Intercostal Block
Editors: Chelly, Jacques E.
Title: Peripheral Nerve Blocks: A Color Atlas, 3rd Edition
Copyright ©2009 Lippincott Williams & Wilkins
> Table of Contents > Section
II – Single-Injection Peripheral Blocks > C – Miscellaneous Blocks
> 20 – Intercostal Block
II – Single-Injection Peripheral Blocks > C – Miscellaneous Blocks
> 20 – Intercostal Block
20
Intercostal Block
Barry F. Bass
Analgesia for thoracic and upper abdominal surgery, analgesia for rib
fracture and to facilitate ventilation in flail chest, and treatment of
neuropathic pain such as postherpetic neuralgia and cancer-related pain
syndromes. Can also be used as a diagnostic procedure to differentiate
neuropathic pain from visceral pain.
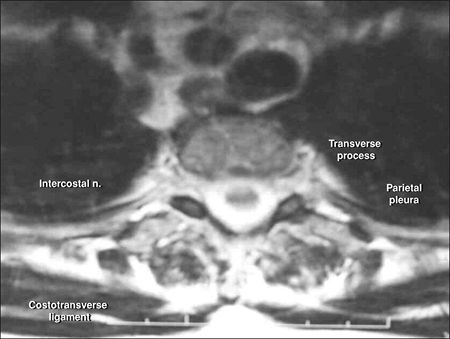
Construct a vertical line joining the spinous processes of the thoracic
vertebra corresponding to the nerves to be blocked. Palpate the edge of
the sacrospinalis muscle and mark the lateral edge. The muscle will
become broader as it extends caudad. A line is drawn along the edge of
the muscle. The inferior border of the rib is marked and extended to
bisect the line marking the lateral border of the muscle. The distance
from the inferior border of the rib to the pleura is about 5 mm (Fig. 20-1).
Skin wheals are raised over the area to be blocked with 1% lidocaine.
For a right-handed operator, the left index finger is placed over the
skin wheal and the skin is retracted cephalad (Fig. 20-2A).
The needle is advanced perpendicularly onto the rib. The needle is
grasped between the index finger and thumb of the operator’s left hand.
Resting the hypothenar eminence against the patient’s paraspinal muscle
steadies the left hand. The needle is now slowly and methodically
walked off the rib in a caudal direction (Fig. 20-2B).
Once off the inferior border of the rib, the needle is slowly advanced
into the neurovascular sheath, which should lie no more than 8 mm below
the upper border of the rib. A slight “pop” may be felt as the needle
enters the sheath. After aspiration, 3 to 5 mL of local anesthetic
solution is injected at each level. The procedure is repeated at each
level to be blocked.
P.186
 |
|
Figure 20-1. Anatomic landmarks.
|
-
If the patient is unable to lie in the
prone position, the lateral position, with the arm on the side to be
blocked rotated over the head, is acceptable. -
Use fluoroscopy whenever available to ascertain accuracy of needle placement and thus avoid pneumothorax.
-
This approach ensures block of the lateral cutaneous branch of the intercostal nerve.
-
The use of light sedation is encouraged to provide a quiet operating field, especially in patients who are being ventilated.
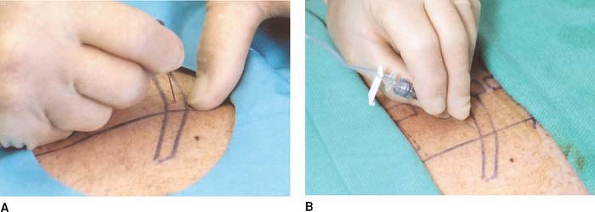 Figure 20-2. A: The index finger is placed over the skin wheal and the skin is retracted. B: The needle is slowly and methodically walked off the rib.P.187
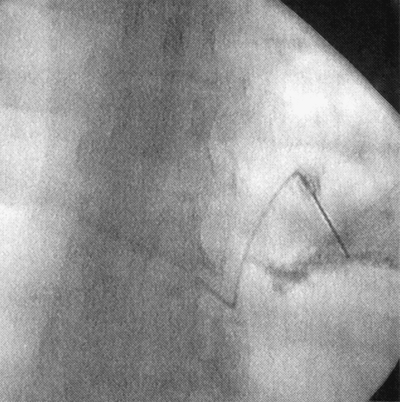
Figure 20-2. A: The index finger is placed over the skin wheal and the skin is retracted. B: The needle is slowly and methodically walked off the rib.P.187![]() Figure 20-3. Procedure done under fluoroscopy.
Figure 20-3. Procedure done under fluoroscopy. -
Use an extension tube on the syringe to provide better control and thus steady the injecting hand.
-
Keep notes of volumes injected to prevent systemic toxicity and epinephrine overdose.
-
Following multiple-level blocks, postblock chest x-ray is recommended. Pneumothorax is a complication in 1% to 2% of cases.
-
If more than three levels are to be
blocked or if analgesia for periods over 8 to 12 hours is requested,
the continuous paravertebral approach is suggested. -
A short rigid-walled catheter connecting
the needle and syringe takes weight off the needle and can allow the
injection to be done by an assistant, allowing the operator more
control of the needle. -
If the procedure is done under
fluoroscopy, injection of 1 mL of contrast will confirm placement of
the needle within the neurovascular space (Fig. 20-3).
Suggested Readings
Moore DC. Intercostal nerve block for postoperative somatic pain following surgery of the thorax and upper abdomen. Br J Anaesth 1975;47:284–286.
Moore DC, Bridenbough LD. Intercostal nerve block in 4333 patients: indications, techniques and complications. Anesth Analg 1962;41:1.
Waldman SD. Interventional pain management, 2nd ed. Philadelphia: WB Saunders, 2001.