Facet Blocks
Editors: Chelly, Jacques E.
Title: Peripheral Nerve Blocks: A Color Atlas, 3rd Edition
Copyright ©2009 Lippincott Williams & Wilkins
> Table of Contents > Section VII – Pain Blocks > 64 – Facet Blocks
64
Facet Blocks
Nashaat N. Rizk
Meera Appaswarny
A. Cervical Facet Block
Cervical facet syndromes as seen with sudden stop of vehicle
(whiplash), athletic or occupational injury, sleeping with the neck in
odd (twisted) positions, and degenerative changes such as those seen in
osteophyte formation or joint capsule hypertrophy.
0.1 to 0.2 mL (<0.5 mL) radio-opaque dye (Isovue-M 200, Bracco
Diagnostics, Princeton, NJ), 0.5 to 1.0 mL 0.5% bupivacaine plus 40 mg
triamcinolone acetate.
Seven cervical vertebrae with two facet joints at each level, synovial
in type. At this level, the facets are posterior to the transverse
process and are formed by the superior articular facet of the lower
vertebra articulating with the inferior articular facet of the upper
vertebra. The joint surfaces are midway between the coronal and axial
planes. The capsule of the facet joint is tough and fibrous
posteriorly, and is in direct contact with the ligamentum flavum on its
anteromedial aspect, adjacent to the neural foramen and nerve root.
Dual level innervation is from the segmental nerve at its vertebral
level and also the nerve at the level caudad to it.
The cervical region is prepared and draped using sterile techniques.
Under fluoroscopic guidance, the cephalocaudad vertebral level of the
facet to be blocked is marked (Fig. 64-1A).
The mediolateral position of the facet joint is also visualized by
rotating the fluoroscope to produce an oblique image of the cervical
spine. After negative
P.432
aspiration
of blood and cerebrospinal fluid (CSF), needle placement is confirmed
with an injection of radiocontrast material. This is then followed with
local anesthetic and steroid.
 |
|
Figure 64-1. Under fluoroscopic guidance, the cephalocaudad vertebral level of the facet to be blocked is marked.
|
For medial branch blocks (C3-7), the patient is
positioned supine with the side to be blocked uppermost. A 20° to 30°
oblique view is obtained by rotating the fluoroscope to visualize the
foramina (in order to avoid them) and before proceeding with the
injection. Figure 64-1B presents the lateral view (with dye) and Figure 64-1C presents the oblique view (with dye).
positioned supine with the side to be blocked uppermost. A 20° to 30°
oblique view is obtained by rotating the fluoroscope to visualize the
foramina (in order to avoid them) and before proceeding with the
injection. Figure 64-1B presents the lateral view (with dye) and Figure 64-1C presents the oblique view (with dye).
Infection of overlying soft tissue is an absolute contraindication.
Contrast dye allergy is a relative contraindication. To avoid, use
nonionic contrast or no contrast.
P.433
-
A good working intravenous line prior to starting and standard monitors are required throughout the procedure.
-
There is a risk of dural spread if needle placement is too anterior.
-
Have resuscitative equipment on standby.
-
Do not use methylprednisolone for
cervical facet joint injections because its unintentional injection
into the vertebral artery may have serious consequences.
Radiofrequency
-
Radiofrequency lesioning probes (Radionics, Burlington, MA).
-
Success rate for cervical denervation is poor unless done at two sites cephalad and caudad at each facet site.
-
Pulsed mode: Probes should be 23-gauge/60-mm or 22-gauge/100-mm.
-
Temperature: 42°C of delivered voltage at 60 V.
-
Pulse generator: 20-ms bursts every 0.5 seconds for 120 seconds.
P.434
B. Lumbar Facet Medial Branch Block
Lumbar facet joint pain; hip/buttock pain; cramping lower extremity
pain; lower back stiffness especially in the mornings and uncontrolled
by rest, nonsteroidal antiinflammatory drugs, or physical therapy in
the absence of any radiologic evidence of disc herniation, spinal
stenosis, or foraminal root impingement.
Radiocontrast dye 0.25 to 0.5 mL, 0.5% bupivacaine, plus 20 mg of
methylprednisone, giving a total volume of less than 2 mL to be
injected after negative aspiration of CSF or blood.
Five lumbar vertebrae, two facet joints at each level. In the lumbar
area, the facet joints are posterior to the transverse processes. In
the lumbar region, the facet joint orientation is 30° oblique to the
sagittal plane.
Medial branch is from the posterior ramus. This also supplies the
paraspinal structure muscles (multifidus and interspinals), ligaments,
and periosteum of the neural arch.
The lumbar region is prepared and draped using usual sterile
techniques. Using fluoroscopy, the C-arm is positioned at 25°
obliquely, using the minimum obliqueness that allows visualization of
the eye of the Scotty dog. The tip of the needle is properly positioned
by the use of multiplane fluoroscopic views. After confirming negative
aspiration of CSF, contrast dye is injected to confirm position. This
is then followed by the injection of the local anesthetic and steroid
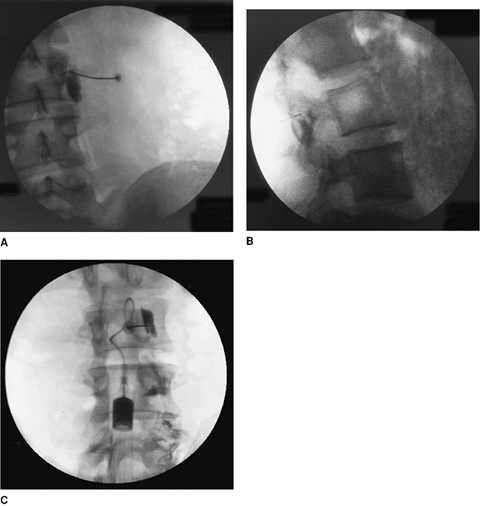
mixture. Figure 64-2 presents anteroposterior (A), lateral (B), and oblique views (C) with dye.
Transient increase in pain, spinal anesthesia, chemical meningitis,
paraspinal infection, entry into intervertebral foramen with vertebral
artery puncture, transient ataxia (unsteadiness secondary to partial
block of upper cervical proprioceptive afferents), and Charcot joints
due to denervation after radiofrequency.
-
Proper patient selection is important after a thorough history and physical exam and review of radiologic studies.
-
Two 3-mL syringes with extension tubing per facet prepared in advance are required.
-
Use only small volumes, as recommended.
Larger volumes (4 to 5 mL) may spread to adjacent segmental nerves and
paraspinous muscles, and make the result of the block difficult to
interpret. -
Although rare, advise the patient of the possibility of an associated neuraxial block.
-
The immediate availability of appropriate resuscitation equipment is necessary.
P.435
 |
|
Figure 64-2. Anteroposterior (A), lateral (B), and oblique (C) views with dye.
|
Radiofrequency
-
Radiofrequency lesioning probes (Radionics, Burlington, MA).
-
Probes: 23-gauge/60-mm or 22-gauge/100-mm.
-
Pulsed mode.
-
Temperature: 42°C.
-
Delivered voltage: 60 V.
-
Pulse generator: 20-ms bursts every 0.5 seconds for 120 seconds.
Suggested Readings
Kline MT. Radiofrequency lesions in the cervical region. Stereotactic radiofrequency lesions as part of the management of pain. Delray Beach, FL: St. Lucie Press, 1996.
Newman M, Raj PP. Facet syndrome and blocks. In: Raj PP, ed. Practical management of pain, 3rd ed. Philadelphia: Mosby, 2000.
Waldman SD. Cervical facet block: medial branch technique. Atlas of interventional pain management. Philadelphia: WB Saunders Co, 1998.
