Hip Arthroscopy Intervention in Early Hip Disease
– HIP > Part C – Operative Treatment Methods > 8 – Hip
Arthroscopy Intervention in Early Hip Disease
was implicated in the evolution of hip arthritis and was cited as a
potential cause for hip pain with normal-appearing radiographs. On the
heels of clinical success with knee and shoulder arthroscopy, hip
arthroscopy emerged in the mid 1980s, predominantly as a treatment
modality for removal of loose bodies and evaluation and resection of
acetabular labral defects.
recognition of the considerably wider spectrum of intra-articular hip
pathology amenable to arthroscopic evaluation, the techniques of hip
arthroscopy have continued to evolve. Most recently, with renewed
interest in minimally invasive surgical techniques, hip arthroscopy is
being explored as a potential adjunct to other surgical interventions
designed to address a wider array of hip pathology.
fusion of the three ossification centers of the pelvis: the pubis,
ischium, and ilium. Normal hip anatomy includes a ball-and-socket
configuration with deep intrinsic stability. The femoral head
articulates at a neck shaft angle typically of 130 degrees and 10
degrees of anteversion. Developmental variances provide a wide spectrum
of head coverage. This variability is compounded by the degree of
anteversion of the acetabular opening and the flexural position of the
pelvis relative to the lumbar spine. The motion of the hip is typically
considered in three planes: sagittal, frontal, and transverse. The
greatest degree of motion occurs in the sagittal plane.
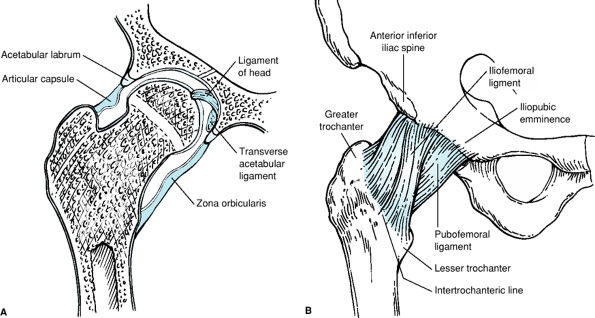
structure that rims the edge of the acetabulum. The labrum originates
anteriorly at the transverse acetabular ligament. The anterior and
superior aspects of the acetabular labrum are typically triangular.
Posteriorly, the labrum is less pronounced and more rounded. A small
sulcus is present between the labrum and the articular margin of the
acetabular cartilage. This sulcus is typically more pronounced
posteriorly. The hip capsule is composed of dense fibrous tissue and
can anatomically be divided into three ligaments. These include the
iliofemoral ligament or Y ligament of Bigelow, which extends from
anterior superiorly on the ileum down to the anterior intertrochanteric
ridge. The ischial femoral ligament is typically considered a capsular
thickening, which wraps forward from the posterior acetabular rim to
the piriformis fossa. The third component of the hip capsule is a
pubofemoral ligament, which extends inferiorly from the pubis to the
posterior inferior femoral neck. The patulence of the hip capsule is
greatest inferiorly, and is constricted around the neck of thefemur by
circular oriented fibers of the hip capsule, forming the zona
orbicularis.
subcutaneous tissues, abductor muscle mass, and the capsular
structures. Because of the intimate configuration of the
ball-and-socket joint, arthroscopic visualization of the articular
surface generally requires distraction of the hip to allow access
between the femoral head and the acetabulum. The thick muscular
envelope and often thick subcutaneous layer require exacting techniques
of portal placement to ensure optimal mobility of the instruments
within the hip joint.
vessels originating from the acetabular bony rim. Nociceptors are
present within the labral tissue. Consequently, damage to the
acetabular labrum can result in pain, and tearing of the acetabular
labrum away from the acetabular rim may devascularize the labral
fragment. The dysvascular labral tear has limitedpotential for
spontaneous healing.
Consequently, hip distraction typically is best achieved with slight
hip flexion. The ligamentum teres remains recessed within the
acetabular fossa. In the neonate, blood supply to the femoral epiphysis
occurs via the terminal branches of the medial femoral circumflex
artery via the ligamentum teres. In the adult, the ligamentum teres
exists primarily as a tendinous structure attached to the base of the
acetabulum at the confluence of the transverse acetabular ligament and
the fovea on the femoral head. In the adult, the artery of the
ligamentum teres supplies only a vestige of blood supply to the femoral
head (Fig. 8-1A, B).
 |
|
Figure 8-1 A: Midcoronal cross-sectional drawing of the right hip. B: Right hip pericapsular structures.
|
understanding of hip anatomy, improvements in distraction techniques,
and instrumentation designed specifically to address hip pathology
arthroscopically. Prior to hip arthroscopy, open exploration of the hip
with dislocation of the hip was the only method to address many
intra-articular problems including loose bodies, acetabular labral
tears, bone spurs, and synovial pathology.
diagnostic evaluation of the painful hip, excision of loose bodies,
management of synovial chondromatosis, resection of labral tears and
chondral flaps, diagnostic evaluation of osteonecrosis, treatment of
torn ligamentum teres, partial synovectomy, foreign body removal,
posttraumatic excision of osteochondral fragments, lavage in
crystalline arthropathy or early sepsis as well as capsular shrinkage
in conditions of instability such as Ehlers-Danlos. Additionally, hip
arthroscopy has been used in removal of loose bodies following total
hip arthroplasty and as an adjunct for management of extra-articular
conditions such as snapping psoas tendon, bursectomy, and soft tissue
releases. The indications will be discussed individually below.
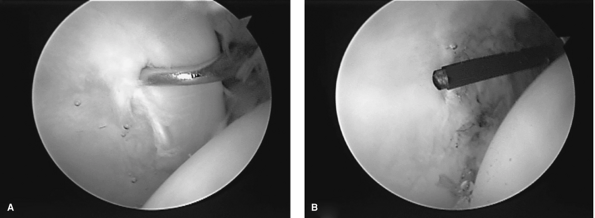
superior quadrant of the acetabulum. When present, a labral tear can
produce functionally limiting symptoms typically characterized as
catching or occasionally popping. Arthroscopic visual inspection can
delineate areas of degenerative tearing that are amenable to resection
and/or stabilization techniques. Acetabular labral stabilization,
although inherently appealing, is technically challenging and is
typically reserved for acute traumatic tears of the acetabular labrum.
Arthroscopy provides excellent visualization and access to the
acetabular labrum (Fig. 8-2A, B).
locking presentation. They may be ossified but commonly are
cartilaginous. These loose bodies within the hip are notoriously
difficult to visualize with either plain x-ray views or other
radiographic studies. Synovial osteochondromatosis can result in
accumulation of dozens of loose bodies within the hip joint.
Arthroscopic techniques are particularly helpful in the management of
loose bodies because removal is associated with a high degree of
symptom relief.
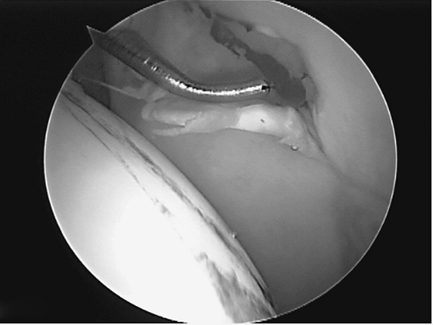
association with loose bodies. These lesions are distinguished from
degenerative wear within the hip, which results in a widespread
thinning of the articular cartilage and exposure of subchondral bone.
Full-thickness osteochondral lesions may occur as a result of impact
injury but more commonly are associated with the delamination of the
chondral surface in association with other entities, including labral
tears and femoro-acetabular impingement (Fig. 8-3).
Resection of chondral flap injury to stable margins is associated with
a high degree of symptom resolution. Clinical outcome is predicated on
the size and location of the articular cartilage injury. The prognosis
is typically poor when full-thickness chondral injury is present on
both the acetabulum and femoral head. Additionally, when acetabular
chondral lesions exceed 1 cm square, the shouldering effect of the
cartilage is diminished and the prognosis is more guarded.
 |
|
Figure 8-2 A:
Tears of the acetabular labrum often occur at the junction of the labrum and the articular cartilage of the acetabulum. The distracted femoral head is visible at the right of the field. B: Flexible thermal ablation probes are quite useful in resection of degenerative labral tears. |
 |
|
Figure 8-3 Chondral delamination is often seen at the anterior origin of the acetabulum in association with labral tears.
|
may result in tearing and degenerative change within the ligamentum
teres. The tendinous ligament, when avulsed from the fovea of the
femoral head, may result in impingement or a catching/locking pain
pattern. Arthroscopic resection of the ligamentum teres from the fovea
typically results in near complete pain relief.
pathologic conditions including crystalline arthropathy, collagen
vascular disease, mechanical irritation, or viral cause. An effusion of
the hip joint can be quite painful and is visible on T2-weighted MRI.
When diagnostic uncertainty exists, aspiration of the hip is not
conclusive, and other serum-based testing fails to yield a diagnostic
conclusion, hip arthroscopy may be used for lavage as well as for
synovial biopsy. Additionally, for conditions that are synovium based,
such as synovial chondromatosis, which result in synovial tissue
production of chondral or osteochondral loose bodies, arthroscopic
excision of the loose bodies and thermal ablation of the visible
synovial tissues can lead to symptom resolution.
villonodular synovitis may be treated in a temporizing manner or even
potentially eradicated with arthroscopic techniques. Collagen vascular
diseases such as lupus, juvenile rheumatoid arthritis, or rheumatoid
arthritis may manifest first with hip pain. Synovial biopsy can prove
diagnostic when these patients are seronegative.
management of acute pyarthrosis of the hip. Clinical series in the
literature support use of hip arthroscopy in both the adult and
pediatric population following the early onset of symptoms, and good
results have been reported in patients with favorable host parameters
and susceptible bacteria. After lavage of the hip joint and
arthroscopic assessment of the cartilaginous surfaces, a small drain
can be left within the hip capsule temporarily to facilitate
decompression. Obviously, arthroscopic management is performed in
conjunction with appropriate antibiotic treatment.
impingement is evolving. There are reports of patients in whom the
offending femoral neck impingement is adequately decompressed
arthroscopically. However, no large series to date substantiates these
findings. Hip arthroscopy also can be used as an adjunct to open
arthrotomy for more involved femoral acetabular impingement.
Arthroscopy allows a more intimate and detailed evaluation of the
acetabular labrum in the area of impingement as well as an assessment
of the articular cartilage prior to initiation of a surgical
dislocation of the hip for femoral neck contouring procedures.
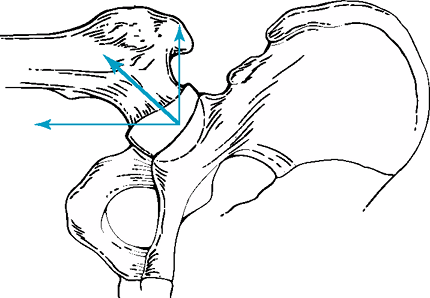
Most hip arthroscopists use a distraction apparatus specifically
designed for hip arthroscopy or a fracture table (Fig. 8-4).
To adequately visualize the inner aspects of the acetabulum and to
assess intra-articular pathology, the femoral head must be distracted
from the acetabulum. The orientation of the traction must affect a
resultant force parallel to the femoral neck. This is typically
achieved with a peroneal post and longitudinal distraction. The hip is
slightly flexed and slightly externally rotated to relax the anterior
hip capsular structures. Image intensification is used to assess joint
distraction, and these cases are typically performed under general
anesthesia with skeletal muscle relaxation to reduce the distraction
force (Fig. 8-5).
 |
|
Figure 8-4
A fracture table is useful to assist with distraction of the hip. Note the positioning of fluoroscopy, which is draped within the surgical field. |
 |
|
Figure 8-5
Axial traction is accompanied by lateral traction via the peroneal post. The resultant traction vector is in line with the femoral neck, allowing the femoral head to lift out of the acetabulum. |
needles that can be advanced into the hip capsule. A small nitinol wire
is passed through the needle, then various cannula and sleeves can be
advanced safely over the wire into the hip joint.
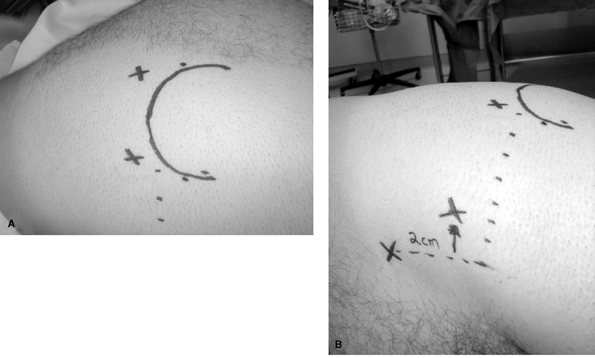
arthroscopy. These include the anterior and posterior peritrochanteric
portals and a direct anterior portal. The location of the
peritrochanteric portal is approximately 1 to 2 cm proximal to the bony
tip of the greater trochanter and located at the anterior and posterior
margins of the trochanteric profile. The direct anterior portal
typically is localized by drawing a vertical line from the anterior
superior iliac spine down on the anterior thigh and a horizontal line
from the top of the greater trochanter intersecting the anterior
superior iliac spine (ASIS) line. From this point on the horizontal,
the portal is lateralized to the junction of the middle third and
medial third of the horizontal line from the tip of the trochanter.
This location will avoid injury to the superficial femoral cutaneous
nerve. The anterior and posterior peritrochanteric portals provide
excellent visualization of the entire intra-articular hip. The direct
anterior portal facilitates a working portal in the anterior inferior
quadrant of the hip (Fig. 8-6A, B).
hip arthroscope sets provide longer instrumentation, scope cannulae,
and lenses. Flexible and maneuverable thermal ablation probes provide
the ability to manipulate synovial and chondral structures, and a
combination of
shavers and burrs are used to assist with contouring and loose body removal.
 |
|
Figure 8-6 A: The trochanteric outline is used to localize the anterior and posterior peritrochanteric portals. B: The anterior portal is typically lateral to the anterior superior iliac crest.
|
the zone orbicularis, can be accessed for loose body removal via the
anterior peritrochanteric and direct anterior portals. The femoral head
is allowed to reduce into the acetabulum as traction is released. The
hip joint is flexed approximately 45 degrees with slight adduction,
which provides increased patulence in the inferior recess of the hip
capsule. Fluoroscopy is helpful in achieving cannula positioning.
relatively safe operative intervention. The complication rate in the
largest series reported to date by Villiar was 1.4%, which included
transient sciatic palsy, transient femoral palsy, vaginal tear, and
hematoma. Avoiding major complications including severe neurovascular
injury requires exacting techniques on the part of the surgeon and
fluoroscopic assistance in portal placement. The surgeon should
carefully pad the perineum and the ankle as considerable distraction
forces are applied during the course of the surgical procedure.
Distraction time should be limited, typically to >2 hours.
as ankylosis; severe petrusio or heterotrophic ossification should
discourage attempted arthroscopy due to the risk of injury from
distraction and obstruction at typical portals from the surrounding
bone. Because of the depth of the hip joint, morbid obesity remains a
relative contraindication.
articular surfaces of the acetabulum and femoral head. Modern
arthroscopy techniques facilitate management of a myriad of pathologic
conditions within the hip joint and permit modulation of early hip
disease. Refinement of indications for hip arthroscopy will continue as
longer-term outcome studies emerge.
JW, Thomas, Jones KS. Diagnostic accuracy of clinical assessment,
magnetic resonance imaging, magnetic resonance qrthrography, and
intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668–1674.
PA, Murphy KP, Carroll JF. Sublabral sulcus at the posteroinferior
acetabulum: a potential pitfall in MR arthrography diagnosis of
acetabular labral tears. AJR Am J Roentgenol. 2004;183:1745–1753.
JL, Salvati EA, Laurencin CT, et al. The arthroscopic drainage,
irrigation, and debridement of late, acute total hip arthroplasty
infections: average 6-year follow-up. J Arthroplasty. 1999;14:903–910.
