Little League Elbow
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Little League Elbow
Little League Elbow
Paul D. Sponseller MD
Description
-
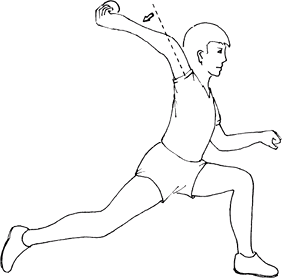
“Little League elbow” refers to a group
of injuries about the elbow that arise in children and adolescents
(ages 7–15 years) from repetitive throwing or use of a racquet or bat (Fig. 1).-
Younger patients (7–11 years old) in that
group often have an injury of the physis, whereas older adolescents
(15–19 years old) are subject to avulsion fractures or ligament tears.
-
-
These injuries also are referred to as osteochondroses, or disordered behavior of growing cartilage under load.
-
Classification:
-
Medial disease involves the MCL, the medial epicondyle, and the surrounding soft tissues.
-
Lateral disease involves the radial head, the capitellum, the lateral epicondyle, and surrounding soft tissues.
-
-
Synonym: Osteochondritis (or osteochondrosis) of the radial head or capitellum (Panner disease)
General Prevention
-
League guidelines (1,2) on the frequency of pitching for juvenile players exist to minimize this disorder.
-
Elbow pain in juvenile athletes should be a guide to slowing down.
Epidemiology
Incidence
The incidence increases with the intensity of competition.
 |
|
Fig.
1. Little League elbow results from valgus strain, which may cause tendinitis medially or osteochondritis laterally in the growing elbow. |
Risk Factors
Throwing or serving sports in young children and adolescents (e.g., baseball, football, javelin, and tennis) are risk factors.
Genetics
No Mendelian inheritance pattern is known.
Etiology
-
Medial epicondylar fragmentation or avulsion
-
Delayed or accelerated growth of the medial epicondyle
-
Delayed closure of the medial epicondylar growth plate
-
Osteochondritis (irregular ossification) of the capitellum
-
Deformation and osteochondritis of the radial head
-
Olecranon apophysitis with or without delayed closure of the olecranon apophysis
Signs and Symptoms
-
Most patients present with medial elbow
pain, although some have lateral pain (see later), with diminished
throwing distance and decreased throwing effectiveness.-
The patient may present with vague
lateral elbow pain and swelling (capitellar osteonecrosis [Panner
disease; ages 7–12 years]) versus osteochondritis dissecans of the
capitellum (ages 13–16 years).
-
-
Pain is aggravated by throwing.
-
Examination shows point tenderness over the medial epicondyle, swelling, and a flexion contracture often >30°.
-
The injury most often involves the dominant elbow.
-
Nocturnal pain is uncommon.
-
Burning around the medial elbow
associated with paresthesias or dysesthesias in the ulnar digits
signifies ulnar nerve involvement. -
Duration of symptoms can help to differentiate injuries such as UCL ruptures (acute) and medial epicondylitis (chronic).
-
Late-presenting lateral symptoms include locking, catching, and severe pain.
-
-
Posterior abnormalities suggest involvement of the olecranon and surrounding soft tissues.
History
Obtain detailed frequency of athletic elbow use.
Physical Exam
-
Document the elbow ROM, including flexion, extension, pronation, and supination.
-
Look for an effusion, as signified by loss of the normal lateral soft-tissue recess.
-
Pinpoint the location of tenderness.
-
Perform a neurovascular examination of the extremity.
-
Observe the patient performing the causative motion.
-
Stability of the elbow to valgus stress with the elbow in 25° of flexion helps assess the collateral ligaments.
Tests
Imaging
-
Radiography:
-
Plain radiographs (AP and lateral) are obtained to rule out fractures, loose bodies, or osteochondritis dissecans.
-
Stress radiographs may be helpful.
-
-
Bone scan is useful to assess asymmetrical activity.
-
MRI may be useful in evaluating injury to cartilage, physis, tendons, muscles, and ligaments (2).
Pathological Findings
-
Weak physes in growing children make
injuries to this area (fracture or osteochondritis) common, whereas
young adults with fused physes tend to develop more soft-tissue
injuries. -
The pathologic process of Panner disease and osteochondritis dissecans is unknown but thought to arise from repetitive trauma.
-
Osteochondritis dissecans may progress to loose bodies with painful locking.
Differential Diagnosis
-
Elbow fracture (supracondylar humerus, olecranon)
-
Ulnar nerve subluxation
-
Ulnar nerve entrapment or posterior interosseous nerve entrapment
-
Tendinitis of the medial or lateral elbow muscle origin
-
Loose bodies in the joint
P.233
General Measures
-
Most injuries resolve with 4–6 weeks of rest.
-
With severe pain, a regimen of 1–2 weeks of splint immobilization is helpful, followed by active ROM exercises.
-
Loose bodies often require surgical removal.
-
Occasionally, large osteochondritis
dissecans fragments and avulsion fragments with >2 mm of
displacement require surgical fixation. -
Activity should be resumed on a gradual, stepwise basis.
-
Stability of the elbow should be assessed before the patient returns to competitive throwing.
-
If symptoms resume with activity after 6
weeks of rest, additional investigation into causes should be
investigated (via CT, MRI).
Special Therapy
Physical Therapy
-
After 6–8 weeks of rest, when the patient
is asymptomatic and has pain-free ROM, begin elbow strengthening
exercises with a progressive throwing program. -
The therapist or trainer may be effective
in supervising the patient’s return to sports more closely than the
physician is able to do.
Medication
-
NSAIDs are the drugs of choice.
-
Steroid injections rarely are indicated.
Surgery
-
Many of these conditions may be treated
arthroscopically, including pinning of osteochondritis dissecans
fragments, removal of loose bodies, and removal of osteophytes. -
Occasionally, open reconstruction or repair of the UCL is necessary for avulsion injuries.
Prognosis
-
Overall, most patients do well with rest.
-
Occasionally, one may develop slight flexion contractures and valgus deformity of throwing arm, which is rarely symptomatic.
Complications
-
Rare: Panner disease may lead to late deformity and collapse of the capitellum articular surface (3).
-
Osteochondritis dissecans fragments may displace and become a loose body in the joint, requiring removal.
-
Epicondyle fractures may progress to a nonunion, usually asymptomatic.
Patient Monitoring
Patients with Panner disease should have follow-up radiographs every 3–4 months to assess healing of the capitellum.
References
1. Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med 2003;33:75–81.
2. Kocher MS, Waters PM, Micheli LJ. Upper extremity injuries in the paediatric athlete. Sports Med 2000;30:117–135.
3. Hang DW, Chao CM, Hang YS. A clinical and roentgenographic study of Little League elbow. Am J Sports Med 2004;32:79–84.
Codes
ICD9-CM
726.32 Little League elbow
Patient Teaching
-
Instruct the patient in proper throwing mechanics.
-
Recognize symptoms early.
-
Rest from throwing activities (6–8 weeks) to avoid additional injury.
-
Advise a gradual return to competitive sports when the patient is asymptomatic.
-
Recurrence of symptoms often requires longer rest followed by strengthening exercises.
FAQ
Q: If a preteen pitcher has Little League elbow, should he be counseled to switch positions?
A:
Recurrence is likely, and switching should be discussed as an option.
However if it is a 1st presentation, a cycle of rest and graduated
resumption of pitching may be successful in some cases.
Recurrence is likely, and switching should be discussed as an option.
However if it is a 1st presentation, a cycle of rest and graduated
resumption of pitching may be successful in some cases.
