Head-Sparing Procedures for Osteonecrosis of the Femoral Head
– HIP > Part C – Operative Treatment Methods > 9 – Head-Sparing
Procedures for Osteonecrosis of the Femoral Head
osteonecrosis in the United States and that osteonecrosis (ON) of the
femoral head accounts for approximately 10% of the more than 250,000
total hip replacements performed annually. 1
Patients with osteonecrosis of the femoral head are commonly in their
30s and 40s at the time of onset, and nearly 50% have bilateral
disease. Results of total hip arthroplasty in this patient group have
been inferior to other diagnostic groups. 2
These factors have led to the development of conservative surgical
methods aimed at sparing the femoral head. However, the efficacy and
the proper indications for these surgical interventions such as core
decompression (with or without grafting), osteotomy, and
hemiresurfacing arthroplasty are still debated. The preferred treatment
varies according to the severity, extent of the disease, condition of
the acetabular articular cartilage, and age of the patient. 2
or more risk factors known to predispose patients to developing this
disorder. Table 9-1 provides a list of the
known risk factors, leaving only about 20% of patients within the
idiopathic group. There is a high prevalence of underlying
thrombophilia or hypofibrinolysis in patients with osteonecrosis. 3
With the increasing number of etiologic associations, it is important
to delineate between these associations and pathogenesis. Mont and
others have proposed that the etiology of ON is multifactorial and
either there exists an accumulated tissue threshold whereby a number of
hits by various etiologic factors eventually meets the threshold for
disease or there are certain at-risk patients in whom some other
factors trigger the pathologic response. 4
that bone necrosis is the end result of severe and prolonged ischemia,
which may involve various mechanisms at different sites in extraosseous
and/or intraosseous vessels. This blockage of the osseous
microcirculation leads to intramedullary stasis, increasing
compartmental pressure, metabolic disturbance, anoxia, and eventually
death of osteocytes. The osteocytic death is eventually followed by the
reparative phase, at which time the femoral head is at greatest risk of
collapse when bone resorption exceeds production. 6
Because the bone most susceptible to vascular compromise is closest to
the joint space, the articular surface of the femoral head can become
incongruous after collapse owing to structural failure of the
underlying bone. More important, the time lapse between diagnosis and
severe joint deterioration of the joint leading to a major surgical
procedure is about 3 years in 50% of cases. 7
old. Males are more likely to be affected than females by a ratio of 8
to 1. 5,6,7,8
The most common symptom, seen in 50% of cases, is sudden pain in the
groin area, which may be progressive and associated with radiation to
the thigh. The pain is often worse at night. 5
The pain is usually triggered by weight bearing or by moving the
affected limb. Fifteen percent of patients will have occurrence of
osteonecrosis in other joints. 4
pain with internal hip rotation, but not uncommonly the exam will fail
to uncover any striking abnormalities. Thus a high index of suspicion
should be maintained. Further investigations to confirm the diagnosis
include plain radiographs and magnetic resonance imaging. Sufficient
plain radiographs must be ordered to permit evaluation of the contour
of the femoral head in more than one plane. In addition to the
anteroposterior and frog lateral radiographs, an anteroposterior pelvis
radiograph with the hip flexed at 45 degrees will show the anterior
contour and a 40-degree caudad view will show the posterior contour.
|
TABLE 9-1 Risk Factors Associated with Osteonecrosis
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
osteonecrotic bone segment are recognized to be the most important
prognostic factors. Ficat and Arlet’s original classification scheme
had four stages and was based on anteroposterior and frog lateral
radiographs. Stages II and III represented the distinction between
precollapse and postcollapse disease, and this classification system
established the premise for staging osteonecrosis and subsequent
classification systems. 5,7 Later on a stage 0 was added and qualified as the silent hip as first described by Marcus. 9
Standard radiographs show only the shadow of the mineralized portion of
a bone; consequently early bone necrosis has no specific radiographic
appearance, and a normal radiograph does not necessarily mean a normal
hip. On the MRI, a single-density line on the T1-weighted image
demarcates the normal ischemic bone interface, and a double-density
line on the T2-weighted image represents the hypervascular granulation
tissue. 6 On plain radiographs, the crescent sign originally described by Ficat 5
is characterized by the pathognomic appearance of a sequestrum on the
radiograph within which occurs a subchondral fracture, i.e., crescent
line.
 |
|
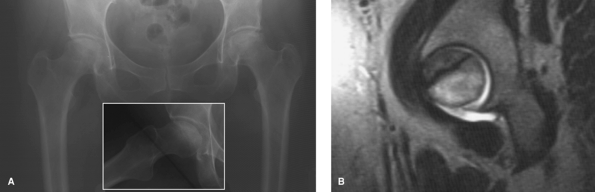
Figure 9-1 A 45-year-old female presents with an 8-month history of bilateral hip pain. A: Plain radiographs show bilateral collapse of femoral heads: stage IVC. Inset is the frog lateral of the right hip. B: Magnetic resonance imaging of the left hip shows the extent of necrotic lesion.
|
size of the necrotic segment has been shown to influence the outcome of
head-sparing procedures and was first quantified by Kerboull et al. 10
His sum included angles of the necrotic segment measured on the
anteroposterior (AP) and lateral radiographs, and found a sum of angles
greater than 200 degrees represented a worse prognosis. 2 (Fig. 9-1).
The more recently developed University of Pennsylvania system
incorporates size of lesion and magnetic resonance imaging findings (Table 9-2) and therefore represents a valuable classification system that aids in management. 11
secondary involvement of the acetabular cartilage owing to mechanical
damage caused by collapse of the femoral head, as demonstrated by both
Steinberg 12 and Beaulé. 13
Thus acetabular cartilage must be carefully evaluated at the time of
the operative procedure, and when there is severe damage, total hip
replacement may be the preferred method of treatment, especially when
patients are older than 40 years of age. 2
reviewed 54 hips to determine the risk of collapse and progression in
hips with osteonecrosis. At a mean followup of 6 years, only 31% of
hips went on to collapse when the necrotic area was less than
two-thirds of the weightbearing area compared to 68% with the larger
areas.
In
addition, the percentage of hips that went on to arthritic changes once
collapsed was 92% with necrotic areas greater than two-thirds compared
to 11% with the smaller area. All hips with >2 mm of initial
collapse continued to collapse. Impending femoral head collapse is seen
on radiographs as a crescent sign, which represents a fracture of the
bone and probably the cartilage as well, which will become further
depressed depending on the size of the lesion and joint loading forces.
|
TABLE 9-2 University of Pennsylvania Staging System for Osteonecrosis of the Femoral Head11
|
|||||||
|---|---|---|---|---|---|---|---|
|
considered carefully; the younger the patient, the more strongly a
joint- or bone-preserving procedure should be favored because it is
probable that he or she may require another operative procedure.
Because with osteonecrosis the acetabular cartilage of the hip is
secondarily mechanically damaged after the femoral head has collapsed
and this phenomenon is progressive, the duration of symptoms (pain)
provides some indication of the quality of the acetabular cartilage.
The extent of acetabular damage will ultimately affect the outcome of
joint and bone preserving procedures, i.e., osteotomy, free
vascularized fibular graft, hemiresurfacing arthroplasty, and the
trapdoor procedure. With respect to the cause and risk factors of
osteonecrosis, the continued use of high-dose steroids, alcohol, and/or
systemic lupus erythematosus is usually associated with a poorer
outcome with certain head-sparing procedures. 15
The judicious selection of the best treatment option is dependent on
careful analysis of patient demographics and cause, the extent of head
involvement, and articular cartilage damage of the acetabulum. The goal
of treatment is to optimize outcome while simultaneously minimizing
morbidity and maintaining treatment options for potential subsequent
secondary procedures.
of osteonecrosis. The best outcomes are for lesions with <15%
involvement with a 78% survivorship at an average of 63 months 16 and in those hips with sclerosis with a 95% survivorship at 10 years. 17 The value of bone grafting in addition to core decompression is uncertain. Aaron and associates 18
reported on 28 hips treated with demineralized bone matrix compared
with another group without grafting, and there was no significant
difference in success rate between these two groups for stage III with
survivorships of 83% and 72%, respectively. More recently, Hernigou and
Beaujean 19 presented their midterm
results of autologous bone marrow grafting after core decompression
using a 3-mm-diameter trephine. Hips with a lesion <25% in stages I
and II had the best outcome with only 9 out of 145 hips requiring a
total hip replacement versus 25 out of 44 hips for the rest of the
stages.
some patients with Steinberg stage III, it has no role in the treatment
of stage IV and V disease because it cannot restore articular
sphericity or remove the collapsed segment from the weight-bearing
area, and further cartilage degeneration is inevitable. Smith et al. 20
reported a 0% survivorship following core decompression at average
follow-up of 3 years for stage IV with all patients requiring another
operative procedure. Mont et al. 21
reviewed the radiographic predictors of outcome for 68 Ficat stage III
(Steinberg stage IV) hips following core decompression with mean
follow-up of 12 years. Only 29% had a satisfactory outcome. If core
decompression is combined with grafting in patients with Ficat stage
II/Steinberg stage III lesions, satisfactory results have been reported
for both nonvascularized and vascularized grafts. 22,23
used to support the subchondral surface and enhance revascularization
in combination with core decompression and osteoinductive cancellous
bone. These grafting procedures have a role in the precollapse stages,
but have inferior results in the postcollapse stages because of
articular cartilage involvement and the inability to restore femoral
head sphericity. For stages IV and V, several authors have reported
survivorships <75% at 5 years with surviving patients having Harris
hip scores <80. 20,22,24
The best results have been with earlier-stage lesions with a
survivorship of 89% at 50 months for stage III compared with 65% for
core decompression alone. However, one must carefully consider the
potential disadvantages of this surgery such as donor site morbidity at
24% 25 and a 2.5% incidence of subtrochanteric fracture. 26
has been used. In this procedure, an arthrotomy is performed to
dislocate the hip anteriorly, the necrotic segment of the head is
curetted out, and iliac crest bone graft is packed inside. This is
done through a cartilage window of the femoral head. Mont et al. 28
reported on a series of 24 hips with Ficat stage III (Steinberg stage
IVA) disease and 6 hips with early stage IV (Steinberg IVB) disease
treated with this procedure. At a mean duration of follow-up of 56
months (range 30 to 60 months), 73% had good to excellent results. Of
the eight hips with poor results, five had undergone subsequent
operative procedures. All of the poor results had combined necrotic
angles greater than 200 degrees. The results are encouraging, but the
procedure has limited indications because of the difficulty in
restoring the sphericity of the femoral head. Further study with longer
duration of follow-up will be required to assess the utility of this
procedure.
osteonecrosis have been variable and sometimes disappointing because of
the difficulty rotating the necrotic segment out from the
weight-bearing zone of the hip, especially when the lesion is large.
Langlais and Forestier 29 reported
their results with either the Sugioka (anterior) or Kempf (posterior)
rotational osteotomy in 20 patients with Ficat stages II and III
(Steinberg III and IV). The Kempf osteotomy was used for the atypical
case where the necrotic zone extended >30 to 40 degrees posteriorly.
Patients older than 45 years and patients with either steroid- or
alcohol-induced osteonecrosis were excluded from their study because of
predictably poor results. They recommended the Sugioka procedure only
for Steinberg stage III and the Kempf procedure for stages III and IV
where the depth of the necrosis was not more than one third of the head
diameter and located posteriorly.
it avoids the need for a greater trochanteric osteotomy and does not
risk compromising the blood supply to the femoral head. Mont et al. 30
reported on this technique in 31 hips with Ficat stage III (Steinberg
IV) disease at a mean follow-up of 11.5 years. Good to excellent
results were obtained in 74% of the hips. Poor results were associated
with age older than 45 years, a combined necrotic angle >200
degrees, and Dinulescu et al. 31
reported similar findings with survivorship of 70% at 5 years and 45%
at 10 years in 50 stage II and stage III hips. One of the main
disadvantages to intertrochanteric osteotomy is the apparent negative
effect on the complication rate and subsequent total hip arthroplasty,
both of which are probably related to the femoral deformity created by
the osteotomy. 30,32,33
Nevertheless, for surgeons with experience with the procedure, a
proximal femoral osteotomy is a reasonable head-sparing operation in
patients younger than 45 years of age, with Kerboull angle <200
degrees, and no continuing steroid use.
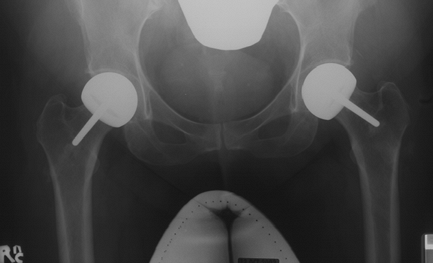
was first preformed in the early 1980s as a custom device in the young,
active population to preserve femoral bone stock and permit conversion
to a total hip replacement with minimal morbidity. 34,35,36,37,38 (Fig. 9-2). The results of this procedure have varied in different reports. Beaulé et al. 13
reviewed a series of 37 hips with a mean follow-up of 6.5 years (range
2 to 18 years), in which the acetabular cartilage involvement was
photographed at the time of the operative procedure and subsequently
graded. It was found that the longer duration of preoperative symptoms
the more severe the acetabular damage, and that hips that had been
converted to total hip replacement had a longer duration of symptoms
prior to their hemiresurfacing arthroplasty than the ones that were
still functioning (17 versus 12 months, respectively). The survivorship
in this series was 79% at 5 years, 62% at 10 years, and 45% at 15
years. Other centers using different hemiresurfacing designs have
reported comparable survivorship (i.e., 80% at 5 years and 60% at 10
years) and pain relief for osteonecrosis of the hip with Ficat stage
III and early IV disease (Steinberg IVA and IVB). However, as shown by
Mont et al., 40 the pain relief is
not as predictable as that following a total hip replacement: In their
patients a hemiresurfacing arthroplasty had a mean Harris hip score of
88 compared with 93 for patients with a total hip resurfacing (THR).
Proper component sizing and acetabular cartilage quality are probably
the two most important factors affecting outcome. A remaining challenge
is durability of the articular cartilage against the hemiresurfacing
component.
 |
|
Figure 9-2 Radiograph of patient shown in fig. 9-1 after bilateral hemiresurfacing arthroplasty.
|
controversial; however, it is generally believed that the size of the
lesion, as well as the stage of the disease at the time of treatment,
determine the outcome of head-sparing procedures. Core decompression
and or bone grafts have a role in the precollapse stages of
osteonecrosis. The size of the necrotic segment plays a critical role
in the outcome of proximal femoral osteotomies. Thus, unless a
relatively small lesion (Kerboull angle <200 degrees) is present,
hemiresurfacing arthroplasty provides a better clinical outcome
compared with other head-sparing procedures with the caveat that the
predictability of the pain relief is not that of a total hip
replacement. Because the acetabular cartilage damage increases over
time once collapse has occurred,
early
surgery is recommended for any type of head-sparing procedure. In the
presence of notable acetabular involvement or advanced Steinberg V
disease, total hip replacement offers the most predictable outcome.
KJ, Zurakowski D, Thornhill TS. Survivorship analysis of hips treated
with core decompression for nontraumatic osteonecrosis of the femoral
head. J Bone Joint Surg. 1999;81A: 200–209.
RK, Ciombor DM, Lord CF. Core decompression augmented with human
decalcified bone matrix for osteonecrosis of the femoral head. In:
Urbaniak JR, Jones JP Jr, eds. Osteonecrosis: Etiology, Diagnosis, Treatment. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1997:301–307.
BE, McKee MD, Richards RR, et al. Treatment of osteonecrosis of the
femoral head by free vascularized fibular grafting: an analysis of
surgical outcome and patient health status. Can J Surg. 1999;42:274–283.
MA, Jones LC, Pacheco I, et al. Radiographic predictors of outcome of
core decompression for hips with osteonecrosis stage III. Clin Orthop. 1998;159–168.
JR, Coogan PG, Gunneson EB, et al. Treatment of osteonecrosis of the
femoral head with free vascularized fibular grafting. A long-term
follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995;77:681–694.
DC, Plakseychuk AY, Rubash HE. Free vascularized fibula grafting for
the treatment of osteonecrosis of the femoral head. Clin Orthop Rel Res. 1997;344:243–256.
MA, Einhorn TA, Sponseller PD, et al. The trapdoor procedure using
autogenous cortical and cancellous bone grafts for osteonecrosis of the
femoral head. J Bone Joint Surg. 1998;80B:56–62.
I, Stanculescu D, Nicolescu M, et al. Long-term follow-up after
intertrochanteric osteotomies for avascular necrosis of the femoral
head. Bull Hosp Jt Dis. 1998;57:84–87.
HC, Grigoris P, Safran MR, et al. Precision-fit surface
hemiarthroplasty for femoral head osteonecrosis. Long term results. J Bone Joint Surg. 1994;76B:423–427.
MW, Mont MA, Scott R, et al. Surface replacement hemiarthroplasty for
the treatment of osteonecrosis of the femoral head. J Bone Joint Surg. 1998;80A:1656–1664.
MA, Rajadhyaksha AD, Hungerford DS. Outcomes of limited femoral
resurfacing arthroplasty compared with total hip arthroplasty for
osteonecrosis of the femoral head. J Arthroplasty. 2001;16(suppl 1):134–139.
