Fractures of the Proximal Radius and Ulna
patients usually involve the metaphysis or physis. True isolated radial
head fractures are rare. In the proximal ulna, the olecranon, which
biomechanically is a metaphysis, often fails with a greenstick pattern.
Fractures in this area also may involve the physis. Fractures of the
olecranon associated with proximal radioulnar joint disruption are
considered part of the Monteggia fracture-dislocation complex and are
discussed in Chapter 12.
of the large amount of cartilage in the radial head. If the fracture
involves the epiphysis, it usually is part of a Salter-Harris type IV
fracture pattern. In 90% of proximal radial fractures, the fracture
line involves either the physis or the neck.39
In six large series of elbow fractures, the incidence of fracture of
the radial neck was remarkably consistent, varying only from 5% to 8.5%.9,26,39,42,52,71
Fractures of the radial neck and head in skeletally immature patients
account for only 14% to 20% of the total injuries of the proximal
radius.30,42
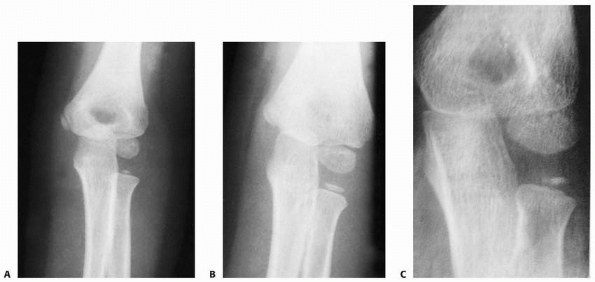
weeks of gestation. By 4 years of age, the radial head and neck have
the same contours as in an adult.71 Ossification of the proximal radius epiphysis begins at approximately 5 years of age as a small, flat nucleus (Fig. 11-1).
This ossific nucleus can originate as a small sphere or it can be
bipartite, which is a normal variation and should not be misinterpreted
as a fracture.11,60,99
(AP) projection radiograph, the edge of the metaphysis of the proximal
radius slopes distally on its lateral border. This angulation is normal
and not a fracture.
In the lateral view, the angulation can vary from 10 degrees anterior
to 5 degrees posterior, with the average being 3.5 degrees anterior.114
 |
|
FIGURE 11-1 Ossification pattern. A. At 5 years, ossification begins as a small oval nucleus. B. As the head matures, the center widens but remains flat. C.
Double ossification centers in developing proximal radial epiphysis. Reprinted with permission from Silberstein MJ, Brodeur AE, Graviss ER. Some vagaries of the radial head and neck. J Bone Joint Surgery AM 1982; 64. |
The radial collateral ligaments attach to the orbicular ligament, which
originates from the radial side of the ulna. The articular capsule
attaches to the proximal third of the neck. Distally, the capsule
protrudes from under the orbicular ligament to form a pouch (recessus
sacciformis). Thus, only a small portion of the neck lies within the
articular capsule.117 Because much
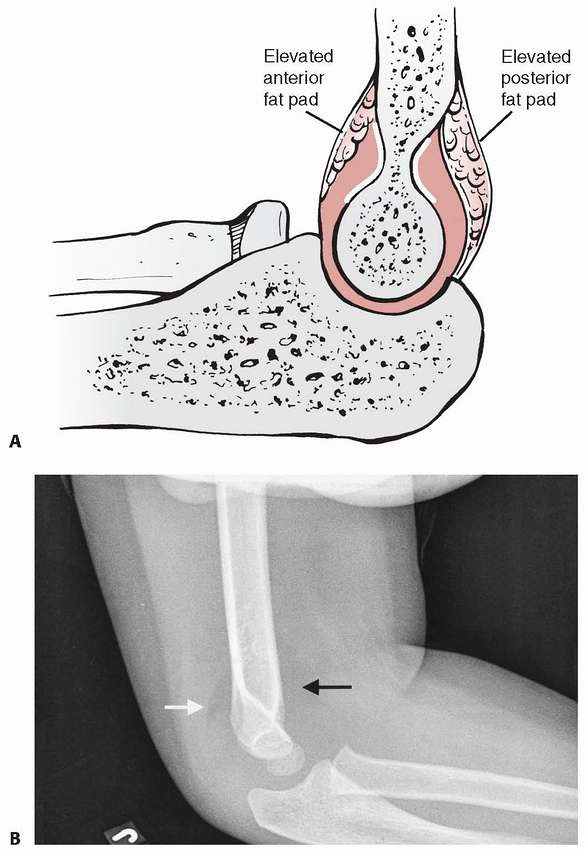
of the neck is extracapsular, fractures involving only the neck may not
produce an intra-articular effusion, and the fat pad sign may be
negative with fracture of the radial neck.11,40,99
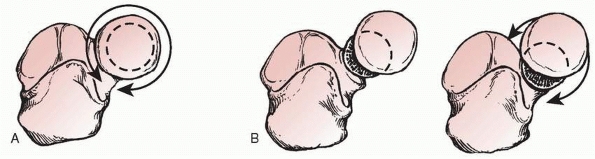
The axis of rotation of the proximal radius is a line through the
center of the radial head and neck. When a displaced fracture disrupts
the alignment of the radial head on the center of the radial neck, the
arc of rotation changes. Instead of rotating smoothly in a pure circle,
the radial head rotates with a “cam” effect. This disruption of the
congruity of the proximal radioulnar joint may result in a loss of the
range of motion in supination and pronation (Fig. 11-2).120
neck is painful. The pain is usually increased more with passive
forearm supination and pronation than with elbow flexion and extension.
In a young child, the primary complaint may be wrist pain,2
and pressure over the proximal radius may accentuate this referred
wrist pain. The wrist pain may be secondary to radial shortening and
subsequent distal radioulnar joint dysfunction. The misdirection of
such a presentation reinforces the principle of obtaining radiographs
of both ends of a fractured long bone.
 |
|
FIGURE 11-2 A. Normal rotation of the forearm causes the radial head to circumscribe an exact circle within the proximal radioulnar joint. B. Any translocation of the radial head limits rotation because of the “cam” effect described by Wedge and Robertson.120
|
lateral radiograph views. Occasionally, oblique views with the forearm
both supinated and pronated will reveal the fracture line clearly.
fracture. Most of these involve the radial head, although a step-off
also can develop as a normal variant of the metaphysis. There may be a
persistence of the secondary ossification centers of the epiphysis.
Comparison views are useful for evaluation of unusual ossification
centers after an acute elbow injury.
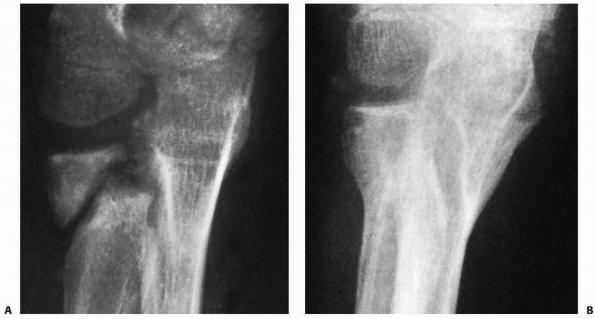
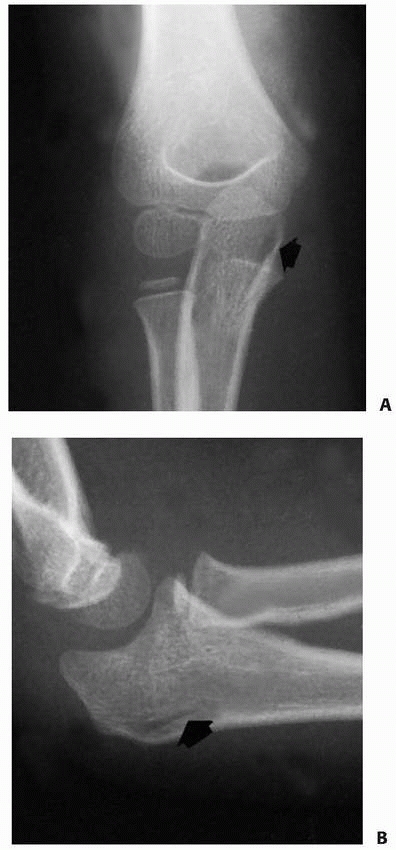
fracture of the radial neck may be difficult in children whose radial
head remains unossified. The only clue may be a little irregularity in
the smoothness of the proximal metaphyseal margin (Fig. 11-3). Rokito et al.93
reported complete displacement of the radial head in a 5-year-old male,
in whom the only clue on radiography was a small speck of ossification
in the elbow joint. The full extent of the injury was appreciated when
the radial head was outlined with magnetic resonance imaging (MRI).
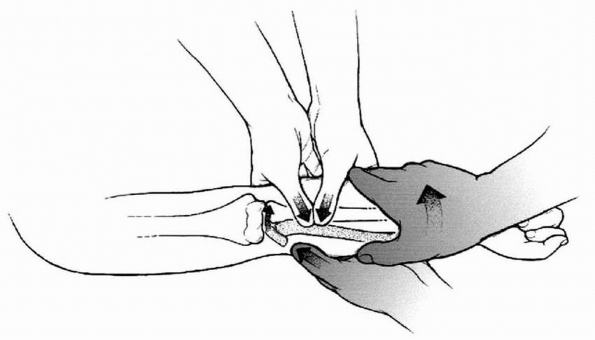
Javed et al.41 suggested considering
an arthrogram to assess the extent of the displacement and the accuracy
of reduction in children with an unossified radial epiphysis (Fig. 11-4).
 |
|
FIGURE 11-3
Preosseous fracture. The only clue to the presence of a fracture of the radial neck with displacement of the radial head was loss of smoothness of the metaphyseal margin (arrow). |
views are necessary to see the elbow in full AP profile. One view is
taken with the beam perpendicular to the distal humerus, and the other
with the beam perpendicular to the proximal radius. A regular AP view
with the elbow flexed may not show the fracture because of obliquity of
the beam. The perpendicular views show the physeal line of the radius
in clear profile.
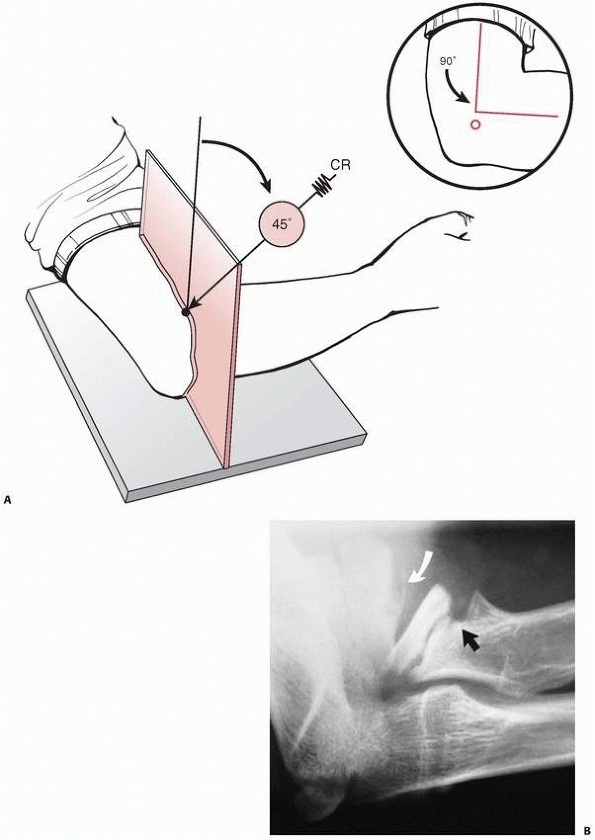
may be difficult to see because it is superimposed on the proximal
ulna, and oblique views of the proximal radius may be helpful.11,117 One oblique view that is especially helpful is the radiocapitellar view suggested by Greenspan et al.36,37 and Hall-Craggs et al.38 This view projects the radial head anterior to the coronoid process (Fig. 11-5) and is especially helpful if full supination and pronation views are difficult to obtain because of acute injury (Fig. 11-6).
head is usually obvious on a radiograph, but a minimally displaced
fracture is difficult to diagnose before ossification has begun.90
The loss of the smoothness of the metaphyseal margin may be the only
finding. Ultrasonography can be used to evaluate for hemarthrosis and
displacement of the fracture and allows a dynamic range-of-motion
evaluation.50 The supinator fat pad
is a small layer of fat that overlies the supinator muscle in the
proximal forearm. Displacement of the supinator fat pad may indicate
fracture of the proximal radius.92
The supinator fat pad and distal humeral anterior and posterior fat
pads are not always displaced with occult fractures of the radial neck
or physis.40,99,97
neck, special studies may be necessary. Arthrography, MRI, and
ultrasound50 are options for determining any displacement of the unossified radial head.
proximal radial fractures into three major groups based on the
mechanism of injury and displacement of the radial head (Table 11-1):
-
Group I: The radial head is primarily displaced (most proximal radial injuries are in this group).
-
Group II: The radial neck is primarily displaced.
-
Group III: Stress injuries.
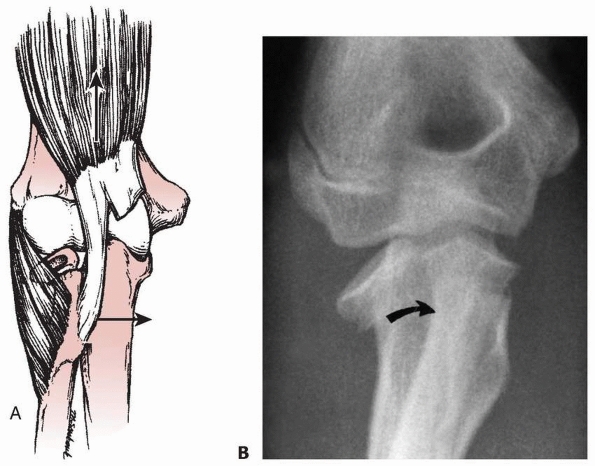
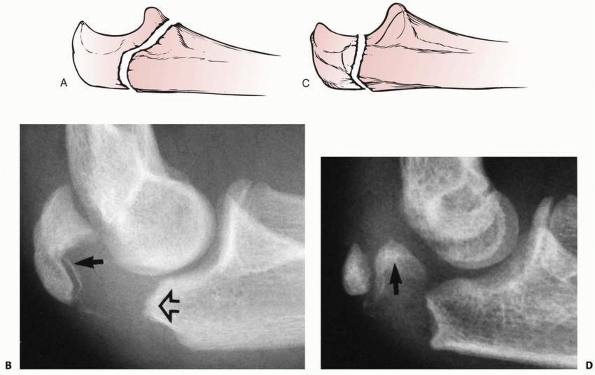
classification based primarily on the mechanism of injury. The two
subclasses of fractures in group I are valgus injuries and those
associated with elbow dislocations. Valgus injuries are subdivided into
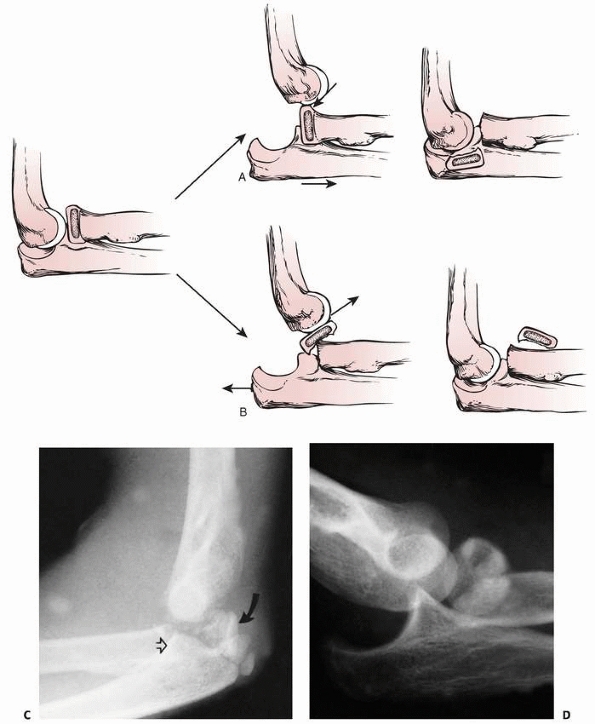
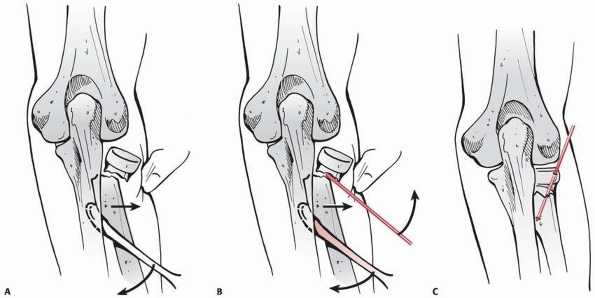
three types based on the location of the fracture line (Fig. 11-7).
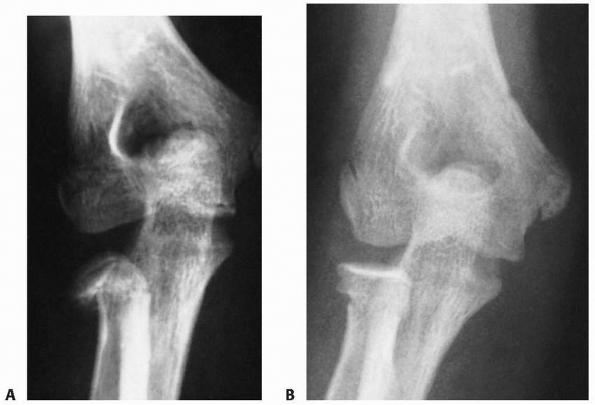
Fractures associated with an elbow dislocation are subdivided into two
types. The first is based on the original concept proposed by Jeffrey42 that the fracture occurs during spontaneous reduction (Fig. 11-8A). In this case, the radial head lies proximal to the posterior aspect of the joint. The second is based on Newman’s70
concept that the fracture and displacement occur during the process of
dislocation of the elbow. In this type, the radial head lies distal to
the anterior portion of the joint (see Fig. 11-8B).
Most radial head fractures in children described in the literature have
been Salter-Harris type IV injuries containing portions of both the
epiphysis and metaphysis, and there is no need to further subclassify
them.
 |
|
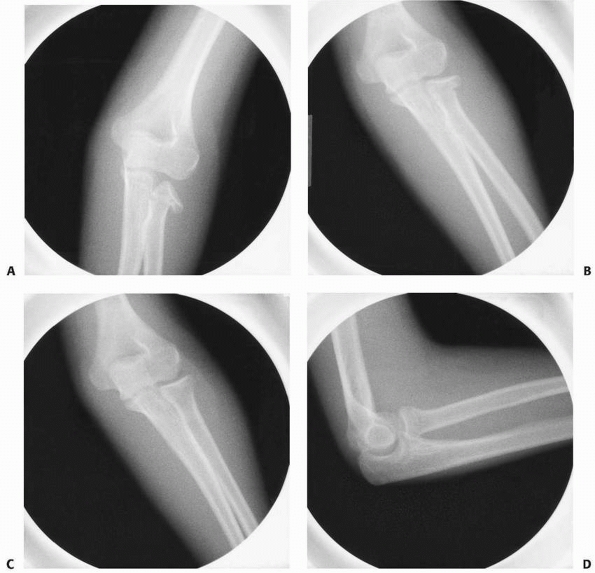
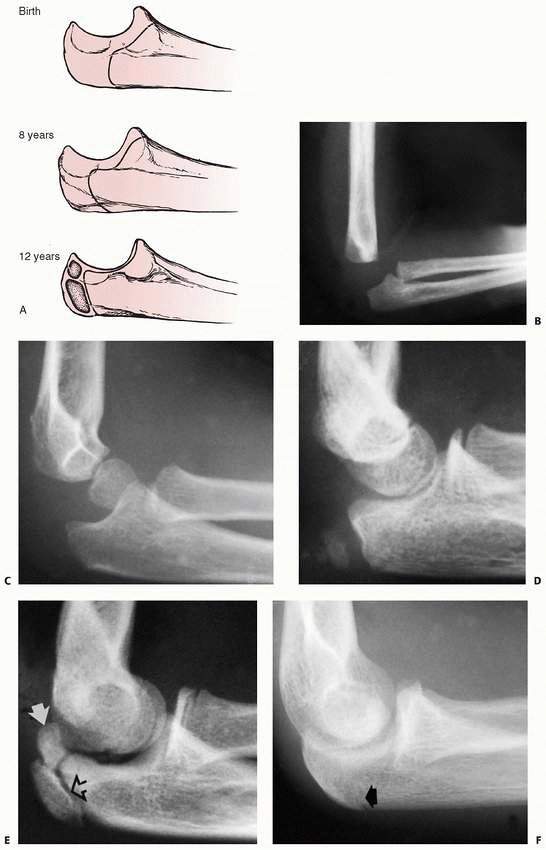
FIGURE 11-4 A,B. AP and lateral radiographs demonstrating a radial neck fracture in a patient with a nonossified proximal radial epiphysis. C. Arthrogram prior to reduction demonstrating location/displacement of nonossified proximal radial epiphysis. D-F.
Arthrogram/radiographs after reduction with intramedullary technique. (From Javed A, Guichet J.M. Arthrography for reduction of a fracture of the radial neck in a child with a nonossified radial epiphysis. J Bone Joint Surg Br 2001;83-B:542-543, with permission.) |
subgroups: angular and torsional. An angular fracture of the radial
neck may be associated with a proximal ulnar fracture. This association
is recognized as a Monteggia variant.
 |
|
FIGURE 11-5 A.
Radiocapitellar view. Center of x-ray beam is directed at 45 degrees to separate proximal radius and ulna on the radiograph. (Reprinted from Long BW. Orthopaedic Radiography. Philadelphia: W.B. Saunders, 1995:152, with permission.) B. Angular stress deformity: anterior angulation of the radial head and neck in a 12-year-old baseball pitcher. There is evidence of some disruption of the normal growth of the anterior portion of the physis (black arrow). The capitellum also shows radiographic signs of osteochondritis dissecans (white arrow). (Courtesy of Kenneth P. Butters, MD.) |
 |
|
FIGURE 11-6 The radiocapitellar view. A.
Radiographs of a 13-year-old female who sustained a radial neck fracture associated with an elbow dislocation. There is ectopic bone formation (arrows). In this view, it is difficult to tell the exact location of the ectopic bone. B. The radiocapitellar view separates the radial head from the coronoid process and shows that the ectopic bone is from the coronoid process (arrows) and not the radial neck. |
|
TABLE 11-1 Classification of Fractures Involving the Proximal Radius
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|
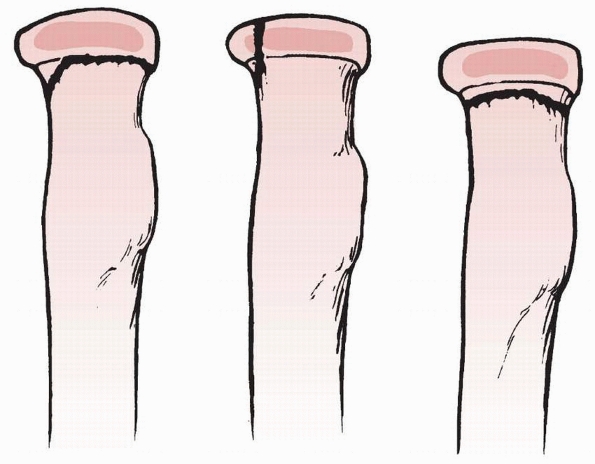
FIGURE 11-7 Types of valgus injuries. Left. Type A: Salter-Harris type I or II physeal injury. Center. Type B: Salter-Harris type IV injury. Right. Type C: Total metaphyseal fracture pattern.
|
osteochondritis of the radial head and physeal injuries of the neck
that produce angular deformities.
is applied to the radial head and is secondarily transmitted to the
radial neck, which fractures because it is metaphyseal bone with a
thinner cortex. Angulation, rotation, translocation, or complete
separation of the radial head from the neck can displace the radial
head. This displacement of the radial head produces an incongruity of
the proximal radioulnar joint, which is the major cause of dysfunction.
For displaced radial head fractures, the treatment goal is to reduce
the proximal radioulnar joint to its normal congruous position and
restore range of motion.
compresses the radiocapitellar joint. The cartilaginous head absorbs
the force and transmits it to the weaker physis or metaphysis of the
neck.117 These fractures characteristically produce an angular deformity of the head with the neck (see Fig. 11-9A).
The direction of angulation depends on whether the forearm is in a
supinated, neutral, or pronated position at the time of the fall. Vostal117
showed that in neutral, the pressure is concentrated on the lateral
portion of the head and neck. In supination, the pressure is
concentrated anteriorly, and in pronation it is concentrated
posteriorly.
of a type I Monteggia lesion. An avulsion fracture of the medial epicondylar apophysis also may occur.13 In Fowles and Kassab’s26 series of patients with radial neck fractures, more than 61% had one of these associated injuries.
 |
|
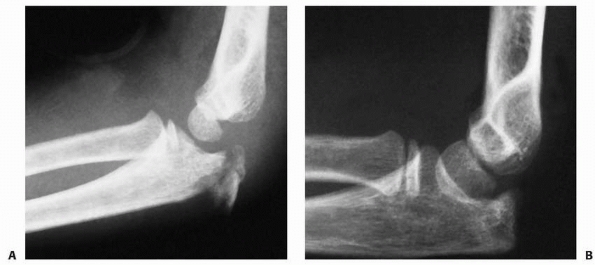
FIGURE 11-8 Dislocation fracture patterns. A.
Type D: The radial neck is fractured during the process of reduction by the capitellum pressing against the distal lip of the radial head.125 B. Type E: The radial neck is fractured during the process of dislocation by the capitellum pressing against the proximal lip of the radial head.98 C. Radiographs of a radial head that was fractured during the reduction of the dislocation (type D). The radial head (solid arrow) lies posterior to the distal humerus, and the distal portion of the neck (open arrow) is anterior. (Courtesy of Richard E. King, MD.) D. Radiograph of the dislocated elbow in which the fracture of the radial neck occurred during the process of dislocation (type E). |
found that the degree of cubitus valgus in patients who sustained this
injury was greater than in patients with other types of elbow fractures.
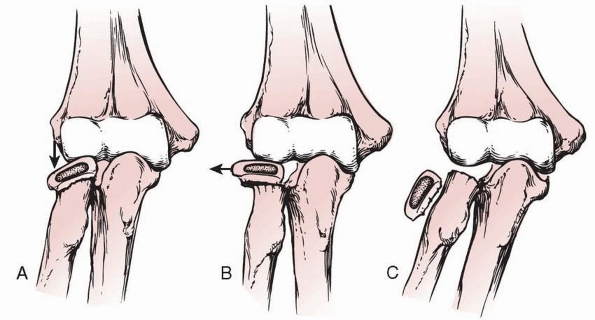
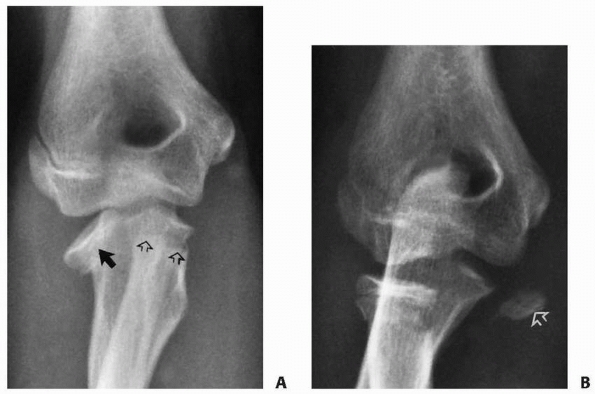
In the first two types, the fracture line involves the physis. Type A
represents either a Salter-Harris type I or II physeal injury. In a
Salter-Harris type II injury, the metaphyseal fragment is triangular
and lies on the compression side. In type B fractures, the fracture
line courses vertically through the metaphysis, physis, and epiphysis
to produce
a Salter-Harris type IV fracture pattern (see Fig. 11-11).
This is the only fracture type that involves the articular surface of
the radial head. In type C fractures, the fracture line lies completely
within the metaphysis (Fig. 11-12), and the
fracture can be transverse or oblique. Type B fractures are rare. The
incidences of types A and C fractures are approximately equal.103
|
TABLE 11-2 Fractures of the Radial Head and Neck: Proposed Mechanisms in Children
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
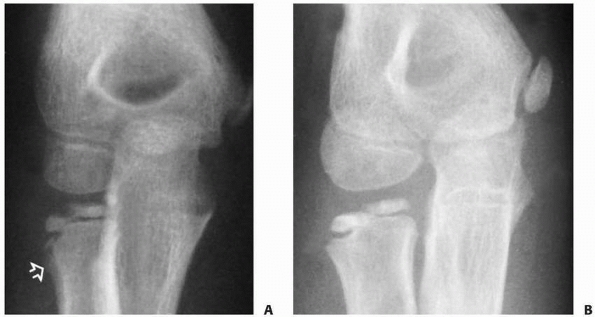
can vary from minimal angulation to complete separation of the radial
head from the neck (Fig. 11-13). With minimal
angulation, the congruity of the proximal radioulnar joint is usually
retained. If the radial head is displaced in relation to the radial
neck, the congruity of the proximal radioulnar joint is lost, producing
the cam effect. Completely displaced fractures are often associated
with more severe injuries.
 |
|
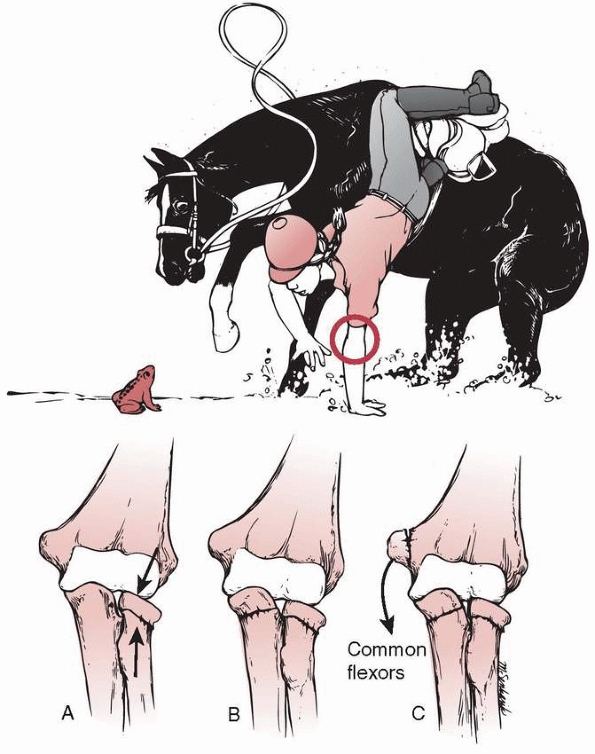
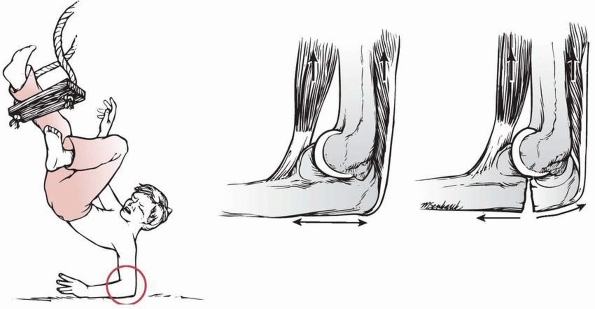
FIGURE 11-9
The most common mechanism of radial neck fractures involves a fall on the outstretched arm. This produces an angular deformity of the neck (A). Further valgus forces can produce a greenstick fracture of the olecranon (B) or an avulsion of the medial epicondylar apophysis (C). (Redrawn with permission from Jeffery CC. Fracture of the head of the radius in children. J Bone Joint Surg Br 1950;32:314-324.) |
 |
|
FIGURE 11-10
Associated fractures of valgus stress. Anteroposterior view of a fracture of the radial neck associated with a greenstick fracture of the olecranon (arrows). |
proximal migration of the distal fragment tends to be ulnarward because of muscle pull by the supinator and biceps muscles (Fig. 11-14). Patterson75
attempted to counteract these forces in his manipulative technique
(“Patterson’s Manipulative Technique”). When there is a strong valgus
component, the proximal portion of the distal fragment of the radius
can get locked medial to the coronoid process, making a closed
reduction almost impossible.24,56
 |
|
FIGURE 11-11 Valgus (type B) injury. A.
Three weeks after the initial injury, there was evidence of distal migration of this Salter-Harris type IV fracture fragment. Periosteal new bone formation has already developed along the distal metaphyseal fragment (arrow). B. Six months after the initial injury, there is evidence of an osseous bridge formation between the metaphysis and the epiphysis. Subsequently, the patient had secondary degenerative arthritis with loss of elbow motion and forearm rotation. |
associated with elbow dislocation, the head fragment is totally
displaced from the neck.5,13,27,42,70,118
The proposed mechanism is a fall on the hand with the elbow flexed,
which causes a momentary partial dislocation of the elbow and forces
the radial head posterior to the capitellum.
suggested that displacement and fracture occurred during spontaneous
reduction of the transiently dislocated elbow. During this reduction
process, the capitellum applies a proximal force to the distal lip of
the radial head, causing it to separate as the forearm and distal
radius are reduced distally (see Fig. 11-8A).
The radial neck and olecranon return to their anatomic locations while
the radial head remains in the posterior aspect of the joint.118
 |
|
FIGURE 11-12 Valgus type C injury. The fracture line is totally metaphyseal and oblique (arrows).
|
type of radial head fracture in which the fracture occurs during the
process of dislocation. In this case, the capitellum applies a distally
directed force to the proximal lip of the radial head as the elbow is
dislocated (see Fig. 11-8B). The elbow may
remain dislocated with the radial head lying anterior and often
parallel to the long axis of the neck fragment. If the dislocation is
reduced, either by manipulation or spontaneously, the radial head lies
free in the anterior portion of the elbow joint.5,70,114
disruption or deformity of the neck while the head remains congruous
within the proximal radioulnar joint. Treatment of these fractures is
manipulation of the distal neck fragment to align it with the head.
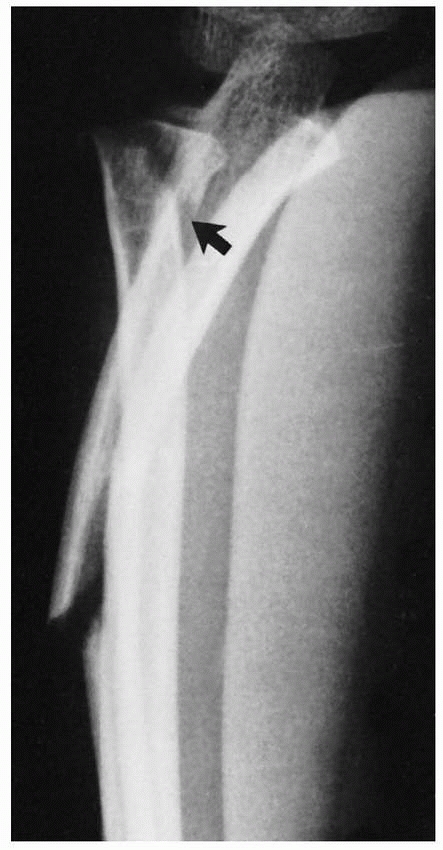
force is applied across the extended elbow, resulting in a greenstick
fracture of the olecranon or proximal ulna and a lateral dislocation of
the radial head.125
Occasionally, however, the failure occurs at the radial neck (Monteggia
III equivalent) and the radial neck displaces laterally, leaving the
radial head and proximal neck fragment in anatomic position under the
orbicular ligament (Fig. 11-15).72
 |
|
FIGURE 11-13 Displacement patterns. The radial head can be angulated (A), translated (B), or completely displaced (C).
|
 |
|
FIGURE 11-14 A.
Forces producing displacement. Once the stabilizing effect of the radial head is lost, the distal fragment (radial neck and proximal shaft) is displaced ulnarward and proximally by the unopposed biceps and supinator muscles (arrows). (Redrawn with permission from Patterson RF. Treatment of displaced transverse fractures of the neck of the radius in children. J Bone Joint Surg 1934;16:695.) B. Radiograph showing proximal and medial (ulnar) displacement of distal neck fragment (arrow). (From Wilkins KE, ed. Operative management of upper extremity fractures in children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:55.) |
children before ossification of the proximal radial epiphysis. Both
reports of this injury are in the European literature,31,39
and in both, the initial rotational force was supination. Reduction was
achieved by pronation of the forearm. Diagnosis of these injuries is
difficult and may require arthrography or an examination under general
anesthesia. This injury should be differentiated from the more common
subluxation of the radial head (pulled elbow syndrome), in which the
forearm usually is held in pronation with resistance to supination. In
addition, on radiography there usually are no signs of hemarthrosis, as
is seen in the torsional fractures.
 |
|
FIGURE 11-15 Angular forces. This 8-year-old sustained a type III Monteggia equivalent in which the radial neck fractured (arrow), leaving the radial head reduced proximally. (Courtesy of Ruben D. Pechero, MD.)
|
stress, both longitudinal and rotational, on either the head or the
proximal radial physis. These injuries are usually the result of
athletic activity in which the upper extremity is required to perform
repetitive motions. Repetitive stresses disrupt growth of either the
neck or the head with eventual deformity. A true stress fracture is not
present.
has produced a number of unique injuries in children related to
repetitive stress applied to growth centers. This is especially true in
the immature elbow. Most injuries are related to throwing sports,
primarily Little League baseball. Most of this “Little League
pathology” involves tension injuries on the medial epicondyle. In some
athletes, however, the lateral side is involved as well because of the
repetitive compressive forces applied to the capitellum and radial head
and neck. Athletes involved in sports requiring upper extremity
weightbearing, such as gymnastics or wrestling, are also at risk. In
the radial head, lytic lesions similar to osteochondritis dissecans may
occur (Figs. 11-16 and 11-17).22,112,123
Chronic compressive loading may cause an osteochondrosis of the
proximal radial epiphysis, with radiographic signs of decreased size of
the ossified epiphysis, increased radiographic opacity, and later
fragmentation. If the stress forces are transmitted to the radial neck,
the anterior portion of the physis may be injured, producing an angular
deformity of the radial neck (see Fig. 11-5).21
 |
|
FIGURE 11-16
Osteochondritis dissecans. Radiograph of this 11-year-old Little League pitcher’s elbow shows fragmentation of the subchondral surfaces of the radial head. These changes and the accelerated bone age are evidence of overuse. |
 |
|
FIGURE 11-17 Elevated anterior and posterior fat pads. A.
Illustration (adapted with permission from Skaggs DL, Mirazayan R. The posterior fat pad sign in association with occult fracture of the elbow in children. J Bone Surg AM 1999;81:1429-1433). B. White arrow: posterior fat pad sign. Black arrow: anterior fat pad sign. |
-
Immobilization with no manipulation
-
Manipulative closed reduction
-
Percutaneous pin reduction
-
Intramedullary pin reduction
-
Open reduction with or without internal fixation
-
Excision of either the entire head or a small head fragment
of treatment, including the degree of angulation and displacement, the
association of other injuries, the age of the patient, and the time
elapsed since the injury.
treatment in determining the final result. A poor result is more likely
if the fracture is associated with other injuries, such as an elbow
dislocation, a fracture of the olecranon, or avulsion of the medial
epicondylar apophysis.26,92 The magnitude of force to the elbow is a major factor in determining the quality of the result.52,103
reported that the number of good results decreased if the initial
angulation exceeded 30 degrees or the amount of displacement exceeded 3
mm. Newman70 found that more than 4
mm of initial displacement increased the frequency of poor results and
the risk of synostosis with the proximal ulna.
believed that in older children, only 15 degrees of angulation should
be accepted without attempting manipulation. The spontaneous correction
that can be expected to occur with growth in younger children is
approximately 10 degrees. Some clinicians accept up to 30 degrees of
residual angulation,52,60,70,84,114 whereas others believe that up to 45 degrees of residual angulation can yield a satisfactory result.8,15,71,116
The cam effect will limit supination and pronation if there is
significant displacement of the proximal fragment. However, adequate
remodeling with a functional range of motion can occur with as much as
40% displacement (Fig. 11-18) in a young child.
injury; the later the surgical intervention, the poorer the result.
McBride and Monnet59 described three
patients in whom an osteotomy of the neck was done for residual
angulation 3 to 5 weeks after injury. All had further loss of range of
motion because of the development of a proximal cross union. Blount8
set a limit of 5 days, after which surgical intervention is more likely
to produce a poorer result than if the fracture is left untreated.
result than an open reduction. This may be true because injuries that
can be managed by closed methods are the result of less severe trauma
than
those requiring open reduction. The poor results in those managed with
open methods may be due just as much to the associated soft-tissue
injuries as to the surgical insult.
 |
|
FIGURE 11-18 Translocation remodeling. A.
Injury film of a 9-year-old who had 60 degrees of supination and pronation by clinical examination with local anesthesia into the elbow joint. Because range of motion was functional, the position was accepted. B. Two months after fracture, there was almost complete remodeling of the translocation. The patient’s forearm rotation was 75 degrees in both directions. (Courtesy of Earl A. Stanley Jr, MD.) |
Thus, at least one in five or six children can be expected to have a
poor result despite adequate treatment. It is wise to counsel the
parents before beginning treatment if poor prognostic factors are
present. Very little improvement in motion occurs after 6 months.
Steinberg et al.103 found that range of motion in their patients at 6 months was almost equal to that when the patients were examined years later.
Immobilization is the treatment of choice for fractures in younger
children in which the angulation of the radial head is less than 20 to
30 degrees. A collar and cuff, a posterior splint, or a light long-arm
cast is sufficient to provide comfort and protection from further
injury. Aspiration of the intra-articular hematoma may decrease pain.
of Angulation). Although acceptable results can be obtained with
angulation of up to 45 degrees, closed reduction should be attempted
for fractures with more than 30 degrees of angulation. A closed
reduction is usually satisfactory for fractures with angulation up to
60 degrees. The chance of achieving a satisfactory closed reduction is
much less when the initial angulation exceeds 60 degrees.
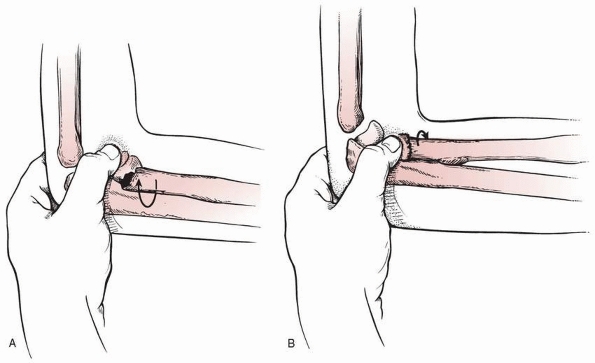
General or regional anesthesia can provide adequate relaxation. The
orbicular ligament should be intact to stabilize the proximal radial
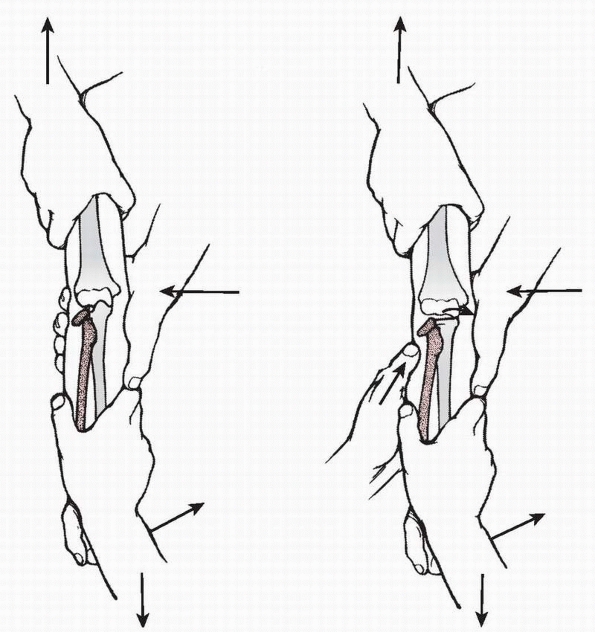
head fragment.60 In Patterson’s75 technique, an assistant grasps the arm proximal to the elbow joint with one hand (Fig. 11-19)
and places the other hand medially over the distal humerus to provide a
medial fulcrum for the varus stress applied across the elbow. The
surgeon applies distal traction with the forearm supinated to relax the
supinators and biceps. A varus force is then placed on the elbow to
overcome the ulnar deviation of the distal fragment so that it can be
aligned with the proximal fragment. This varus force also helps open up
the lateral side of the joint, which facilitates manipulation of the
head fragment.
muscle, supination may not be the best position for manipulation of the
head fragment. Jeffrey42 pointed out that the tilt of the radial
head can be anterior or posterior depending on the position of the
forearm at the time of injury. With this degree of rotation, the
prominent tilt of the proximal fragment can be felt laterally. The
direction of maximal tilt can be confirmed by radiograph. The best
position for reduction is the degree of rotation that places the radial
head most prominent laterally. If the x-ray beam is perpendicular to
the head in maximal tilt, it casts an oblong or rectangular shadow; if
not, the shadow is oval or almost circular.42
With a varus force applied across the extended elbow, the maximal tilt
directed laterally, and the elbow in varus, the radial head can be
reduced with the pressure of a finger (see Fig. 11-19, right).
 |
|
FIGURE 11-19 Patterson’s manipulative technique. Left.
An assistant grabs the arm proximally with one hand placed medially against the distal humerus. The surgeon applies distal traction with the forearm supinated and pulls the forearm into varus. Right. Digital pressure applied directly over the tilted radial head completes the reduction. (Redrawn with permission from Patterson RF. Treatment of displaced transverse fractures of the neck of the radius in children. J Bone Joint Surg 1934;16:696-698.) |
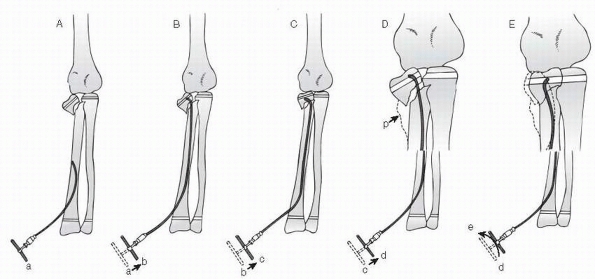
described a two-person technique for the reduction of severely
displaced radial neck fractures. This technique is performed with the
elbow in extension and the patient under general anesthesia. An
assistant uses both thumbs to place a laterally directed force on the
proximal radial shaft while the surgeon applies a varus stress to the
elbow. Simultaneously, the surgeon uses his other thumb to apply a
reduction force directly to the radial head (Fig. 11-20).
proposed another technique in which the elbow is manipulated in the
flexed position. The surgeon presses his or her thumb against the
anterior surface of the radial head with the forearm in pronation.
reduction because it is the forearm motion most often restricted after
fracture.120 Some have recommended
supination because they believe it is easier for the patient to regain
active pronation than active supination during rehabilitation. Whether
pronation or supination is chosen, they recommend 90 degrees of flexion
for the elbow. Fluoroscopy can determine whether pronation or
supination results in the optimal reduction of the fracture.
completely displaced proximally, with the head perpendicular to the
shaft of the radius. In four reports since 1960, closed reduction,27,122,124 resulted in rotation of the proximal fragment180
degrees so that the articular surface of the head (concavity) was
facing the fracture surface of the radial neck. Open reduction is
needed to reduce the fragment, with a high risk of complications.
redisplacement can occur, especially if the initial tilt was more than
60 degrees.20,43
Fractures with more than 90 degrees of angulation, especially those in
which the head fragment is lying free in the joint, are almost
impossible to reduce by closed methods.
 |
|
FIGURE 11-20
Neher and Torch reduction technique. (From Neher CG, Torch MA. New reduction technique for severely displaced pediatric radial neck fractures. J Pediatr Orthop 2003;23:626-628, with permission.) |
reduction with an image intensifier is a popular method of
satisfactorily reducing moderately to severely displaced fractures.3,6,19,78,102 Various authors have used an awl, a Steinmann pin,89 a periosteal elevator,28 or a double-pointed “bident”3
that in theory controls rotation better. Some authors describe using
the pin to directly push the displaced radial head fragment back into
position,61 while others describe a pin leverage technique,78,102 inserting the pin into the fracture site and then leveraging the radial head against the capitellum to reduce the fracture (Fig. 11-21). Pesudo et al.,78
in their series of 22 displaced radial neck fractures, found that the
results after percutaneous pin reduction were superior to those after
open reduction.
described driving the pin used to reduce the radial head across the
fracture site to stabilize it. The pin is removed and motion is allowed
after 3 weeks.
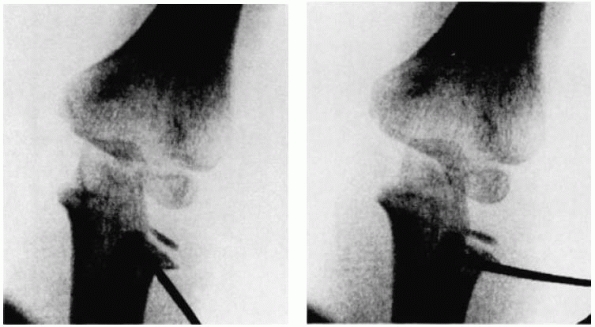
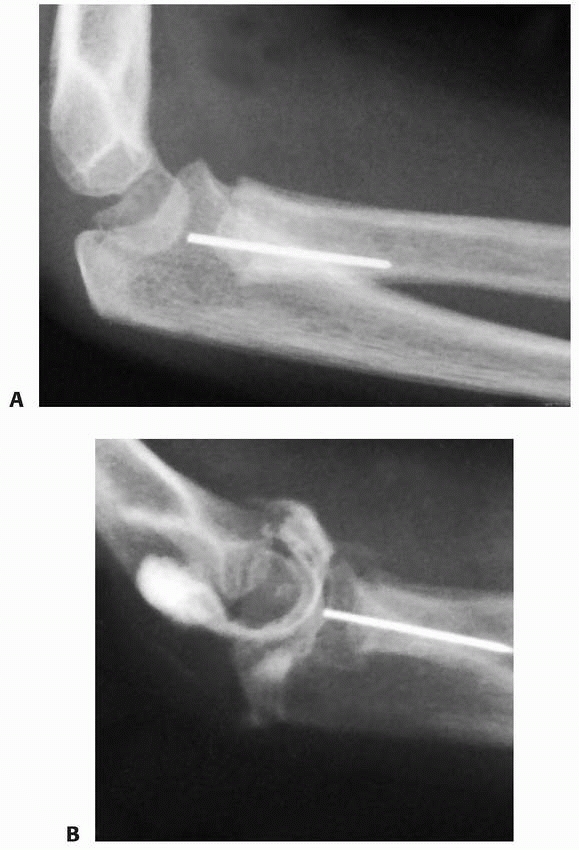
proposed reducing severely tilted radial neck fractures with an
intramedullary wire passed from the distal metaphysis. A report 13
years later61 demonstrated the
effectiveness of this technique. A wire is inserted into the medullary
canal through an entrance hole in the distal metaphysis (Fig. 11-22).
Once the wire reaches the fracture site, the angulation at the tip
enables it to engage the proximal fracture site at the neck. Once
engaged, the wire is twisted to reduce the head and neck fragment. This
technique has produced results superior to open reduction with fewer
complications.32,98
have reported good to excellent results using the intramedullary pin
reduction technique for severely displaced radial neck fractures.
Schmittenbecher et al.96 reported
good to excellent results in 18 (78%) of 23 fractures after reduction
and fixation with 2-mm elastic intramedullary nails. Other authors have
recommended using Kirschner-wires for the intramedullary technique. One
challenge with this technique is that oftentimes Kirschnerwires are not
long enough to allow for optimal use with the intramedullary reduction
method. However, the pointed tip of the Kirschner-wire is helpful in
engaging the displaced radial neck fragment during this reduction
maneuver. Nawabi et al.67 reported
the use of a smooth 1.8-mm Ilizarov wire in two children. The added
length of the Ilizarov wire allowed sufficient wire to remain outside
the skin to simplify the reduction maneuver. When using a Kirschner
wire or Ilizarov wire, it is important to contour the distal 3 to 4 mm
with a relatively sharp bend to allow for easier capture of the
displaced radial head fragment. It remains controversial as to whether
or not the intramedullary implant needs to remain in place after the
fracture reduction.
Fluoroscopy in an AP projection is used to determine the forearm
rotation that exposes the maximum amount of deformity of the fracture,
and the level of the bicipital tuberosity of the proximal radius is
marked. A 1-cm dorsal skin incision is made at that level just lateral
to the subcutaneous border of the ulna. A periosteal elevator is gently
inserted between the ulna and the radius,
with
care not to disrupt the periosteum of the radius or the ulna. The
radial shaft is usually much more ulnarly displaced than expected, and
the radial nerve is lateral to the radius at this level. While
counterpressure is applied against the radial head, the distal fragment
of the radius is levered away from the ulna. An assistant can aid in
this maneuver by gently applying traction and rotating the forearm back
and forth to disimpact the fracture fragments. If necessary to correct
angulation, a percutaneous Kirschner-wire can be inserted into the
fracture site, parallel to the radial head, to lever the physis
perpendicular to the axis of the radius.
 |
|
FIGURE 11-21
Radiographs demonstrating the pin leverage technique for reduction of a radial neck fracture. (From Steele JA, Graham HK. Angulated radial neck fractures in children: a prospective study of percutaneous reduction. J Bone Joint Surg Br 1992;74:760-764, with permission.) |
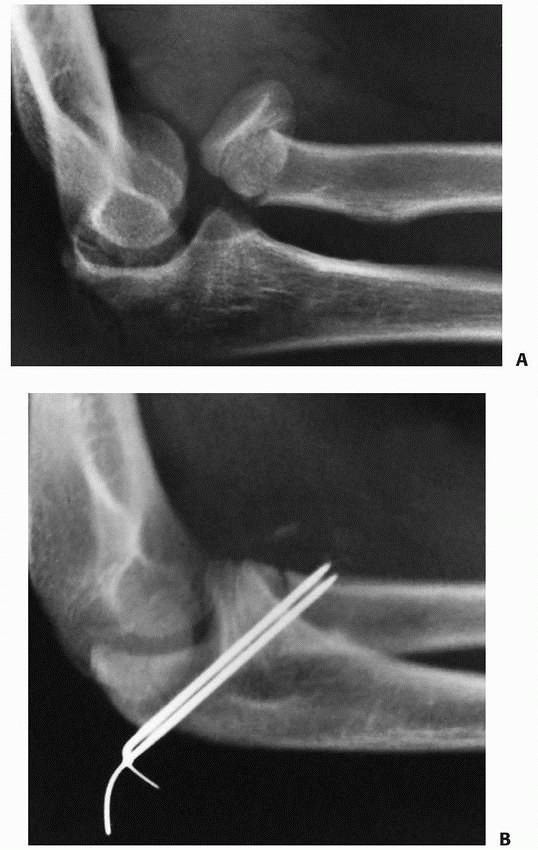
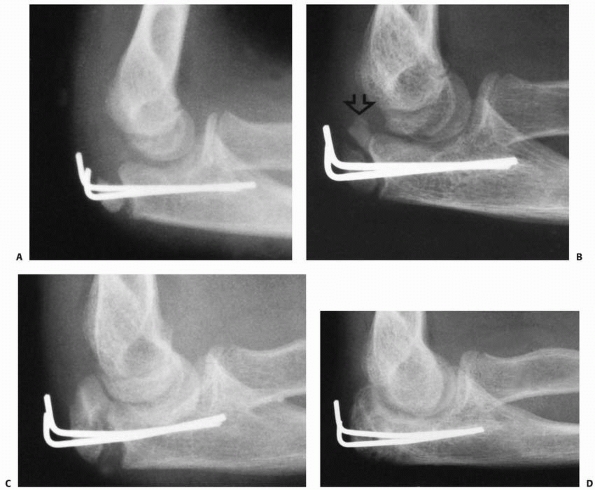
Kirschner-wire is inserted to provide fracture fixation. The wire is
removed 3 weeks after surgery (Figs. 11-23 and 11-24).
 |
|
FIGURE 11-22 Intramedullary pin reduction. A. The insertion point for the curved flexible pin is in the metaphysis. B. The curved end of the rod passes in the shaft and engages the proximal fragment. C. Manipulation of the rod disimpacts the fracture. D,E.
Once disimpacted, the head fragment is rotated into position with the intramedullary rod. (From Metaizeau JP, Lascombes P, Lemelle JL, et al. Reduction and fixation of displaced radial neck fractures by closed intramedullary pinning. J Pediatr Orthop 1993;13:355-356; with permission.) |
45 degrees probably produces as good a result as trying to achieve a
perfect reduction surgically. An acceptable closed reduction can
produce a better result than an anatomically perfect open surgical
reduction (Table 11-3).
series42,43,78,110
and reported 49% good results after operative treatment compared to 25%
after nonoperative treatment. None of these authors used percutaneous
pin reduction. The results of moderately displaced fractures treated
operatively were equal to the results of those treated nonoperatively.
 |
|
FIGURE 11-23 Wallace radial head reduction technique. A. A periosteal elevator is used to lever the distal fragment laterally while the thumb pushes the proximal fragment medially. B. Kirschner-wires are used to assist the reduction if necessary. C. The position of the reduction can be fixed with an oblique Kirschner-wire.
|
 |
|
FIGURE 11-24 A. Radial neck fracture angulated 45 degrees in a 14-year-old female. B. Radiograph after closed reduction using thumb pressure on the radial head. C. Final reduction after manipulation of the distal fragment with an elevator using the Wallace technique. D. Lateral view of the elbow after reduction.
|
|
TABLE 11-3 Acceptable Reduction
|
||
|---|---|---|
|
results are usually better with surgical intervention. Some authors
have shown that a completely separated radial head remains viable if
surgically replaced as late as 48 hours after injury.30,46
because interposition of the capsule or annular ligament between the
head and neck blocks reduction.117 Strong et al.105
described an unusual fracture pattern in which the radial head was
trapped by the orbicular ligament. They found that these fractures were
irreducible by closed methods and required open reduction.
 |
|
FIGURE 11-25 Transcapitellar pin in a 4-year-old with a completely displaced fracture of the radial neck. A. Three weeks after injury, when the pin was removed, it had fractured and a portion remained in the proximal radius. B.
An arthrogram revealed that the fractured end was at the joint surface of the radial head. The piece was left in place, with subsequent resumption of normal elbow motion. |
have recommended inserting a small wire through the capitellum across
the radial head and into the neck to fix radial head fractures, but
this technique has a high incidence of complications.26,70,97,120 Even in a long-arm cast, the elbow joint has slight motion, which can cause the pin to fatigue and break (Fig. 11-25).
The retrieval of the remaining portion of the pin from the proximal
radius is almost impossible without imposing considerable trauma. Even
if the pin does not break, the motion of the pin may erode the joint
surface and fragment the radial head.70,120
neck after open reduction include intramedullary bone pegs, direct pin
insertion through the head by way of an olecranon osteotomy,55 or with a forked plate.51
 |
|
FIGURE 11-26 Oblique pin. A. Displaced fracture of the radial neck in a 10-year-old. B.
A closed reduction was performed, and to stabilize the head fragment, two pins were placed percutaneously and obliquely across the fracture site from proximal to distal. If open reduction and pinning are done, the preferred alignment is obliquely across the fracture site from distal to proximal. (From Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:57, with permission.) |
found that patients without internal fixation had more good results
than those with internal fixation. Use of internal fixation does not
guarantee that the fragment will not slip. Newman70 described two patients in whom the head slipped postoperatively despite Kirschnerwire fixation.
demonstrated that with the forearm in pronation, the posterior
interosseous nerve displaces ulnarward, out of the way of the surgical
dissection. They also recommended that the patient be prone during
exploration of the proximal radius to help keep the forearm pronated.
 |
|
FIGURE 11-27 Miniscrew fixation. A,B.
Anteroposterior and lateral views of the elbow of a 6-year-old male in whom the head fragment lies posterior to the capitellum (arrows). C. At the time of open reduction a Salter-Harris type III fracture through the epiphysis and proximal physis was apparent. The fragment involved 60% of the head diameter and had soft tissue attached. D. A screw placed through the epiphysis fixed the reduction. E. Six months after surgery, an arthrogram showed maintenance of the architectural structure of the medial head after screw removal. The patient had 60 degrees of supination and pronation. (From Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:58, with permission.) |
marginal fragment can be safely removed and the remaining large portion
of the head reduced without internal fixation.120
reported good to excellent results with the use of absorbable
polyglycolide pins in patients older than 13 years of age. Transient
local abacterial tissue reaction occurred but did not lead to any
long-term negative effects. There was no comment on the effect on the
physis. To fix a large displaced head fragment in a Salter-Harris type
III or IV fracture, a transepiphyseal screw is useful (Fig. 11-27).
|
TABLE 11-4 Treatment of Radial Head Fractures
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
fragment was popular in the 1920s and 1930s, but reported results have
been uniformly poor.20,39,43 Cubitus valgus and radial deviation at the wrist are common sequelae. The procedure is contraindicated in a growing child.
Although they may appear reasonably minor both radiographically and
clinically, we initially emphasize to the parents that some loss of
motion may occur even with an anatomic reduction. The problem is
usually a loss of range of motion in supination and pronation. Little
pain or loss of upper extremity function occurs despite the residual
loss of forearm rotation.
 |
|
FIGURE 11-28 Flexion-pronation (Israeli) reduction technique.45 A. Radiograph of the best reduction obtained by the Patterson75 method. B. Position of the radial head after the flexion-pronation method. (Courtesy of Gerald R. Williams, MD.)
|
attempt a manipulative closed reduction. In adolescent patients, we may
attempt a closed reduction for less than 30 degrees in an attempt to
normalize the anatomy as much as possible. If there is a great amount
of pain or resistance to pronation and supination, we aspirate the
elbow after a sterile preparation and frequently inject 2 to 3 mL of 1%
lidocaine,18 but a general
anesthetic is preferable for full relaxation. We prefer the Israeli
technique for simple, moderately displaced radial head fractures (Fig. 11-28).45
The important aspect is to ensure that the elbow is flexed at 90
degrees for the manipulation. Usually there is resistance to pronation (Fig. 11-29). With thumb pressure applied to the radial head, the opposite hand forces the forearm into full pronation (see Fig. 11-29). After reduction, the range of motion should be at least 60 degrees of supination and pronation (see Fig. 11-28B).
If the range of supination and pronation is adequate, we accept the
reduction regardless of the radiograph appearance. We attempt closed
reduction first even with completely displaced radial neck fractures.
Occasionally a surprisingly satisfactory reduction can be obtained (Fig. 11-30).
found that he could reduce the fracture by wrapping the extremity
tightly from distal to proximal with an elastic Esmarch bandage (Fig. 11-31).
fractures, we attempt a reduction using the percutaneous pin reduction technique (Fig. 11-32).
A good image intensifier is essential. We have found that a
single-point awl or the blunt end of a Steinmann pin is adequate. If
the radial head is small or soft, we use a small Craig biopsy needle or
the blunt end of the Steinmann pin to prevent penetration of the radial
head with a sharp end of a Steinmann pin.
 |
|
FIGURE 11-29 Flexion-pronation (Israeli) reduction technique.45 A.
With the elbow in 90 degrees of flexion, the thumb stabilizes the displaced radial head. Usually the distal radius is in a position of supination. The forearm is pronated to swing the shaft up into alignment with the neck (arrow). B. Movement is continued to full pronation for reduction (arrow) (see also Fig. 11-18). |
insert the pin as closely as possible to the lateral aspect of the
olecranon (see Fig. 11-32A). The direct push
technique is used initially, and if the radial head cannot be pushed
into a satisfactory position, the pin leverage technique is used as
described by Steele and Graham.102
Again, we accept 45 to 60 degrees of angulation as long as the
displacement is small and the patient has at least 50 to 60 degrees of
supination and pronation after reduction.
 |
|
FIGURE 11-30 Widely displaced fracture of the radial head in a 9-year-old female. A. The neck fragment (open arrows) was medial and the head fragment (closed arrow) remained within the orbicular ligament. B. Reduction was satisfactory using the flexion-pronation method. The small fragment medially (arrow)
is from the metaphysis. The patient resumed full rotation of the forearm after reduction. (From Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:55, with permission.) |
In some instances, this technique is used in conjunction with the
percutaneous pin technique. This combination is successful in obtaining
a satisfactory reduction in almost all cases.
without the need to open the fracture. One challenge clinically with
this technique is that the cut end of the pin often remains prominent
at the wrist.
 |
|
FIGURE 11-31 Elastic bandage wrap reduction. A. The final position achieved after manipulation by the Patterson75 method. B. Position of the radial head after applying an elastic bandage to exsanguinate the extremity.
|
 |
|
FIGURE 11-32 Percutaneous pin reduction. A.
Image intensification shows the awl inserted next to the olecranon and directed proximally toward the radial head fragment. This is to avoid injury to the posterior interosseous nerve. B. Totally displaced valgus injury. C. Position of the Steinmann pin during reduction. D. Appearance 2 months after surgery. The patient has 60 degrees of supination and pronation with full elbow extension and flexion. |
of motion is significant, we prefer an open reduction with as little
dissection as possible. We approach the fracture with the patient prone
and the forearm pronated. After making the skin incision, we dissect
between the anconeus and extensor carpi ulnaris muscles to reach the
orbicular ligament and reposition the head as gently as possible.
Usually, the head fragment is stable after reduction. If it is not, we
stabilize the reduction with a small pin placed obliquely through a
separate stab incision from distal to proximal across the fracture site.
significant supination or pronation forearm motion, we reduce the head
surgically, if reduction is not possible closed. However, we warn the
patient’s parents of the possibility for myositis ossificans and
proximal radioulnar synostosis.
extremity with the elbow in 90 degrees of flexion and the forearm in
slight pronation. The patient starts active motion in 1 to 3 weeks.
After a closed reduction, we start gradual active motion at 10 to 14
days, depending on the initial displacement and the degree of stability
of reduction. We prefer to use a long-arm cast. The bivalved cast is
useful as a splint during rehabilitation.
especially those associated with other fractures or a dislocation of
the elbow, range from the most common problem of loss of motion to rare
nerve injuries (Table 11-5). The most complete reviews of these complications are by Steinberg et al.103 and D’Souza et al.15
|
TABLE 11-5 Complications of Radial Head and Neck Fractures
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
joint congruity and fibrous adhesions. Loss of pronation is more common
than loss of supination. Flexion and extension are rarely significantly
limited. Enlargement of the radial head, a common sequela, can
contribute to the subsequent loss of elbow motion.30
forearm, radial head overgrowth is probably the most common sequela
(20% to 40%).15,114
The increased vascularity following the injury may stimulate epiphyseal
growth, but the mechanisms of overgrowth following fractures are poorly
understood. Radial head overgrowth usually does not compromise
functional results,19,43 but it may produce some crepitus or clicking with forearm rotation.15
that notching of the radial head in several patients was secondary to
scar tissue forming around the neck from the orbicular ligament. It did
not result in any functional deficit. Notching may be a normal variant
of radial head anatomy.
after fractures of the radial head and neck. This complication did not
appear to affect the overall results significantly, except in one
patient described by Fowles and Kassab,26 who had a severe cubitus valgus. Newman70 found that shortening of the radius was never more than 5 mm compared with the opposite uninjured side.
reported nine patients with radial neck nonunions, all of whom were
treated with open reduction after failed attempts at closed reduction.
These authors recommended observation of patients with radial neck
nonunions who have limited symptoms and a functional range of motion.
They suggested open reduction for displaced nonunions, patients with
limited range of motion, and patients with restricting pain.
reported the frequency to be 10% to 20% in their patients, 70% of whom
had open reductions. In patients with open reduction, the overall rate
of osteonecrosis was 25%. Jones and Esah43 and Newman70
found that patients with osteonecrosis had poor functional results. It
has been our experience, however, that revascularization can occur
without any significant functional loss. Only in those in whom a
residual functional deficit occurs is osteonecrosis considered a
problem (Fig. 11-34).
carrying angle often is 10 degrees more (increased cubitus valgus) than
on
the uninjured side.15,43 The increase in carrying angle appears to produce no functional deficit and no significant deformity.
 |
|
FIGURE 11-33 Nonunion. A.
Eight months after radial neck fracture in an 8.5-year-old female. Patient had mild aching pain, but no loss of motion. There was some suggestion of proximal subluxation of the distal radioulnar joint. B. Three months later, the fracture is united after long-arm cast immobilization and external electromagnetic stimulation. (Courtesy of Charles T. Price, MD.) |
 |
|
FIGURE 11-34
Osteonecrosis with nonunion in a radial head 1 year after open reduction. Both nonunion and osteonecrosis of the radial neck and head are present. Severe degenerative arthritis developed subsequently. (Courtesy of Richard E. King, MD.) |
and posterior interosseous nerve injury may occur as a direct result of
the fracture, but most injuries to the posterior interosseous nerves
are caused by surgical exploration15 or percutaneous pin reduction.5 These posterior interosseous nerve injuries usually are transient.
described three patients with volar forearm compartment syndrome after
minimally displaced or angulated fractures of the radial head. All
required volar fasciotomy.
but it can occur after closed reduction. Delayed treatment increases
the likelihood of this complication. All three patients described by
Gaston et al.30 had treatment initiated more than 5 days after injury.
noted that some myositis ossificans occurred in 32% of his patients. In
most, it was limited to the supinator muscle. If ossification was more
extensive and was associated with a synostosis, the results were poor.
 |
|
FIGURE 11-35 Radioulnar synostosis. A.
Surgical intervention with wire fixation was necessary for a satisfactory reduction in this patient who had a totally displaced radial neck fracture. B. Six weeks after surgery, there was evidence of a proximal radioulnar synostosis. C. Radiograph taken 6 months after reduction shows a solid synostosis with anterior displacement of the proximal radius. (Courtesy of R. E. King, MD.) |
reported a rare case of hematogenous osteomyelitis after a closed
fracture of the radial neck. The diagnosis was delayed despite the fact
that the child had fever and continuous pain after the fracture.
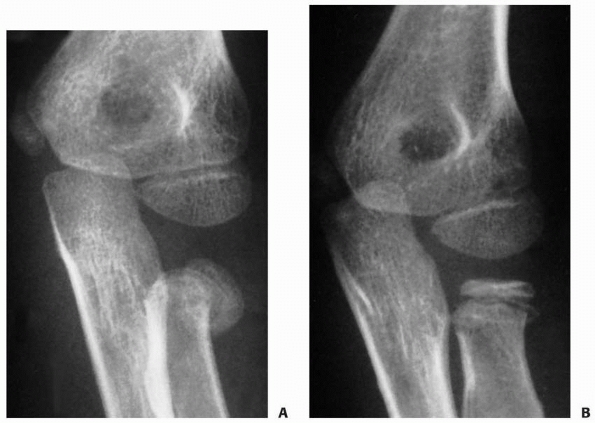
radial fracture in a young child often results in an angulated radial
neck with subsequent incongruity of both the proximal radioulnar joint
and the radiocapitellar joint (Fig. 11-36). Partial physeal arrest also can create this angulation (see Fig. 11-5).
incongruity of the radiocapitellar joint, often results in erosion of
the articular surface of the capitellum, with subsequent degenerative
joint disease. In the English literature, there is little information
about using osteotomies of the radial neck to correct this deformity.
are less favorable than those after closed reduction. However,
fractures requiring open reduction are usually the result of a more
severe injury. Closed reductions with angulations of up to 45 degrees
produce clinical results as good as those with a more anatomic
reduction after operation. The surgeon should warn the patient’s
parents of the likelihood of residual loss of motion after open
reduction. Whenever possible, internal fixation should be avoided.
This quote from Poland’s 1898 textbook on epiphyseal fractures is still
true. Few fractures of the ulnar apophysis are described in the English
literature.34,80,95,101 In addition to acute injuries in children, some have been described in young adults with open physes.47,76,100,111 In the French literature, Bracq10
described 10 patients in whom the fracture extended distal and parallel
to the apophyseal line and then crossed it at the articular surface.
Most reports of apophyseal olecranon fractures describe patients with
osteogenesis imperfecta, who seem predisposed to this injury.
the metaphysis of the proximal ulna extends only to the midportion of
the semilunar notch. At this age, the leading edge of the metaphysis is
usually perpendicular to the long axis of the olecranon (Fig. 11-37A,B).
As ossification progresses, the proximal border of the metaphysis
becomes more oblique. The anterior margin extends proximally and to
three fourths of the width of the semilunar notch by 6 years of age. At
this age, the physis extends distally to include the coronoid process
(see Fig. 11-37C). A secondary center of
ossification occurs in the coronoid process. Just before the
development of the secondary center of ossification in the olecranon,
the leading edge of the metaphysis develops a well-defined sclerotic
margin.95 Ossification of the olecranon occurs in the area of the triceps insertion at approximately 9 years of age (see Fig. 11-37D).95 Ossification of the coronoid process is completed about the time that the olecranon ossification center appears.80
The term “apophysis” is usually applied to an epiphysis that is
subjected to traction by a muscle insertion. “Apophysis” and
“epiphysis” are used interchangeably in this chapter to describe the
olecranon secondary growth center because it contributes to length and
articular surface as well.
within the tip of the olecranon is enveloped by the triceps insertion. This was referred to by Porteous82 as a traction center.
The second and smaller center, an articular center, lies under the
proximal fourth of the articular surface of the semilunar notch.
 |
|
FIGURE 11-36 Angulation. A. Injury film showing 30 degrees of angulation and 30% lateral translocation of a radial neck fracture in a 10-year-old. B. Radiograph appearance of the proximal radius taken about 5 months later, showing lateral angulation of the neck. C.
Lateral view showing the anterior relationship of the radial neck with proximal migration. At this point the patient had full supination and pronation but a clicking sensation with forearm rotation in the area of the radial head. D. Three-dimensional reconstruction showing the incongruity of the proximal radiocapitellar joint. (Courtesy of Vince Mosca, MD.) |
the metaphysis, which progresses from anterior to posterior, occurs at
approximately 14 years of age. The sclerotic margin that defines the
edge of the metaphysis may be mistaken for a fracture (see Fig. 11-37F).95 Rarely, the physeal line persists into adulthood,47,76,111 usually in athletes who have used the extremity in repetitive throwing activities.16,87,100,113,121 The chronic tension forces applied across the apophysis theoretically prevent its normal closure.
This ossicle is completely separate and can articulate with the
trochlea. It is usually unilateral, unlike other persistent secondary
ossification centers, which are more likely to be bilateral and
familial. Zeitlin126 believed that the patella cubiti was a traumatic ossicle rather than a developmental variation.
findings of an olecranon fracture are tenderness and swelling. If the
fragment is completely displaced, the child cannot extend the elbow. A
palpable defect may be present between the apophysis and the proximal
metaphysis. Poland80 described the crepitus between the fragments as being muffled because cartilage covers the fracture surfaces.
radiographic diagnosis may be difficult before ossification of the
olecranon apophysis. The only clue may be a displacement of the small
ossified metaphyseal fragment (Fig. 11-38), and
the diagnosis may be based only on the clinical sign of tenderness over
the epiphyseal fragment. If there is any doubt about the degree of
displacement, injection of radiopaque material into the joint may
delineate the true nature of the fracture.
metaphysis distal to the physis probably accounts for the rarity of
fracture along the physeal line. Only a few reports mention the
mechanism of these physeal injuries. In most of the fractures reported
by Poland,80 three of which were confirmed by amputation
specimens, the force of the injury was applied directly to the elbow.
The force may be applied indirectly, producing an avulsion type of
fracture. In our experience, this fracture is usually caused by
avulsion forces across the apophysis with the elbow flexed, similar to
the more common flexion metaphyseal injuries. Children with
osteogenesis imperfecta (usually the tarda form) seem especially
predisposed to this injury.17,63
 |
|
FIGURE 11-37 Olecranon ossification. A. Limits of the border of ossification at birth, 8 years, and 12 years. B. Lateral view of olecranon at 6 months of age. The proximal margin is perpendicular to the long axis of the ulna. C. Lateral view of the olecranon at 6 years of age. The proximal margin is oblique. D.
Secondary ossification center developing in the olecranon in a 10-year-old. A sclerotic border has developed on the proximal metaphyseal margin. E. Bipartite secondary ossification center. The larger center is the traction center (open arrow). The smaller, more proximal center is the articular center (white arrow). F. Before complete fusion, a partial line remains (arrow), bordered by a sclerotic margin. |
 |
|
FIGURE 11-38 Apophysitis. A. Chronic stimulation with irregular ossification of the articular apophyseal center (arrows) in a basketball player who practiced dribbling 3 hours per day. B. Normal side for comparison.
|
athletes (especially baseball players) who place considerable recurrent
tension forces on the olecranon.74 Stress injuries also have been reported in elite gymnasts54 and tennis players.87 If the recurring activity persists, a symptomatic nonunion can develop.76,87,111,113,121
The apophyseal line may widen. Type II is an incomplete stress fracture
that involves primarily the apophyseal line, with widening and
irregularity (see Fig. 11-39B). A small
adjacent cyst may form, but usually the architecture of the secondary
ossification center is normal. These injuries occur primarily in sports
requiring repetitive extension of the elbow, such as baseball pitching,74 tennis,87 or gymnastics.54
Type III injuries involve complete avulsion of the apophysis. True
apophyseal avulsions (type IIIA) occur in younger children as a
fracture through the apophyseal plate (see Fig. 11-39A,B). In some of his amputation specimens, Poland80
found that the proximal apophyseal fragment included the distal tongue,
which extended up to the coronoid process. Apophyseal-metaphyseal
combination fractures (type IIIB), in which metaphyseal fragments are
attached to the apophysis (see Fig. 11-39C,D), usually occur in older children. Grantham and Kiernan34
likened it to a Salter-Harris type II physeal injury. Proximal
displacement of the fragment is the only clue seen on a radiograph.
|
TABLE 11-6 Classification of Apophyseal Injuries of the Olecranon
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
such fractures have been described. For fractures with significant
displacement, treatment is usually open reduction with internal
fixation using a combination of axial pins and tension-band wiring (Fig. 11-40).34,80,101 Gortzak et al.33
described a technique of open reduction using percutaneously placed
Kirschner-wires and absorbable sutures instead of wires for the tension
band. The percutaneously placed wires are subsequently removed 4 to 5
weeks postoperatively, eliminating the need for implant removal. There
has been concern that applying compressive forces across the apophysis
might cause growth arrest. In our experience, fusion of the apophysis
to the metaphysis is accelerated. Apophyseal fractures usually occur
when the physis is near natural closure. The growth proximally is
appositional rather than lengthwise across the apophyseal plate itself.
As a result, we have not found any functional shortening of the
olecranon because of the early fusion of the apophysis to the
metaphysis (see Fig. 11-40D). In practice, the
use of a compression screw across an ossified olecranon fracture causes
no loss of ulnar length. Children who sustain injuries before the
development of the secondary ossification center may develop a
deformity that is visible on radiographs (Fig. 11-41).
Although there may be shortening of the olecranon, it does not appear
to produce functional problems. There are no reports of the effects of
this injury in very young children or infants. Most stress injuries
respond to simple rest from the offending activity.
However,
a chronic stress fracture can result in a symptomatic nonunion. Use of
a compressive screw alone across the nonunion often is sufficient,54 but supplemental bone grafting may be necessary to achieve union.47,76
 |
|
FIGURE 11-39 Apophyseal avulsions. Pure apophyseal avulsions. A. The fracture follows the contour of the apophyseal line. B. The distal fracture line is in the shape of the apophyseal line (open arrow) with a small metaphyseal flake attached to the apophysis (solid arrow). Apophyseal-metaphyseal combination. C. The fracture line follows the line of tension stress. D. A large portion of the metaphysis (arrow) is often with the proximal metaphyseal fragment.
|
the patient to cease the offending activity. During this period of
rest, the patient should maintain upper extremity strength with a
selective muscle exercise program as well as maintain cardiovascular
conditioning. When a persistent nonunion of the olecranon in an
adolescent does not demonstrate healing after a reasonable period of
simple rest, we place a cannulated compression screw across the
apophysis to stimulate healing.
closed reduction can be obtained with the elbow extended. We usually
immobilize the elbow in a long-arm cast in extension. Percutaneous
pinning will stabilize the reduction if there is any concern about loss
of reduction. Completely displaced fractures are treated operatively
using a tension-band technique. In young children, we use small
Steinmann or Kirschner pins. The tension band is a strong absorbable
suture of one of the polyglycolic acid substances. Alternatively,
standard 16- to 18-gauge wire can be used in older adolescents.
Patients with large ossification centers are treated with a compression
screw similar to those with metaphyseal fractures.
overgrowth of the epiphysis proximally may produce a bony spur. In some
patients, these proximal spurs became symptomatic and were removed.
They are often associated with other fractures about the elbow. In the
combined series of 4684 elbow fractures reviewed, 230 were olecranon
fractures, for an incidence of 4.9%. This agrees with the incidence of
4% to 6% in the major series reported.25,58,73 Only 10% to 20% of the total fractures
reported in these series required an operation. Six reports totaling
302 patients with fractures of the olecranon in children are in the
English literature.29,34,58,69
Considering all age groups, 25% of olecranon fractures in these reports
occurred in the first decade and another 25% in the second decade.49 During the first decade, the peak age for olecranon fracture was between age 5 and 10 years.35,69
Approximately 20% of patients had an associated fracture or dislocation
of the elbow, most involving the proximal radius. Only 10% to 20%
required an operation.
 |
|
FIGURE 11-40 Operative treatment of an apophyseal fracture. A. Postoperative radiograph of the fracture shown in Figure 11-40D, which was stabilized with small Steinmann pins alone. B. Five months later, growth has continued in the traction center and the articular center is ossified (arrow). C.
One year after injury, the apophysis was partially avulsed a second time. The two secondary ossification centers are now fused. D. Three months after the second fracture, the fracture gap has filled in, producing a normal olecranon. |
 |
|
FIGURE 11-41 Preosseous apophyseal arrest. A.
Comminuted fracture of the proximal olecranon from a direct blow to the elbow in an 8-year-old male. This fracture was treated nonoperatively. B. Radiograph 18 months later shows cessation of the proximal migration of the metaphyseal margin and a lack of development of a secondary ossification center. Despite this arrest of the apophysis, the patient had a full range of elbow motion. |
|
TABLE 11-7 Incidence of Metaphyseal Fractures of the Olecranon
|
||||||
|---|---|---|---|---|---|---|
|
is relatively thin, allowing for the development of greenstick-type
fracture deformities. The periosteum is immature and thick, which may
prevent the degree of separation seen in adults. Likewise, the larger
amount of epiphyseal cartilage in children may serve as a cushion to
lessen the effects of a direct blow to the olecranon. In the production
of supracondylar fractures, ligamentous laxity in this age group tends
to force the elbow into hyperextension when the child falls on the
outstretched upper extremity. This puts a compressive force across the
olecranon and locks it into the fossa in the distal humerus, where it
is protected. An older person, whose elbow does not go into
hyperextension, is more likely to fall with the elbow semiflexed. This
unique biomechanical characteristic of the child’s olecranon
predisposes it to different fracture patterns than those in adults.
olecranon fracture. The abrasion or contusion associated with a direct
blow to the posterior aspect of the elbow provides a clue as to the
mechanism the injury. If there is wide separation, a defect can be
palpated between the fragments. In addition, there may be weakness or
even lack of active extension of the elbow, which is difficult to
evaluate in an anxious young child with a swollen elbow.
flexion injuries are usually perpendicular to the long axis of the
olecranon. This differentiates them from the residual physeal line,
which is oblique and directed proximal and anterior.95
In extension injuries, the longitudinally directed greenstick fracture
lines may be difficult to appreciate, and radiographs should be
scrutinized to detect associated fractures of the proximal radius or
distal humerus.
defined two major groups of olecranon fractures in which the fracture
line is either intra-articular or extra-articular. The degree of
displacement defines subclassifications in each group. We prefer to
classify these fractures based on the mechanism of injury (Table 11-8):
those associated with flexion injuries, those associated with extension
injuries, and shear injuries. Extension injuries are further divided
into varus and valgus patterns.
|
TABLE 11-8 Classification of Metaphyseal Fractures of the Olecranon
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
fractures, depending on whether the elbow is flexed or extended at the
time of injury. First, in injuries occurring with the elbow flexed,
posterior tension forces play an important role. Second, in injuries in
which the fracture occurs with the elbow extended, the varus or valgus
bending stress across the olecranon is responsible for the typical
fracture pattern. Third, a less common mechanism involves a direct blow
to the elbow that produces an anterior bending or shear force across
the olecranon. In this type, the tension forces are concentrated on the
anterior portion of the olecranon.
tension forces across the posterior aspect of the olecranon process.
Proximally, the triceps applies a force to the tip of the olecranon
process. Distally, there is some proximal pull by the insertion of the
brachialis muscle. Thus, the posterior cortex is placed in tension.
This tension force alone, if applied rapidly enough and with sufficient
force, may cause the olecranon to fail at its midportion (Fig. 11-42).
A direct blow applied to the posterior aspect of the stressed olecranon
makes it more vulnerable to failure. With this type of mechanism, the
fracture line is usually transverse and perpendicular to the long axis
of the olecranon (Fig. 11-43). Because the fracture extends into the articular surface of the semilunar notch, it is classified as intra-articular.
depends on the magnitude of the forces applied versus the integrity of
the soft tissues. The low incidence of displaced olecranon fractures
indicates that the soft tissues are quite resistant to these avulsion
forces. In flexion injuries, there are relatively few associated soft
tissue injuries or other fractures.69
elbow tends to hyperextend when a child breaks a fall with the
outstretched upper extremity. In this situation, the olecranon may be
locked into the olecranon fossa. If the elbow goes into extreme
hyperextension, usually the supracondylar area fails. If, however, the
major direction of the force across the elbow is
abduction
or adduction, a bending moment stresses the olecranon. Most of this
force concentrates in the distal portion of the olecranon. Because the
olecranon is metaphyseal bone, the force produces greenstick-type
longitudinal fracture lines (Fig. 11-44).
Most of these fracture lines are linear and remain extra-articular. In
addition, because the fulcrum of the bending force is more distal, many
of the fracture lines may extend distal to the coronoid process and
into the proximal ulnar shaft regions. The major deformity of the
olecranon with this type of fracture is usually an angulated greenstick
type of pattern.
 |
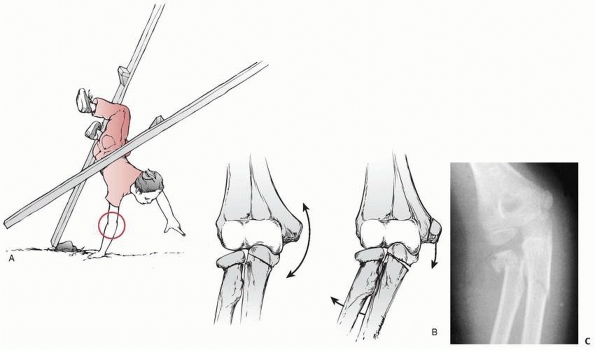
|
FIGURE 11-42 Mechanism of flexion injuries. Center. In the flexed elbow, a tension force develops on the posterior aspect of the olecranon (small double arrow) because of the pull of the brachialis and triceps muscles (large arrows). Right.
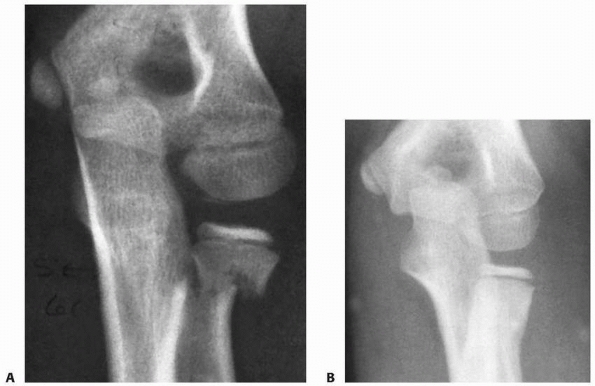
Failure occurs on the tension side, which is posterior as a result of the muscle pull or a direct blow to the prestressed posterior olecranon. |
injuries in the elbow region, which depend on whether the bending force
is directed toward varus or valgus. If a child falls with the forearm
in
supination, the carrying angle tends to place a valgus stress across
the elbow. The result may be a greenstick fracture of the ulna with an
associated fracture of the radial neck or avulsion of the medial
epicondylar apophysis (Fig. 11-45). If the fracture involves the radial neck, Bado35 classified it as an equivalent of the type I Monteggia lesion.
 |
|
FIGURE 11-43 Radiograph of flexion injury showing greater displacement on the posterior surface.
|
 |
|
FIGURE 11-44 A. Anteroposterior view of a linear greenstick fracture line (arrow) in the medial aspect of the olecranon. B. Lateral view showing the posterior location of the fracture line (arrow).
|
 |
|
FIGURE 11-45 Valgus pattern of an extension fracture. A. A fall with the elbow extended places a valgus stress on the forearm. B.
With increased valgus, a greenstick fracture of the olecranon can occur with or without a fracture of the radial neck or avulsion of the medial epicondylar apophysis. C. Radiograph of a valgus extension fracture of the olecranon with an associated fracture of the radial neck. |
or if the forearm is pronated, a varus force is placed across the elbow
(Fig. 11-46). The major injury associated with this varus force is a partial or total lateral dislocation of the radial head. Bado4 classified this as a type III Monteggia lesion. In this type of fracture, the posterior interosseous nerve may be injured.
when a direct blow to the proximal ulna causes it to fail with an
anterior tension force; the proximal radioulnar joint maintains its
integrity. The most common type of shear injury is caused by a shear
force applied directly to the posterior aspect of the olecranon, with
the distal fragment displacing anteriorly (Figs. 11-47 and 11-48).
The intact proximal radioulnar joint displaces with the distal
fragment. In this type of injury, the elbow may be either flexed or
extended when the direct shear force impacts the posterior aspect of
the olecranon. These fractures are due to a failure in tension, with
the force concentrated along the anterior cortex. This is opposite to
the tension failure occurring on the posterior aspect of the cortex in
the more common flexion injuries. In the shear-type injury, the
fracture line may be transverse or oblique. The differentiating feature
from the more common flexion injury is that the thick posterior
periosteum usually remains intact. The distal fragment is displaced
anteriorly by the pull of the brachialis and biceps muscles. Newman70
described one patient in whom a shear force was directed medially; the
radial neck was fractured, and the radial head remained with the
proximal fragment.
fractures. Most displace minimally and require immobilization with the
elbow in no more than 75 to 80 degrees of flexion (Fig. 11-50).
Even if the fracture displaces severely, immobilization in full or
partial extension usually allows the olecranon to heal satisfactorily.25,101,127
comminuted, open reduction with internal fixation usually is required.
Recommended fixation devices vary from catgut or absorbable suture57 to an axial screw,55 tension-band wiring with axial
pins,23,34,57,91,94,101 or a plate.107
Internal fixation allows early motion. No one has reported significant
growth disturbances from internal fixation of metaphyseal olecranon
fractures.
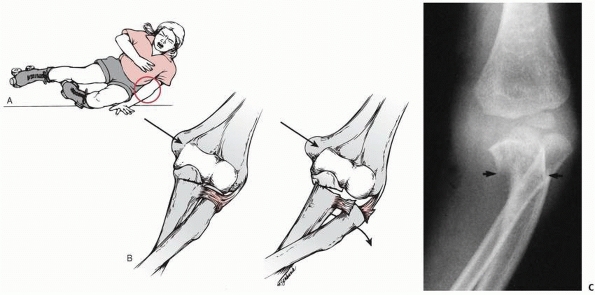 |
|
FIGURE 11-46 Varus pattern of an extension fracture. A. A fall against the extended elbow places a varus stress on the forearm. B.
The result is a greenstick fracture of the olecranon with a lateral dislocation of the radial head (type III Monteggia lesion). C. Radiograph of a varus extension injury showing subluxation of the radial head and greenstick fracture of the ulna (arrows). |
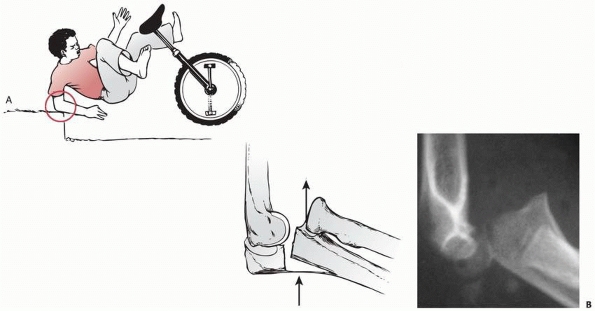 |
|
FIGURE 11-47 Flexion shear injuries. A.
Fracture with the elbow flexed. The direct blow to the distal portion of the posterior olecranon causes the fracture to fail in tension of the anterior surface. The intact proximal radioulnar joint displaces anteriorly. B. Radiograph of a flexion shear injury showing the distal fragments displaced anteriorly as a unit. |
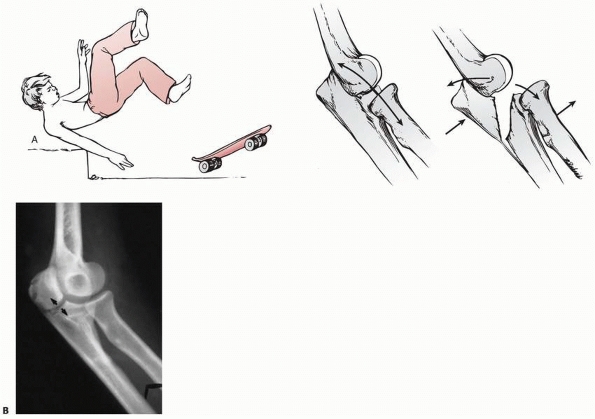 |
|
FIGURE 11-48 Extension shear injuries. A.
Fracture with the elbow extended. If the elbow is extended when the direct blow to the posterior aspect of the elbow occurs, the olecranon fails in tension but with an oblique or transverse fracture line (arrows). B. With the elbow extended, the initial failure is in the anterior articular surface (arrows). |
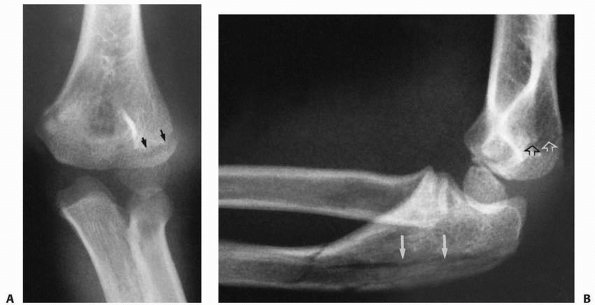 |
|
FIGURE 11-49 A. Undisplaced fracture of the lateral condyle (arrows) associated with a varus greenstick fracture of the olecranon. B. Lateral view showing greenstick fractures in the olecranon (solid arrows) and a nondisplaced fracture of the lateral condyle (open arrows).
|
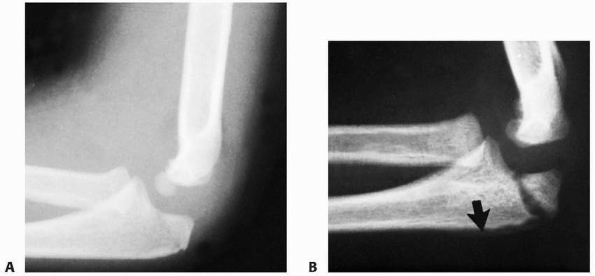 |
|
FIGURE 11-50 Simple immobilization of a flexion injury. A. Injury film, lateral view, showing minimal displacement. B. Three weeks later, the fracture has displaced further. Periosteal new bone is along the posterior border of the olecranon (arrow). Healing was complete with a normal range of motion. (Courtesy of Jesse C. DeLee, MD.)
|
compared the failure of various fixation devices under rapid loading:
(a) figure-of-eight wire alone, (b) cancellous screw alone, (c) AO
tension band, and (d) cancellous screw with a figure-of-eight wire
combination. The cancellous screw alone and figure-of-eight wire alone
were by far the weakest. The greatest resistance to failure was found
in the combination of a screw plus figure-of-eight wire, followed
closely by the AO tension-band fixation. In their clinical evaluation
of patients, comparing the AO tension band and combination of screw and
figure-of-eight wire, they found more clinical problems associated with
the AO technique.65 The main problem with the AO technique is the subcutaneous prominence of the axial wires.53 To prevent proximal migration of these wires, Montgomery66 devised a method of making eyelets in the proximal end of the wires through which he passed the figure-of-eight fixation wire.
realignment of the angulation of the olecranon and treatment of the
secondary injuries. Often in varus injuries, correction of the
alignment of the olecranon also reduces the radial head. The olecranon
angulation corrects with the elbow in extension. This locks the
proximal olecranon into the olecranon fossa of the humerus so that the
distal angulation can be corrected at the fracture site with a valgus
force applied to the forearm. Occasionally, in extension fractures,
complete separation of the fragments requires open reduction and
internal fixation (Fig. 11-51).
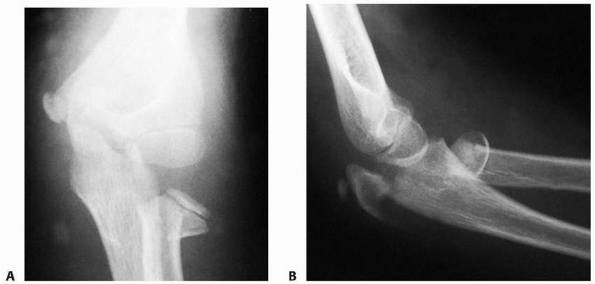 |
|
FIGURE 11-51 Open reduction of a valgus extension injury. A. Anteroposterior injury film shows complete displacement of the radial head. B.
Lateral view also shows the degree of displacement of the olecranon fracture. This patient required surgical intervention with internal fixation to achieve a satisfactory reduction. |
that the original angulation tends to redevelop in some fractures. If a
varus force produced the fracture, the proximal ulna or olecranon may
drift back into varus, which can cause a painful subluxation of the
radial head. A secondary osteotomy of the proximal ulna or olecranon
may be necessary if the angulation is significant.
recognition that the distal fragment is displaced anteriorly and the
posterior periosteum remains intact. The intact posterior periosteum
can serve as an internal tension band to facilitate reduction.
and the posterior periosteum serves as a compressive force to maintain
the reduction. Smith101 reported
treatment of this fracture using an overhead sling placed to apply a
posteriorly directed force against the proximal portion of the distal
fragment. The weight of the arm and forearm helps supplement the
tension-band effect of the posterior periosteum.
with an oblique screw perpendicular to the fracture line (Fig. 11-52).
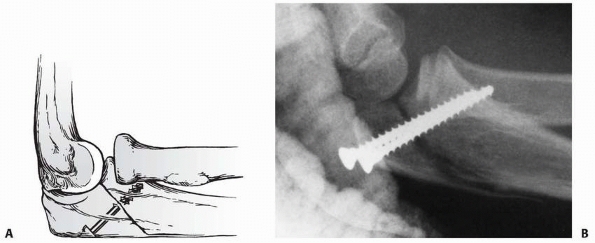 |
|
FIGURE 11-52 Operative treatment of extension shear fractures. A.
If the periosteum is insufficient to hold the fragments apposed, an interfragmentary screw can be used, as advocated by Zimmerman.115 B. An extension shear type of fracture secured with two oblique interfragmentary screws. |
the elbow in 5 to 10 degrees of flexion for approximately 3 weeks. It
is important to obtain radiographs of these fractures after
approximately 5 to 7 days in the cast to ensure that there has not been
any significant displacement of the fragment.
palpate the fracture for a defect and flex the elbow to determine the
integrity of the posterior periosteum. If the fragments separate with
either of these maneuvers, they are unstable and are fixed internally
so that active motion can be started as soon as possible.
Originally we used the standard AO technique with axial Kirschner-wires
or Steinmann pins and figure-of-eight stainless steel as the tension
band (Fig. 11-53A). Because removal of the wire
often required reopening the entire incision, we now use an absorbable
suture for the figure-of-eight tension band. Number 1 polydioxanone
(PDS) suture, which is slowly absorbed over a few months, is ideal (see
Fig. 11-53B). When rigid internal fixation is
applied, rapid healing at the fracture site produces internal stability
before the PDS absorbs. We prefer Kirschner-wires in patients who are
very young and have very little ossification of the olecranon apophysis
(see Fig. 11-40). If the axial wires become a
problem, we remove them through a small incision. Most recently, we
have used a combination of an oblique cortical screw with PDS as the
tension band (see Fig. 11-53C,D) and are
pleased with the results. In the past, we had to remove almost all the
axial wires; very few of the screws cause enough symptoms to require
removal. Occasionally, we use the tension-band wire technique with 16-
or 18-gauge wire in a heavier patient.
allow a forceful manipulation of the olecranon while it is locked in
its fossa in extension. Because this is a greenstick fracture, we
slightly overcorrect to prevent the development of reangulation. These
fractures may require manipulation/remanipulation in 1 to 2 weeks if
the original angulation recurs. Associated fractures are treated as if
they were isolated injuries.
usually immobilize them in enough hyperflexion to hold the fragments
together, if the posterior periosteum is intact (Fig. 11-54). If the periosteum is torn, an oblique screw is an excellent way to secure the fracture (see Fig. 11-52).
If considerable swelling prevents the elbow from being hyperflexed
enough to use the posterior periosteum as a tension band, an oblique
screw is a good choice.
in a long-arm cast. The cast should be bivalved if there is excessive
swelling. The cast or posterior splint is worn for 3 weeks, at which
time the patient begins active range of motion.
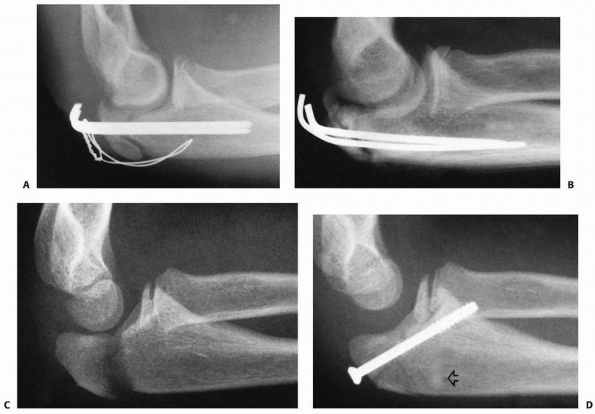 |
|
FIGURE 11-53 Internal tension-band techniques. A. Standard AO technique with stainless steel wire. The wire can be prominent in the subcutaneous tissues. B. Axial wires plus polydioxanone sutures (PDS) 6 weeks after surgery. C. A displaced flexion-type injury in an 11-year-old male. There is complete separation of the fracture fragments. D.
A cancellous lag screw plus PDS. The screw engages the anterior cortex of the coronoid process. The PDS passes through a separate drill hole in the olecranon (open arrow) and crosses in a figure-of-eight manner over the fracture site and around the neck of the screw. |
one fracture treated with suture fixation ultimately progressed to a
nonunion. Despite this, the patient had only a 10 degrees extension lag
and grade 4 triceps strength. An accessory ossicle, such as a patella
cubiti, is not a nonunion.
illustrates a delayed union in which the apophysis became elongated to
the point that it limited extension. This proximal overgrowth of the
tip of the apophysis has occurred in olecranon fractures after routine
open reduction and internal fixation.73
immobilization may lose reduction, which results in a significant loss
of elbow function (Fig. 11-57).
consists of epiphyseal and physeal cartilage at the distal end of a
tongue extending from the apophysis of the olecranon. The coronoid
process does not develop a secondary center of ossification, but
instead ossifies along with the advancing edge of the metaphysis (see Fig. 11-37).
Because most fractures of the coronoid process occur with dislocations
of the elbow, it seems logical that they would happen in older
children. However, in a review of 23 coronoid fractures in children,
Bracq10 found that the injuries
occurred in 2 peak age groups: one was between 8 and 9 years of age and
the other between 12 and 14 years.
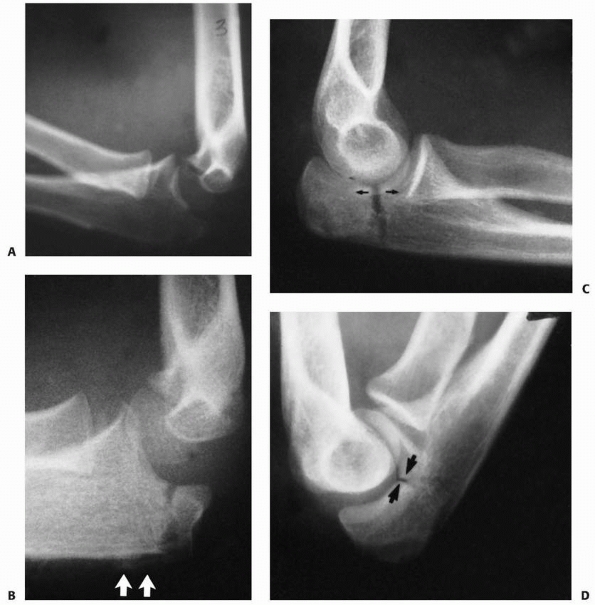 |
|
FIGURE 11-54 Shear injuries. A. Flexion pattern: radiograph of the patient seen in Figure 11-45A after the elbow was flexed. The intact posterior periosteum acted as a tension band and held the fracture reduced. B. Radiograph taken 4 weeks after surgery shows new bone formation under the intact periosteum (arrows) on the dorsal surface of the olecranon. C. Extension pattern: radiograph of patient with an extension shear injury showing an increase in the fracture gap (arrows) (see also Fig. 11-45B). D. Because the dorsal periosteum and cortex were intact, the fracture gap (arrows) closed with flexion of the elbow.
|
 |
|
FIGURE 11-55
Congenital pseudarthrosis of the olecranon in a 9-year-old female who had limited elbow extension and no antecedent trauma. The edges of the bone were separated by thick fibrous tissue. (Courtesy of Michael J. Rogal, MD.) |
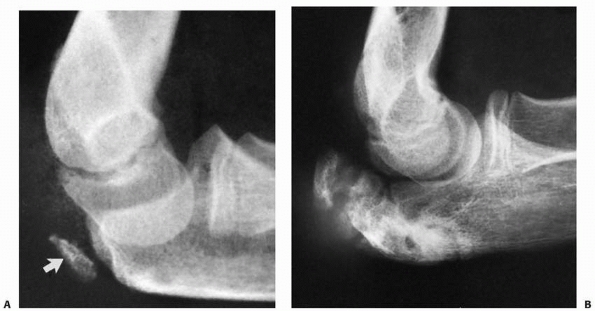 |
|
FIGURE 11-56 A. Injury film showing partial avulsion of the tip of the olecranon apophysis (arrow). B.
Radiograph taken 4 years later shows a marked elongation and irregular ossification of the apophysis. (Courtesy of Joel Goldman, MD.) |
elbow dislocations, fractures of the olecranon, medial epicondyle, and
lateral condyle also can occur.70 The fracture of the coronoid may be part of a greenstick olecranon fracture (i.e., the extension-type metaphyseal fracture; Fig. 11-58).
Isolated coronoid fractures are theoretically caused by avulsion by the
brachialis or secondary to an elbow dislocation that reduced
spontaneously, which is usually associated with hemarthrosis and a
small avulsion of the tip of the olecranon process (Fig. 11-59).
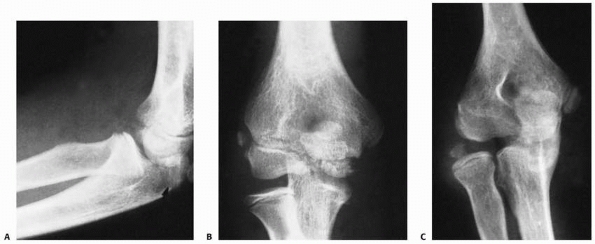 |
|
FIGURE 11-57 Loss of reduction. A. Lateral radiograph of what appeared to be a simple undisplaced fracture (arrow) of the olecranon in a 13-year-old female. B.
On the anteroposterior film, the fracture also appears undisplaced. The mild lateral subluxation of the radial head was not recognized. C. Radiographs taken 5 months later showed further lateral subluxation with resultant incongruity of the elbow joint. (Courtesy of Richard W. Williamson, MD.) |
is often difficult because on the lateral view the radial head is
superimposed over the coronoid process. Evaluation of a minimally
displaced fracture may require oblique views (Fig. 11-60).103 The radiocapitellar view (see Fig. 11-6) shows the profile of the coronoid process.
back into the joint. The only clue to this fracture may be the presence
of a small flake of bone in the anterior part of the joint on the
lateral radiograph.
 |
|
FIGURE 11-58 Fracture of the coronoid (arrow)
as part of an extension valgus olecranon fracture pattern. There was an associated fracture of the radial neck. Both the neck fracture and the distal portion of the coronoid process show periosteal new bone formation (open arrows). |
 |
|
FIGURE 11-59
Lateral radiograph of an 11-year-old male who injured his left elbow. Displaced anterior and posterior fat pads, plus a small fracture of the coronoid (arrow), indicate a probable partially dislocated elbow as the primary injury. |
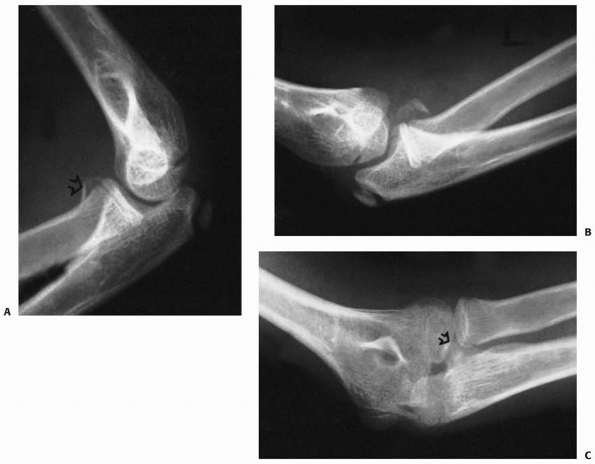 |
|
FIGURE 11-60 A.
Based on this original lateral radiograph, a 12-year-old male with a swollen elbow was thought to have a fracture of the radial neck (arrow). B. With an oblique view, it is now obvious that the fragment is from the coronoid process. C. Five months later, the protuberant healed coronoid process (arrow) is seen on this radiocapitellar view. |
|
TABLE 11-9 Classification of Fractures of the Coronoid Process
|
|||
|---|---|---|---|
|
This classification is useful in predicting the outcome and in
determining the treatment. Type I fractures involve only the tip of the
process (see Fig. 11-59), type II fractures involve more than just the tip but less than 50% of the process (see Fig. 11-60), and type III fractures involve more than 50% of the process.
elbow instability guides the treatment. The associated injuries also
are a factor in treatment. Regan and Morrey85,86
treated types I and II fractures with early motion if there were no
contradicting associated injuries. For initial immobilization, if the
fracture is associated with an elbow dislocation, the elbow is placed
in approximately 100 degrees of flexion, with the forearm in full
supination.70 Occasionally, in
partial avulsion fractures, the fracture reduces more easily with the
elbow in extension. In these rare cases, the brachialis muscle may be
an aid in reducing the fragment in extension.69 Regan and Morrey85
found that the elbow often was unstable in type III fractures, and they
secured these fractures with internal fixation. They had satisfactory
results with type I and II fractures, but in only 20% of type III
fractures were the results satisfactory.
much as we do elbow dislocations. The presence of a coronoid fracture
alerts us to be especially thorough in looking for other injuries. In
children, surgery is rarely necessary. If there is a large fragment and
marked displacement, open reduction is done through a Henry anterior
approach to the elbow. The fragment is fixed with a minifragment screw
or sewn in place through two drill holes in the posterior aspect of the
ulna.
fragment (type III), the elbow may be unstable and prone to recurrent
dislocations. Nonunion with the production of a free fragment in the
joint occurs rarely in children.74
AA. New method for treatment of the dislocated radial neck fracture in
children. In: Chapchal G, ed. Fractures in Children. New York: Georg
Thieme, 1981: 192-194.
HG. Fractures of the proximal radius and ulna. In: Kasser JR, Beaty JH,
eds. Rockwood & Wilkins’ Fractures in Children 5th ed.
Philadelphia: Lippincott Williams & Wilkins, 2001:483-528.
S, Vaishya R, Klenerman L. Management of radial neck fractures in
children. A retrospective analysis of 100 patients. J Pediatr Orthop
1993;13:232-238.
Cesare PE, Sew-Hoy A, Krom W. Bilateral isolated olecranon fractures in
an infant as presentation of osteogenesis imperfecta. Orthopedics
1992;15:741-743.
G-F, Wu C-C, Shin C-H. Olecranon fractures treated with tension band
wiring techniques: comparisons among three different configurations.
Chang Keng I Hsueh 1993;16:231-238.
EE, Blake NS, Regan BF. Fracture of the radial neck with medial
displacement of the shaft of the radius. Br J Radiol 1983;56:486-487.
KE. Displaced fracture of the proximal end of the radius in a child. A
case report of the deceptive appearance of a fragment that had rotated
180 degrees. J Bone Joint Surg Am 1995;77:782-783.
T, Tsukamoto Y, Itoman M. Percutaneous reduction of displaced radial
neck fractures. J Shoulder Elbow Surg 1995;4:162-167.
BC, Strecker WB, Schoenecker PL. Surgical treatment of displaced
olecranon fractures in children. J Pediatr Orthop 1997;17:321-324.
P, Alvarez-Romera A, Burgos J, et al. Displaced radial neck fractures
in children treated by closed intramedullary pinning (Metaizeau
technique). J Pediatr Orthop 1997;17:325-331.
Y, Mercado E, Atar D, et al. Pediatric olecranon fractures: open
reduction and internal fixation with removable Kirschner wires and
absorbable sutures. J Pediatr Orthop 2006;26:39-42.
A, Norman A. The radial head-capitellum view: useful technique in elbow
trauma. AJR Am J Roentgenol 1982;138:1186-1188.
A, Norman A, Rosen H. Radial head-capitellum view in elbow trauma:
clinical application and radiographic-anatomic correlation. AJR Am J
Roentgenol 1984; 143:355-359.
MA, Shorvon PJ, Chapman M. Assessment of the radial head-capitellum
view and the dorsal fat-pad sing in acute elbow trauma. AJR Am J
Roentgenol 1985; 145:607-609.
A, Guichet J.M. Arthrography for reduction of a fracture of the radial
neck in a child with a nonossified radial epiphysis. JBJS Br
2001;83-B:542-543.
EB. Surgical approach to the proximal end of the radius and its use in
fractures of the head and neck of the radius. J Bone Joint Surg
1941;23:86-92.
B, Rinott MG, Tanzman M. Closed reduction of fractures of the proximal
radius in children. J Bone Joint Surg Br 1989;71:66-67.
JI, Baker BE, Mosher JF. Fracture-separation of the olecranon
ossification center in adults. Am J Sports Med 1985;13:105-111.
LA. Fracture patterns in children. Analysis of 8,682 fractures with
special reference to incidence, etiology and secular changes in a
swedish urban population. 1950-1979. Acta Orthop Scand Suppl
1983;202:1-109.
RD, Waters PM, Jaramillo D. The use of ultrasonography in the diagnosis
of occult fracture of the radial neck: a case report. J Bone Joint Surg
Am 1998;80:1361-1364.
S, Hugasson C. Significance of associated lesions including dislocation
of fracture of the neck of the radius in children. Acta Orthop Scand
1979;50:79-83.
A II. Medial displacement of the shaft of the radius with a fracture of
the radial neck. J Bone Joint Surg Am 1979;61:788-789.
JP, Lascombes P, Lemelle JL, et al. Reduction and fixation of displaced
radial neck fractures by closed intramedullary pinning. J Pediatr
Orthop 1993;13:355-360.
JP, Prevot J, Schmitt M. Reduction et fixation des fractures et
decollements epiphysaires de la tete radiale par broche
centromedullaire. Rev Chir Orthop 1980; 66:47-49.
DF, Greene WB, Gilbert JA, et al. Displaced olecranon fractures in
adults. Biomedical analysis of fixation methods. Clin Orthop Relat Res
1987;224:210-214.
RJ. A secure method of olecranon fixation: a modification of tension
band wiring technique. J R Coll Surg Edinb 1986;31:179-182.
CG, Torch MA. New reduction technique for severely displaced pediatric
radial neck fractures. J Pediatr Orthop 2003;23:626-628.
RF. Treatment of displaced transverse fractures of the neck of the
radius in children. J Bone Joint Surg 1934;16:695-698.
H, Torg JS, Jacobs B, et al. Nonunion of olecranon epiphysis: two cases
in adolescent baseball pitchers. AJR Am J Roentgenol 1981;136:819-820.
K, Hirvensalo E, Bostman O, et al. Treatment of radial head fractures
with absorbable polyglycolide pins: a study on the security of the
fixation in 38 cases. J Orthop Trauma 1994;8:94-98.
JV, Aracil J, Barcelo M. Leverage method in displaced fractures of the
radial neck in children. Clin Orthop 1982;169:215-218.
CL, Scott SM. Compartment syndrome in the forearm following fractures
of the radial head or neck in children. J Bone Joint Surg Am
1995;77:1070-1074.
KR, Garg NK, Bruce CE. Elastic stable intramedullary nail fixation for
severely displaced fractures of the neck of the radius in children.
JBJS Br 2006;88-B: 358-361.
RK, Wepfer JF, Olen DW, et al. Case report 355: delayed closure of the
right olecranon epiphysis in a right-handed tournament-class tennis
player. Skeletal Radiol 1986;15:185-187.
M, Moulies D, Longis B, et al. Les fractures de l’extremite superieure
du radius chez l’enfant. Chir Pediatr 1986;27:318-321.
EC. Displaced fractures of the head and neck of the radius in children:
open reduction and temporary transarticular internal fixation.
Orthopedics 1991;14:697-700.
SL, Mac Ewan DW. Changes due to trauma in the fat plane overlying the
supinator muscle: a radiologic sign. Radiology 1969;92:954-958.
SE, Anticevic D, Strongwater AM, et al. Case report and review of the
literature: chronic fracture-separation of the radial head in a child.
J Orthop Trauma 1995;9: 259-262.
SA, Burkhart SS. Tension band wiring of olecranon fractures. A
modification of the AO technique. Clin Orthop Relat Res
1992;277:238-242.
PP, Haevernick B, Herold A, et al. Treatment decision, method of osteo
synthesis, and outcome in radial neck fractures in children. A
multicenter study. J Pediatr Orthop 2005;25:45-50.
JE, Miller JH. Fracture of the neck of the radius in children:
prognostic factors and recommendations for management. J Bone Joint
Surg Br 1985;67:491.
S, Lascombes P, Prevot J, et al. Fractures of the radial head and
associated elbow injuries in children. J Pediatr Orthop B
1996;5:200-209.
JA, Graham HK. Angulated radial neck fractures in children: a
prospective study of percutaneous reduction. J Bone Joint Surg Br
1992;74:760-764.
JCH, Ellis BW. Vulnerability of the posterior interosseous nerve during
radial head resection. J Bone Joint Surg Br 1971;53:320-323.
ML, Kropp M, Gillespie R. Fracture of the radial neck and proximal ulna
with medial displacement of the radial shaft. Report of two cases.
Orthopedics 1989;12: 1577-1579.
MD, Lubahn JD. Olecranon fracture with unilateral closed radial shaft
fracture in a child with open epiphysis. Orthopedics 1990;13:463-465.
SD, Ierodiaconou MN, Roussis N. Fracture of the upper end of the ulna
associated with dislocation of the head of the radius in children. Clin
Orthop Relat Res 1988;228:240-249.
CJP, van Ouwerkerk WPL, Scheele PM, et al. Unilateral patella cubiti: a
probable posttraumatic disorder. Eur J Radiol 1992;14:60-62.
JS, Moyer R. Nonunion of a stress fracture through the olecranon
epiphyseal plate observed in an adolescent baseball pitcher. J Bone
Joint Surg Am 1977;59:264-265.
AH, Andrews JR, Schob CJ, et al. Fractures of unfused olecranon physis:
a reevaluation of this injury in three athletes. Orthopedics
1995;18:390-394.
N, Laliotis N, Vlachos E. Acute osteomyelitis complicating a closed
radial fracture in a child: a case report. Acta Orthop Scand
1992;63:341-342.
AK, Von Laer L. Displaced fractures of the radial neck in children:
long-term results and prognosis of conservative treatment. J Pediatr
Orthop B 1998;7:217-222.
WT, Williams JJ. Radial neck fracture complicating closed reduction of
a posterior elbow dislocation in a child: case report. J Trauma
1991;31:1686-1688.
RD, Johns JC. Nonunion of an olecranon stress fracture in an adolescent
gymnast: a case report. Am J Sports Med 1990;18:432-434.
SK. Reversal of the radial head during reduction of fractures of the
neck of the radius in children. J Bone Joint Surg Br 1969;51:707-710.
PR. Greenstick fracture of the upper end of the ulna with dislocation
of the radio-humeral joint or displacement of the superior radial
epiphysis. J Bone Joint Surg Br 1963;45:727-731.
H. Fractures of the elbow. In: Weber BG, Brunner C, Freuler F, eds.
Treatment of Fractures in Children and Adolescents. New York:
Springer-Verlag, 1980.
