance to Applied Ankle Inversion and Eversion
Moments. Am J Sports Med 1995;23:418.