Radial and Ulnar Shaft Fractures
stability. In fish, amphibians, and birds, the forearm skeletons are
rigid in order to provide stability. In reptiles and some mammals, the
huge pisiform contributes to a three-bone forearm skeleton articulating
with the carpal bones and thus allowing only side-to-side movement. The
appearance of bipedalism in evolution freed the upper extremity from
the requirements of support, placing greater emphasis on increasing
mobility rather than stability.2 The
recession of the pisiform from the forearm and the appearance of the
synovial distal radioulnar joint (DRUJ) were the crucial steps in the
development of pronation and supination, which greatly increased the
mobility of the forearm and the wrist.
extremity function, facilitating placement of the hand in space thus
helping to provide the upper extremity with its unique mobility. The
presence of the proximal and distal radioulnar joints allows pronation
and supination, and such movements are important to all of us in the
usual activities of daily living. Moreover, the forearm serves as the
origin for muscles inserting on the hand. Therefore, fractures
involving the bones of the forearm present unique problems not
encountered with fractures of other long bones and may significantly
affect the function of the upper limb.
fractures can facilitate restoration of function and is now the
standard for treatment of fractures of the shaft of the forearm. This
is supported by the good results of rigid plate fixation in many
studies. Dynamic compression plating has been used in the past. In an
attempt to preserve vascularity of the bone, new plates with limited
contact between the plate and the bone have been devised. A new locking
screw concept has also been introduced in plate fixation of forearm
fractures.
shafts of forearm, fracture-dislocations involving fractures of the
radius associated with DRUJ injury (Galeazzi fracture), and fractures
of the ulna associated with proximal radioulnar joint injury
(Monteggia fracture). A description of the Essex-Lopresti injury is also included.
of the radius and ulna. Common to all, a significant energy of trauma
must be present before the forearm bones can be broken. Most forearm
diaphyseal fractures are caused by a fall from standing height, a
direct blow, or a road traffic accident. Causes of direct blow injuries
include fights in which the victim is struck on the forearm with a hard
object. By instinct, the victim lifts up the forearm to defend against
an attacker and to protect his or her head. The forearm is then the
recipient of the violence. An isolated fracture of the ulna shaft
resulting from such a direct blow, known as a nightstick fracture, can
occur at any site along the ulnar length. It is often more stable than
other forearm fractures, especially if the displacement is less than
50% when there is less injury to the interosseous membrane.22
disability with damage to associated tendons and nerves. A common cause
of open fractures is gunshot injury. Besides nerve or soft tissue
injuries, there is frequently significant bone loss, leading to delay
in healing and the necessity for additional surgery.
displaced. This is usually due to the significant force causing the
fracture in adults and also the fact that the pull of the fracture
fragments by the forearm muscle tends to accentuate the displacement.
As a result of the displacement and the instability, the diagnosis can
easily be made from the signs and symptoms, including pain, deformity,
and loss of function. In nightstick fractures, palpation along the
subcutaneous border of the ulna usually elicits tenderness at the level
of the fracture. Some degree of swelling is almost always present and
is usually related to both the force causing the injury and the time
since the injury.
evaluation of the motor and sensory functions of the radial, median,
and ulnar nerves, especially in open fractures with penetrating injury
which are commonly associated with nerve and major blood vessel injury.
If the forearm is swollen and tense, a compartment syndrome may be
present or may be developing. In such cases, pain on passive stretch as
well as neurologic deficit should be sought. Compartment pressures
should then be measured and immediate treatment by fasciotomy is
required when a compartment syndrome is diagnosed (see Chapter 27).
associated injuries to the soft tissues, particularly the ligaments of
the elbow and the wrist, are often seen. There are three such lesions
that are associated with forearm fractures: the Monteggia, Galeazzi,
and Essex-Lopresti lesions. Prompt recognition of these injuries is
important, since the correct treatment should consist of both adequate
fracture stabilization and accurate restoration of the normal wrist and
elbow articulation. In order to achieve this, soft tissue repair and
reconstruction is sometimes needed. These three injuries are described
in the following section.
dislocation of the radial head are uncommon injuries that comprise less
than 5% of all forearm fractures. This injury was first described by
Monteggia in 1814.
dislocation will complain of pain about the elbow and a mechanical
block to elbow flexion and forearm rotation. Depending on the type of
Monteggia injury, the radial head may be palpable over the anterior or
posterior aspect of the elbow.
nerves, especially the posterior interosseous nerve with a reported
incidence as high as 17%.11 The
cause of the injury is often due to stretching of the nerve by a
dislocated radial head. According to the reports by Spinner95 and later Boyd and Boals,9
all of these nerve palsies recover spontaneously. However, entrapment
of the posterior interosseous nerve causing a Monteggia lesion to be
irreducible has occasionally been reported.75,94,105
In these rare situations, an open exploration of the nerve should be
performed. Even with successful closed reduction of the radioulnar
articulation, if there is no return of function by 8 weeks, a surgical
exploration and decompression of the nerve is advocated.54 Injuries of other nerves, including the anterior interosseous nerve,26 median nerve, and ulnar nerve can also occur.
distal thirds commonly occurs in association with a dislocation of the
DRUJ (Fig. 31-1). This lesion, reported by Galeazzi30
in 1934, is characterized by its unstable nature and the need for open
reduction and internal fixation to achieve a satisfactory functional
outcome. A high index of suspicion should be maintained by the surgeon,
especially when the radiographs show a widened gap between the distal
radius and the ulna and a relative shortening of the radius. Any
instability of the DRUJ must be detected by careful ballottement after
the radius fracture has been surgically stabilized.
results from the large force that caused the radial shaft fracture and
was then transmitted via the interosseous membrane to the ulna. The
ulnar head is dislocated and tearing of the triangular fibrocartilage
complex occurs, rendering the entire DRUJ complex unstable. The ulnar
styloid may be fractured. A special type of Galeazzi injury with both
the radial and ulnar shaft fractured71 can also occur, and sometimes disruption of the distal radioulnar joint may be overlooked.
in 1951 and is a rare complex injury of the forearm that may be best
described as a radioulnar dissociation. It usually occurs after a fall
on the outstretched hand, resulting in a fracture of the head of the
radius and disruption of both the interosseous membrane and the DRUJ
leading to proximal migration of the radius. It is often missed because
of the attention directed to the radial head fracture to the exclusion
of the rest of the forearm. The pathomechanics of the proximal
migration of the radius was shown by Hotchkiss et al.50
to be a result of the large force causing the fracture and concomitant
disruption of the DRUJ together with the interosseous membrane. Besides
radial head fractures, such
proximal migration of radius and disruption of DRUJ joint has also been associated with Galeazzi fracture,58 radial shaft fracture,24 and elbow dislocation.7
 |
|
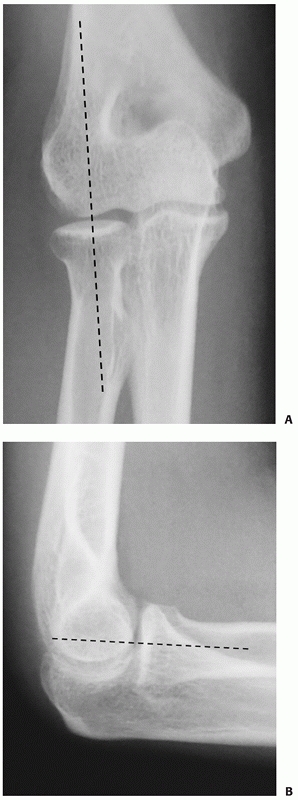
FIGURE 31-1 A Galeazzi fracture dislocation. Anteroposterior (A) and lateral (B) views.
|
of radial head fractures. Hence, Essex-Lopresti injuries can easily be
overlooked or the correct diagnosis is delayed unless a careful history
is taken to elicit symptoms of wrist pain and examination of the
forearm and wrist is performed. All patients with comminuted radial
head fractures should have radiographs of their wrists to assess radial
length.
the forearm are usually sufficient to diagnose a forearm fracture. The
elbow and wrist must be included in order to exclude associated
articular fractures or fracture-dislocations and especially any
Monteggia, Galeazzi, or Essex-Lopresti lesions. Computed tomography
scan or magnetic resonance imaging is rarely required. The
configuration of shaft fractures of the radius and ulna varies
depending on the mechanism of injury and the degree of violence
involved. Low-energy fractures are often not comminuted and of short
oblique or transverse type, whereas high-energy injuries often cause
comminuted or segmental fractures.
wrist joints as they have significant implications for prognosis and
treatment. In cases where there is uncertainty about the integrity of
the proximal or DRUJs, an oblique view can also be taken. In any of the
projections of the proximal forearm, a line drawn through the proximal
radial shaft and the center of the radial head should pass through the
center of the capitellum,69 as shown in Figure 31-2.
ulna on an anteroposterior radiograph. On a true lateral projection,
the distal ulna may also be dorsally displaced. There may also be a
fracture of the ulnar styloid at its base. Ring et al.84
defined injury of the DRUJ as more than 5 mm of ulnar-positive variance
on radiographs taken before any manipulative or surgical reduction.
Ultrasound examination can be used to detect interosseous membrane
tears.29
 |
|
FIGURE 31-2 On normal radiographs, a line drawn through the proximal radial shaft (A) and the center of the radial head (B) should pass through the center of the capitellum.
|
described according to the level of fracture, the pattern of the
fracture, the degree of displacement, the presence or absence of
comminution or segmental bone loss, and whether they are open or
closed. For descriptive purposes, it is also useful to divide the
entire length of the radius and ulna into upper, middle, and lower
thirds.
 |
|
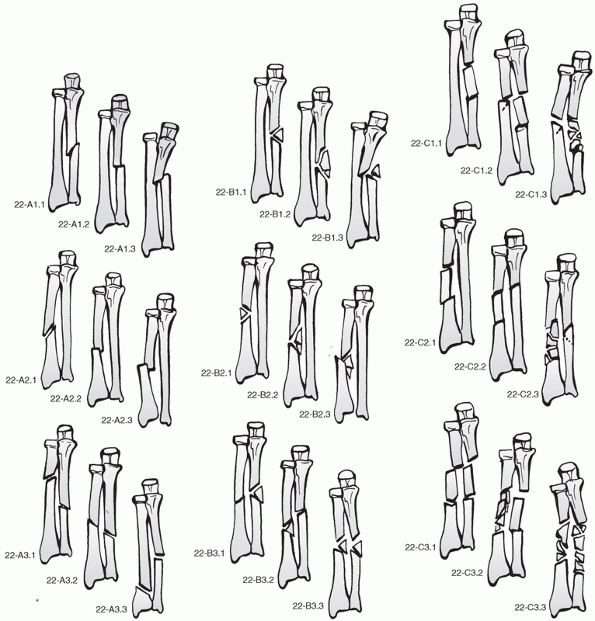
FIGURE 31-3 AO/OTA classification.
|
Type A fractures are the unifocal simple fracture with A1 being
isolated ulnar fractures, A2 radial fractures, and A3 fractures in both
bones. In the A1 and A2 fractures, the
suffixes
refer to the morphology of the fracture and the presence of a proximal
or distal dislocation of the radioulnar joint. The A1.1 and A2.1
fractures are oblique and the A1.2 and A2.2 fractures are transverse.
The suffix .3 indicates either a Monteggia fracture (A1.3) or a
Galeazzi fracture (A2.3). In A3 fractures, the suffix relates to the
position of the radial fracture with A3.1 being in the proximal third
of the radius, A3.2 in the middle third, and A3.3 in the distal third.
of is similar to type A fractures although it also differentiates
between an intact or a fragmented wedge. In B1 and B2 fractures, the
suffix .1 signifies an intact wedge, .2 a fragmented wedge, and .3 a
fracture-dislocation. B1.3 fractures are Monteggia lesions and B2.3 are
Galeazzi fractures. B3 fractures are both bone fractures with the
suffix signifying different combinations of simple and wedge fractures
(see Fig. 31-3).
complex ulnar fractures with (C1.2) or without (C1.1) a simple radial
fracture. C1.3 is a Monteggia fracture with a complex ulnar fracture
and simple radial fracture. C2 fractures are similar with the complex
fracture being radial and the C2.3 being a Galeazzi fracture. C3
fractures are complex fractures involving both bones with the
complexity increasing from C3.1 to C3.3.
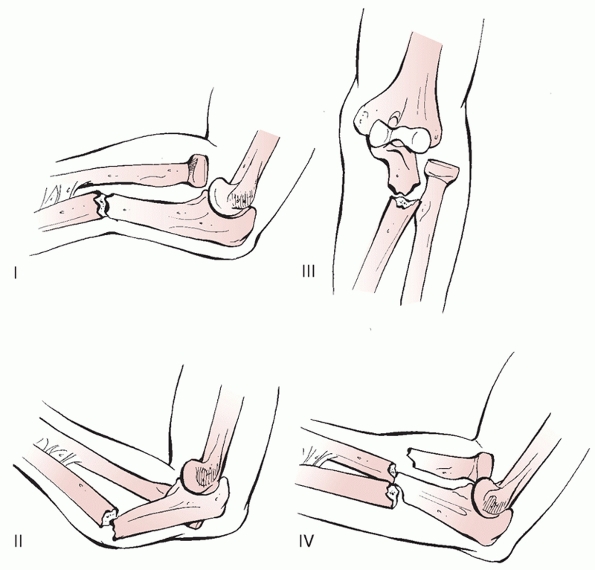
dislocation of the radial head was first described by Monteggia in
1814. In 1967, Bado3 reported a series of such injuries, and he classified the injury into four distinct types (Fig. 31-4):
with anterior angulation at the fracture site and an associated
anterior dislocation of the radial head (Fig. 31-5A).
|
TABLE 31-1 The Epidemiology of Forearm Fractures
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|
FIGURE 31-4 Bado classification of Monteggia fracture dislocation.
|
angulation at the fracture site and a posterolateral dislocation of the
radial head.
radius and ulna at the same level with an anterior dislocation of the
radial head.
In type 2a, the fracture of the ulna involves the distal part of the
olecranon and the coronoid process. In type 2b, the fracture is at the
metaphyseal-diaphyseal junction distal to the coronoid, and in type 2c,
the fracture is diaphyseal. The fourth subtype, type 2d, extends into
the proximal half of the diaphysis of the ulna. A complex variation of
the type 2 Monteggia with associated ulnohumeral dislocation has also
been reported.79
fractures. In adult patients, the Bado type 2 injury is the most
common, being reported in 59% to 79% of cases.60,82
In these reports, type 1 injuries occur in 15% to 30%, with types 3 and
4 occurring in very few cases. Males and females were equally
represented, and the average age was 52 years. Sixty percent of cases
were low-energy injuries. However, when the Bado types 1 and 2 injuries
were compared there was a preponderance of middle-aged to elderly women
with Bado type 2 fractures, with much higher prevalences of coronoid
and radial head fractures.82
the radius with a dislocation of the DRUJ. These injuries account for
3% of forearm fractures (see Chapter 3) and are more common in
males.71,74
They can be separated into two types: type 1 in which the radial
fracture is in the distal third within 7.5 cm of the distal radial
articular surface and type 2 in which the radial fracture is in the
middle third of the radius and more than 7.5 cm from the articular
surface of the distal radius.80 Type 2 fractures are more likely to have DRUJ instability with a reported prevalence of 55% compared to 6% in type 1 fractures.80
 |
|
FIGURE 31-5 A. A type I Monteggia fracture dislocation. B. A type III lesion
|
high-energy injury occurring in patients ranging in age from youth to
middle age. Edwards and Jupiter24
classified the injury depending on the type of radial head fracture.
Type 1 fractures were large displaced radial head fractures. Type 2
fractures were severely comminuted radial head fractures, and type 3
were old injuries with irreducible proximal migration of the radius.
|
TABLE 31-2 Monteggia Equivalents Described by Bado4
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
of muscles, tendons, bones, and joints. A coordinated function of all
these structures is responsible for arm and hand movement, including
rotation.
contact with each other only at the two ends. During rotational
movements, the radius rotates around the relatively immobile ulna.
Besides coordinated muscle exertion, these movements also rely on the
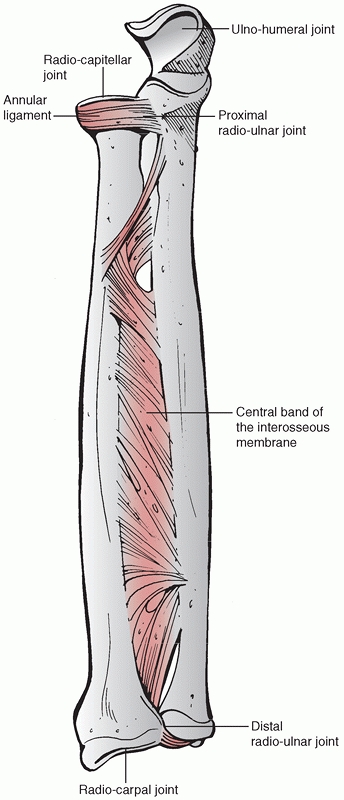
normal function of five articulations (Fig. 31-6).
At the elbow, the two bones articulate directly with the humerus to
form the ulnohumeral and the radiocapitellar joints. At the wrist, only
the radius articulates directly with the carpal bones to form the
radiocarpal joint. The two bones also articulate with each other
proximally and distally at the proximal and distal radioulnar joints.
The two bones are bound proximally by the capsule of the elbow joint
and the annular ligament and distally by the capsule of the wrist
joint, the dorsal and volar radioulnar ligaments, and the triangular
fibrocartilage complex. The interosseous membrane is frequently
referred to as a separate joint of the forearm bones, and its
disruption or contracture can lead to instability or stiffness.
smoothly, the ulna has a relatively straight form, but the radius has a
more pronounced curve. Sage87
measured the curves in cadaveric radii and found that the proximal
curvature averaged 13.1 degrees apex medial and 13.1 degrees apex
anterior in the coronal and sagittal planes, respectively. The distal
curvature averaged 9.3 degrees apex lateral and 6.4 degrees apex
posterior in the coronal and sagittal planes, respectively. He87
pointed out the importance of maintaining these curves, especially the
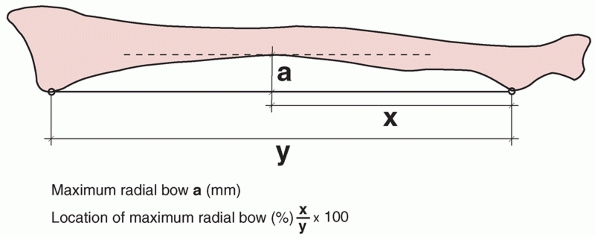
lateral bow of the radius. A study by Schemitsch and Richards90
confirmed the importance of restoration of the radial bow for forearm
function after fracture. They described a method of quantifying
the amount and location of the radial bow (Fig. 31-7)
and correlated restoration of the radial bow with forearm function.
They found that restoration of function was significantly better in
cases in which the radial bow was restored to a mean of less than
1.5-mm difference and to within 9% for the location compared to the
opposite side.
 |
|
FIGURE 31-6
The two bones are connected by ligaments at the proximal and distal radioulnar joints and in their midportions by the interosseous membrane that transmits any force at the wrist from the radius to the ulna. The central part of the interosseous membrane is thickened to form the central band. There are five articulations, namely the radiohumeral, the ulnohumeral, radiocarpal, and the proximal and distal radioulnar joints. |
into consideration during fixation of an ulnar fracture. There is an
apex posterior bow along the entire length of ulna that can be
visualized on a lateral radiograph. The posterior border of the ulna is
subcutaneous and easily palpable throughout its length.
ulna are both triangular in cross section with their interosseous
apices representing the attachment of the interosseous membrane. The
fibers of the interosseous membrane run obliquely across the
interosseous space from the proximal radius at the level of the
pronator quadratus to the junction of the middle and distal thirds of
the ulna. It consists of a thin membranous part and a thick ligamentous
part called the central band, which measures about 3.5 cm in width and
is 2 or 3 times as thick as the membranous part (see Fig. 31-6). Experimental studies by Hotchkiss et al.50
showed that incision of the triangular fibrocartilage complex alone
decreased relative stability by 8%. Incision of the triangular
fibrocartilage complex and interosseous membrane proximal to the
central band decreased stability by only 11%. Incision of the central
band, however, reduced stability by 71%. The thickened central band of
the interosseous membrane is a constant structure and is the second
principal stabilizer of the radius, particularly when the radial head
is injured and requires resection. Proximal migration of the radius may
occur following radial head resection resulting in painful ulnocarpal
impingement.
groups of muscles: the mobile wad and the flexor pronator group. The
mobile wad consists of brachioradialis, extensor carpi radialis longus
(ECRL), and extensor carpi radialis brevis (ECRB). They lie on the
lateral side of the forearm and are innervated by the radial nerve. The
flexor-pronator group lies on the medial aspect and has three layers:
-
Superficial—pronator teres, flexor carpi
radialis (FCR), palmaris longus, and flexor carpi ulnaris (FCU), in
order from lateral to medial -
Middle-flexor digitorum superficialis (FDS)
-
Deep-flexor digitorum profundus (FDP), flexor pollicis longus (FPL), and pronator quadratus
forearm. The superficial extensors (extensor digitorum communis [EDC],
extensor digiti minimi and extensor carpi ulnaris [ECU]) and anconeus
lie on the ulnar aspect. The extensors are supplied by the posterior
interosseous nerve while the anconeus has its own branch of the radial
nerve arising proximal to the elbow.
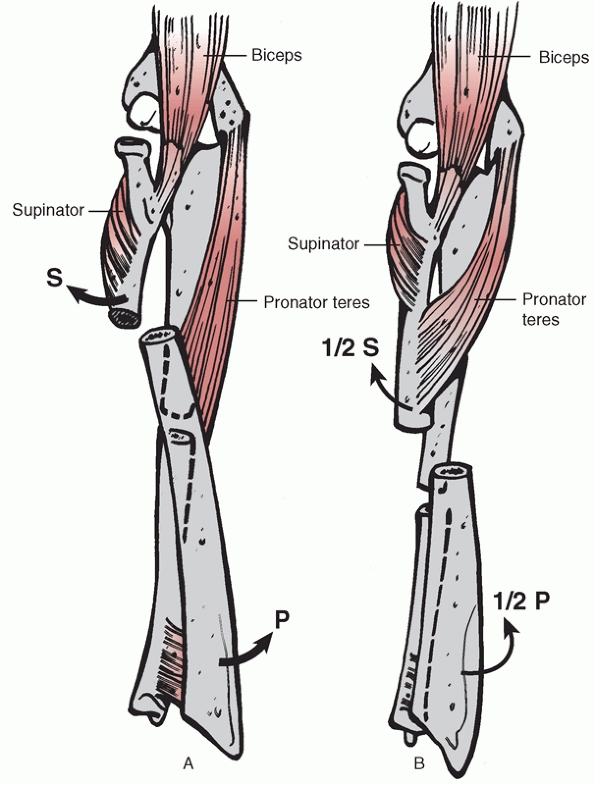
forces on different parts of the bones, and these forces can cause
displacement if the bones of the forearm are fractured. There are three
muscles which join the radius and the ulna: the supinator, pronator
teres, and pronator quadratus. When there is a fracture, these muscles
tend to approximate the radius and ulna and decrease the interosseous
space. In addition, the forearm muscles that take origin on the ulnar
aspect of the forearm and insert on the radial side of the wrist or
hand, such as the pronator teres, pronator quadratus, and the flexor
carpi radialis, tend to exert a pronating force.87
In a similar manner, muscles such as the abductor pollicis longus (APL)
and brevis and the extensor pollicis longus (EPL), which have their
origins on the ulna and interosseous membrane on the dorsal side and
are inserted on the radial side of the dorsum of the wrist, tend to
exert a supinating force.
 |
|
FIGURE 31-7 The method of Schemitsch et al.90 for quantifying the maximum radial bow and its location relative to the length of the entire radius.
|
brachii is a powerful supinator of the radius. In fractures of the
upper radius below the insertion of the supinator and above the
insertion of the pronator teres, two strong muscles (the biceps and the
supinator) exert an unopposed force that supinates the proximal radial
fragment (Fig 31-8A). In fractures of the
radius located distal to the pronator teres, the combined force of the
biceps and supinator is somewhat neutralized. In these fractures, the
proximal fragment of the radius is usually in a slightly supinated or
neutral position (Fig. 31-8B). In performing
reduction of forearm fractures, the location of the fracture of the
radius helps to determine the degree of supination of the distal
fragment needed to correct rotational alignment. Failure to correct
this will lead to rotational malunion and a resultant loss of rotation.
It is therefore crucial that an anatomic reduction should be achieved,
usually by open surgery.
 |
|
FIGURE 31-8 A. In fractures proximal to the pronator teres insertion onto the radius, biceps, and supinator supinate the proximal fragment. B.
When the fracture is distal to the pronator teres insertion, the proximal fragment is either slightly supinated or in the neutral position. |
location of the three nerves in the forearm: ulnar, median, and radial.
The ulnar nerve enters the forearm under the fascial band of the origin
of FCU and then runs between FCU and FDS incorporated into the
epimysium of FDP, lying lateral to the tendon of FCU distally. Its
superficial branch crosses the distal end of the ulna from volar to
dorsal and is at risk in the exposure of the distal third of the ulna.
The median nerve enters the forearm in the cubital fossa and passes
between the heads of pronator teres. It then runs between FDS and FDP.
The anterior interosseous nerve arises proximal to the elbow and is a
distinct branch running on the interosseous membrane between FPL and
FDP, ending in the pronator quadratus. The radial nerve has two
branches in the forearm: its superficial branch and the posterior
interosseous nerve. The superficial branch runs on the undersurface of
brachioradialis and crosses from volar to dorsal over the distal third
of the radius where it is vulnerable to injury. The posterior
interosseous nerve lies between the two heads of supinator at the
arcade of Frohse and is usually separated from the radial neck by the
deep head of supinator. The surgeon should be aware that in some cases
the nerve is directly applied to the neck of the radius where it is at
risk of iatrogenic injury.
lies on the supinator muscle. It then runs distally on the undersurface
of brachioradialis with the superficial radial nerve. At the wrist, it
lies on the radial side of FCR. The ulnar artery runs deep to pronator
teres and FDS proximally and then superficial to FDP between FDS and
FCU with the ulnar nerve.
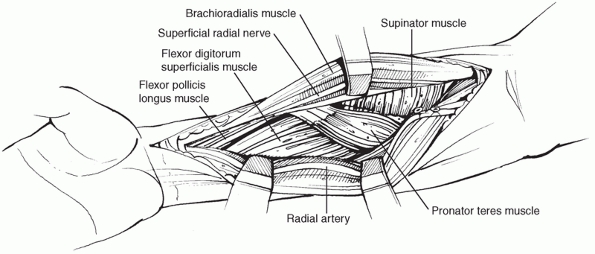
The patient is positioned supine on the operating table with the arm
abducted on a hand table. The arm is then prepped and draped to just
above the elbow. A tourniquet is used unless there has been a vascular
injury. The arm is held in supination. The medial edge of the mobile
wad forms the course of the planned incision.
care to preserve, if possible, the superficial veins. The fascia is
split at the edge of the brachioradialis muscle. The dissection is then
extended between the flexor-pronator mass on the ulnar side and the
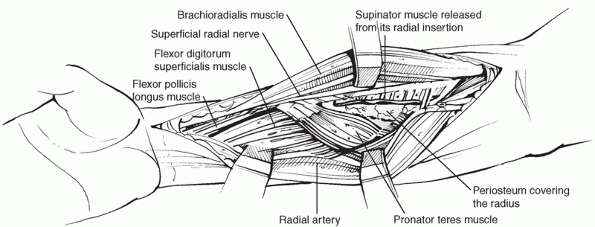
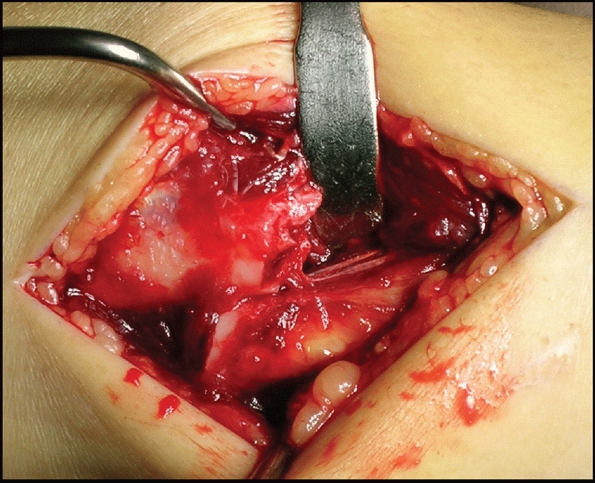
radial artery and the mobile wad on the radial side (Fig. 31-9).
Small branches of the radial artery should be carefully ligated to
facilitate retraction of the mobile wad. Care should be taken not to
damage the superficial radial nerve, which is situated underneath the
brachioradialis and is retracted laterally with the mobile wad. The
radial artery is exposed and retracted medially.
 |
|
FIGURE 31-9
After the interval between brachioradialis and FCR is exposed and the radial artery retracted medially, supinator, pronator teres, FPL, and FDS can be seen. |
supinator must be detached from the bone. The forearm should be
supinated to expose the insertion of the supinator and displace the
posterior interosseous nerve laterally and posteriorly. The muscle can
then be elevated subperiosteally (Fig. 31-10). It must always be handled with care to reduce any traction on the nerve.
forearm is pronated allowing release of the insertion of the pronator
teres from the radial aspect of the radius from proximal to distal.
FPL, pronator quadratus, and supinator can also be elevated if required.
tendon to the ulnar side exposes the transverse fibres of pronator
quadratus which should be elevated subperiosteally from the radial side
of the radius to expose the bone.
to the dorsal surface of the radius. This approach utilizes the
internervous plane between the mobile wad of Henry (brachioradialis,
ECRL, and ECRB), which is innervated by radial nerve and the extrinsic
hand extensor muscles on the back of the forearm.
with the arm abducted and the forearm pronated on a hand table. The
skin incision lies on a line from the lateral epicondyle of the
humerus, along the ulnar border of the mobile wad dorsally and
finishing at Lister’s tubercle. The underlying fascia is divided in the
same line. The approach then follows the interval between EDC and ECRB
from the midpart of the forearm distally to where APL and EPB cross the
field. These muscles may have to be released extraperiosteally from the
radius and mobilized proximally and distally. Proximally, the common
origin of ECRL
and
ECRB is split to reveal the supinator muscle. At this stage, it is
important to identify and protect the posterior interosseous nerve
which is most easily found as it exits supinator. If necessary, the
course of the nerve can be followed through supinator. The forearm is
then supinated to expose the anterior insertion of supinator which is
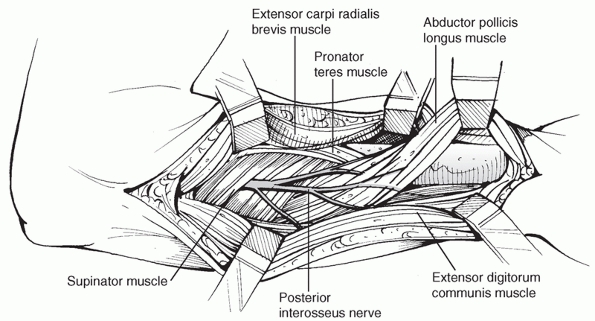
detached extraperiosteally to expose the proximal radius (Fig 31-11). Distally, the dorsum of the radius is exposed by developing the interval between ECRB and EPL.
 |
|
FIGURE 31-10
The insertion of supinator should be released with the patient’s arm held in supination. The posterior interosseous nerve should be left within the muscle. |
extensile. Proximal and distal exposure is more difficult than with
Henry’s approach. The posterior interosseous nerve must be protected in
the proximal third of both approaches.
length and there are no major neurovascular structures between the skin
and the bone, surgical exposure of the ulna is relatively
straightforward. Access is usually achieved with the arm abducted and
the elbow flexed. The ulna can also be exposed with the arm across the
chest or with the patient in the lateral decubitus position with the
arm on an arm rest. The latter is only suitable for isolated ulnar
fractures as it restricts access to the anterior forearm. The fascia is
incised in the same line as the skin incision, exposing the plane
between extensor and flexor carpi ulnaris. This plane is developed to
expose the underlying bone. Distally, the dorsal branch of the ulnar
nerve is encountered and should be protected as it passes dorsally over
ECU. Anteriorly, the ulnar nerve and artery run deep to FCU, which
should therefore be retracted with care.
 |
|
FIGURE 31-11
Development of the interval between ECRB and EPL reveals the radius distal to EPB. Proximally, the nerve can be mobilized where it exits the supinator if required. The posterior interosseous nerve should be identified and protected throughout the whole procedure. |
order to avoid any loss of function. Bony union is not the only goal of
treatment. The fracture must be reduced precisely, restoring the length
and axial and rotational alignment of the forearm. Anatomic reduction
of the proximal and DRUJs is essential to allow full recovery of
supination and pronation. If full and speedy functional recovery is to
be achieved, the fracture must be stabilized rigidly and range of
motion exercise should be started shortly after the surgery.
fractures usually results in a poor functional outcome because of the
importance
of
the anatomic relationship of the radius and ulna and the difficulty in
obtaining and maintaining an acceptable reduction. Treatment by closed
reduction and cast immobilization risks a poor functional outcome with
unsatisfactory results reported in up to 92% of cases,15,51,59
usually caused by malunion, nonunion, or synostosis. Most series of
conservatively treated displaced both bone fractures of the forearm
were published before 1960, indicating that closed reduction and cast
treatment for both bone fractures of the forearm has been effectively
abandoned with the advent of modern plating systems.
in cases of both bone fractures of the forearm. Thirteen of their 44
cases were both bone fractures treated with closed manipulation and
initial plaster cast followed by functional bracing applied an average
of 15 days after fracture. At final review, there was an average of 12
degrees loss of pronation and 19 degrees loss of supination. Union time
was an average of 15 weeks with a range from 9 to 33 weeks.
nightstick fracture, can be successfully treated in a cast. The
fracture is more stable probably due to the splinting effect of the
intact radius. Dymond22 showed that
if the fracture displacement is less than 50% of the width of the bone,
then the interosseous membrane is largely intact and the fracture can
be immobilized by a below-elbow cast. De Boeck et al.18
showed that in their 46 patients with isolated distal ulnar shaft
fractures, treatment with a below-elbow cast can yield satisfactory
results in 89% of patients. Gebuhr et al.36
reported a randomized trial and found that patients treated with a
prefabricated functional brace had significantly better wrist function
and were more satisfied than those treated with a long-arm cast. The
Cochrane Review attempted to assess the effects of various forms of
treatment for isolated fractures of the ulnar shaft, but no conclusion
could be drawn from the data obtained so far.42
reported a union rate of 99% and good to excellent function in 96% of
cases. In addition, when nonunion of the ulnar shaft occurs, its
prevalence has not been shown to be reduced by early fixation.10
In our opinion, if the fracture displacement is more significant or if
an early return of function is necessary, operative treatment with open
reduction and compression plating should be performed.
both radius and ulna is absolutely essential in order to restore full
functional recovery. The indications for surgery are summarized in Table 31-3.
fractures is best performed as early as possible after injury. In most
circumstances, there is no need to wait for the soft tissue swelling to
subside. Prolonged delay in fixation may increase the difficulty of the
reduction of the fracture as well as the surgical dissection leading to
devascularization of the bone fragments. In open fractures, an urgent
débridement followed by external or internal fixation should be done.
|
TABLE 31-3 Indications for Surgical Treatment of Forearm Fractures in Adults
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
condition with major visceral injuries or other significant fractures
such as pelvis or femoral shaft, then it is acceptable to delay the
surgery until the patient is stabilized. If there is delay in admission
to the hospital and the patient presents with compromised soft tissues
with fracture blisters or infected wounds near the intended incision
sites, it is also advisable to delay fixation until the soft tissue
conditions improve.
reported on 258 adults treated with compression plating for diaphyseal
fractures of the radius and ulna. There were 193 radial fractures and
137 ulnar fractures with rates of union of 98% for fractures of the
radius and 96% for fractures of the ulna. Autologous bone grafting was
used in 26% but did not increase the union rates compared to those
treated without grafting. An excellent or satisfactory result was
achieved in 86% of their patients. Despite the passage of several
decades, there has been no significant change in the reported outcomes
in more recent papers.17,41,46
They reported on a retrospective review of 132 fractures treated with
compression plating with a mean review period of 10 years. Uneventful
union within 6 months was reported in 96% of fractures. There was a
superficial infection in 1 patient but no deep infections.
bone and the risk of infection by minimizing the contact on bone, the
limited contact dynamic compression plate (LC-DCP) and the point
contact fixator (PC-Fix) were developed.25,78 This has been termed biologic fixation. We have reported our results of a randomized study of plate fixation using the PC-Fix and the LC-DCP.63
There were 92 patients with 125 forearm fractures. Five of 66 fractures
in the LC-DCP group and 4 of the 59 treated with the PC-Fix went on to
delayed union. There were no nonunions. One deep infection and one
refracture occurred in each group. Using the original criteria of
Anderson3 to determine the range of
motion, all patients in both PC-Fix and LC-DCP groups achieved a full
or nearly full range of motion. The study also showed that the pattern
of bone healing was affected by the quality of fracture reduction
rather than the type of implant used. When anatomic reduction was
achieved in either group, there was minimal callus formation and
primary bone healing was found. Despite the fact that the PC-Fix and
the LC-DCP use different concepts of fixation,48 both implants
were shown to be highly effective in the treatment of diaphyseal forearm fractures.
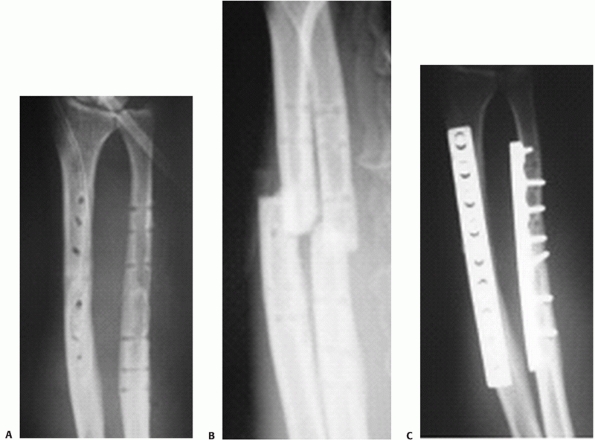
fractures treated with open reduction and internal fixation using the
locking compression plate (LCP) as the fixation method.64
This plate allows a combination of compression and a stable construct
conferred by the locking screws. There were two delayed unions and no
deep infections. All patients had full or nearly full range of motion.
Although the LCP (Fig. 31-12) represents the
latest development in plate development, its usage in fractures with
simple configuration and its superiority over conventional plating
systems (e.g., LC-DCP) has yet to be proven.
 |
|
FIGURE 31-12 Fracture of the forearm treated with a locking compression plate. A. The application of locking screw. Good alignment and uneventful healing was seen in the anteroposterior (B) and lateral (C) follow-up radiographs at 6 months.
|
The results were disappointing with a high rate of nonunion (20%) and a
poor final range of rotation. This paper was the stimulus for the
development of the Sage nail, a prebent, triangular intramedullary
nail. In the latter report, Sage87
described the rationale for and the design of his intramedullary
forearm nail with improved results. He reported a non- or delayed union
rate of 11%.
studied 18 patients with 32 diaphyseal forearm fractures treated with
the ForeSight (Smith & Nephew, Memphis, TN) forearm interlocking
nail which has a diameter of 4 to 5 mm (Fig. 31-13). Compared
with the normal arm, the mean loss of rotation of the forearm was 32
degrees. There was mild to moderate impairment demonstrated with the
Disabilities of the Arm, Shoulder, and Hand (DASH) score. The overall
infection rate was 12.5% but all were superficial. Weckbach et al.107
reported a series of 33 forearm fractures treated with intramedullary
ForeSight nails. They found the surgical technique demanding but still
satisfactory despite a nonunion rate of 8% and loss of rotation in 12%
of patients. Intramedullary nailing using multiple Kirschner-wires in
288 forearm fractures in 184 patients was recently reported from a
developing country.1 The authors
reported a delayed or nonunion rate of 12%, a deep infection rate of
2%, and cross union in 2% of forearms. Twenty-three percent of patients
had unsatisfactory results but the authors pointed out that the method
is cheap and required minimal expertise. They concluded that Kirschner
wiring remains acceptable for use in developing countries.
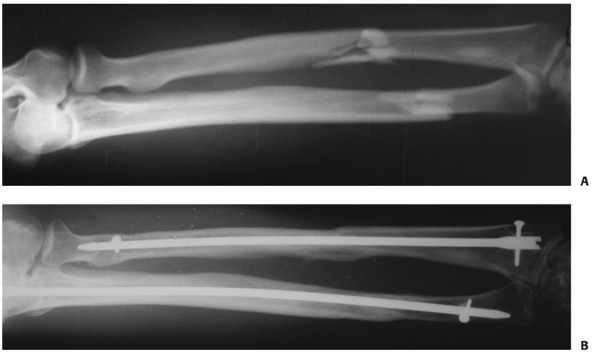 |
|
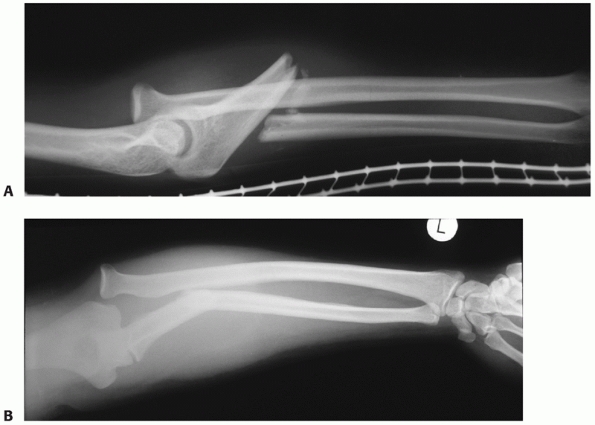
FIGURE 31-13 A. A 51-year-old man sustained a closed displaced diaphyseal forearm fracture (AO type B3) in a traffic accident. B.
Fractures were reduced and fixed with interlocking intramedullary nail (ForeSight nail) using a closed technique. Radiographs taken 12 months after the injury showed satisfactory union and alignment. (Courtesy of Dr. Gao Hong, MD, Department of Orthopaedics, The Sixth Affiliated People’s Hospital of Jiaotong University, Shanghai, PR of China.) |
reported a series of 15 patients with nonunion of diaphyseal forearm
fractures treated with intramedullary nailing and bone grafting.
Forty-seven percent of patients had unsatisfactory or poor results. The
authors concluded that interlocking intramedullary nailing of nonunions
of the diaphysis of the radius or ulna with an open reaming technique
should not be considered an adequate alternative to plate fixation of
these injuries.
available cannot fulfil the surgical goals of restoration of normal
bowing, adequate rotational stability, and early mobilization. We do
not advocate their use for displaced forearm fractures in adults where
plating is possible.
regarded as an alternative management of open forearm fractures when
there is significant soft tissue or bone loss.108 Schuind et al.91
advocated external fixation of both closed and open diaphyseal
fractures of the radius and ulna. However, the reported malunion rate
was 16.5% and the delayed or nonunion rate was 8.5%. Restoration of
forearm rotation was disappointing. External fixation of the forearm is
also associated with pin track infection.92
than internal fixation and hence the length of the bones and the normal
bowing are usually poorly restored. Its use should be temporary, and a
sequential exchange to internal fixation is mandatory once the soft
tissue condition improves or when soft tissue cover is achieved.44 External fixation of the forearm can also be employed in severely injured patients for damage control surgery (see Chapter 22) and can be useful in combat situations.43
placed in the ulna. The whole subcutaneous border of the ulna can be
palpated and offers a safe site for pin placement. Caution should be
exercised at the proximal and distal part of the ulna where the ulnar
nerve lies in close proximity to the bone.
In order to avoid inadvertent nerve and blood vessel damage, an open
pin insertion technique should be used. When a pin is placed in the
proximal radius, care must be taken not to damage the posterior
interosseous nerve. When a pin is placed in the radial aspect of the
shaft of the radius, care must also be taken not to damage the sensory
branch of the radial nerve. Simple unilateral fixators usually suffice
as an exchange to internal fixation and should be done once the soft
tissue condition has stabilized.
relocation of the dislocated radial head, together with reduction and
fixation of the ulna.81 Any residual angulation of the ulnar fracture predisposes to subsequent redislocation or subluxation of the radial head.89 In the adult patient, open reduction and internal fixation should be used.
should be made for open reduction and plate fixation of the ulna. After
fixation of the ulna, the reduction of the radial head must be
confirmed
with image intensification. A line along the proximal radial shaft and
the center of the radial head should pass through the center of the
capitellum in any position of the elbow, confirmed with two
radiographic views (see Fig. 31-2).68
after accurate reduction of the ulna, a small separate anterolateral
(Kocher) incision should be made and the radial head inspected for
interposition of the annular ligament. In young adults, the annular
ligament may remain intact with the radial head having slipped out due
to axial traction. In these cases, it may be necessary to divide the
annular ligament, reduce the radial head, and then repair the ligament.
fractures were poor. Watson-Jones stated in 1943 that, “no fracture
presents so many problems; no injury is beset with greater difficulty;
no treatment is characterised by more general failure.”106 He reported that 95% of Monteggia fractures had permanent disability.106 In 1974, Bruce et al.11
reported the results of the treatment of 21 adults with Monteggia
fractures, 5 by closed reduction and cast immobilization, and the
remaining 16 were treated with either an intramedullary rod or
compression plating. There were no excellent results and only 24% had
good results. There was a high rate of complications including
iatrogenic nerve palsies in 2 patients and nonunion in 8.
outcome of management of these injuries. In a series of 48 adult
patients with Monteggia injuries treated with open reduction and rigid
internal fixation,82 there were 83%
excellent or good results, though this was achieved after a number of
reoperations and reconstructive surgery. The majority of the poorer
results resulted from Bado type 2 injuries; all had a radial head
fracture and half of the cases had a coronoid fracture. More recently
Konrad and his coauthors60 reported
on the outcome of 47 adult patients who had sustained a Monteggia
fracture and were treated with open reduction and internal fixation.
There was a similar preponderance of women in the Bado type 2 group
although with a younger average age than in the series by Ring et al.84
Seventy-three percent had excellent or good results at an average
review period of 8.4 years. The authors correlated Bado type 2
fractures, Jupiter type 2a fractures, radial head fracture, coronoid
fracture, and complications requiring reoperation with a poorer
prognosis. Associated ulnohumeral instability has also been noted as a
poor prognostic factor.98
together with a precise reduction of the radial fracture which is
rigidly fixed. An anterior (Henry) approach is used to expose the
fracture, and a plate is applied to the volar aspect of the distal
radial shaft. Reduction of the DRUJ must then be confirmed with image
intensification in two planes and by passive rotation of the forearm.
If the joint is stable throughout the entire range of rotation and is
well aligned on the image intensifier views, there is no need for
additional postoperative immobilization and early range of motion
exercises should be started.
easily with a combination of clinical and radiologic examination.
However, a number of features should raise suspicion of instability.
These are listed in Table 31-4.
|
TABLE 31-4 Indications of Possible Distal Radioulnar Joint Instability7,12
|
||||||
|---|---|---|---|---|---|---|
|
instability on forearm rotation, the distal ulna can be transfixed to
the radius using two Kirschner wires with the forearm in supination.67,80 An above-elbow splint with the forearm in supination is then applied. The wires are removed at 6 weeks.
Frequently, there is an associated ulnar styloid fracture. If the DRUJ
is irreducible, an open reduction through a small separate incision
should be performed, any interposed tissue removed, and the soft tissue
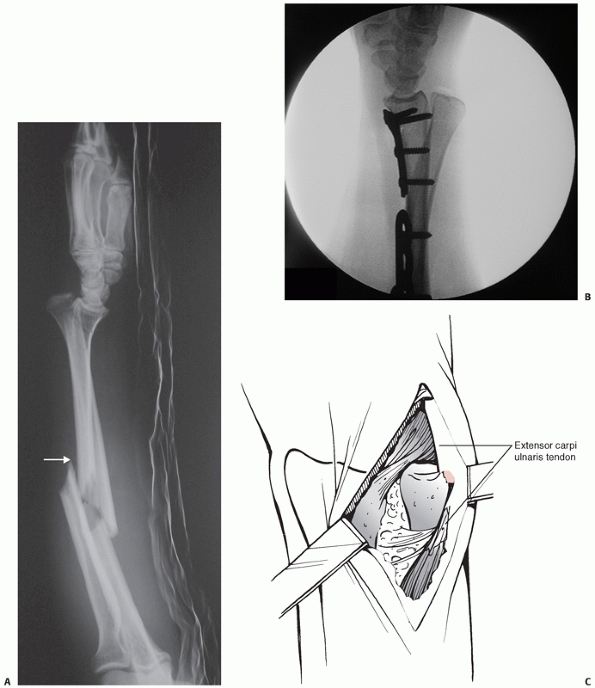
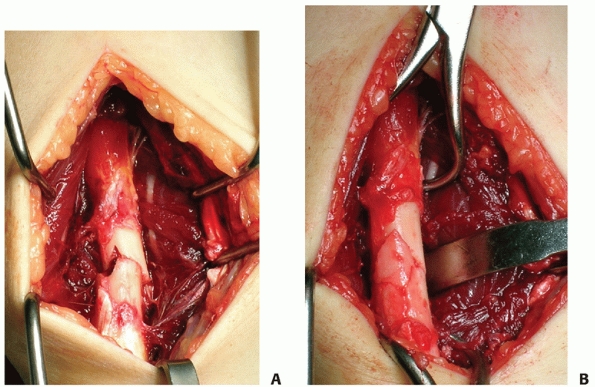
defect repaired with tight sutures (Fig. 31-14). If the ulnar styloid fracture is of sufficient size, it should be reduced and internally fixed.
fractures, but it is clear that anatomic reduction is mandatory. Any
residual shortening of the radial fracture predisposes to subsequent
problems with the DRUJ.100 In this
series of 19 patients with long-term follow-up, those patients with
radiographic evidence of anatomic fracture reduction had minimal
deficit and better functional results than patients with imperfect
reduction. Moore and his coauthors74
reported on 36 closed Galeazzi fractures treated using compression
plating. The average restoration of grip strength was 71%, and only one
patient failed to return to employment. Loss of grip strength was more
severe in seven patients with significant restriction of wrist and
forearm movement.
reported a complication rate of 39%, including nonunion, malunion,
infection, refracture after plate removal, and instability of the DRUJ.
Nerve injury was the most common with seven injuries to the radial
nerve and six to the dorsal branch. One to the dorsal interosseous
branch was attributed to retraction.
restoration of the length of the radius and stabilization of the DRUJ.
If the radial head is fractured with large fragments (type 1), open
reduction and internal fixation with small Herbert screws, mini-AO
screws, or miniplates should be performed. If the fracture fragments of
the radial head are comminuted and not amenable to internal fixation
(type 2), a radial head prosthesis should be inserted to maintain the
length of the radius.66a,101
All concomitant injuries, including radial shaft fracture and
ligamentous injuries around the elbow should be dealt with in order to
treat all components of this complex injury (Fig. 31-15).
 |
|
FIGURE 31-14 A.
A patient with a variant of Galeazzi injury with a segmental radius fracture and an ulnar shaft fracture. She complained of burning sensation along the distribution of the superficial branch of radial nerve. Intraoperatively, there was pressure on the nerve from a sharp piece of bone at the fracture (white arrow). B. The DRUJ was also irreducible on closed manipulation. C. A separate incision for open reduction was made. The ECU tendon was found trapped beneath the ulnar head. |
intraoperatively. If the joint is reduced and stable, external
immobilization in supination should be maintained for 3 weeks. If the
ulnar head is not stable after reduction, a radioulnar pin can be
inserted with the forearm in supination and maintained for 3 to 4 weeks.
accurate realignment of the radius and ulna is necessary and usually
requires radial head replacement. Distal ulnar procedures such as ulnar
shortening or a Sauve-Kapandji procedure are frequently required.
Recently, a technique of reconstruction of the central band of the
interosseous membrane was described by Chloros et al.16
by rerouting of the pronator teres tendon and using it as a graft.
Although all the components of the Essex-Lopresti injury are addressed,
the efficacy of this procedure has yet to be confirmed.
reported three excellent results in seven cases. All three were treated
within 1 week of injury. The remaining four had treatment delayed by 4
weeks or more.
 |
|
FIGURE 31-15 A. A young man fell from a horse and sustained a fracture of the radial shaft. The DRUJ was also disrupted. B. Intraoperative screening showed a dislocation of the radial head as well. C. Plate fixation of the radial shaft fracture, repair of annular ligament, and percutaneous ulnoradial pinning were performed. D. Follow-up at 1 year showing both normal elbow and wrist joint articulations. The patient had nearly full functional recovery.
|
important initial management of open fractures of the forearm is
thorough irrigation and débridement (see Chapter 10).
Following débridement, the method of stabilization of the fracture must
be considered. In earlier series, primary plate fixation was not
favored,3 fearing that it might lead
to increased risk of infection. More recently, however, authors have
recommended immediate internal fixation of such fractures. Moed et al.73
in a series of 50 patients with open forearm fractures including 11
Gustilo type 3 injuries, found a 4% incidence of deep infection and 12%
incidence of nonunion. The functional results were excellent or good in
85% of the series. Chapman14 reported only a 2% incidence of infection after primary plate fixation of open forearm fractures. Duncan et al.21
reported a series of 103 open forearm fractures treated with immediate
internal fixation within 24 hours. They recommended that immediate
plating can be done in grade I, II, and IIIA open forearm fractures.
Lenihan et al.62 reported a series
of seven forearm fractures from low-velocity gunshot wounds treated
with open reduction and internal fixation and found no cases of
infection. Jones55 reported 18
patients with grade III open forearm injuries treated with immediate
plate fixation in conjunction with aggressive soft tissue management,
including eight IIIB and three IIIC open fractures. He reported good or
excellent results in 12 patients and only one deep infection, which was
managed successfully with subsequent surgeries.
immediate internal fixation with plating following a thorough
débridement. If possible, the implant should be covered with muscles or
other soft tissues but the skin should be left open. Redébridement
should be done at 24 to 48 hour intervals until the wound is suitably
healthy to allow secondary closure or soft tissue cover.
loss, a bridging plate should be used taking care to restore the axial
and rotational alignment and the length of the radius. Bone grafting is
usually employed as a secondary procedure after healing of all soft
tissue wounds, usually at 8 to 10 weeks postoperatively.55
coverage or the wound is severely contaminated, a temporary external
fixator can be applied to stabilize the fracture followed by secondary
internal fixation when the soft tissues are stabilized.
It should provide the surgeon a full picture of the surgical procedure
and the possible problems that may be encountered during the surgery. A
number of factors should be considered before embarking on surgery.
These are listed in Table 31-5.
the surgeon studies the radiographs thoroughly and decides the type of
plate fixation to be used. In general, the OTA classification of
diaphyseal fractures can serve as a guide. All simple fractures (group
A) can be fixed with compression plating or lag screws with plating.
Almost all wedge fractures (group B) can be fixed with interfragmentary
lag screws with neutralization plating. Complex (group C) fractures can
be fixed with either compression plating or bridge plating. If the
fracture is bifocal, with each of the fractures being of a simple
configuration, then compression plating can be applied. In the presence
of increasing comminution with smaller fracture fragments that are not
amenable to lag screw fixation, bridge plating should be used.
|
TABLE 31-5 Checklist before Performing Plate Fixation of Forearm Fracture
|
||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
the type of fracture and associated soft tissue injury. Routinely, the
Henry approach is used for the radius, but the Thompson approach may be
required for specific reasons such as a dorsal soft tissue injury
requiring débridement. The authors prefer extraperiosteal dissection (Fig. 31-16).
If periosteal stripping is necessary to achieve a precise anatomic
reduction, it should be limited to 1 to 2 mm at the fracture ends.
Stripping of the periosteum along the length of the plate is
contraindicated since this may lead to delay in healing and increased
risk of infection. In particular, modern locking plates are applied
with minimal contact between the plate and the bone allowing
preservation of the periosteum.
surrounding soft tissues, indirect reduction techniques involving
continuous longitudinal traction applied through an external fixation
device or directly through an applied plate using a plate-tensioning
device have been advocated.
reduction methods to achieve anatomic reduction. With the size of the
forearm bones, most fracture fragments can be held and manipulated with
ease using small pointed reduction forceps (Fig. 31-17).
The reduction is performed under longitudinal traction and direct
vision. Depending on the fracture configuration, the reduction may
require traction or a rotational maneuver. The relatively sharp edge of
the interosseous border of the bones should also be matched on both
sides of the fracture and used as a landmark for precise reduction of
rotational alignment. In the case of a transverse fracture, lag screw
application is not necessary and interfragmentary compression is
achieved by the dynamic compression screw mechanism.
 |
|
FIGURE 31-16
Preservation of soft tissue surrounding the fracture, exposing bare bone only if necessary. After the fracture is exposed, a Hohmann retractor is put under the fracture to retract the surrounding soft tissues and to support the fracture |
achieved, a third pair of pointed reduction forceps is applied to close
the fracture gap completely and hold the fracture temporarily to allow
lag screw fixation. In our experience, the use of 2.7-mm screws is very
helpful in fixing smaller bone fragments that cannot accommodate a
3.5-mm screw. A neutralization plate is then applied to provide
stability to the whole bone-implant construct.
 |
|
FIGURE 31-17 A. Pointed reduction clips are applied to the main fracture fragments. B. Longitudinal traction was applied. C. The fracture is reduced under direct vision.
|
fragments are too small for lag screw fixation, excessive soft tissue
dissection in order to reduce each fracture fragment anatomically
should be avoided. If indirect reduction is used, the fracture site is
not exposed and remains covered by the surrounding soft tissues with
maximal preservation of the biology surrounding the bone fragments. The
aim of the reduction is to restore the length and curvature of the
forearm bones. It is therefore essential to confirm the physiologic
bowing of the forearm bones and the normal articulation of the proximal
and distal radioulnar joints on image intensification during surgery.
have set the standard of plate fixation of forearm fractures. The
length of the plate is intimately related to the extent of the
fracture. It is generally accepted that three cortical screws engaging
in at least six to seven cortices in each main fragment are recommended
to secure the fixation.76 The number
may be decreased due to anatomic reasons (metaphyseal/epiphyseal
regions) or increased because of bone quality (osteoporosis).
including dynamic compression plate, limited contact dynamic
compression plate, PC-Fix, and LCP. In general, the authors prefer to
use the locking compression plate, which offers the flexibility of
being used as a compression plate, as a bridging fixator, or as a
system combining both techniques. The LCP also offers better fixation
in osteoporotic
bone
and the cancellous bone of metaphyseal region. Each screw hole, or
“combination hole,” can allow the insertion of a conventional screw or
a locking head screw as the hole has features of both a smooth sliding
compression hole and a threaded locking hole.104
 |
|
FIGURE 31-18 A. In fracture with a small wedge fragment, the two main fracture fragments can be reduced first. B.
The small bony piece is placed in the cortical defect. Interfragmentary compression is then applied, and no bone graft is needed. |
suggested that from a mechanical perspective, at least two monocortical
screws on each main fragment are required, but in clinical practice, it
is advisable to insert more screws. We feel that if the locking screws
are inserted properly and engaging in strong cortical bone, then
fixation in only four cortices is necessary in each fracture fragment.
This can be in form of two bicortical screws or one bicortical with two
monocortical screws. If the fracture fixation is in osteoporotic bone
or in the metaphysis, then only bicortical screws should be inserted as
monocortical screws can easily pull out from the thin cortex.
undue tension at the wound edges that might lead to necrosis and wound
breakdown. In general, there is no need to suture the fascial layer, as
this will increase the compartment pressure of the forearm. Instead,
the skin wound should be closed and the bone and metal implants should
be covered by soft tissues. In cases of severe swelling which makes
primary closure inappropriate or impossible, it is acceptable to leave
the wound open over the radius, which is usually covered by the forearm
muscles. Secondary skin closure or split skin grafting can be done once
the swelling reduces.
stability is achieved, it is not necessary to apply any splints or
casts postoperatively. The patient is instructed to keep the arm
elevated and early active movement of the wrist and elbow can be
started as early as the first postoperative day. Normal daily
activities can be resumed after 2 to 3 weeks, while the patient should
refrain from any manual work or sports activities involving the injured
arm until bony union has occurred, which may take 12 to 16 weeks.
comminution first, so as to achieve a more anatomic initial reduction
and to have a better chance of restoring the normal length and
rotation. If both the radius and ulna have the same degree of
comminution, then the radius is usually fixed first, as it is easier to
operate first on the volar aspect of the supinated forearm. Afterward,
the elbow can be flexed to allow access to the ulna.
recommended bone grafting in the presence of comminution more than one
third of the circumference of the bone. However, Ring et al.83 reported that the use of bone graft was not associated with a higher union rate.
The only exception is the case of a comminuted fracture with several
small devascularized cortical fragments that are not amenable to lag
screw fixation and preclude a good interfragmentary compression between
the two main fragments. In that case, one should restore the normal
length and curvature of the bone with bridge plate fixation. The bone
defect is then filled with cancellous bone graft obtained from the
ipsilateral olecranon or the iliac crest. It is of utmost importance
that such bone grafts should not be placed in the interosseous space so
as to prevent radioulnar synostosis.
the upper limbs, it is a potentially serious complication. Risk factors
include crush injury and other high-energy trauma that cause the
forearm fracture.10a Moed and Fakouri72
reported a 10% incidence of compartment syndrome in 131 cases of
forearm gunshot wounds with or without fractures. Fracture location was
the only significant risk factor and the majority of compartment
syndromes they reported occurred in gunshot
fractures
of the proximal third of the forearm. Young men with associated
fracture of the distal end of the radius have also been found to be at
risk of compartment syndrome.70
examination are of paramount importance in making a correct diagnosis
of compartment syndrome. Excruciating pain that is disproportional to
the clinical picture, severe pain on passive stretching of the fingers,
and reduced hand sensibility or paresthesiae are cardinal features of
compartment syndrome.37
Intracompartmental pressure should be measured and, where differential
pressures are below 30mm Hg for any length of time, forearm fasciotomy
is indicated (see Chapter 27).
When indicated, an additional straight dorsal incision may be used. The
postfasciotomy compartment pressure can be determined intraoperatively
to assess the adequacy of the surgical release.
the incision should continue in the midline distally and cross the
wrist crease to release the carpal tunnel. If the compartment syndrome
progresses to include symptoms or signs of ulnar nerve involvement, it
should also be released.
and ulnar arteries, which form the superficial and the deep palmar
arches. The collateral circulation is usually sufficient to maintain
adequate perfusion of the hand. As a result, revascularization is
usually unnecessary in the face of a single artery injury. Vascular
repair of the blood vessels of the forearm would be indicated in
severely crushed forearm or traumatic amputation and should be done
after the fracture is stabilized by plate fixation or an external
fixator (see Chapter 12).
However, the posterior interosseous nerve is by far the most common
nerve injury, especially in association with a Monteggia fracture
dislocation. In general, most of these injuries are neurapraxias, and
nerve exploration is only indicated if there are no signs of recovery
at 2 to 4 months.54,77
However, where there is a deteriorating neurologic status, an arterial
injury, an open wound, or an irreducible fracture, earlier exploration
is indicated. This does not usually require added surgery as most cases
are treated surgically in any case.
operative treatment of the forearm fractures. The posterior
interosseous nerve is particularly at risk of injury when the proximal
radial shaft is exposed. In order to prevent its damage during a Henry
approach, the bone must be exposed subperiosteally, with the forearm in
maximal supination. Careful retraction of the muscle after the nerve is
identified is advisable when the proximal radius is exposed surgically
via a dorsal (Thompson) approach.
injured in forearm fractures as a result of impingement by a bone
fragment (see Fig. 31-14A) or damage during operative fixation or plate removal.61
When the anterior or Henry approach is used to expose the radius, the
nerve is usually retracted laterally along with the brachioradialis
muscle. Care must be taken to use only blunt and broad retractors for
this muscle and to avoid prolonged impingement on the nerve by a
retractor.
plating, perioperative antibiotic prophylaxis, good surgical
techniques, and modern implants that preserve more blood supply to the
bone have resulted in a low incidence of infection after plate fixation
of forearm fractures.14,63,64
Immediate plate fixation of open forearm fractures carries an
acceptable risk of infection even in open fractures and is the method
of choice along with adequate and appropriate soft tissue management.15,55,73
If infection does occur, adequate débridement with copious irrigation
is recommended, followed by an appropriate antibiotic treatment, which
should be based on the results of bacteriologic studies (see Chapter 24).
Implant removal is not advised in the presence of infection provided
the bone fragments are vascularized and the fixation is stable.
Maintenance of stable internal fixation aids wound care, maintains
alignment, facilitates bone union, and allows early function.
inadequate stability or compromise of the vascularity of the bone.
Intramedullary nailing of forearm fractures offers less stability than
plate fixation and hence carries a higher chance of nonunion.93,99
Rigidity of the internal fixation device has been reported to have a
significant effect on the healing process when rigid and nonrigid
devices were compared.65 However,
some flexibility has also been shown to be beneficial. In a
biomechanical study of the locked internal fixator, Stoffel et al.97
examined a simple fracture with a small interfragmentary gap of less
than 2 mm. They suggested that the placement of screws in one or even
two plate holes near the fracture gap should be omitted to retain some
physiologic flexibility of the construct, so as to stimulate bone
healing.
between compression plating and bridge plating, diaphyseal nonunions of
forearm fractures are unusual. The current reported incidence of
nonunion in forearm fractures treated with plate fixation is less than
2%.14,63,64
With modern techniques, nonunions can often be ascribed to technical
errors. The common pitfalls include the use of inappropriate implants
(e.g., one third tubular plates) or plates of inadequate length (Fig. 31-19).
Failure to achieve precise reduction of simple or wedge fracture
configurations will also lead to compromise in the rigidity of the
fixation and a higher risk of a poor result.61a Open fracture with significant bone loss is also a common cause of delay in union.
reported successful treatment with autogenous cancellous bone grafting
in bone defects of 1 to 6 cm. They reported a high rate of union and
improved upper limb function. The prerequisites are stable plate
fixation and a healthy and vascular soft tissue envelope.
the integral parts of forearm movement, especially supination and
pronation. If the surgeon fails to restore the normal anatomic radial
and ulnar bows, bony union will take place in the presence of narrowing
of the interosseous space and subsequent contracture of the
interosseous membrane. Such malunion will result in significant loss of
function, especially in forearm rotation.
usage in pediatric fractures. This is due to failure to restore and
maintain the normal bowing of bone and rotational alignment. With the
plate fixation that requires a precise reduction, malunion as a
complication is rarely reported.
 |
|
FIGURE 31-19 Poor fixation technique, as in this example of intramedullary pinning, can cause nonunion.
|
reported 55 patients with malunion and found that good functional
results were associated with restoration of the normal amount and
location of the radial bow. Trousdale and Linscheid102
reported a series of 27 cases of malunion of forearm fractures with
limitation of motion treated with corrective osteotomy. They suggested
that early correction may have a greater improvement in motion than
late correction after 1 year of original injury.
 |
|
FIGURE 31-20 Radiographs of a 26-year-old man showing (A) bone union after implant removal at 12 months. Both the radius and ulna refractured after a fall (B) and were fixed with a plate that was longer than the original plate (C).
|
Before embarking on this surgery, union should be confirmed as an
increased risk of refractures has been found in cases in which there
are factors which might predispose to nonunion. These include
high-energy, crush, or open injuries, failure of reduction or
compression, and persistent radiolucency at the fracture site.19
or through an old screw track. The use of excessively large screws and
early removal of plates before 1 year are both associated with higher
risk of refracture.14,85,86 The use of monocortical screws does not reduce the risk of refracture. Leung and Chow63
compared the use of PC-Fix using monocortical screws versus LC-DCP
using bicortical screws and reported the same risk of refracture of 4%.
All refractures occurred through the old screw track, even when the
original screw engaged in one cortex only. Equally, the advent of new
implants such as the LCP does not decrease the risk of refracture.
Leung and Chow63 also reported two cases of refracture (9%) after removal of forearm LCP, both at the original fracture site (Fig. 31-20). Both original fractures
were of simple transverse configuration and demonstrated primary bone
union with no callus. Removal was undertaken at 11 and 12 months after
the initial fixation, which were earlier than the average 16 months for
the series. The authors postulated that the combination of
interfragmentary compression with a superimposed locking internal
fixator can produce a very stable construct, though it may not be
conducive to sound fracture healing, including callus formation.
we believe that elective plate removal is contraindicated in the
asymptomatic patient. Plate removal should only be considered if there
is pain or another symptom resulting from hardware irritation to the
soft tissues. It should be delayed for at least 18 months after the
initial fixation.
operative treatment of forearm fractures. Although radioulnar
synostosis is more common with fractures of the both the radius and
ulna, especially if they are at the same level or in the proximal third
of the forearm, it can still occur when only one bone is fractured and
the other bone is intact. The incidence of synostosis after plate
fixation reported in the literature ranges from 2% to 9%.5,96,103 Bauer et al.5
reported an increased risk using a single incision to approach both
bones and advised the use of two separate incisions. Botting8
reported a series of 10 cases of radioulnar synostosis in which seven
were associated with a delay in fixation. Vince and Miller103
suggested that severe local trauma and delayed open reduction may
predispose to synostosis. Bone fragments left in the interosseous space
and bone screws that breached the opposite part of the cortex extending
into the interosseous space were common findings in their reported
cases. A further risk factor is forearm fracture in patients with head
injuries.33
 |
|
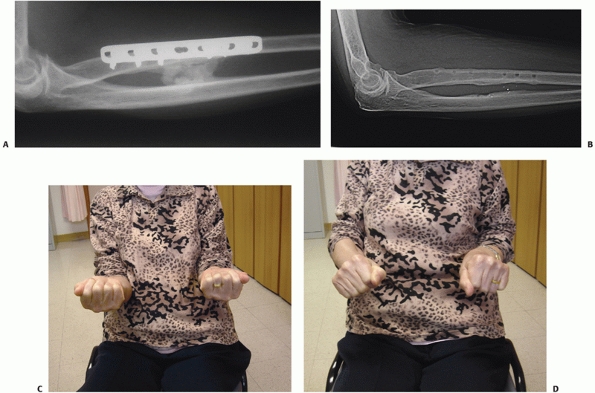
FIGURE 31-21 A. A 61-year-old lady developed radioulnar synostosis after plate fixation of a radial shaft fracture. B. Excision was done at 9 months after the initial fixation. C,D. The patient had good range of motion afterward.
|
During the initial fixation of fractures of both the radius and ulna, a
separate incision should be used for each bone. Surgical dissection
near the interosseous membrane should be limited and narrowing of the
interosseous space must be avoided. In cases of proximal forearm
fracture, the two bones lie in close vicinity and the surgeon must take
care not to penetrate the other bone with a drill during plate
application. When the use of bone graft is necessary in comminuted
fractures, it should not be placed near the interosseous space.
with complete loss of forearm rotation, surgical excision of the
synostosis is recommended (Fig. 31-21). A computed tomography scan is
very helpful to delineate the extent and the location of the bone block, especially when it occurs in the proximal forearm.
and hemostasis ensured. Interposition of free fat tissue in the
interosseous space helps to prevent recurrence.57
The patient should be given adequate analgesics in the postoperative
period and early range-of-motion exercises should be encouraged. As in
heterotopic ossification occurring in other parts of the body,
indomethacin should be prescribed to decrease chance of recurrence. We
do not adopt the use of postoperative irradiation as a prophylaxis.
fixation has been the standard in management of forearm fractures with
very satisfactory results in terms of alignment and union. Few studies
have attempted to assess patient orientated outcomes. Goldfarb et al.39
analyzed the DASH and the musculoskeletal functional assessment (MFA)
after fractures of both bones of forearm in 23 patients. The mean DASH
score was 12 and the mean MFA score was 19. Significant reduction in
pronation (mean difference 10 degrees) and grip strength (mean
difference 6 Kg) were found compared to the contralateral forearm.
Decreased range of rotation and wrist movement correlated with poorer
subjective scores. Droll et al.20
investigated the DASH and SF-36 as patient-based functional outcomes
and measured strength following plate fixation of fractures of both
bones of forearm in a cohort of 30 patients. They reported an average
loss of 30% strength, although it should be noted that there was a high
proportion of high-energy or open injuries. The main determinant of the
final DASH score was pain, and the authors suggested that perceived
disability was determined by pain more than by objective physical
impairment.
our surgical treatment, then a large part of this goal has been
achieved by the modern method of plate fixation of forearm fractures.
The introduction of locking implants will add the further benefit of
stronger fixation in osteoporotic bones. The technique of minimally
invasive plate osteosynthesis has gained much popularity recently, and
we feel that the ulna fractures may be suitable for this technique.
However, with its many muscles attachment and a deeper position in the
forearm, the radius is not ideal for this technique.
forearm restores nearly normal anatomy and motion, there is still room
for improvement in terms of patient-based outcome. We suggest that
measuring bony union and motion after treatment of forearm fractures is
not sufficient. All future studies on this fracture should include a
patient-assessed outcome measurement to evaluate the effectiveness of
the treatment methods.
A, Dossim A, Assiobo A, et al. Intramedullary fixation using multiple
Kirschner wires for forearm fractures: a developing country
perspective. J Orthop Surg 2007;15: 319-322.
LD, Sisk D, Tooms RE, et al. Compression-plate fixation in acute
diaphyseal fractures of the radius and ulna. J Bone Joint Surg Am
1975;57(3):287.
G, Arand M, Mutschler W. Posttraumatic radioulnar synostosis after
forearm fracture osteosynthesis. Arch Orthop Trauma Surg
1991;110(3):142-145.
GW, Cohen MS, Resnick D. Fracture-dislocation of the elbow with
inferior radioulnar dislocation: a variant of the Essex-Lopresti
injury. Skeletal Radiol 1992;21(5):315-317.
PH, Corea JR, Blakemore ME. Nonunion of the isolated fracture of the
ulnar shaft in adults. Injury 1981;12(5):371-375.
JD, Lichtman DM, Alexander AH. Complex dislocations of the distal
radioulnar joint. Clin Orthop Relat Res 1992;275:90-103.
MW, Gordon JE, Zissimos AG. Compression-plate fixation of acute
fractures of the diaphyses of the radius and ulna. J Bone Joint Surg Am
1989;71(2):159-169.
GD, Wiesler ER, Stabile KJ, et al. Reconstruction of Essex-Lopresti
injury of the forearm: technical note. J Hand Surg Am
2008;33(1):124-130.
JR, Brakenbury PH, Blakemore ME. The treatment of isolated fractures of
the ulnar shaft in adults. Injury 1981;12(5):365-370.
Boeck H, Haentjens P, Handelberg F, et al. Treatment of isolated distal
ulnar shaft fractures with below-elbow plaster cast. A prospective
study. Arch Orthop Trauma Surg 1996;115(6):316-320.
PE, Lindsay RW, Ruwe PA. Refracture of bones of the forearm after the
removal of compression plate. J Bone Joint Surg Am 1988;70(9):1372-1376.
KP, Perna P, Potter J, et al. Outcomes following plate fixation of
fractures of both bones of the forearm in adults. J Bone Joint Surg Am
2007;89(12):2619-2624.
R, Geissler W, Freeland AE, et al. Immediate internal fixation of open
fractures of the diaphysis of the forearm. J Orthop Trauma
1992;6(1):25-31.
GS Jr, Jupiter JB. Radial head fractures with acute distal radioulnar
dislocation. Essex-Lopresti revisited. Clin Orthop Relat Res
1988;234:61-69.
H, Hauke C, Arens S, et al. PC-Fix and local infection
resistance—influence of implant design on postoperative infection
development, clinical, and experimental results. Injury 2001;32(Suppl
2):B38-B43.
WD, Keene JS. Anterior interosseous nerve palsy associated with a
Monteggia fracture. A case report. Clin Orthop Relat Res
1983;174:133-137.
P. Fractures of the radial head with distal radioulnar dislocation;
report of two cases. J Bone Joint Surg Br 1951;33B(2):244-247.
JM, Amadio PC, Morrey BF. Posttraumatic proximal radioulnar synostosis.
Results of surgical treatment. J Bone Joint Surg Am
1989;71(8):1208-1213.
JM, Jacobson J, van Holsbeeck M. Ultrasound diagnosis and surgical
pathology of the torn interosseous membrane in forearm
fractures/dislocations. J Hand Surg Am 1999;24:257-266.
R. Ueber ein besonderes syndrom bei verletzungen im Bereich der
unterarmknocken. Arch. Orthop Unfallchir 1934;35:557-562.
H, Luo CF, Zhang CQ, et al. Internal fixation of diaphyseal fractures
of the forearm by interlocking intramedullary nail: short-term results
in eighteen patients. J Orthop Trauma 2005;19(6):384-391.
M, Kumar S. Entrapment and transection of the median nerve associated
with minimally displaced fractures of the forearm: case report and
review of the literature. Arch Orthop Trauma Surg 2001;121(9):544-545.
T, Koebke J, Pennig D, et al. The anatomical base of unilateral
external fixation in the upper limb. Injury 2000;31(Suppl 1):11-20.
P, Holmich P, Orsnes T, et al. Isolated ulnar shaft fractures.
Comparison of treatment by a functional brace and long-arm cast. J Bone
Joint Surg Br 1992;74(5):757-759.
RH, Garfin SR, Hergenroeder PT, et al. Compartment syndromes of the
forearm: diagnosis and treatment. Clin Orthop Relat Res
1981;161:252-261.
RH, Zakaib GS, Mubarak SJ, et al. Decompression of forearm compartment
syndromes. Clin Orthop Relat Res 1978;134:225-229.
CA, Ricci WM, Tull F, et al. Functional outcome after fracture of both
bones of the forearm. J Bone Joint Surg Br 2005;87(3):374-379.
N, Hauke C, Schutz M, et al. Treatment of diaphyseal fractures of the
forearm using the Point Contact Fixator (PC-Fix): results of 387
fractures of a prospective multicentric study. Injury 2001;32(Suppl
2):B51-B62.
HH, Pearce PK. Interventions for isolated diaphyseal fractures of the
ulna in adults. Cochrane Database Syst Rev 2004;2:CD000523.
B, Jovanovic S, Wetheimer B, et al. External fixation as a primary and
definitive treatment of open limb fractures. Injury 1995;26:245-248.
R, Pisan M, Lambert S, et al. Plate osteosynthesis of diaphyseal
fractures of the radius and ulna. Injury 1996;27:545-548.
HP, Wildburger R, Szyszkowitz R. Observations concerning different
patterns of bone healing using the Point Contact Fixator (PC-Fix) as a
new technique for fracture fixation. Injury 2001;32(Suppl 2):B15-B25.
G, Cong-Feng L, Hui-Peng S, et al. Treatment of diaphyseal forearm
nonunions with interlocking intramedullary nails. Clin Orthop Relat Res
2006;450:186-192.
RN, An KN, Sowa DT, et al. An anatomic and mechanical study of the
interosseous membrane of the forearm: pathomechanics of proximal
migration of the radius. J Hand Surg Am 1989;14(2 Pt 1):256-261.
Y, Horiuchi Y, Takahashi M, et al. Extensor tendon involvement in
Smith’s and Galeazzi’s fractures. J Hand Surg Am 1987;12:535-540.
JB, Ring D. Operative treatment of post-traumatic proximal radioulnar
synostosis. J Bone Joint Surg Am 1998;80(2):248-257.
JS, Kattapuram SV, Becker S, et al. Galeazzi injury with an associated
fracture of the radial head. Clin Orthop Relat Res 1988;234:70-71.
MR, Brien WW, Gellman H, et al. Fractures of the forearm resulting from
low-velocity gunshot wounds. J Orthop Trauma 1992:6(1):32-35.
F, Chow SP. A prospective, randomized trial comparing the limited
contact dynamic compression plate with the point contact fixator for
forearm fractures. J Bone Joint Surg Am 2003;85-A(12):2343-2348.
F, Chow SP. Locking compression plate in the treatment of forearm
fractures: a prospective study. J Orthop Surg (Hong Kong)
2006;14(3):291-294.
G, Ioannidis TH, Hartofylakidis-Garofalidis G. The influence of timing
and rigidity of internal fixation on bony union of fractures of the
forearm. Injury 1981;15:53-56.
I, Fitzgerald B, Miller JH. Silastic replacement of the head of the
radius in trauma. J Bone Joint Surg Br 1979;61-B(4):494-497.
BR, Kellam JF, Foster RJ, et al. Immediate internal fixation of open
fractures of the diaphysis of the forearm. J Bone Joint Surg
1986;68:1008-1017.
TM, Klein JP, Patzakis MJ, et al. Results of compression-plating of
closed Galeazzi fractures. J Bone Joint Surg Am 1985;67(7):1015-1021.
SM. The concept of biological plating using the limited contact-dynamic
compression plate (LC-DCP). Scientific background, design and
application. Injury 1991;22(Suppl 1):1-41.
CF, Chen AL, Wolinsky PR, et al. Posterior dislocation of the elbow
with concomitant fractures of the proximal ulnar diaphysis and radial
head: a complex variant of the posterior Monteggia lesion. J Orthop
Trauma 2003;17:530-533.
D, Allende C, Jafarnia K, et al. Ununited diaphyseal forearm fractures
with segmental defects: plate fixation and autogenous cancellous
bone-grafting. J Bone Joint Surg Am 2004;86-A(11):2440-2445.
D, Rhim R, Carpenter C, et al. Comminuted diaphyseal fractures of the
radius and ulna: does bone grafting affect nonunion rate? J Trauma
2005;59(2):438-441.
D, Rhim R, Carpenter C, et al. Isolated radial shaft fractures are more
common than Galeazzi fractures. J Hand Surg Am 2006;31(1):17-21.
JW, Shearer JR. Refracture after the removal of plates from the
forearm—an avoidable complication. J Bone Joint Surg Br 1991;73:415-417.
FP. Medullary fixation of fractures of the forearm. A study of the
medullary canal of the radius and a report of 50 fractures of the
radius treated with a prebent triangular nail. J Bone Joint Surg Am
1959;41-A:1489-1516.
A, Cooper JS, Sinclair WF. Forearm fractures. Early functional
bracing—a preliminary report. J Bone Joint Surg Am 1975;57(3):297-304.
A, Latta LL, Zych G, et al. Isolated ulnar shaft fractures treated with
functional braces. J Orthop Trauma 1998;12:420-423.
EH, Richards RR. The effect of malunion on functional outcome after
plate fixation of fractures of both bones of the forearm in adults. J
Bone Joint Surg Am 1992;74(7):1068-1078.
F, Andrianne Y, Burny F. Treatment of forearm fractures by Hoffman
external fixation. A study of 93 patients. Clin Orthop Relat Res
1991;266:197-204.
M, Freundlich BD, Teicher J. Posterior interosseous nerve palsy as a
complication of Monteggia fractures in children. Clin Orthop Relat Res
1968;58:141-145.
K, Dieter U, Stachowiak G, et al. Biomechanical testing of the LCP—how
can stability in locked internal fixators be controlled? Injury
2003;34(Suppl 2):B11-B19.
EJ, Tejwani NC, Preston CF, et al. The posterior Monteggia lesion with
associated ulnohumeral instability. J Bone Joint Surg Br 2006;88:84-89.
J, Gerber C. Distal radioulnar joint function after Galeazzi
fracture-dislocations treated by open reduction and internal plate
fixation. Clin. Orthop Relat Res 1993;293:240-245.
AB, Jaeger SH, La Rochelle D. Comminuted fractures of the radial head.
The role of silicone-implant replacement arthroplasty. J Bone Joint
Surg Am 1981;63(7):1039-1049.
BM, Pess GM, Kircher MT, et al. Ulnar nerve laceration in a closed both
bone forearm fracture. J Orthop Trauma 1996;10(2):131-134.
JJ Jr, Hanson GW, Bennett JB, et al. External fixation use in the
management of massive upper extremity trauma. Clin Orthop Relat Res
1982;164:172-176.
K, Tchang SP. Traumatic radioulnar synostosis treated by excision and a
free fat transplant. A report of two cases. J Bone Joint Surg Br
1983;65(4):433-435.
