Flexor Tendon Laceration
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Flexor Tendon Laceration
Flexor Tendon Laceration
John J. Carbone MD
Dawn M. LaPorte MD
Description
-
Flexor tendon laceration may require emergency surgical repair, depending on:
-
Location of the laceration
-
Hand dominance
-
Age and occupation of the patient
-
-
Lacerations located between the distal
transverse palmar crease and the PIP joint flexor crease represent an
area of increased risk from scarring or adhesions and poor functional
outcome resulting from the complex and precise anatomy in this area
(“no-man’s land”) (1,2). -
The superficial and deep flexors are at
risk at different locations in the hand because each has a superficial
course on the palmar surface. -
Each tendon adds to the strength and independent function of the fingers in flexion.
-
Classification is by the name of the tendon lacerated (superficial versus deep) and the location of the laceration.
-
The level of the laceration is described most easily by the zone of the injury (3).
-
Zone 1: Fingertip to PIP flexor crease
-
Zone 2: PIP flexor crease to distal palmar transverse crease
-
Zone 3: Distal palmar transverse crease to distal wrist flexor crease
-
Epidemiology
Incidence
This injury is one of the most common types of tendon lacerations.
Risk Factors
Working with sharp objects
Etiology
The cause of the injury is sharp laceration to the tendon (e.g., via knife, glass).
Associated Conditions
-
Digital nerve laceration
-
Digital artery laceration
Signs and Symptoms
-
Laceration to the palmar aspect of the hand
-
Change in the resting posture of the finger relative to the other fingers (e.g., slight extension of the injured finger)
-
Loss of independent flexion of the distal digital joint when tested
-
Loss of ability to flex the finger
-
Decreased strength of finger flexion
-
Evidence of tendon injury during wound exploration
-
Evidence of tendon sheath or pulley laceration during wound exploration
Physical Exam
-
Test independent DIP and PIP flexor flexion (Figs. 1 and 2).
-
Test for lacerations of adjacent nerves.
-
Test the strength of each finger.
-
Explore the wound for a tendon or pulley injury.
Tests
Imaging
Obtain radiographs to rule out foreign body, fracture, dislocation, or avulsion injury.
Differential Diagnosis
-
Fracture-dislocation
-
Avulsion injury of tendon
-
Rupture of tendon
 Fig.
Fig.
1. Testing for an intact profundus tendon is performed by holding the
proximal joints straight and asking the patient to flex only the distal
joint.
General Measures
-
Tetanus shot
-
Wound washout using normal saline
-
Antibiotics (usually 3rd-generation cephalosporin IV)
-
Elevation and splinting of the hand until surgical evaluation is performed
-
Orthopaedic consultation and preoperative laboratory tests
-
Digital nerve and artery laceration:
-
Careful and complete neurovascular
examination, including 2-point discrimination and Doppler study of the
neurovascular bundle on each side of the tendon in question
-
Special Therapy
Physical Therapy
-
Postoperative ROM depends on the lesion location and the type and quality of repair.
-
Usually, the goal is passive ROM as soon as the skin repair tolerates motion.
-
Children and adults who cannot follow restrictions should be immobilized postoperatively.
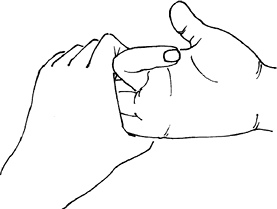 Fig.
Fig.
2. Testing for an intact sublimis flexor tendon is done by asking
patient to flex an individual finger while holding the other fingers in
full extension. The finger then will flex only at the proximal joint.
-
P.141
Medication
Antibiotic choice may be related to the contamination at the time of injury.
Surgery
-
Flexor tendon repair and results depend on the location, level, and type of injury.
-
Primary acute repair has provided the most functional results (4).
-
Repair should be performed within 1–2 weeks after injury.
-
In the presence of a flexor tendon sheath
injury, early repair may be done to minimize scarring and adhesions and
to give the best functional result.
Prognosis
-
Prognosis depends heavily on the type and location of the injury.
-
Injuries located between the distal
transverse palmar crease and the most distal digit flexor crease often
result in finger stiffness. -
In other areas, results are better.
Complications
-
Infection
-
Decreased ROM secondary to scarring or adhesions
-
Loss of strength
-
Need for delayed repair or reconstruction
-
Tendon rupture
References
1. Amadio
PC, Hunter JM. Prognostic factors in flexor tendon surgery in zone 2.
In: Hunter JM, Schneider LH, Mackin EJ, eds. Tendon Surgery in the
Hand. St. Louis: CV Mosby, 1987:138–147.
PC, Hunter JM. Prognostic factors in flexor tendon surgery in zone 2.
In: Hunter JM, Schneider LH, Mackin EJ, eds. Tendon Surgery in the
Hand. St. Louis: CV Mosby, 1987:138–147.
2. Tang JB. Flexor tendon repair in zone 2C. J Hand Surg 1994;19B:72–75.
3. Boyer MI. Flexor tendon injury. Acute injuries. In: Green DP, Hotchkiss RN, Pederson WC, et al., eds. Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier Churchill Livingstone, 2005: 219–240.
4. Strickland JW. Development of flexor tendon surgery: twenty-five years of progress. J Hand Surg 2000;25A:214–235.
Codes
ICD9-CM
840.9 Upper limb tendon laceration
Patient Teaching
-
The patient should understand the severity of the injury even though the laceration may appear small.
-
Functional outcome strongly depends on the compliance and cooperation of the patient.
-
Postoperative hand therapy is critical to a good result.
Prevention
United States Occupational Safety and Health Administration guidelines should be used when working with sharp objects.
FAQ
Q: Do partial flexor tendon lacerations need to be repaired?
A:
If the laceration involves >60% of the tendon, repair is
recommended. If it involves ≤60% of the tendon, repair is not necessary
and débridement is indicated only for entrapment of the tendon under
the pulley system (e.g., triggering).
If the laceration involves >60% of the tendon, repair is
recommended. If it involves ≤60% of the tendon, repair is not necessary
and débridement is indicated only for entrapment of the tendon under
the pulley system (e.g., triggering).
Q: What are the timing requirements for flexor tendon repair?
A:
Repair should be performed in the operating room within 3 weeks,
optimally in <2 weeks, of the laceration. Primary repair usually is
not recommended in presentations delayed >5–6 weeks.
Repair should be performed in the operating room within 3 weeks,
optimally in <2 weeks, of the laceration. Primary repair usually is
not recommended in presentations delayed >5–6 weeks.
