FRACTURES OF THE HINDFOOT
for less than 1% of all fractures, they are fraught with serious
complications, including skin necrosis, infection, avascular necrosis,
malunion, nonunion, ankle and subtalar arthrofibrosis, and
posttraumatic arthritis (18,23,51,55,72,81).
Injuries range from osteochondral fractures of the dome to fractures of
the talar neck and body, with or without subluxation or dislocation of
the ankle and subtalar joints. With advances in methods of treatment,
morbidity is decreasing and complications are being managed more
effectively.
articulates with the tibia, posterior subtalar facet, and lateral
malleolus; the head anteriorly, which articulates with the navicular,
anterior and middle subtalar facets, and calcaneonavicular ligament;
and the neck, which has no articulations.
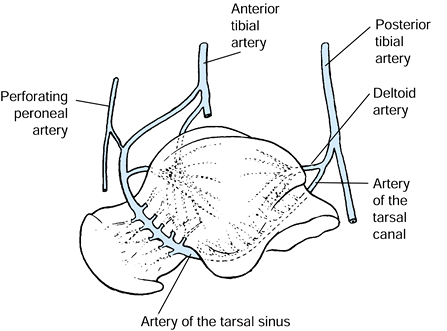
Because of its large articular surface and lack of muscular
attachments, the talus has a limited surface area for vascular supply.
Although it has a rich blood supply, with contributions from all three
main arteries of the lower limb, the limited access makes its blood
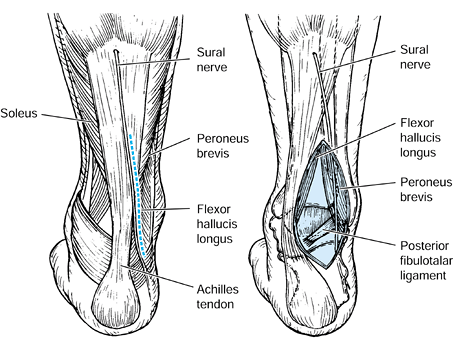
supply particularly vulnerable to injury. The three main extraosseous
vascular sources are arterial branches to the dorsal neck arising from
the anterior tibial and peroneal arteries, the artery of the sinus
tarsi arising from the anterior tibial and peroneal arteries, and the
artery of the tarsal canal arising from the posterior tibial artery (Fig. 110.1). Additionally, the deltoid branch of the artery to the tarsal canal supplies blood to the medial talar body (46,62). Numerous smaller channels enter through capsular and ligamentous attachments.
 |
|
Figure 110.1.
Blood supply of the talus. The three main arterial contributions are shown, in addition to the deltoid branch to the medial talar body. (From Mayo KA. Fractures of the Talus: Principles of Management and Techniques of Treatment. Tech Orthop 1988;3:42, with permission.) |
demonstrated injury to the intraosseous arterial network in
nondisplaced, experimentally produced talar neck fractures, with
progressive damage to the main extraosseous arterial channels as
fracture displacement progressed.
major traumatic events. They make up 50% of all major injuries to the
talus (23). Once termed aviator’s astragalus,
talar neck fractures are no longer caused primarily by flying
accidents; motor vehicle accidents and falls from heights are now more
common mechanisms of injury. These fractures initially were thought to
be caused by forced dorsiflexion of the talus against the anterior
margin of the tibia, but laboratory studies have shown that they are
more likely caused by a dorsally directed shear force exerted against
the sole of the foot with the body of the talus fixed between the tibia
and calcaneus. Fractures occur in a vertical or slightly oblique plane
between the middle and posterior subtalar facets, and the distal
fragment is characteristically displaced dorsally and medially (18). The force required to fracture the talus is roughly twice that required to fracture either the calcaneus or the navicular (74).
With additional force, the body of the talus is dislocated posteriorly
out of the ankle mortise, usually medial to the Achilles tendon.
into chip and avulsion fractures, compression fractures of the head,
fractures of the neck, and fractures of the body. Dislocations and
fracture–dislocations were further subdivided into those associated
with dislocations of the ankle, subtalar, and midtarsal joints.
Type I fractures are nondisplaced and disrupt only those blood vessels
entering the body via the dorsal talar neck in addition to intraosseous
vessels crossing the neck. Type II fractures are displaced with
subluxation or dislocation of the subtalar joint. These fractures
disrupt the dorsal neck arterial branches
and
the branches entering inferiorly from the sinus tarsi and tarsal canal,
leaving undisturbed only the vessels entering through the deep deltoid
ligament and medial talar body. Type III fractures are displaced with
dislocation of the talar body from both the ankle and the subtalar
joints. The body of the talus is usually displaced posteriorly and
medially, stretching and compressing the neurovascular bundle. All
three main sources of blood supply to the body of the talus are
disrupted in these injuries. Canale and Kelly (20)
added type IV, which are fractures associated with complete dislocation
of the talar body and subluxation or dislocation of the talar head from
the talonavicular joint.
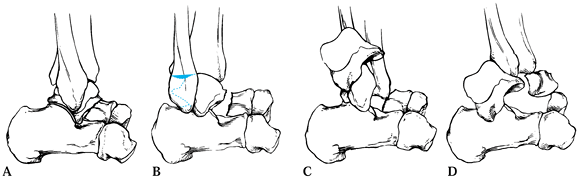 |
|
Figure 110.2. Modified Hawkins (41) classification of talar neck fractures. A: Type I, nondisplaced. B: Type II, displaced with subluxation or dislocation of the subtalar joint. C: Type III, displaced with dislocation of the talar body from both ankle and subtalar joints. D:
Type IV, subluxation or dislocation of talar head in addition to dislocation of talar body. (From Delee JC. Fractures and Dislocations of the Foot. In: Mann RA, ed. Surgery of the Foot, 5th ed. St. Louis: Mosby, 1986:656, with permission.) |
Look for associated injuries. Tomograms or computed tomography (CT)
scans are occasionally required to assess the fracture configuration
and displacement.
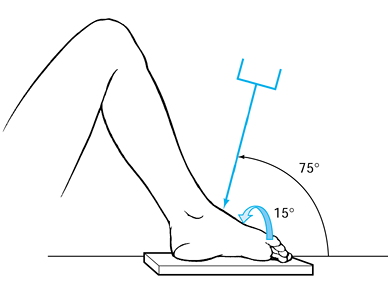 |
|
Figure 110.3.
Pronated oblique view of midfoot to better visualize the talar neck. Ankle is in maximal equinus, with foot pronated 15°. Direct the roentgen tube 75° from the horizontal. (From Delee JC. Fractures and Dislocations of the Foot. In: Mann RA, ed. Surgery of the Foot, 5th ed. St. Louis: Mosby, 1986:656, with permission.) |
nondisplaced (type I) talar neck fractures. Treat in a short-leg,
non-weight-bearing cast for 6–8 weeks. Once union occurs, begin
progressive weight bearing and mobilization of the ankle and subtalar
joints.
talar neck fractures (types II, III, and IV). Reduction is difficult to
maintain using closed methods because of tearing of the talocalcaneal
interosseous ligament (33). Type II fractures
require anatomic reduction to correct subtalar incongruity. Fractures
of type III or IV require prompt reduction of the talar body to reduce
the risk of pressure necrosis of the overlying skin. Early reduction
and rigid internal fixation reestablishes soft-tissue circulation,
enhances bony revascularization, and allows early motion, which reduces
the risk of persistent edema, soft-tissue atrophy, stiffness, and
osteoporosis (i.e., “fracture disease”) (24,63,86).
Open injuries require immediate and thorough irrigation and debridement
of the wound, anatomic reduction, internal fixation, and appropriate
antibiotics.
methods using fluoroscopic guidance, most type III and IV fractures
require open reduction. Reduction of the talar body into the mortise is
often facilitated by equinus positioning of the foot and axial traction
through a calcaneal pin. Reduce the body as gently as possible to
prevent further damage to the blood supply and articular cartilage.
Osteotomy of the medial malleolus may facilitate reduction of the
dislocated talar body; it also protects the deep deltoid blood supply
to the talus (32).
and rigid screw fixation for definitive fixation. Screws prevent
fracture displacement and malunion, and they enhance body union and
early mobilization of the ankle and subtalar joints. Screws placed
anterior to posterior allow visualization of the fracture, but often
they must be placed through the weaker talar neck or talar head
articular surface (38,86).
Screws placed posterior to anterior avoid disruption of the
talonavicular joint and further damage to the dorsal blood supply to
the talar neck, but they do not allow direct visualization of fracture
reduction (30,48,93) unless a combined anterior and posterior exposure is performed. A mechanical study by Swanson et al. (85)
demonstrated that posterior screw fixation gives more rigid fixation
than anterior screws, and both are superior to Kirschner wire (K-wire)
fixation. The choice of surgical approach ultimately depends on the
presence and location of traumatic wounds, the condition of skin,
fracture classification and configuration, and the presence of adjacent
fractures (53). Cannulated screws are now available for percutaneous fixation of fractures accurately reduced using closed methods (20).
approach avoids the neurovascular bundle and is generally recommended for type II fractures.
-
Place the patient in the prone or lateral
decubitus position with the affected extremity uppermost. Make a 4 cm
longitudinal incision just lateral to the Achilles tendon, taking care
to protect the sural nerve, which is anterior (Fig. 110.4). Figure 110.4. Make the skin incision for the posterolateral approach to the talus just lateral to the Achilles tendon.
Figure 110.4. Make the skin incision for the posterolateral approach to the talus just lateral to the Achilles tendon. -
Locate the posterior process of the talus through the peroneus brevis and flexor hallucis longus tendons (Fig. 110.5).
![]() Figure 110.5.
Figure 110.5.
Posterolateral approach to the talus. Retract the sural nerve
anteriorly. Expose the posterior talus through the interval between the
peroneus brevis and flexor hallucis longus tendons. (From Mayo KA.
Fractures of the Talus: Principles of Management and Techniques of
Treatment. Tech Orthop 1988;3:42, with permission.) -
Next, perform a closed reduction by
plantar-flexing and abducting the forefoot under fluoroscopic guidance.
Use a 2.0 mm K-wire as a “joystick” to manipulate the fracture if
needed. If you cannot obtain an adequate closed reduction, make a small
anterior incision to facilitate the reduction. -
Drive two K-wires from the nonarticular
aspect of the talar body into the talar head to hold the reduction, and
reassess the reduction with standard radiographs if needed (53). -
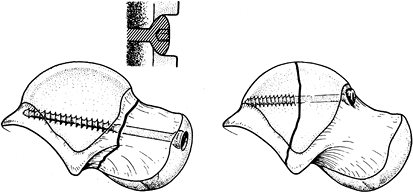
Achieve rigid fixation with dual 4.0 mm cancellous screws, entering just lateral to the posterior process (Fig. 110.6).
Be certain that threads extend past the fracture site but not into the
talonavicular joint. Try to place screws perpendicular to the fracture
plane for maximal compression. With the advent of cannulated screws,
talar neck fractures can be rigidly fixed percutaneously using a single
6.5 mm cancellous screw entering through the posterior, nonarticular
part of the talus (20).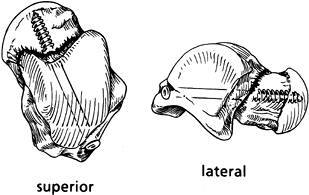 Figure 110.6.
Figure 110.6.
Posterior cancellous screw fixation of a talar neck fracture. Notice
that the screw enters the nonarticular aspect of the posterior talus.
It passes directly through the center of the talar neck, as
perpendicular to the fracture plane as possible. (From Adelaar RS.
Fractures of the Talus. Instr Course Lect 1990;34:147, with permission.)
dislocations because it allows osteotomy of the medial malleolus,
facilitating reduction of the dislocated body (or fixation of
concomitant medial malleolar fractures).
-
Place the patient in the supine position
with a sandbag under the contralateral buttock and with the affected
extremity in a figure-four position. Make a 6 cm longitudinal incision
between the medial malleolus and the Achilles tendon (Fig. 110.7), taking care to carefully isolate the neurovascular bundle (Fig. 110.8). Carry dissection posterior to posteromedial neurovascular structures.![]() Figure 110.7. Make the skin incision for the posteromedial approach to the talus between the medial malleolus and Achilles tendon.
Figure 110.7. Make the skin incision for the posteromedial approach to the talus between the medial malleolus and Achilles tendon.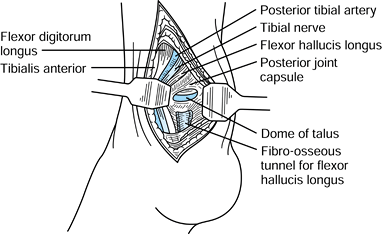 Figure 110.8. Posteromedial approach to the talus. (From Hoppenfeld S, deBoer P.Surgical Exposures in Orthopaedics: The Anatomic Approach. Philadelphia: Lippincott, 1984:487, with permission.)
Figure 110.8. Posteromedial approach to the talus. (From Hoppenfeld S, deBoer P.Surgical Exposures in Orthopaedics: The Anatomic Approach. Philadelphia: Lippincott, 1984:487, with permission.) -
To reduce the dislocated talar body, place a Steinmann pin in the calcaneus for axial traction if needed.
-
If you still cannot reduce the dislocated
body, dissect subcutaneously and perform a medial malleolar osteotomy.
To osteotomize the medial malleolus, predrill screw holes for
reattachment. Perform the osteotomy at 30° to 45° from the plane of the
articular surface, toward the medial corner of the tibial plafond. Take
care not to disrupt the tenuous deltoid ligament blood supply. -
After reducing the talar body, develop
the interval between the flexor hallucis longus and the peroneus
tendons. The flexor hallucis longus occasionally needs to be dislocated
medially out of its groove. -
Proceed with reduction and fixation of the fracture as described for the posterolateral approach.
-
Reattach the medial malleolus with dual 4.0 mm cancellous screws (30).
anteromedial or an anterolateral incision. The anteromedial approach is
most widely used and can be combined with medial malleolar osteotomy to
improve exposure, or it can be used to fix concomitant medial malleolar
fractures.
-
Make a curvilinear incision just medial to the tibialis anterior tendon (Fig. 110.9). Take care to avoid the saphenous vein and nerve. Carry the dissection down to the ankle joint capsule and neck of the talus.
![]() Figure 110.9. For the anteromedial approach to the talus, make a curvilinear incision just medial to the tibialis anterior tendon.
Figure 110.9. For the anteromedial approach to the talus, make a curvilinear incision just medial to the tibialis anterior tendon. -
Dissect subcutaneously to perform a medial malleolar osteotomy, if necessary (Fig. 110.10).
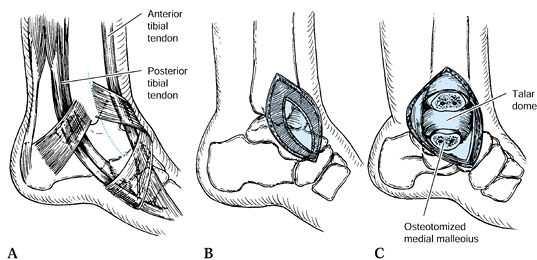 Figure 110.10. Anteromedial approach to the talus. A: Skin incision in relationship to the deep structures. B: Incise the deep fascia and open the ankle joint capsule. C:
Figure 110.10. Anteromedial approach to the talus. A: Skin incision in relationship to the deep structures. B: Incise the deep fascia and open the ankle joint capsule. C:
Osteotomize the medial malleolus with a sharp osteotome just distal to
the plafond of the tibia if further exposure is required. (From Mayo
KA. Fractures of the Talus: Principles of Management and Techniques of
Treatment. Tech Orthop 1988;3:42, with permission.) -
Achieve rigid fixation using 4.0 mm
cancellous screws placed through the nonarticular talar neck, or
directly through the talar head after countersinking (Fig. 110.11).![]() Figure 110.11. Anterior screw fixation of a talar neck fracture. A: Screws placed through the articular cartilage must be countersunk below the articular surface. B:
Figure 110.11. Anterior screw fixation of a talar neck fracture. A: Screws placed through the articular cartilage must be countersunk below the articular surface. B:
The preferred fixation, if possible, is through the neck of the talus.
(From Grob D, Simpson LA, Weber BG, Bray T. Operative Treatment of
Displaced Talus Fractures. Clin Orthop 1965;199:88, with permission.)
-
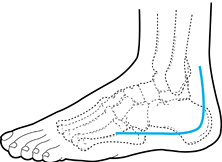
Make a slightly curved incision from 2 cm anterior to the distal aspect of the fibula toward the fourth metatarsal base (Fig. 110.12).
 Figure 110.12.
Figure 110.12.
For the anterolateral approach to the talus, make a curvilinear
incision just anterior to the lateral malleolus, toward the fourth
metatarsal base. -
Incise the fascia and extensor retinaculum, taking care to preserve any branches of the superficial peroneal nerve.
-
Dissect lateral to the extensor digitorum
longus and peroneus tertius tendons. The sinus tarsi and talar neck can
be exposed by retracting these tendons medially (Fig. 110.13).![]() Figure 110.13. Anterolateral approach to the talus. A: Skin incision in relationship to the deep structures. B:
Figure 110.13. Anterolateral approach to the talus. A: Skin incision in relationship to the deep structures. B:
Incise the extensor retinaculum and capsule lateral to the extensor
tendons and expose the tarsal sinus and talar neck. (From Mayo KA.
Fractures of the Talus: Principles of Management and Techniques of
Treatment. Tech Orthop 1988;3:42, with permission.) -
Reduce the fracture as described for the
anteromedial approach, and stabilize it using 4.0 mm cancellous screws
placed through the talar neck into the body.
gaping occurs on the contralateral side of single-sided anterior
fixation constructs. The mechanics of screw fixation
placed
either laterally or medially may cause the fracture to gape open on the
other side, resulting in malreduction or instability. Therefore,
combined anterolateral and anteromedial approaches provide the
advantages of both approaches and rigid, anatomic reduction and
debridement of the subtalar joint. The surgical technique is exactly
the same as described for the approaches performed individually. To
date, there is little scientific evidence that suggests the
two-incision approach provides better functional outcomes than any of
the other techniques. There may be a biomechanical advantage to
fixation if small miniplates are used bilaterally, rather than screws
as commonly described.
wounds are healed. If rigid fixation has been achieved, institute early
ankle and subtalar motion using a removable fracture brace or splint
once soft tissues are healed, generally by 10–14 days. Begin
progressive weight bearing in a removable brace when fracture union is
evident, usually by 6–8 weeks.
necrosis and infection. Skin necrosis is generally seen only with type
III and IV fractures, and it can be minimized by prompt reduction of
the talar body. Infection may occur after open injuries but can often
be avoided by early irrigation and debridement, rigid fracture
fixation, delayed wound closure, and prophylactic antibiotics. However,
if the talar body is completely avascular, an established osteomyelitis
may be resistant to treatment (55).
malunion, and posttraumatic arthritis. Absence of avascular necrosis
can often be recognized at 6–8 weeks by the presence of subchrondral
atrophy in the dome of the talus (Hawkins’ sign) (41). Its absence, however, is not a definite indicator of avascular necrosis (18),
nor does its presence rule out small areas of necrosis. Magnetic
resonance imaging (MRI) is the most useful modality for diagnosing
avascular necrosis. However, MRI requires the use of nonferromagnetic
screws (1) because it cannot be used after internal fixation with stainless steel screws (53).
amount of vascular disruption. Type I fractures have minimal arterial
disruption, with rates of avascular necrosis of 0% to 13%. Some authors
have postulated that avascular necrosis in this group is caused by an
occult, displaced injury that spontaneously reduces (81).
Type II fractures have moderate disruption of vascular channels and
avascular necrosis rates of 20% to 50%. Type III and IV fractures have
disruption of most arterial sources, with avascular necrosis rates of
up to 100%.
necrosis is probably the result of differences in methods of detection
and methods of acute fracture management. Several series (17,24,32,38,86) report lower rates of avascular necrosis with open reduction and internal fixation (ORIF).
stems from the finding that not all avascular tali go on to collapse,
and that those destined to collapse often do so only after a number of
years (17,18,41). Although no study has unequivocally proved that protected weight bearing reduces the likelihood of collapse, many authors (30,53,86) recommend use of a patellar tendon-bearing brace until the revascularization process is complete. Davis et al. (29)
showed a decrease in weight transmitted across the ankle joint with
this brace. If the avascular process involves only a portion of the
talar body, allow full weight bearing in a cast or brace that
neutralizes varus–valgus ankle stresses (24).
alternatives include tibiocalcaneal fusion with or without
interposition iliac crest bone grafting, and the Blair tibiotalar
fusion (8,31,50,53,59,77).
The Blair fusion is generally preferred because it preserves heel
height, maintains the medial longitudinal arch, and allows for some
hindfoot motion (1,30,53,81).
However, if the talar head cannot be salvaged, tibiocalcaneal fusion
with interposition iliac crest bone grafting provides a stable hindfoot
in most cases.
neck fractures, but nonunions are rare, generally occurring in less
than 1% of fractures (71). The incidence is even lower when rigid internal fixation is used (24,53,81). Malunions are more common, reported in up to 27% in some series (18,20). Most are either dorsal or varus malunions, and anatomic reduction with rigid internal fixation reduces the incidence (18,20,55).
Dorsal “beak” resections have been successful for symptomatic dorsal
malunions, and triple arthrodesis has been used to treat varus
malunions (20).
Causes are initial traumatic damage to the articular cartilage,
avascular necrosis, and fracture malunion. Arthrofibrosis and loss of
motion can be minimized by promoting venous drainage with elevation of
the extremity in the early postoperative period, and by early
mobilization of the ankle and subtalar joints (55).
Subtalar or triple arthrodesis is indicated for symptomatic subtalar
arthritis, and tibiotalar arthritis is best managed by ankle
arthrodesis. Take care to accurately localize the symptomatic joint
before proceeding with arthrodesis (18).
Large forces are required to fracture the body. Because of its crucial
role in the ankle and subtalar joints, any residual incongruity may
cause symptoms. Although the mechanism of injury and general morphology
of these fractures are similar to those of talar neck fractures, the
prognosis is generally worse, and therefore we consider these fractures
separately (23,57,83).
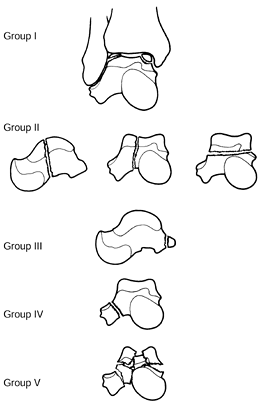
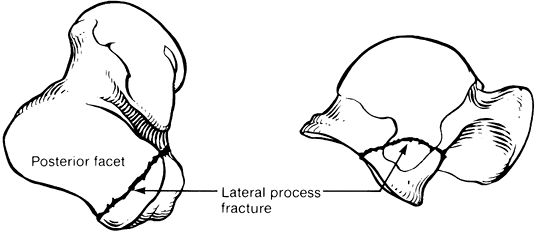
into five groups: I, transchondral dome fractures; II, shear fractures;
III, posterior tubercle fractures; IV, lateral process fractures; and
V, crush fractures (Fig. 110.14). Shear
fractures can be further subdivided into coronal, sagittal, and
horizontal fractures. Only shear (II) and crush (V) fractures are
discussed in this section; groups I, III, and IV will be considered
separately.
 |
|
Figure 110.14. Classification of talar body fractures. (From Delee JC. Fractures and Dislocations of the Foot. In: Mann RA, ed. Surgery of the Foot, 5th ed. St. Louis: Mosby, 1986:656, with permission.)
|
closed treatment when displacement is minimal (less than 2 mm). Apply a
short-leg, non-weight-bearing cast for 6–8 weeks or until union is
apparent. If the fracture fragments appear stable, begin cautious early
motion using a removable fracture brace or splint before this time, if
desired. Thereafter, begin progressive weight bearing in a removable
fracture brace. Manage displaced horizontal shear fractures with closed
treatment if a satisfactory closed reduction
can be obtained using a combination of calcaneal pin traction and manipulation (9). Immobilize in a short-leg, non-weight-bearing cast until union occurs.
fractures when comminution is limited. For shear fractures in the
coronal plane, operative approaches, fixation techniques, and
postoperative management are essentially identical to those described
for talar neck fractures (1). Because of the
larger anterior fragment, these fractures often are more amenable to
posterior screw fixation than are neck fractures. Shear fractures in
the sagittal plane can be fixed with screws through an anteromedial or
anterolateral approach. Medial malleolar osteotomy may be necessary for
adequate visualization and internal fixation (32).
Irreducible horizontal shear fractures can be managed by open reduction
with or without pin or screw fixation. Be certain that pins or screw
heads are countersunk below the articular surface. Herbert screws
through the articular surface provide satisfactory fixation of these
fractures.
have recommended primary talectomy, tibiocalcaneal fusion, pantalar
arthrodesis, and Blair fusion for irreparable fractures. Primary
talectomy should rarely be performed acutely because it may compromise
subsequent reconstruction, and no harm results when definitive
treatment is delayed. Tibiocalcaneal fusion results in loss of heel
height and medial longitudinal arch, whereas pantalar arthrodesis
precludes hindfoot motion. With severe collapse of the talar body, the
Blair tibiotalar fusion maintains heel height, preserves the medial
longitudinal arch, and allows for some tibiopedal motion (1,8,30,31,50,59,81).
those seen with talar neck fractures: avascular necrosis, nonunion,
malunion, arthrofibrosis, and posttraumatic arthritis of the ankle and
subtalar joints. However, the incidence of these complications is
higher with talar body fractures, leading to a larger proportion of
poor results.
fractures is about 25% for nondisplaced fractures, 40% to 50% for
displaced fractures, and 90% for displaced fractures with complete
dislocation of the body (30,57,83).
Because these fractures occur more posteriorly than talar neck
fractures, and because the fracture line may exit medially through the
deltoid ligament attachment, even minimal displacement may result in
complete avascularity of the talar body. In horizontal shear fractures,
the incidence of avascular necrosis of the dome is even higher due to
complete isolation from all vascular sources (9).
in those developing avascular necrosis; nonunion is rare after talar
body fractures (57). Malunion can develop in up to one third of displaced fractures when inadequately reduced (83).
body fractures because the fracture line passes through both the talar
dome articular surface and the posterior facet of the subtalar joint.
Other causes of arthritis include acute cartilaginous injury, malunion,
and avascular necrosis (11,23,83). Sneppen et al. (83) found a 75% incidence of degenerative arthritis in fractures that healed without displacement.
to 10% of all talus injuries. These fractures result from longitudinal
compression of a plantar-flexed foot, with or without a simultaneous
abduction or adduction
force (23,69).
Fractures are either a compression type or a split in the longitudinal
or oblique plane. Because the head of the talus is well vascularized,
avascular necrosis is uncommon (1).
non-weight-bearing cast with a well-molded arch for 6–8 weeks until
union occurs. Displaced fractures often require surgical intervention.
If the fracture fragment involves more than half of the articular
surface, ORIF through an anteromedial approach is usually preferred,
whereas if the fracture involves less than half of the articular
surface, excision is often the best treatment. Late problems include
talonavicular joint arthrosis and midtarsal instability (1).
Known by several terms (transchondral fracture, osteochondral fracture,
flake fracture, osteochondritis dissecans), these lesions are most
likely traumatic in origin (7,64,65,75,76). Many affected patients are treated originally for sprains or more serious ankle injuries (2,4).
Characteristic locations are the anterolateral and posteromedial talar
dome, with roughly equal proportions in each location (7,19,76). Lateral lesions are typically wafer like or flakelike, whereas medial lesions are often cup-shaped (19) (Fig. 110.15).
 |
|
Figure 110.15.
Classic locations and configurations of transchondral dome fractures. (From Delee JC. Fractures and Dislocations of the Foot. In: Mann RA, ed. Surgery of the Foot, 5th ed. St. Louis: Mosby, 1986:656, and redrawn from Canale ST, Belding RH. J Bone Joint Surg Am 1980;62:97, with permission.) |
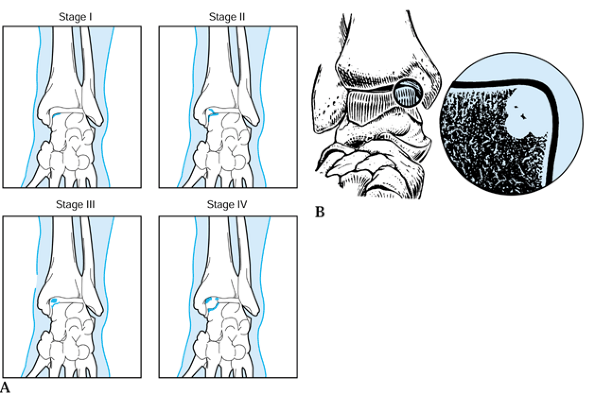
classified transchondral dome fractures. Stage I lesions involve a
small area of subchondral compression of the talar dome. Stage II
lesions are partially detached osteochondral fragments. Stage III
lesions are completely detached, with the fragment remaining within the
crater formed by its detachment. Stage IV lesions are completely
detached, with the fragment displaced from its original location (Fig. 110.16A). Recently, with the advent of better imaging techniques, including CT and MRI, Fisher et al. (35) have added stage V, the radiolucent defect (subchondral cyst) (Fig. 110.16B).
They found, using these imaging techniques, that 80% of osteochondral
lesions were purely cavitary, with no associated bony or cartilaginous
fragments in the joint.
 |
|
Figure 110.16. Classification of transchondral dome fractures. (From Canale ST, Belding RH. Osteochondral Lesions of the Talus. J Bone Joint Surg Am 1980;62:97, with permission.)
|
fractures were largely evaluated using plain radiographs and tomograms.
Plain radiographs, although mandatory in the evaluation of these
lesions, are often negative (4,35). Bone scanning is an excellent screening tool because it has a sensitivity for these lesions approaching 100% (35). Further evaluation requires MRI when radiographs are negative, or CT scans when bony involvement is seen on radiographs (4,35).
MRI can detect cartilaginous lesions or areas of subchondral
compression (stage I lesions), and CT scanning can delineate cavitary
lesions (stage V) or assess displacement of osteochondral fragments
(stage II, III, and IV lesions).
recommend a trial of immobilization even for chronic, nondisplaced
lesions. Operative treatment is indicated for persistent symptoms after
an adequate trial of conservative treatment or when the osteochondral
fragment is displaced.
fragment when present and drilling of the defect to promote
revascularization and fibrocartilaginous metaplasia (28,64,76,81). Only acute lesions involving at least one third of the medial or lateral dome are treated by ORIF.
Fibrin adhesives and absorbable pins have recently been developed for this use.
anteromedial approach with osteotomy of the medial malleolus or through
a posteromedial approach without osteotomy of the medial malleolus (35). Lateral lesions can be reached through a standard anterolateral approach.
transchondral dome fractures. Arthroscopic removal of loose fragments,
curettage, debridement, and drilling of the defect greatly reduce
postoperative morbidity as compared to open treatment (2,94) (see Chapter 93).
ROM exercises is recommended after arthroscopic or open treatment of
transchondral dome fractures (2,30,94). After internal fixation of larger transchondral dome fragments, delay weight bearing until fracture union is present (81).
of transchondral dome fractures are limitation of ankle motion and
posttraumatic arthritis. Results are influenced by the stage, location,
and size of the lesion; weight and activity level of the patient; type
of treatment; and extent of delay in treatment (75,76,81).
In general, nondisplaced lesions have a more favorable prognosis than
displaced lesions, with results of medial lesions being superior to
lateral lesions in some series (75). A delay in treatment longer than 12 months may worsen the prognosis (65). Several authors (2,7,19,65,76) suggest that surgically treated lesions have a better prognosis than those that are not surgically treated.
It articulates with both the distal fibula and the posterior facet of
the calcaneus and serves as the attachment point for several ligaments,
including the anterior taliofibular and lateral talocalcaneal
ligaments. Fractures of the lateral talar process account for 24% of
talar body fractures (81).
 |
|
Figure 110.17.
Lateral talar process fracture. Note the involvement of the articular surfaces for both the talofibular and subtalar joints. (From Delee JC. Fractures and Dislocations of the Foot. In: Mann RA, ed. Surgery of the Foot, 5th ed. St. Louis: Mosby, 1986:656, with permission.) |
combination of forced dorsiflexion and inversion, a mechanism similar
to that causing lateral ankle sprains (40,60). Indeed, the signs and symptoms of lateral process fractures and lateral ankle sprains are almost identical. Therefore,
this injury should be considered when any patient complains of posttraumatic lateral ankle pain.
views of the ankle. A 20° internal oblique view of the ankle best
demonstrates this fracture (60). Tomograms and CT scans are also useful in delineating fracture fragment size and displacement (30).
nondisplaced fractures. Because the lateral process involves a
weight-bearing surface, 4–6 weeks in a short-leg, non-weight-bearing
cast is generally recommended (40,81,83).
Some recommend attempted closed reduction of displaced fragments, and
others recommend open reduction because of the difficulty in obtaining
a satisfactory closed reduction (30,40,81).
large, displaced fragments; small or comminuted fragments are best
treated by excision (40,60).
Lateral process fractures can be successfully reached through a
modified anterolateral approach. Begin the incision 5 cm proximal to
the ankle joint, curving just distal to the tip of the fibula (30). Rigid internal fixation with a cancellous screw is generally preferred.
ankle for 2–3 weeks. Thereafter, allow ROM exercises using a removable
splint. After ORIF, allow weight bearing when union is demonstrated
radiographically, usually by 6 weeks. After excision, allow progressive
weight bearing at 3 weeks (30).
Nonunion, malunion, or impingement are indications for exploration and
fragment excision or subtalar arthrodesis if significant arthritis is
present (40,81).
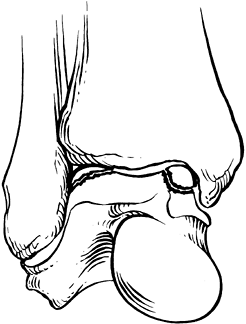
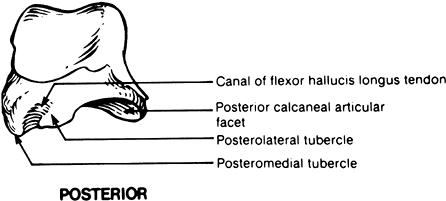
and lateral tubercles separated by a groove for the flexor hallucis
longus tendon (Fig. 110.18). The lateral
tubercle serves as the attachment for the posterior talofibular
ligament. Lateral tubercle fractures are much more common than medial
tubercle fractures and must often be distinguished from a commonly
found accessory bone, the os trigonum (54). The
mechanism of injury for fractures of the lateral tubercle of the
posterior process is either forced plantar flexion with impingement
against the tibial plafond or forced dorsiflexion with avulsion of the
tubercle by the posterior talofibular ligament (30).
 |
|
Figure 110.18.
Medial and lateral tubercles of the posterior talar process. (From Delee JC. Fractures and Dislocations of the Foot. In: Mann RA, ed. Surgery of the Foot, 5th ed. St. Louis: Mosby, 1986:656, with permission.) |
lateral tubercle. An acute fracture can be distinguished from a normal
os trigonum by technetium bone scanning (68).
treated by 6 weeks of cast immobilization. Most authors recommend
non-weight-bearing because the inferior surface normally articulates
with the calcaneus. Symptomatic
chronic injuries can often be successfully treated with a course of cast immobilization (30,68).
excision of the posterior process fragment is indicated. This can be
done through either a posterolateral or a posteromedial approach. ORIF
can be considered for acute fractures of large fragments (30,68).
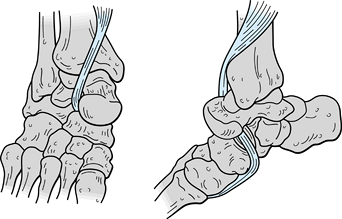
dislocation of both the talonavicular and the talocalcaneal joints,
resulting in disruption of joint capsules, the interosseous
talocalcaneal ligament, and additional supporting structures both
medially and laterally. These injuries are rare and result from
high-energy mechanisms (12).
lateral, anterior, or posterior, depending on the direction of
displacement of the foot with respect to the talus. Medial dislocations
are by far the most common, making up 80% of all subtalar dislocations (12). The talus may also rarely undergo total dislocation from the subtalar and ankle joints.
lateral, and oblique radiographs are not obtained and carefully
studied. An AP view of the foot often discloses a medial or lateral
subtalar dislocation by the absence of the talar head in the concavity
of the navicular (5).
reduction and cast immobilization. Reduce the dislocation by flexing
the knee, applying gentle traction to the forefoot, accentuating the
deformity to unlock the dislocation, and reversing the deformity.
Digital pressure over the talar head may aid in reduction of medial or
lateral dislocations (11). After reduction,
immobilize the foot in a short-leg, non-weight-bearing cast for 4–6
weeks, followed by progressive weight bearing and range of motion (ROM)
(81).
buttonholing of the talar head through the joint capsule or tendons.
Medial dislocations are most commonly entrapped by extensor tendons,
whereas lateral dislocations may be entrapped by the posterior tibial
tendon (47) (Fig. 110.19).
When you cannot reduce these injuries closed, perform open reduction
through a longitudinal incision over the talar head, followed by gentle
unlocking of the involved structures and reduction of the dislocation.
Postoperative
management is similar to that for closed reduction.
 |
|
Figure 110.19.
This lateral subtalar dislocation is irreducible because of entrapment by the tibialis posterior tendon, which has slipped out of its normal position in the groove of the posterior tibia. (From Leitner B. Obstacles to Reduction in Subtalar Dislocations. J Bone Joint Surg Am 1954;36:304, with permission.) |
degrees of subtalar arthrosis and loss of motion, instability can be an
even greater clinical problem, particularly in younger patients (12,95). Recurrent dislocation during cast immobilization has been reported (44).
Therefore, some authors recommend a full 6 weeks of cast immobilization
for young, active patients, whereas 4 weeks may be adequate for older
patients. Symptomatic subtalar arthritis can be managed by subtalar or
triple arthrodesis (44). Avascular necrosis occurs in less than 5% of these injuries (95).
fractures are difficult. The nondisplaced neck fracture can be treated
nonoperatively; however, serial radiographs must be frequently and
closely examined. Minimal degrees of displacement affect adversely the
force distribution in the subtalar joint. A minimally displaced type II
fracture can be treated successfully by closed reduction and posterior
screw placement. Laboratory studies have confirmed better mechanical
stability by posterior screw placement, and, by placing the screws in
the central axis of the bone, no medial or lateral gaping occurs. Types
III and IV fractures are probably best treated by combined approaches
and dual fixation. This technique allows anatomic reduction and
debridement of the subtalar joint with placement of stable fixation.
New miniplate constructs placed medially and laterally just inferior to
the articular surface may provide the most rigid fixation.
fracture frequently is incomplete and asymptomatic. Positive imaging
studies should not be of major concern. It has been shown that small
areas of focal avascular necrosis are well tolerated by the joint and
can result in an excellent, functional outcome.
joint function is still best treated with ankle arthrodesis. Creative
hindfoot fusions are required because obtaining a fusion in the
presence of avascular bone can be difficult. Therefore, techniques such
as interpositional bone grafting, calcaneal–tibial arthrodesis, and
bone transport techniques have all been described.
arthroscopic techniques. Utilizing ankle distraction, visualization of
the talus is excellent enough to allow drilling and fixation.
Biodegradable pins are useful.
treatment of fractures of the calcaneus whenever it is possible and
advisable. However, frustration in treatment of these fractures has led
many to abandon attempts at open reduction, and instead to treat these
difficult fractures by elevation of the foot, compression dressing, and
early motion. The end result is usually a bulbous heel that will not
fit a shoe properly; a short heel in valgus with a relatively short
heel cord; a mass of bone laterally producing impingement on the
peroneal tendons; and disruption of the subtalar joint, which may
result in traumatic arthritis.
results of treatment of calcaneus fractures over the years have not
been good. It is logical to assume that patients are better off with an
anatomic or near-anatomic reduction than to be left with the
deformities. The more anatomic the reduction, the better the functional
results you can expect. Regardless of the fracture type and method of
treatment, always try to restore the normal width of the heel as well
as the length and height of the calcaneus.
articular surfaces are located on the dorsal aspect of its anterior
half (58). The posterior half, the tuberosity,
provides the site of insertion of the Achilles tendon. It inserts about
midway down the posterior aspect of the tuberosity with a small bursa
located between the tendon and the calcaneus in the superior portion.
The plantar fascia originates from the medial and lateral processes
located on the plantar aspect of the tuberosity. The calcaneal portion
of the subtalar joint is made up of a posterior facet, which is the
largest and is convex in shape; it is separated by the tarsal sinus and
the tarsal ligament from the middle and anterior facets, which are
concave in shape and usually contiguous with each other. The middle
facet is located on the prominent medial projection of the anterior
calcaneus, called the sustentaculum tali. The anterior surface provides
a saddle-shaped articular surface for the cuboid. The calcaneus is
composed of dense cancellous bone covered by a very thin cortical
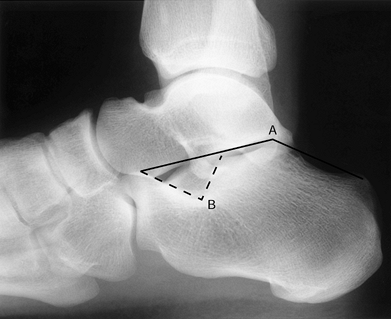
shell. On a lateral radiograph of the calcaneus (Fig. 110.20),
two important angles are used to help determine the quality of
reduction after fractures. Böhler’s tuber angle, measured by a line
drawn from the posterior superior prominence of the tuberosity to the
superior apex of the posterior facet to the superior aspect of the
anterior process, measures between 25° and 40° in most individuals.
Gissane’s angle, also known as the critical angle, is directly beneath
the lateral process of the talus
and
is where axial compressive forces are applied by the talus during
vertical loading, which is the most common mechanism of injury for
fractures of the calcaneus.
 |
|
Figure 110.20. Lateral view of the calcaneus. A: Böhler’s tuber angle. B: Crucial angle of Gissane.
|
calcaneus is a direct blow to the plantar aspect of the heel from
either a fall or a severe deceleration injury such as in high-speed
motor vehicle accidents. Twisting forces are more likely to produce
extra-articular fractures such as those of the anterior process, the
sustentaculum, and the medial process. Fractures of the tuberosity are
usually caused by avulsion of the Achilles tendon insertion. Bilateral
fractures are usually caused by vertical loading of both lower
extremities. Remember that the calcaneal fractures are often associated
with fractures of cancellous bone in other portions of the skeleton,
particularly the thoracolumbar spine.
 |
|
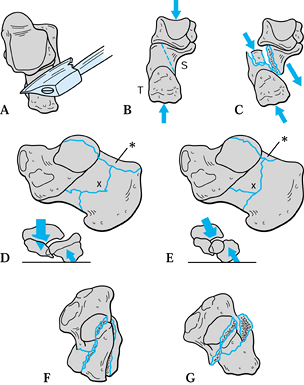
Figure 110.21. A: Superior view of the talus and calcaneus, showing the sharp posterolateral edge of the talus that produces the fracture. B: Posterior view of the talus and calcaneus. C: Posterior view of the talus and calcaneus after fracture. The fracture line is along the dotted line, as shown in (B). D: The calcaneus seen from the medial side, showing a tongue-type fracture. E: Medial view of the calcaneus, showing a joint depression–type fracture. F: Superior view of a tongue-type fracture. G: Superior view of a joint depression–type fracture.
|
It drives down across the calcaneus like an axe, producing a
corresponding oblique fracture line through the calcaneus. The center
of the tuberosity is slightly offset lateral to the center of the
talus, so if a force is applied to the top of the talus with the
tuberosity fixed to the ground, a shear line develops, as shown in Figure 110.21B. This shear line consistently produces a sustentacular fragment (S in Fig. 110.21B) and a tuberosity fragment (T in Fig. 110.21B).
underside of the talus by the talocalcaneal ligaments. Therefore, the
sustentacular fragment remains attached to the talus and descends with
it (Fig. 110.21C), while the tuberosity fragment, which has no ligamentous attachments, is unstable and moves laterally and upward. The star in Figure 110.21C
shows production of either a tongue-type or a joint depression–type
fragment by the descending posterolateral edge of the talus.
is long and extends to the posterior part of the tuberosity. The joint
depression–type fragment is short and extends just posterior to the
posterior facet (star in Fig. 110.21E).
The fractures are quite similar both in the shape of the sustentacular
fragments and in the path of the fracture line through the lateral part
of the posterior facet. The major difference in the fractures is the
length of the superolateral fragments.
show the displacement of the fragments. The tongue-type fragment is
depressed in front and elevated to the rear, and the joint
depression–type fragment is pushed straight down and rotated so that
the articular cartilage of the fragment faces forward.
tongue-type fracture from above. The fracture line runs through the
lateral part of the posterior facet and parallels the posterolateral
edge of the talus. The front of the tongue is depressed, leaving an
offset in the posterior facet surface. Figure 110.21G
shows the short joint depression–type fragment depressed into the body
of the calcaneus, leaving an offset in the posterior facet surface.
This fragment is also rotated downward in front.
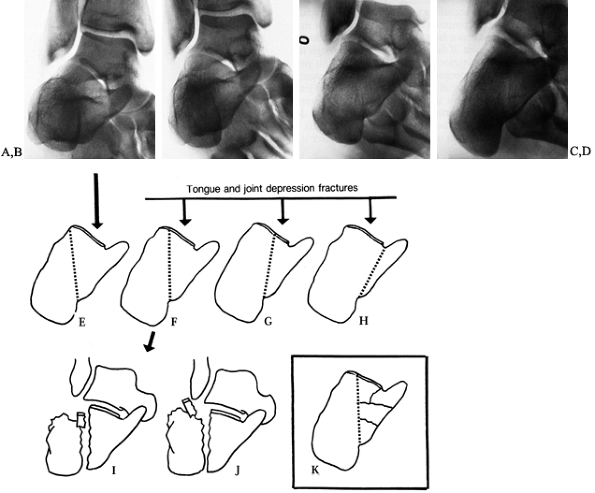
calcaneus fractures are the lateral, tangential, and Broden’s views.
Broden’s views are oblique views made with the leg internally rotated
45°. Four views are made, at 10°, 20°, 30°, and 40° distal to the
perpendicular with the x-ray beam centered on the sinus tarsi. Figure 110.22A, Figure 110.22B, Figure 110.22C and Figure 110.22D show these views of a normal foot. The 10° view (Fig. 110.22A) shows the posterior aspect of the joint. The 20° and 30° views show the central part (Fig. 110.22B and Fig. 110.22C), and the 40° view shows the anterior aspect (Fig. 110.22D).
The location of the fracture line in relation to the posterior facet can be determined from these views.
 |
|
Figure 110.22. A: Broden’s view of a normal heel made at 10°. B: Broden’s view of a normal heel made at 20°. C: Broden’s view of a normal heel made at 30°. D: Broden’s view of a normal heel made at 40°. E–H:
Classification of the tongue-type and joint depression-type fractures is made according to the location of the fracture line in relation to the posterior facet, as shown in the 30° Broden’s views. I: The fragment is depressed, leaving a step in the posterior facet surface. J: The fragment has slipped upward and from under the talus to lie at the tip of the lateral malleolus. K: Fracture with comminution of the sustentacular fragment. |
concluded that two-dimensional CT scans tend to overestimate the degree
of comminution, whereas conventional radiographs provide an
underestimation. Three-dimensional reconstructions from CT scans were
superior, except in their somewhat poor resolution of intra-articular
pathology. Carr et al. (21) proposed that
three-dimensional CT reconstructions were most useful in preoperative
planning to assist an inexperienced surgeon in learning to interpret
the standard plain films. An experienced surgeon can analyze the
fracture pattern and plan a procedure based on the standard lateral,
tangential, and Broden’s views without the need for CT. The surgeon
must be familiar with Broden’s views and must be able to interpret
them, because they are used in surgery to determine whether the
depressed fragment has been elevated properly; the CT scan cannot be
used in surgery.
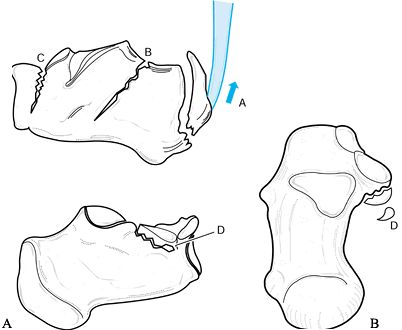
extra-articular and intra-articular fractures. Extra-articular
fractures make up 25% to 30% of all calcaneal fractures (25,26)
and include fractures of the anterior process, beak or avulsion
fractures of the tuberosity, medial process fractures, and fractures of
the sustentaculum tali and body (Fig. 110.23).
 |
|
Figure 110.23. A: Lateral and medial views of the calcaneus. B: Superior axial view of the calcaneus. A, avulsion fracture of tuberosity; B, body fracture; C, anterior process fracture; D, fracture of sustentaculum tali.
|
tongue-type fractures can be made according to the location of the
fracture line in relation to the posterior facet (14). The fracture line may run lateral to the posterior facet (Fig. 110.22E), producing no damage to the joint. If the fracture line runs through the lateral part of the posterior facet (Fig. 110.22F), it produces a classic joint depression–type or tongue-type fracture, as described by Essex-Lopresti (34).
Because the tongue-type or joint depression–type fragment is relatively
small and contains only a small part of the articular facet, it is not
always depressed into the body of the calcaneus (Fig. 110.22I). It may slip laterally out from under the talus and displace upward (Fig. 110.22J).
but it still produces a classic tongue-type or joint depression–type
fracture, but with a larger fragment containing more of the posterior
facet cartilage.
posterior facet and produce a large tongue- or joint depression–type
fragment, which will contain the entire posterior facet (Fig. 110.22H).
Before beginning surgery, obtain Broden’s views or a CT scan so that
you will know what type of fracture you are dealing with.
fractures to operatively reduce and internally fix. There has been
great debate in the literature as to whether combinations of medial
approaches, lateral approaches, or dual approaches provide the best
opportunity to attain anatomic reduction (14,15,30,56,66,67,84). Treatment options for calcaneal fractures include the following:
-
No reduction, with elevation of the foot, compression dressing, and early ROM.
-
Closed reduction, with elevation of the foot, compression dressing, and early motion.
-
Percutaneous reduction techniques such as Essex-Lopresti (34).
-
Open reduction and internal fixation as popularized by Palmer (67) and McReynolds (56).
-
Primary arthrodesis.
overall shape of the calcaneus to as close to anatomic position as
possible. Anatomic restoration of the articular surface is rarely
possible by closed techniques, but it is worth trying as it is
occasionally successful. The goals of ORIF are to safely restore the
anatomy of the hindfoot. This
includes anatomic reduction of the articular facets (61);
reconstitution of hindfoot height, width, and length; and realignment
of the tuberosity to appropriate axial alignment. The entire osseous
morphology of the hindfoot must be anatomically reduced to provide the
best chance of good long-term outcomes.
the complex three-dimensional shape of the bone, ever-changing fixation
devices, open fractures, and osteopenic bone disease. Patients with
diabetes mellitus, hypertension, or peripheral vascular disease, and
tobacco chewers and smokers, have an increased incidence of wound
complications. Surgery in these patients may be contraindicated despite
the degree of injury to the calcaneus.
medial approach to fixation and stated that the key to a successful
reduction is restoration of the medial wall of the calcaneus by
realigning the medial cortex of the tuberosity fragment with the medial
cortex of the stable sustentacular fragment (14,15 and 16).
Although this helps to restore height and axial alignment, it is
difficult to reduce the posterior facet or address anterior
calcaneal–cuboid pathology from the medial side.
The calcaneal–cuboid joint and distal comminution can be addressed, as
well as the reduction of the posterior facet, the axial tuberosity
alignment, and the height and width of the hindfoot. Some surgeons (84)
have advocated mini-open medial approaches to assist in the reduction
of the tuberosity to the sustentacular fragment, then a more extensile
exposure laterally for the remainder of the pathology, including bone
grafting and lateral wall reduction. Because of the complications from
open approaches, there has recently been increased interest in
percutaneous reduction techniques with joysticks, small elevators, and
percutaneous cannulated screws, which are modifications of the original
Essex-Lopresti technique (34).
the insertion of any pins or fixation, is indicated in minimally
displaced fractures or in displaced fractures where percutaneous
reduction techniques or ORIF is contraindicated. Examples are in
patients with massive swelling and blood-filled fracture blisters on
the foot; for calcaneal fractures in patients with multiple injuries,
where only the minimum can be done initially because of the patient’s
unstable condition; in patients with systemic disease contraindicating
any type of intervention; or for local conditions of the foot, such as
skin ulcers or active infection, that contraindicate any type of
operative intervention. In addition, even when ORIF is anticipated to
occur eventually, if it cannot be done immediately, then closed
reduction under anesthesia may be useful to obtain initial alignment,
which improves venous and lymphatic return from the foot, decompresses
associated neurovascular structures, eliminates tenting of the skin,
and generally improves the condition of the foot for the subsequent
ORIF. However, remember that in general, except in neglected injuries
or after extremely severe crushing type injuries with major soft-tissue
damage, the earlier ORIF is carried out, the better the results. The
technique is as follows:
-
Administer a general or regional
anesthetic and perform the reduction under fluoroscopic control with a
C-arm. This is most easily done with the patient in the supine position
and the C-arm positioned with the flat surface of the receiver at the
foot of the table. By externally rotating the extremity at the hip, the
foot then can be placed in the lateral position on the C-arm for
visualization of the reduction. -
If there is a tongue depression–type
fracture, or the tuberosity is displaced superiorly, restoration of
Böhler’s angle and restoration of the tuberosity to its normal position
is the first step. In displaced fractures, this requires grasping the
tuberosity of the calcaneus in some manner. The simplest technique is
to prepare the heel and grasp the tuberosity percutaneously through the
skin with a large AO tenaculum-type bone-holding forceps, or large
tenaculum pelvic-reduction clamps. An alternative is to temporally
insert either a K-wire or a Steinmann pin and attach to it the
appropriate bow for applying traction. To reduce the tuberosity and
restore Böhler’s angle, simultaneously pull plantarward the forefoot
and the tuberosity of the calcaneus while visualizing the reduction on
the fluoroscope. This also usually restores axial alignment. -
Next, grasp the calcaneus between the
bases of both palms with your fingers interlocked beneath the heel.
Apply strong manual compression to reduce the lateral wall fragments
back into position, and position the tuberosity beneath sustentaculum
tali. Ensure that axial alignment is restored. -
Small 2.0 mm K-wires can be placed temporarily or long term for stabilization.
to restore displaced articular fragments. Although occasionally with
the maneuvers described here some intra-articular fractures will reduce
if the intra-articular fragments are attached directly to the major
fragments manipulated in the closed reduction.
these fractures, it is not feasible to hold reduction with a cast.
Fortunately, a significant majority are reasonably stable after closed
reduction if not subjected to forces that
would
displace them. After completion of the reduction, take AP, lateral,
axial, and Broden radiographic views to document the reduction. Then
apply a well-padded U-type short-leg splint along with a posterior
splint to maintain the foot in a neutral position. Overwrap the splints
with bias-cut stockinet.
level of the heart and observe closely for excessive swelling. The
dressings and splint often need to be split down to skin anteriorly
within the first 24 hours because of excessive swelling. Once the
swelling has resolved and prior to discharge from the hospital,
overwrap the splint. Between 2 and 3 weeks after injury, the swelling
will have subsided sufficiently, and a well-molded short-leg cast can
usually be applied. When sufficient consolidation has occurred (usually
by 6–8 weeks), the cast can be removed and the patient placed in a
prefabricated orthosis such as a Cam-walker. At this point, institute
ankle and foot joint ROM exercises. Delay weight bearing in most cases
until 10–12 weeks after injury.
involvement, they typically lose 50% or more of subtalar joint motion.
If the overall external anatomy of the calcaneus has been restored,
however, they will be able to successfully wear most types of shoes,
and the average urban dweller who usually walks on flat surfaces will
not complain of the loss of subtalar joint motion.
described a percutaneous technique for the reduction of fractures of
the calcaneus. It worked best for tongue-type fractures with minimal
intra-articular involvement, and it utilized a spline inserted into the
posterior aspect of the calcaneus to perform the reduction. Tornetta (92)
described its use for tongue-type fractures of the calcaneus. I have
modified this technique utilizing percutaneous manipulation of the
fracture fragments and internal fixation with percutaneous K-wires
and/or cannulated screws. This technique is indicated for displaced
fractures of the calcaneus when there is minimal or no intra-articular
involvement, or when formal ORIF is contraindicated. Elderly patients
with displaced fractures, if they are sedentary and will place limited
demands on their lower extremities, are excellent candidates for this
technique, particularly if they have any associated systemic diseases
or local extremity problems that would increase the rate of
complications after open reduction.
prior to surgery is essential. You must have a good feeling for the
three-dimensional anatomy of the fracture, in particular the size and
the position of the sustentaculum tali and the displaced
intra-articular fragments. Stability is achieved by the insertion of a
pin or cannulated fixation screw from an intact tuberosity fragment
into the sustentaculum tali. This fixation usually enters on the
posterolateral surface of the tuberosity of the calcaneus and passes
across the fracture site in an anterior-to-medial direction into the
sustentaculum. The preferred fixation is into the sustentaculum, as
this avoids crossing the mid-foot joints. If the sustentaculum is too
small or is comminuted, which is unusual, fixation can be extended into
the talus, navicular, or cuboid. I try to avoid this, however, as it
transfixes the intervening joints and damages somewhat the articular
cartilage. This technique is difficult on the severely swollen foot,
but it is achievable, particularly if the foot is overwrapped with a
compression dressing and a foot pump applied preoperatively to “milk”
edema out of the foot and heel. In addition, this technique is most
successful when the fracture hematoma is liquid, so it should be done
as soon as possible after the fracture occurs, preferably within the
first 12 hours. As time passes, the effectiveness of this technique
gradually diminishes; after 7 days, it may be ineffective because of
the firm organization of the fracture hematoma.
-
Administer a general or regional
anesthetic and place the patient in a supine position on a radiolucent
fracture table. Place a tourniquet on the upper thigh. This is usually
not required but is handy to have in place in case there is excessive
bleeding from the puncture wounds used for the technique. An
alternative technique is to use the lateral decubitus position,
particularly if implants will be inserted from the lateral side. -
As for the closed reduction technique
previously described, position a C-arm adjacent to the side of the foot
of the table on the affected side, with the large flat surface of the
receiver head level with the tabletop. Prepare and drape the extremity
from the tourniquet distally. -
First, perform a closed reduction as
described previously, as the initial repositioning of the fragments
makes the remainder of this procedure easier. -
Externally rotate the extremity at the hip and flex the knee to place the foot in the lateral position on the C-arm (49).
-
Beginning 1 cm proximal to the insertion
of the Achilles tendon into the calcaneus (note that this is about 50%
distalward on the posterior aspect of the calcaneus), make a vertical
midline posterior incision through the skin and subcutaneous fat
approximately 2 cm in length. -
Under fluoroscopic control, insert a
1¼-inch (6 mm) threaded Steinmann pin at or somewhat distal to the
proximal insertion of the Achilles tendon, slightly to the lateral side
of the midline of the calcaneus. Drill this in slowly under
fluoroscopic control, keeping the pin
P.2972
parallel
to the superior surface of the tuberosity fragment and directing the
pin in an anteromedial direction toward the sustentaculum tali. Since
the fracture is not fully reduced, this is technically the most
challenging part of the procedure. Insert the pin until it just exits
the tuberosity fragment into the fracture site (Fig. 110.24A).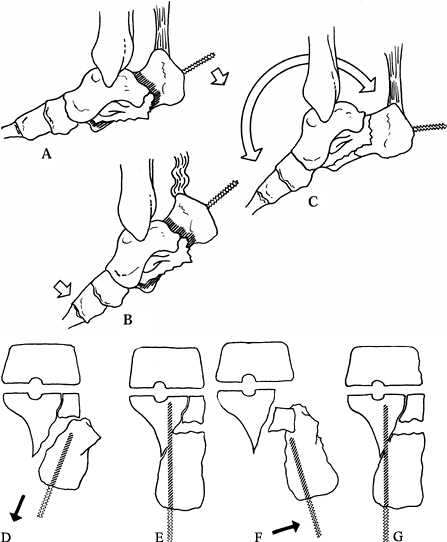 Figure 110.24. Modified Essex-Lopresti technique. Reduction aided by plantar-flexing the foot. A: Insert a Steinmann pin into the tuberosity up to the fracture. B: Plantar-flex the forefoot. C: Distract and lever the tuberosity distalward while maintaining forefoot plantar flexion. D: Use the pin in the tuberosity to also correct the axial alignment. E: Line up the medial cortex and insert the pin across the fracture into the sustentaculum fragment. F:
Figure 110.24. Modified Essex-Lopresti technique. Reduction aided by plantar-flexing the foot. A: Insert a Steinmann pin into the tuberosity up to the fracture. B: Plantar-flex the forefoot. C: Distract and lever the tuberosity distalward while maintaining forefoot plantar flexion. D: Use the pin in the tuberosity to also correct the axial alignment. E: Line up the medial cortex and insert the pin across the fracture into the sustentaculum fragment. F:
Where the lateral joint surface of the posterior facet is displaced,
the pin–tuberosity fragment unit can sometimes be used to manipulate
and elevate the articular surface. G: After reduction, insert the pin into the sustentaculum as described. -
If there is a depressed posterior facet
fragment, it is often possible to reduce it now, by running this pin
anteriorly under fluoroscopic control just beneath the displaced
fragment (Fig. 110.24F, Fig. 110.24G). -
If there is a depressed posterior facet
fragment that you feel cannot be reduced with the Steinmann pin, begin
reduction by making a puncture wound medially so that a small elevator
can be inserted percutaneously beneath the posterior facet fragment.
Take care to avoid injury to medial neurovascular structures and
tendons (Fig. 110.25).![]() Figure 110.25. Tricks for percutaneous reduction and fixation of more complex fractures. A: Percutaneously insert a small pin beneath the tenaculum into the tuberosity and use it to pry the tuberosity down. B: Then use lateral manual compression to reduce the lateral wall and restore axial alignment. C: Use an elevator to disimpact the lateral wall. D,E: Disimpact and derotate the tongue fragment. F,G: Use an elevator (can also be inserted from laterally) to elevate and derotate a depressed joint fragment. H–M: Reduce a tongue-type intra-articular fragment with Essex-Lopresti technique. Insert a pin into the tongue fragment (H). Reduce the fragment (I). Stabilize it by inserting the pin across the subtalar joint into the talus (J). Insert a second pin into the tuberosity fragment and reduce it (K). Stabilize the tuberosity by fixing it to the sustentaculum (L). Lateral view of the fixation (M).
Figure 110.25. Tricks for percutaneous reduction and fixation of more complex fractures. A: Percutaneously insert a small pin beneath the tenaculum into the tuberosity and use it to pry the tuberosity down. B: Then use lateral manual compression to reduce the lateral wall and restore axial alignment. C: Use an elevator to disimpact the lateral wall. D,E: Disimpact and derotate the tongue fragment. F,G: Use an elevator (can also be inserted from laterally) to elevate and derotate a depressed joint fragment. H–M: Reduce a tongue-type intra-articular fragment with Essex-Lopresti technique. Insert a pin into the tongue fragment (H). Reduce the fragment (I). Stabilize it by inserting the pin across the subtalar joint into the talus (J). Insert a second pin into the tuberosity fragment and reduce it (K). Stabilize the tuberosity by fixing it to the sustentaculum (L). Lateral view of the fixation (M). -
Next, perform a closed reduction. This
usually requires two surgeons, one manipulating the foot and the other
inserting the pins (Fig. 110.24B, Fig. 110.24C).
If you do not feel that manipulation of the tuberosity fragment with
the Steinmann pin alone will reduce the fragment, insert a second
transverse K-wire or Steinmann pin attached to an appropriate bow just
distal to the Essex-Lopresti pin. This will greatly aid in applying
traction to the tuberosity fragment to reduce it. The reduction
maneuver now involves traction on the tuberosity fragment to pull it
P.2973
distalward
to restore Böhler’s angle and to restore the length of the calcaneus,
while the forefoot is plantar-flexed. While holding the foot in this
position, pull the Essex-Lopresti pin plantarward to reduce the
tuberosity and help reduce the posterior facet. If necessary, use an
elevator beneath the facet to aid in the reduction (Fig. 110.25). -
Once the reduction is achieved on the
lateral view, gently pick the foot up off the C-arm and compress the
calcaneus laterally and medially to reduce the lateral wall and line up
the tuberosity with the sustentaculum tali (Fig. 110.26).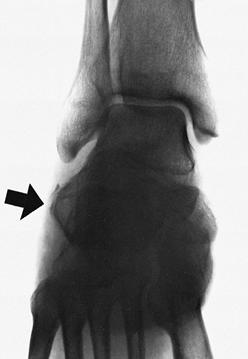 Figure 110.26. The large bulge of the lateral wall of the calcaneus (arrow) impinges on the peroneal tendons and must be reduced.
Figure 110.26. The large bulge of the lateral wall of the calcaneus (arrow) impinges on the peroneal tendons and must be reduced. -
Under fluoroscopic control, drill the
Steinmann pin forward into the sustentaculum fragment to secure the
reduction. If at this point the posterior facet fragment or other
components of the fracture are unstable and tend to redisplace
percutaneously, insert guide pins for cannulated screws or K-wires or
small Steinmann pins to control and fix the fragments (Fig. 110.24F, Fig. 110.24G). -
Once the guide pins, K-wires, and
Steinmann pins have been inserted and stability achieved, carefully
examine the calcaneus with the fluoroscope and plain radiographic
images. A good axial view of the calcaneus is essential to assess the
axial alignment of the calcaneus
P.2974
and
to ensure that the primary Steinmann pin is in the sustentaculum. As
mentioned before, if the sustentaculum does not offer sufficient
fixation or is too difficult to hit with the pin, then running the pin
forward into the midfoot bones or superiorly into the talus will
achieve good fixation. -
Next, insert cannulated screws. Usually
two 6.5mm screws are sufficient to stabilize the fracture. The
temporary K-wire placement can be left to help stabilize the fracture. -
Close the posterior heel wound in the
usual fashion. Apply sterile dressings and a bulky well-padded splint
utilizing a medial lateral sugar-tong splint around the foot and a
posterior splint to support the foot in a neutral position. -
Postoperatively, elevate the foot 10 cm
above the heart. Observe closely for excessive swelling and expect to
split the dressing anteriorly down to skin within the first 24 hours
after the procedure. Maintain elevation of the foot at all times,
except for the necessities of daily living until swelling has abated.
Once the swelling is down, apply a well-padded short-leg cast
protecting the protruding pins. Essex-Lopresti (34)
advocated early motion of the subtalar joint, but in my experience this
has led to wound complications and loss of fixation. Therefore, I
immobilize the patient for 6 weeks in a short-leg cast. At 6 weeks, all
the protruding wires and pins can be removed in an outpatient setting
and an additional short-leg cast applied for 2 weeks more. At 6–8
weeks, remove the cast and apply a removable orthosis such as a
cam-walker, and begin active ROM exercises for the foot and ankle.
Delay weight bearing until 10–12 weeks. Neither the closed reduction
technique described previously nor this one permits early motion in the
subtalar joint, which is a disadvantage. The primary goal of this
treatment is to restore the overall
P.2975
shape of the calcaneus as opposed to preserving subtalar joint motion.
percutaneous techniques described, the need for subtalar joint fusion
for subsequent subtalar joint pain and/or arthritis has been
exceedingly rare. The subtalar joint, however, usually is quite stiff,
with only a bit of motion remaining.
or lateral, approach with the subperiosteal dissection of a
full-thickness flap off the lateral calcaneal wall is used for the
exposure from the calcaneal tuberosity to the calcaneal cuboid joint.
The principles of reduction include stabilization of the
calcaneal–cuboid joint, the critical angle of Gissane, and the
posterior facet; realignment of the calcaneal tuberosity to the
sustentaculum; and finally replacement of the lateral wall. Bone grafts
are used for large defects and fixation utilizes either a custom 3.5 or
a 2.7 plate that has been specifically designed for calcaneal fracture
fixation. The surgery can be difficult and tedious, but it is the best
method for restoring the anatomy of the calcaneus, in particular the
articular surfaces.
-
Place the patient in a lateral decubitus
position on a radiolucent fracture table with the foot to be operated
uppermost. The surgery can be prolonged, so carefully position the
upper extremities and pad bony prominences and neurovascular
structures. Pad the down leg well and create a well-padded platform to
operate on. With the legs in a slightly scissored position, lateral
radiographs are easy to obtain. With external rotation, the tuberosity
view can easily be obtained to check hindfoot alignment. -
Start the incision 6–7 cm above the
lateral malleolus, and posterior along the lateral edge of the Achilles
tendon. Extend it distally parallel to the Achilles tendon almost to
the weight-bearing skin on the heelpad; then gently curve it forward
and extend the transverse limb to the base of the fifth metatarsal (Fig. 110.27).
Carry dissection directly down to the calcaneus, avoiding injury to
sensory nerves. Then sharply elevate this entire full-thickness flap at
a subperiosteal level, which includes the peroneal tendons, the
calcaneal fibular ligaments, and the sural nerve. Full development of
this exposure provides access to the calcaneal cuboid joint, the
subtalar joint, the sinus tarsi, and the retrocalcaneal tuberosity.
Place several folded towels under the tibia to allow the foot to be
adducted, thereby increasing the exposure. For retraction of the flap,
place K-wires in the lateral process of the talus, the fibula, and the
cuboid, and bend them away from the surgical field to hold the flap.
Avoid excessive tension and kinking of the flap, which can lead to
marginal necrosis of the tip of the flap.![]() Figure 110.27. Skin incision for open reduction of the calcaneus from a lateral approach.
Figure 110.27. Skin incision for open reduction of the calcaneus from a lateral approach. -
After this exposure, inspect the
fractures and bulge of the lateral wall of the calcaneus. Reflect the
lateral wall posteriorly to visualize the interior of the calcaneus and
the facet joints. An osteotomy of the lateral wall is sometimes
necessary. The lateral posterior facet usually
P.2976
is
depressed deep into the midbody of the calcaneus and rotated clockwise
as visualized in this approach. The tuberosity fragment is short and in
varus. Anteriorly, expose and examine the calcaneal–cuboid joint for
fracture or displacement, as the reduction generally starts from the
anterior aspect of the calcaneus and progresses posteriorly. -
Address the anterior calcaneus and the
calcaneal–cuboid joint first. Use multiple 1.6 or 2.0 K-wires to reduce
and fix the anterior body of the calcaneus and then the
calcaneal–cuboid joint. -
Reduce and temporarily fix with K-wires
the depressed posterior facet fragment. If the fracture line is lateral
and noncomminuted, fixation can be fairly easy, whereas a more medial
fracture line or comminution can make this quite challenging. Access to
the articular fragments can be improved by distracting the tuberosity
fragment to restore the length of the calcaneus, which displaces the
tuberosity fragment inferiorly, medially, and posteriorly. Reduction
often requires a combination of techniques. Insert a small osteotome or
elevator into the primary fracture line and displace the body of the
calcaneal tuberosity. In addition, a “Gissane spike” (a 6.5 mm, fully
threaded distraction bolt) or a transverse or a longitudinal Steinmann
pin can be placed into the tuberosity to manipulate the tuberosity,
provide traction, and aid with the reduction. -
Now elevate and rotate the depressed
posterior facet joint fragments into anatomic position. Fix the
posterior facet fragments to the intact portions of the facet and to
the sustentaculum. Do all of this under fluoroscopic visualization to
ensure anatomic reduction and appropriate placement of the wires. At
this point, check Broden’s views to be certain that the posterior facet
joint is anatomically restored. It is usually best to complete the
fixation of the articular surface by inserting 3.5 mm lag screws with
washers prior to final reduction of the calcaneal tuberosity and
placement of the calcaneal plate. -
Complete the reduction and fixation of
the tuberosity. This is usually the most difficult part of the
reduction and frequently takes more than one attempt before
satisfactory hindfoot alignment is achieved. -
Use the pins or spike previously placed
in the tuberosity to align it with the remainder of the calcaneus. Try
to line up the medial cortex with the sustentaculum. At this point, a
defect in the cancellous bone of the calcaneus beneath the posterior
facet joint is usually evident. Stability of the reduction can be
improved by packing this defect with autologous cancellous bone graft,
morcelized allograft, or a synthetic bone graft substitute (90). Obtain temporary fixation of the reduction with K-wires. -
Reduce the lateral wall of the calcaneus
back into position. If it is intact, it provides a good guide to
reduction, as it should fit anatomically into place. -
Obtain final fixation by applying a
specially designed calcaneus plate or a combination of mini-fragment or
small fragment plates utilizing 2.7 and/or 3.5 mm screws. -
I prefer the AO calcaneal plate (Synthes,
Paoli, PA), which must be carefully molded to fit the entire lateral
surface of the calcaneus so that the fracture is not displaced with
insertion of the screws. This plate provides many alternative locations
for screws, not all of which need to be used. Insert screws where
necessary to obtain as solid a fixation of the fracture as possible (45). Obtain final plain radiographs, including AP, lateral, tuberosity, and Broden’s views (Fig. 110.28). Figure 110.28. A: Intra-articular fracture of the calcaneus. Note the reversal of Böhler’s angle on this lateral radiograph. B: CT scan showing intra-articular stepoff. C:
Figure 110.28. A: Intra-articular fracture of the calcaneus. Note the reversal of Böhler’s angle on this lateral radiograph. B: CT scan showing intra-articular stepoff. C:
Postoperative lateral radiograph showing restoration of Böhler’s angle
and fixation with a low-profile titanium calcaneus plate. D: Axial view. (Courtesy of C. Finkemeier, Sacramento, CA.) -
The wound closure is critical to help
prevent wound complications. Insert a small drain. Use interrupted
figure-eight sutures from the periosteal flap to the deep tissues,
including the fascia of the abductor digiti minimi. Place all
deep sutures prior to tying and then tie from anteriorly to
posteriorly. This provides even tension on the flap. Close subcutaneous
fat and then the skin with either Allgöwer-type subcuticular vertical
nylon mattress sutures or staples. Apply a well-padded short-leg splint
incorporating bulk cotton to allow for swelling, holding the foot and
ankle in a neutral position.
or a small medial approach can be combined with a lateral approach to
assist in the reduction of the calcaneal tuberosity to the
sustentaculum tali, especially in fractures that are more than 3 weeks
old.
-
Begin the skin incision halfway between
the medial malleolus and the bottom of the heel using a curvilinear
incision that is parallel and posterior to the posterior tibial tendon
and the neurovascular bundle. Reflect this flap in a subperiosteal
manner superiorward to expose the calcaneus. Try to identify and
preserve the sensory nerves. -
Identify the fracture lines, in particular the spike of bone of the sustentacular fragment, which is the key to the reduction.
-
The techniques of reduction and fixation
are similar to those already described for the lateral side. Lever the
body of the tuberosity posteriorly and medially; the fracture fragments
usually key into an anatomic position. Insert multiple K-wires through
the calcaneal tuberosity into the sustentaculum or mid foot to hold the
tuberosity fragment. Obtain fixation with staples, wires, screws,
and/or small plates. As mentioned earlier, the lateral approach is
necessary for reduction of the calcaneal–cuboid joint, the angle of
Gissane, and the posterior facet joint. -
Wound closure is as described for the lateral side.
-
Postoperatively, continue intravenous
antibiotics for 24 hours. Keep the foot elevated 10 cm above the heart.
Foot pumps may help to prevent edema (89).
Discharge patients in the bulky dressing and splint, and see them for a
follow-up at approximately 10 days. Continue elevation at home. If the
flaps are healthy without drainage, convert to a removable splint to
allow early ankle and hindfoot motion. Keep them non-weight-bearing. If
the patients are unreliable, place the foot in a short-leg cast and see
them regularly in the office for supervised active and passive ROM
exercises. At 6–8 weeks, at least 50% of the motion should have
returned to the ankle and hindfoot. If radiographs show healing,
initiate partial weight bearing up to 50 pounds. By 12–14 weeks, allow
full weight bearing, and begin strengthening exercises.
shoes, using elastic hose to control edema. They must practice walking
until they can walk across the room on tiptoe. If they fail to make
sufficient progress, send them to a physical therapist for supervised
exercises. They begin by walking on a combined treadmill–trampoline
machine and progress as tolerated. Full recovery requires a full year,
and some patients show additional improvement in the following year.
comminuted that anatomic reduction is not possible and posttraumatic
arthritis is inevitable, some authors (13,78)
advocate primary subtalar arthrodesis at the time of internal fixation
of the calcaneus, feeling that the overall long-term recovery is
shortened and a second operation avoided. In addition, this makes the
fixation of the calcaneus easier as implants can be placed into the
talus across the subtalar joint. To add subtalar arthrodesis to
fixation of the calcaneus, remove the cartilage from the joint surfaces
on the talus when the subtalar joint is exposed and curet the
subchondral bone to expose bleeding cancellous bone. Be certain that
the calcaneus is well aligned and in good position and pack autologous
bone into the subtalar joint. Assuming the tuberosity of the calcaneus
will provide good fixation, a long screw inserted from the plantar
surface of the tuberosity through a stab wound on the heel can be
angled up through the posterior facet joint into the body of the talus
to obtain good fixation. Place a washer on the screw to prevent it from
sinking into the calcaneus.
keep it in place until union of the calcaneus and subtalar joint
occurs. During this period, keep the patient non-weight-bearing. After
8 weeks, patients can be progressed toward full weight bearing either
in a short-leg cast or with a removable orthosis such as a Cam-walker
until solid union occurs, usually around 12 weeks.
medially and laterally. This is potentially very serious, as it can
lead to secondary infection and exposure of the bone and fixation
hardware (10,36). If
not well managed, or if it occurs in the presence of peripheral
vascular disease or systemic disease such as diabetes mellitus, deep
bone infection can occur, which can result in amputation. Avoid this
complication by careful patient selection, maintaining a full-thickness
flap, using gentle retraction of the flap (which avoids the kinking of
the flap), and avoiding prolonged operating times.
preserve the blood supply to the skin is essential. If swelling occurs
during surgery, so that a tension-free closure is not possible, leave
the wound open; cover it with a biological dressing and return the
patient to surgery for a delayed primary closure when the soft-tissue
swelling has resolved. Necrosis of the tip of the superior flap of 5 mm
or less can usually be treated by debridement on an outpatient basis,
and with wet-to-dry dressing changes, allowing the wound to heal by
secondary intention. If the wound necrosis is so large that bone and/or
fixation will be exposed, consult with an orthopaedic or plastic
surgeon with experience in local or free microvascularized flaps, so
that the wound can be debrided back to viable tissue and closed as soon
as possible.
cellulitis, which can be treated with deep cultures and administration
of appropriate intravenous bactericidal antibiotics. For deep infection
with abscess formation, irrigate and debride the wound as soon as
infection is detected, obtain deep cultures, and begin culture-specific
bactericidal intravenous antibiotics. Usually, the wound needs to be
left open, but it should be closed secondarily as soon as the acute
infection resolves. If the construct remains stable and hardware
fixation is solid, the implants can be left in place. If deep infection
with osteomyelitis occurs with loosening of the implants, then removal
of all implants and debridement of nonviable bone may be necessary to
resolve the infection. This usually leads to an unsatisfactory outcome:
a scarred, shortened heel with significant loss of function.
after any of the described methods of reduction because of the
difficulty in treating
these
challenging fractures. The most frequent problem in my experience is
residual shortening, with proximal migration of the tuberosity and
residual valgus. This can lead to weakness in pushoff, difficulty with
shoeware, and impingement on the peroneal tendons or tip of the fibula,
which can lead to chronic pain and tendinitis. Reconstruction for late
deformities of the calcaneus are very difficult and are beyond the
scope of this chapter (see Chapter 115).
some extent in the majority of these fractures. It is primarily the
result of the original trauma itself, although inadequate reduction can
hasten the onset of arthritis. According to McReynolds (56),
about 20% of calcaneal fractures will require subtalar arthrodesis for
traumatic arthritis. This is much higher than in my experience, where
less than 5% ever require arthrodesis, probably because many go on to
stable pain-free fibrous ankylosis of the subtalar joint. If the
overall anatomic shape and alignment of the calcaneus is restored, this
minimizes the stresses on the subtalar joint and keeps the necessity
for subsequent arthrodesis low. See Chapter 115 for a discussion of arthrodesis of the subtalar joint.
studies comparing ORIF of calcaneal fractures to less invasive methods
that have shown better functional outcomes with ORIF (87,91).
There is an ongoing large randomized study in Canada, which is
unpublished, that suggests that ORIF may provide a slightly better
long-term result in certain displaced types of fractures. There is
general agreement among fracture surgeons that anatomically
reconstructing the calcaneus produces acceptable functional outcomes in
the majority of selected patients, and that there is a tremendous
advantage to subsequent reconstruction if the hindfoot anatomy is
reasonably normal (87,91).
calcaneus. As mentioned, there are limited indications for small open
medial approaches to assist in the reduction. Popularity is gaining for
more aggressive percutaneous reduction techniques; however, these will
probably not be universally applied in community practice settings
until the techniques are better developed. Long-term results of this
method are lacking. I prefer the lateral position using fluoroscopic
control and the extensile lateral approach when the soft-tissue
envelope is healthy. Calcaneal plate fixation with or without bone
grafting provides the best opportunity for anatomic reconstruction by
most general orthopaedic or fracture surgeons.
can be well managed by using a rocker-bottom shoe and oral
anti-inflammatories prior to recommending a hindfoot fusion. In the
event of a failed calcaneal fracture, a reasonable salvage approach is
a subtalar arthrodesis (22,88).
Occasionally, the hindfoot will require bone block distraction to
realign the hindfoot and the talonavicular joint with or without
calcaneal osteotomy (79).
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
AH, Lichtman DM. Surgical Treatment of Transchondral Talar Dome
Fractures (Osteochondritis Dissecans): Long-Term Follow-up. J Bone Joint Surg Am 1980;62:646.
SM, Mears DC. Three-Dimensional Analysis of Calcaneal Fractures.
Presented at the American Orthopaedic Foot and Ankle Society Meeting,
1988, Atlanta.
BD Jr. Fractures of the Calcaneus: Open Reduction and Internal Fixation
from the Medial Side, a 21-year Prospective Study. Foot Ankle Int 1997;18:685.
JB, Noto AM, Stevenson S. Volumetric Three-Dimensional Computed
Tomography for Acute Calcaneus Fractures: Preliminary Report. J Orthop Trauma 1990;4:346.
C, Loomer R, Amman W, et al. Osteochondral Lesions of the Talus: A New
Classification, New Imaging Techniques and Surgical Approach. Orthop Trans 1989;13:681.
JW, Starr AJ, Early JS. Early Wound Complications of Operative
Treatment of Calcaneus Fractures: Analysis of 190 Fractures. J Orthop Trauma 1999;13:369.
A II, Weber TG. Fasciotomy of the Foot: An Anatomical Study with
Special Reference to Release of the Calcaneal Compartment. Foot Ankle 1990;10:267.
DM, McCormack DM, Stephens MM. Intra-articular Calcaneal Fractures:
Effect of Open Reduction and Internal Fixation on the Contact
Characteristics of the Subtalar Joint. 1998;19:842.
JR. Treatment of Displaced Intra-Articular Fractures of the Calcaneus
Using Medial and Lateral Approaches, Internal Fixation and Early
Motion. J Bone Joint Surg Am 1987;69:115.
DB, Hedman TP, Yetkinler DN, et al. Superior Compression Strength of a
Calcaneal Fracture Construct Augmented with Remodelable Cancellous Bone
Cement. J Bone Joint Surg Am 1999;81:239.
A, Bousquet G, Lapeyre B. Les Fractures-Separations Totales du Col ou
du Corps de L’Astragale. Interet du Vissage par Voie Posterieure. Rev Chir Orthop 1970;56:529.