Fractures and Dislocations of the Foot
-
Mechanism of injury.
Calcaneal fractures are more frequent than any other fracture of the
tarsal bones and comprise 1% to 2% of all fractures. These fractures,
which are often bilateral, are likely to occur when a person falls from
a height and lands on the heels. Associated injuries include
compression fractures of the lumbar spine and occasionally fractures
about the knee or pelvis. -
Classification. Although there are many classification systems (Sander’s classification is the most widely utilized) (1), a description of the fracture location provides the most information.
-
Avulsion fractures
occur in the posterior process of the tubercle as a result of increased
tension in the Achilles tendon. This tension causes a fracture of the
calcaneus rather than a ruptured tendon. If the avulsion fracture is
large and runs into the body of the calcaneus (into or beyond the
posterior facet), it is termed a tongue-type fracture (Fig. 27-1). -
Fractures into the body of the calcaneus
-
Fractures not involving the subtalar joint, with or without disruption of the plantar surface of the calcaneus, can result in heel shortening and varus.
-
Fractures involving the subtalar joint
typically involve a triangular-shaped subarticular fragment that
remains in place medially, the fractured and impacted posterior facet
(generally the anterior portion is driven down into the body of the
calcaneus to a greater degree than the posterior portion), and
displacement of the lateral wall or the calcaneus under the fibula.
This is termed a joint depression fracture (Fig. 27-1).
-
-
-
Examination.
Pain and tenderness in the heel are present, with associated broadening
of the heel and ecchymosis. Ecchymosis on the posterior sole of the
foot with calcaneal tenderness is nearly diagnostic of a calcaneal
fracture. When open fractures are occurring, the wound is most often
medial near the sustentaculum talus. A foot compartmental syndrome can
occur in 2% to 5% of patients and must be treated with urgent
decompression (see Chap. 2). Because of the risk of associated injuries, the spine and pelvis must be thoroughly evaluated. -
Radiographs.
Fractures are identified on roentgenograms by a fracture line of
increased (impaction) or decreased bone density. Consideration must be
given to any distortion of the normal shape of the calcaneus. In
addition to the lateral radiographs, calcaneal (axial) views and
computed tomography (CT) are valuable to clarify the fracture pattern
and to assess any increased width of the calcaneus. As with any severe
fracture, analgesics often are required for the patient’s comfort
during the radiographs examination. -
Treatment.
All fractures should initially be treated in a well-padded splint for
the first 7 to 10 days until the swelling begins to resolve.-
Isolated avulsion fractures do not usually involve the subtalar joint.
-
Those with minimal displacement may be treated by a short-leg, non–weight-bearing cast with the ankle in a neutral position for 4 to 6 weeks (1). The lack of displacement should be confirmed by a roentgenogram after the cast is applied.
-
Avulsion fractures (tongue type) with major displacement require reduction and internal fixation of the displaced bone to reattach the Achilles tendon.
P.384
This procedure, generally accomplished with two lag screws, is followed
by non–weight-bearing immobilization in a short-leg cast. The foot is
held in slight plantar flexion for the first 3 to 4 weeks and then in a
neutral position for an additional 3 to 4 weeks. Alternatively, a
percutaneous reduction maneuver as described by Essex-Lopresti provides
excellent reduction (2).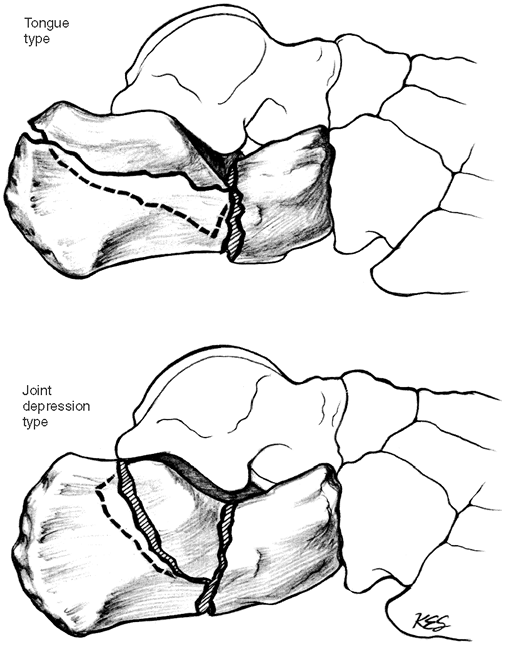 Figure 27-1. Diagrammatic representation of tongue type and joint depression type calcaneal fractures. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:355, with permission.)
Figure 27-1. Diagrammatic representation of tongue type and joint depression type calcaneal fractures. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:355, with permission.)
-
-
Fractures into the body of the calcaneus
-
Treatment
-
The tuber (Böhler) angle should be restored
with treatment whenever possible. The tuber angle, which is established
by the lateral roentgenogram, is formed by the intersection of one line
along the superior aspect of the tuber of the calcaneus with a second
line
P.385
along
the superior aspect of the middle and anterior portions of the
calcaneus. The angle is normally 30 degrees, but it could also be
compared to the uninjured side. -
With conservative treatment, restoration of this angle is thought to be unnecessary, and treatment consists of compression to prevent edema and decrease hemorrhage, followed by early subtalar motion and 6 to 12 weeks of no weight bearing.
-
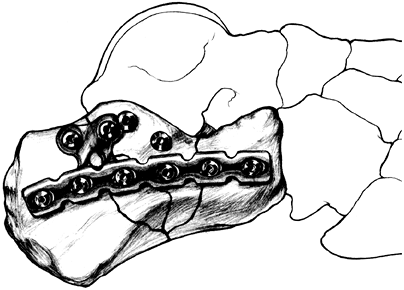
Open reduction
for anatomic restoration is desirable to realign articular fragments
and prevent peroneal impingement while allowing for normal shoe wear (Fig. 27-2).
There is no solid evidence to suggest that patients who have open
reduction and internal fixation (ORIF) have better functional results (3,4,5).
Most experienced surgeons believe that the risk of infection that
accompanies ORIF is outweighed by better foot shape and heel position. -
Early subtalar arthrodesis may be appropriate in very severely comminuted articular fractures, but such treatment is rarely advocated.
-
-
The authors advocate
a surgical reduction for intraarticular fractures only when the
fracture can be anatomically reduced and held in that reduced position (4).
The calcaneus is cancellous bone, and fractures of the calcaneus
usually are comminuted. Attempts at reconstruction require a great deal
of operative skill and knowledge of internal fixation with specialized
implants. Referral to an experienced surgeon is recommended. When the
surgeon is inexperienced and referral is not possible, these fractures
should be treated by compression and early motion under proper
supervision (1,3,6).
Early motion should be started within the first 72 hours. Short-term
hospital treatment appears to be worth the cost in improving the end
result and shortening the period of disability following this serious
and frequently disabling injury (7). The authors recommend the following treatment program:![]() Figure 27-2. Postoperative view of standard internal fixation for a joint depression fracture. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:359, with permission.)P.386
Figure 27-2. Postoperative view of standard internal fixation for a joint depression fracture. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:359, with permission.)P.386-
The patient is admitted to the hospital when necessary for adequate pain medication, elevation of the foot, and a proper compression dressing.
-
After control of pain and within 2 to 3 days, motion
is begun, with emphasis on inversion and eversion. Once the patient is
comfortable with the therapy and after outside follow-up therapy is
arranged, the patient is discharged. -
Weight bearing
may be started as soon as the fracture is consolidated (usually 8–10
weeks). When partial weight bearing is begun, a sponge placed in the
heel is helpful. A wheelchair is generally required for 8 to 12 weeks
for patients with bilateral fractures.
-
-
-
-
Complications
-
Fracture blisters and skin loss can occur.
-
Persistent pain can arise from swelling (the sequela of a compartmental syndrome), deformity, and stiffness.
-
Problems with shoe fitting occur because of heel widening and varus. A pedorthotist should be consulted for specialized shoes and inserts.
-
Persistent pain,
usually associated with loss of subtalar motion, can be severe enough
to require a triple arthrodesis. This procedure does not always produce
a pain-free foot and should be undertaken with caution (8).
Pain frequently occurs beneath the lateral malleolus because of
widening of the calcaneus with impingement of the peroneal tendons and
loss of heel height. Surgical relief involving the decompression of the
peroneal tendons can improve symptoms and should be considered.
-
-
Calcaneal fractures in children (9)
-
Calcaneal fractures in children follow the same pattern and are caused by the same mechanisms as in adults.
-
The treatment program follows the same general plan as for the adult.
-
Unreduced intraarticular fractures persist in limiting subtalar joint motion but have minimal symptoms in short-term follow-up.
-
-
Definition
-
A subtalar dislocation
occurs through the subtalar joint with the ankle and foot displaced
medially or laterally. The talus can snap back by itself inside the
mortise, leaving the foot displaced medially or laterally relative to
the toes (10,11,12). -
In a talar dislocation, the talus is completely dislocated from its position within the mortise and tarsus. This is a rare injury.
-
-
Mechanism of injury.
Progressive degrees of inversion forces applied to the foot cause
rupture of progressively more ligaments around the talus, resulting in
a subtalar-talonavicular or a complete talar dislocation. Inversion,
internal rotation, and equinus forces cause rupture of the
talonavicular ligament. More displacement ruptures the medial,
interosseous, and lateral talocalcaneal ligaments; finally, the lateral
ligaments (anterior talofibular, calcaneal-fibular, and posterior
talofibular ligaments) can rupture. The talus can ultimately be forced
from its major attachments and dislocate. The skin often breaks; in
this event, the talus may extrude from the foot. This injury can also
be associated with a fracture of the neck of the talus, which is also
commonly an open injury (8,13). -
Examination
-
A subtalar dislocation
shows a classic positioning of the foot medially or laterally on the
ankle. There is always marked tenting of the skin on the side opposite
the foot. -
With a closed talar dislocation, the talus comes to rest under the skin on the dorsolateral aspect of the ankle.
-
With both injuries, swelling is always severe. These are true emergencies.
-
-
Radiographs.
The diagnosis may be made on physical examination, but the extent of
injury and the exact position of the involved bones should be confirmed
by multiple roentgenographic views. Do not delay. Arrange for
anesthesia even before obtaining roentgenograms. -
Treatment
-
It may be advisable to carry out a manual reduction
by slow but firm traction in the line of the deformity with analgesia,
but only if there are delays with gaining access to the operating room
for anesthesia services. Reduction is easy unless there is trapping of
the posterior tibial tendon around the neck of the talus in a lateral
subtalar dislocation where open reduction is necessary. -
After reduction, a short-leg Jones compression splint is applied until swelling is controlled; then active range-of-motion exercises are begun.
-
An associated fracture must be reduced anatomically
and the reduction rigidly maintained, preferably with small fragment
lag screws. Where fixation is stable, early active motion may be
started using a removable posterior splint.
-
-
Complications
-
Ischemic skin loss can be seen.
-
Avascular necrosis of the body of the talus can occur with a talar dislocation (3,11).
-
Pain and stiffness can ensue.
-
Subtalar arthritis can develop.
-
-
Neck of the talus (13). Talus neck fractures are generally classified by the Hawkins’ system (Fig. 27-3).
Type I is nondisplaced and type II is displaced with associated
subtalar joint subluxation. In type III, the talar body is dislocated
from the ankle mortise, and in type IV the talonavicular joint is also
subluxated.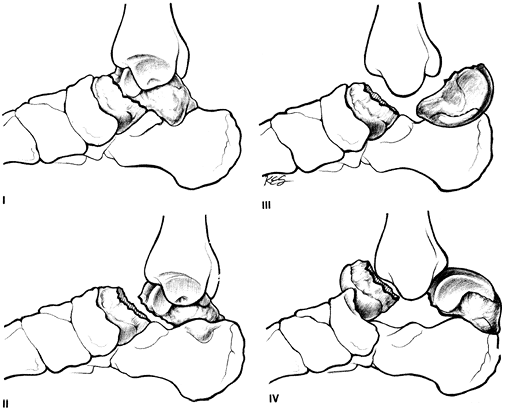 Figure 27-3. Diagrammatic representation of Hawkins’ classification of talar neck fractures. I, nondisplaced; II, displaced with associated subtalar joint subluxation; III, talar body dislocated from the ankle mortise; IV, talonavicular joint subluxated also. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:340, with permission.)P.388
Figure 27-3. Diagrammatic representation of Hawkins’ classification of talar neck fractures. I, nondisplaced; II, displaced with associated subtalar joint subluxation; III, talar body dislocated from the ankle mortise; IV, talonavicular joint subluxated also. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:340, with permission.)P.388-
Mechanism of injury.
This injury is most commonly the result of forceful ankle dorsiflexion.
Historically, it occurred with biplanes impacting the ground (the
“aviator’s astralagus”). The talus impinges on the anterior portion of
the tibia, causing a fracture through the talar neck. The fracture,
which may not be displaced, is easily overlooked without adequate
radiographs. -
Treatment.
Accurate reduction and rigid immobilization are important. To preserve
the function of the hind foot joints, open anatomic reduction and
internal fixation are recommended. Placement of small fragment lag
screws across the fracture site is advisable. Because post-traumatic
avascular necrosis of the body of the talus occurs commonly, most
surgeons recommend waiting for subchondral resorption of the body of
the talus to be apparent in the mortise radiographs before allowing
full weight bearing (Hawkins’ sign). This complication is less frequent
with emergent reduction and fixation of widely displaced fractures. -
Complications
-
Dislocation of the peroneal tendons occurs as an associated injury that should be ruled out and treated if present.
-
Avascular necrosis is the most serious complication. Ankle arthrodesis can be difficult in this setting, and specialized techniques must be used (2).
-
-
-
Other talar fractures.
Fractures may involve the body of the talus as well as the neck.
Anatomic reduction is necessary for fractures involving the articular
surfaces (14). Whenever the fragments are large
enough and it is technically possible, ORIF usually is required. (See
the foregoing discussion of Hawkins’ sign.)
most common. Whenever there is displacement of greater than 2 mm, the
authors recommend open anatomic reduction and screw fixation (15).
When associated with midfoot fractures or subluxations, reduction and
fixation can be difficult. Referral to a surgeon experienced in the
management of the fractures should be considered. Swelling can be
severe, as with calcaneus fractures, so the procedure may be delayed 7
to 10 days while swelling subsides. Postoperative treatment involves 6
weeks in a non–weight-bearing cast or brace followed by 6 weeks in a
short-leg weight-bearing boot or cast.
-
Radiographs.
The usual deformities can be masked in massive swelling.
Anteroposterior, lateral, and oblique radiographs of the foot are
essential. It is frequently helpful to compare these with films of the
normal foot. Midfoot subluxations can be subtle, and a high index of
suspicion is necessary when there is a history of axial loading of the
foot and midfoot tenderness. Standing films, when possible, may expose
Lisfranc joint subluxation as the bones separate when force (weight
bearing) is applied. Stress radiographs of the midfoot are indicated
when the diagnosis is not clear. -
Treatment. Manipulative reduction is done; anesthesia is usually used for forefoot
dislocations. If reduction is possible and if stability is sufficient,
plaster immobilization for 4 weeks is adequate. If reduction is
incomplete or if there is instability, then displacement may occur,
leading to malunion, persistent subluxation, and a painful planovalgus
forefoot. If the reduction is unstable, then open reduction may be
required and internal fixation is generally necessary.-
For midtarsal dislocations and subluxations (The Lisfranc joint injury),
accurate anatomic reduction is required to prevent the sequelae of
forefoot abduction and collapse of the medial arch. Open reduction and
fixation with screws is recommended (16). This
allows arthrofibrosis of the injured joints, which preserves the normal
slope of the foot. Although screw breakage can occur, it is generally
advisable to leave the screws in place because removal can lead to
planovalgus deformity. Although nearly all patients experience
long-term discomfort and swelling, the normal shape of the foot makes
the management of these complaints easier. -
Phalangeal dislocations
require only reduction and symptomatic treatment. Stiff-soled shoes are
often helpful for 4 to 6 weeks postinjury. Taping of injured toes to
the adjacent uninjured toe can be helpful.
P.389 -
-
The diagnosis of a forefoot fracture is usually suspected when localized bony tenderness or deformity is found.
-
Anteroposterior, oblique, and lateral roentgenograms of the foot generally confirm the diagnosis.
-
Treatment
-
Metatarsals
-
Avulsion fractures of the base of the fifth metatarsal
(the insertion of the peroneus brevis) should be treated
symptomatically unless there is gross (>3 mm) displacement, in which
case the treatment of choice is ORIF. Symptomatic treatment usually
consists of a compression dressing and elevation until the swelling is
controlled, followed by a short-leg weight-bearing cast with a
well-molded arch. Anything more distal than avulsion fractures have the
risk of nonunion and must be managed much more carefully. This fifth
metatarsal proximal neck shaft junction fracture (Jones fracture) is prone to delayed union and nonunion (17,18). Therefore, no weight bearing for 10 to 12 weeks is indicated. Open reduction and bone grafting is required for nonunions (17)
and may be considered as a primary option in others. For example,
athletic individuals may choose this option, as well as certain elderly
patents who may not tolerate 10 to 12 weeks of non–weight bearing. For
surgical fixation, intramedullary screw fixation is preferred. -
Fractures of the metatarsal shaft
are caused by a crushing injury. As a rule, the soft-tissue injury is
more severe than the fracture. Initial treatment should include a
compression dressing and elevation to control swelling, which is
followed by reduction if the fracture is displaced. If the great toe
remains cocked up or the first web space remains widened with fractures to the first metatarsal,
then the reduction is incomplete or unstable. Open reduction with small
fragment plates for this type of unstable first metatarsal fracture is
recommended. If the second through fifth metatarsal fractures are seen
to have the metatarsal heads at the same level without excessive (>5
mm) shortening, then the reduction is satisfactory. If displacement is
more severe, then closed reduction with axial Kirschner wire fixation
may be necessary to prevent long-term transfer metatarsalgia. After
proper reduction, the foot is placed in a short-leg plaster cast with
well-contoured longitudinal and metatarsal arches. No weight bearing is
allowed on the affected foot for 4 to 6 weeks. An additional 6 weeks is
spent in a walking cast or fracture boot. Open reduction rarely is
indicated for lesser metatarsal fractures unless there is marked
shortening or plantar angulation. -
Fractures of the metatarsal necks
can be associated with displacement of the metatarsal head toward the
weight-bearing surface of the foot, which disrupts the normal mechanics
of proper weight bearing.-
Fractures of the first metatarsal neck or of multiple metatarsal necks
must be reduced and are usually held with some type of percutaneous
wire fixation because they are often unstable. Pins can be placed
through the plantar surface of the foot, through the metatarsal heads,
and into the shaft of the metatarsals. Roentgenographic image
intensification aids in the placement of these pins, but with proper
palpation and anesthesia, it can ordinarily be accomplished
percutaneously. -
An isolated metatarsal neck fracture
should be grossly aligned to avoid abnormal pressure of the metatarsal
head on the sole of the foot (transfer metatarsalgia) and to avoid
forcing the toe against the top of the shoe. Immobilize in a short-leg
walking cast for 6 to 10 weeks.
-
-
-
Toes
-
Fractures of the toes
are treated by taping them to the adjacent toe, which acts as an
adequate splint. Avoid maceration by using dry cotton or Webril between
the toes. -
A fracture of the great toe often requires a short-leg cast with a platform under the toes for comfort as well as immobilization.
-
Fractures of the sesamoids of the great toe
-
Mechanism of injury.
These fractures are usually the result of a direct force applied to
this area of the foot either from a fall with landing on the metatarsal
heads or from a weight being dropped on the foot. Occasionally, these
injuries occur as avulsion fractures from forceful hyperextension of
the great toe or from traction injuries to the flexor hallucis brevis.
The fractures are usually transverse. -
Examination.
The patient experiences localized pain over the area. Differential
diagnosis takes into account a congenital bipartite sesamoid. Local
pain and irregular surfaces on the roentgenogram are the distinguishing
features for a fracture. It is sometimes difficult to visualize on
plain x-ray and a CT may be needed. -
Treatment. No
weight bearing is allowed as long as the area is painful. After initial
treatment, a metatarsal pad can help relieve pressure. Occasionally,
pain persists; sesamoid resection and reconstitution of the tendon are
then indicated.
-
-
P.390 -
bearing for 12 weeks with early subtalar motion where nonoperative
treatment is selected, ORIF with non–weight-bearing and passive
subtalar motion for 12 weeks where ORIF indicated
with small fragment lag screws via medial and lateral approaches;
subtalar joint must be debrided of bone/cartilage fragments; non–weight
bearing for 8 to 12 weeks
Incision on the side of the deformity, exploration of the subtalar
joint after removing tissue blocking reduction ORIF with small or
minifragment screws of larger fragments
Displacement of first, second, third metatarsal bases with ligament
disruption or major displacement of base of the first, second, third
metatarsals
orthosis or shoe wear for 6 to 8 weeks, progressive weight bearing as
tolerated, buddy taping of lesser toe fractures
HV, Triffitt PD, Gregg PJ. Intra-articular fractures of the calcaneum
treated operatively or conservatively a prospective study. J Bone Joint Surg (Br) 1993;75:932–937.
DB, Krieger LE. Operative vs. non-operative treatment of
intra-articular fractures of the calcaneus: a prospective randomized
trial. Foot Ankle Int 1996;17:2–9.
JR. Treatment of displaced intraarticular fractures of the calcaneus
using medial and lateral approaches, internal fixation and early
motion. J Bone Joint Surg (Am) 1987;69:115–130.
JL, Kirwan EOG, Jackson AM. The long-term results of conservative
management of severely displaced fractures of the calcaneus. J Bone Joint Surg (Br) 1984;66:386–390.