Olecranon
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > III – Upper Extremity Fractures and Dislocations > 19 – Olecranon
19
Olecranon
EPIDEMIOLOGY
-
Bimodal distribution is seen, with
younger individuals as a result of high-energy trauma and older
individuals as a result of a simple fall.
ANATOMY
-
The coronoid process delineates the
distal border of the greater sigmoid (semilunar) notch of the ulna,
which articulates with the trochlea. This articulation allows motion
only about the flexion-extension axis, thus providing intrinsic
stability to the elbow joint. -
The articular cartilage surface is interrupted by a transverse ridge known as the “bare area.”
-
Posteriorly, the triceps tendon envelops
the articular capsule before it inserts onto the olecranon. A fracture
of the olecranon with displacement represents a functional disruption
of the triceps mechanism, resulting in loss of active extension of the
elbow. -
The ossification center for the olecranon
appears at 10 years and is fused by about age 16. There can be
persistent epiphyseal plates in adults; these are usually bilateral and
demonstrate familial inheritance. -
The subcutaneous position of the olecranon makes it vulnerable to direct trauma.
MECHANISM OF INJURY
Two common mechanisms are seen, each resulting in a predictable fracture pattern:
-
Direct: A fall on the point of the elbow or direct trauma to the olecranon typically results in a comminuted olecranon fracture.
-
Indirect: A fall onto the outstretched
upper extremity accompanied by a strong, sudden contraction of the
triceps typically results in a transverse or oblique fracture. -
A combination of these may produce
displaced, comminuted fractures, or, in cases of extreme violence,
fracture-dislocation with anterior displacement of the distal ulnar
fragment and radial head.
CLINICAL EVALUATION
-
Patients typically present with the upper
extremity supported by the contralateral hand with the elbow in
relative flexion. Abrasions over the olecranon or hand can be
indicative of the mechanism of injury. -
Physical examination may demonstrate a
palpable defect at the fracture site. An inability to extend the elbow
actively against gravity indicates discontinuity of the triceps
mechanism. -
A careful neurosensory evaluation should
be performed, because associated ulnar nerve injury is possible,
especially with comminuted fractures resulting from high-energy
injuries.
P.205
RADIOGRAPHIC EVALUATION
-
Standard anteroposterior and lateral
radiographs of the elbow should be obtained. A true lateral radiograph
is imperative, because this will demonstrate the extent of the
fracture, the degree of comminution, the degree of articular surface
involvement, and displacement of the radial head, if present. -
The anteroposterior view should be
evaluated to exclude associated fractures or dislocations. The distal
humerus may obscure osseous details of the olecranon fracture.
CLASSIFICATION
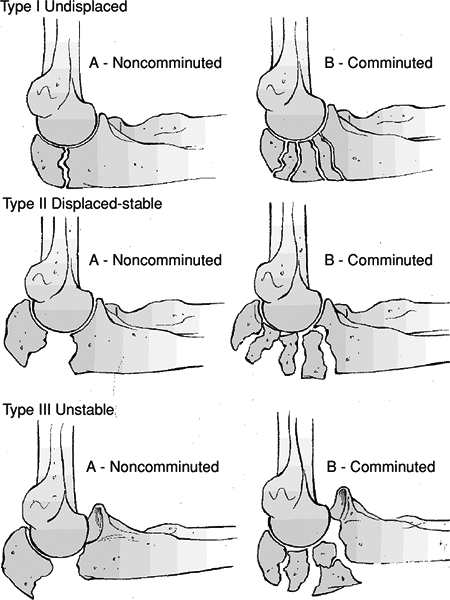
Mayo Classification (Fig. 19.1)
This distinguishes three factors that have a direct
influence on treatment: (1) fracture displacement, (2) comminution, and
(3) ulnohumeral stability.
influence on treatment: (1) fracture displacement, (2) comminution, and
(3) ulnohumeral stability.
-
Type I fractures are nondisplaced or
minimally displaced and are subclassified as either noncomminuted (type
1A) or comminuted (type 1B). Treatment is nonoperative. -
Type II fractures have displacement of
the proximal fragment without elbow instability; these fractures
require operative treatment.-
Type IIA fractures, which are noncomminuted, can be treated by tension band wire fixation.
-
Type IIB fractures are comminuted and require plate fixation.
-
-
Type III fractures feature instability of the ulnohumeral joint and require surgical treatment.
Schatzker (Based on Fracture Pattern) (Fig. 19.2)
-
Transverse: This occurs at the apex of
the sigmoid notch and represents an avulsion fracture from a sudden,
violent pull of both triceps and brachialis, and uncommonly from direct
trauma. -
Transverse-impacted: A direct force leads to comminution and depression of the articular surface.
-
Oblique: This results from hyperextension injury; it begins at midpoint of the sigmoid notch and runs distally.
-
Comminuted fractures with associated
injuries: These result from direct high-energy trauma; fractures of the
coronoid process may lead to instability. -
Oblique-distal: Fractures extend distal to the coronoid and compromise elbow stability.
-
Fracture-dislocation: It is usually associated with severe trauma.
OTA Classification of Proximal Radius/Ulna Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT OBJECTIVES
-
Restoration of the articular surface
-
Restoration and preservation of the elbow extensor mechanism
-
Restoration of elbow motion and prevention of stiffness
-
Prevention of complications
P.206
TREATMENT
 |
|
Figure
19.1. The Mayo classification of olecranon fractures divides fractures according to displacement, comminution, and subluxation/ dislocation. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
Nonoperative
-
This is indicated for nondisplaced fractures and displaced fractures in poorly functioning older individuals.
-
Immobilization in a long arm cast with
the elbow in 45 to 90 degrees of flexion is favored by many authors,
although in reliable patients a posterior splint or orthosis with
gradual initiation of range of motion after 5 to 7 days may be used. -
Follow-up radiographs should be obtained
within 5 to 7 days after treatment to rule out fracture displacement.
Osseous union is usually not complete until 6 to 8 weeks. -
In general, there is adequate fracture
stability at 3 weeks to remove the cast and to allow protected
range-of-motion exercises, avoiding flexion past 90 degrees.
P.207
 |
|
Figure 19.2. Schatzker classification of olecranon fractures.
(From Browner BD, Jupiter JB, Levine AM, eds. Skeletal Trauma. Philadelphia: WB Saunders, 1992:1137, with permission.)
|
Operative
-
Indications for surgery
-
Disruption of extensor mechanism (any displaced fracture)
-
Articular incongruity
-
-
Types of operative treatment:
-
Intramedullary fixation: 6.5-mm
cancellous lag screw fixation. The screw must be of sufficient length
to engage the distal intramedullary canal for adequate fixation. This
may be used in conjunction with tension band wiring (described later).-
With screw techniques, beware of bowing of the ulna intramedullary canal that may shift the fracture with screw advancement.
-
-
Tension band wiring in combination with
two parallel Kirschner wires: This counteracts the tensile forces and
converts them to compressive forces and is indicated for avulsion-type
olecranon fractures (Fig. 19.3). -
Plate and screws: They are used for
comminuted olecranon fractures, Monteggia fractures, and olecranon
fracture-dislocations. A plate should also be for oblique fractures and
for fractures that extend distal to the coronoid.-
No mechanical difference exists between posterior or lateral placement.
-
Fewer problems with plate prominence are noted when it is placed laterally.
-
-
Excision (with repair of the triceps tendon): This is indicated for nonunited fractures, extensively comminuted fractures,
P.208
fractures in elderly individuals with severe osteopenia and low functional requirements, and extraarticular fractures.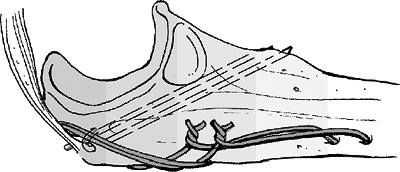 Figure 19.3. The Kirschner wires are then bent 180 degrees and are impacted into the olecranon beneath the triceps insertion.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 19.3. The Kirschner wires are then bent 180 degrees and are impacted into the olecranon beneath the triceps insertion.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)-
Wolfgang et al. reported that excision of as much as 50% of the olecranon is effective in treating comminuted fractures.
-
Morrey et al. demonstrated decreasing elbow stability with increasingly larger fragment excision.
-
This is contraindicated in
fracture-dislocations of the elbow or fractures of the radial head,
because excision results in compromised elbow stability.
-
-
-
Postoperative management: the patient
should be placed in a posterior elbow splint. With a stable repair, one
should initiate early range-of-motion exercises.
COMPLICATIONS
-
Hardware symptoms occur in 22% to 80% of patients.
-
From 34% to 66% require hardware removal.
-
-
Hardware failure occurs in 1% to 5%.
-
Infection occurs in 0% to 6%.
-
Pin migration occurs in 15%.
-
Ulnar neuritis occurs in 2% to 12%.
-
Heterotopic ossification occurs in 2% to 13%.
-
Nonunion occurs in 5%.
-
Decreased range of motion: This may
complicate up to 50% of cases, particularly loss of elbow extension,
although most patients note little if any functional limitation.
