Distal Radius Fractures: Open Reduction Internal Fixation
A number of factors have contributed to this changing perspective.
Among these include a greater recognition of the wide variation in
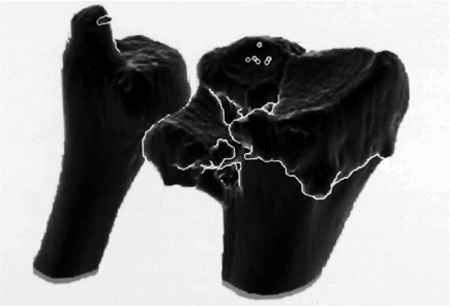
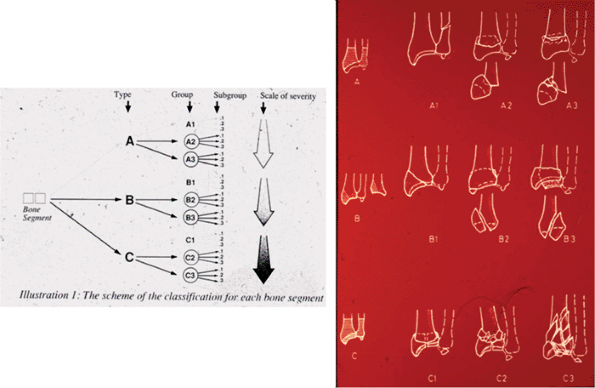
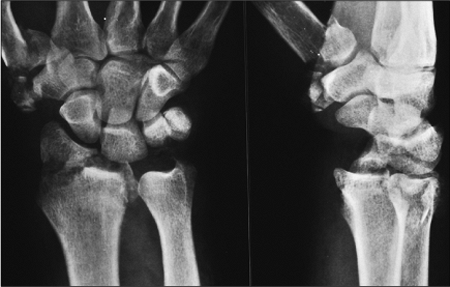
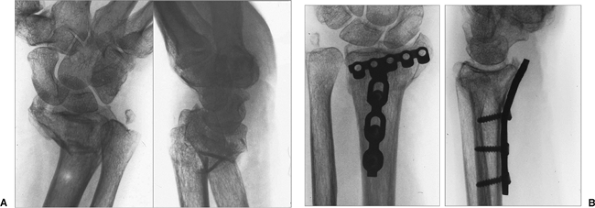
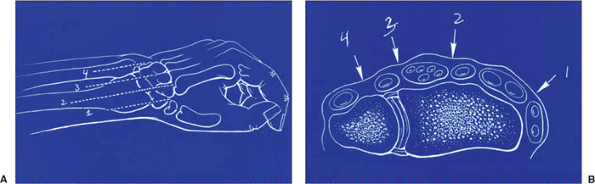
fracture patterns (18,19,20). The availability of computed tomography (CT) has permitted a three-dimensional projection of the fracture morphology (Fig. 13.1) (5,21). In fact, distal radial fractures differ to the extent that only the distal nature of the injury is in common among them (Fig. 13.2).
Fractures that involve a shearing mechanism displacing part of the
articular surface along with the carpus (Barton’s and reverse Barton’s
fracture) (22,23,24,25),
radiocarpal fracture-dislocations, displaced articular fractures
associated with high-energy trauma and metaphyseal-diaphyseal
comminution, articular compression fractures involving rotation of a
volar lunate facet component, and some unstable extra-articular
fractures are all amenable to open reduction and internal fixation.
fracture patterns has been an expanded appreciation for the structural
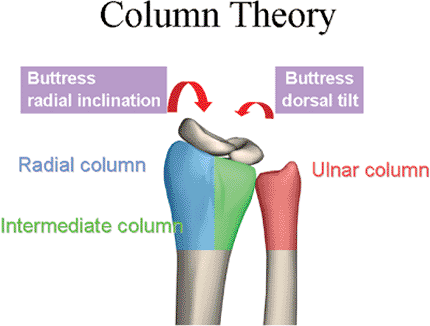
anatomy of the distal radius. Rikli and Regazzoni (26)
divided the distal radius into a strong, cortical radial “column”; an
intermediate column, which contains the articular surfaces of both the
lunate facet as well as the sigmoid notch; and the distal ulna column
with its firm attachment to the radius through the triangular
fibrocartilage complex (Fig 13.3). Recognition
of this unique anatomical orientation and patterns of articular injury
has led to the development of a method of operative treatment coined
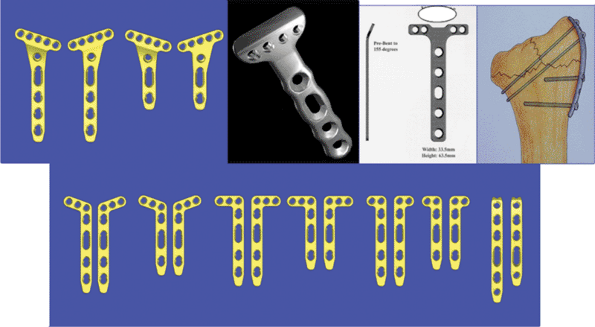
“fragment-specific fixation,” through which small strategically-placed
implants are used to support the critical structural components of the
fracture (Fig. 13.4).
of certain fractures involves those injuries associated with
intercarpal injury (27,28).
Fracture patterns involving compression or shearing of the radial
styloid and/or scaphoid facet of the distal radius are recognized to
have the potential of accompanying injuries to the scapholunate
ligament as well as the lunate facet and the lunotriquetral ligament (Fig 13.5).
(DRUJ) has also stimulated more operative intervention. DRUJ
instability following stabilization of the radius fracture,
especially in the presence of a large ulnar-styloid fracture, is best treated by operative fixation of the ulnar styloid.
 |
|
Figure 13.1. A three-dimensional CT image clearly shows the components of the articular injury.
|
generated by the development of a variety of technologically advanced
implants that are specific to the distal radius. These new pieces have
features, such as locking screws that enhance fixation in osteopenic
bone, that have led to interest in the volar approach to internal
fixation of dorsally displaced fractures. A volar approach would limit
the potential for problems involving the overlying extensor tendons on
the dorsal surface.
 |
|
Figure 13.2.
The comprehensive classification of the AO/ASIF demonstrates three major types, nine groups, and twenty-seven subgroups reflecting the enormous variation of fracture patterns. |
 |
|
Figure 13.3. The column concept, developed by Rikli and Regazzoni (26), includes the radial, intermediate, and ulnar columns.
|
 |
|
Figure 13.4.
Implants constructed specifically for the anatomy of the distal radius have allowed limited fixation of fracture components and minimization of prior problems associated with larger nonspecific implants. |
 |
|
Figure 13.5. Fractures involving compression or shearing of the articular surface may be accompanied by intercarpal ligament injury.
|
|
Table 13.1. Definite Indications for Open Reduction and Internal Fixation
|
|
|---|---|
|
on operative fixation of distal radius fractures: specific aspects of
the fracture itself, the presence of associated soft-tissue injury such
as median nerve dysfunction; associated ipsilateral limb injury, and
the overall physical and medical condition of the patient. With the
advent of fixed-angle locking screw-plate constructs, underlying
osteopenia is no longer a contraindication to internal fixation.
subluxations or dislocations, displaced radial-styloid fractures,
articular fractures involving a displaced and rotated volar
lunate-facet component, and those displaced fractures presented 3 weeks
after the injury (Table 13.1).
different fractures. These include bilateral displaced fractures,
fractures associated with ipsilateral limb trauma, some fractures with
associated progressive swelling or nerve dysfunction, open fractures,
fractures associated with DRUJ instability, or unstable extra or
intra-articular fractures that were not reduced after closed reduction
and cast immobilization (Table 13.2).
of anesthesia, with poor compliance, or with local soft-tissue
conditions, such as active infection or complex regional pain syndrome,
may not benefit from internal fixation for their fracture (Table 13.3).
of the patient’s overall condition, as well as that of the involved
limb and hand, must be made before a decision is rendered to proceed
with operative intervention. The fracture characteristics are not
always easily appreciated before the fracture is reduced and repeat
x-rays are taken. Furthermore,
additional
x-ray views, including oblique views to focus on the articular surface,
or CT studies may further influence the decision about intervening
operatively.
|
Table 13.2. Relative Indications for ORIF
|
|
|---|---|
|
|
Table 13.3. Relative Contraindications to ORIF
|
|
|---|---|
|
and/or extensive metaphyseal comminution, the potential for autogenous,
allograft, bone-substitute grafts should be noted in the preoperative
plan. The patient should also be informed that bone grafting may be
necessary.
tourniquet control, and have the involved limb extended on a hand
table. The advent of relatively small, versatile, mini c-arms has
greatly facilitated intraoperative imaging. Because distal radius
fractures may be operatively approached through different exposures, we
will highlight several approaches with emphasis on the pitfalls and
pearls for each.
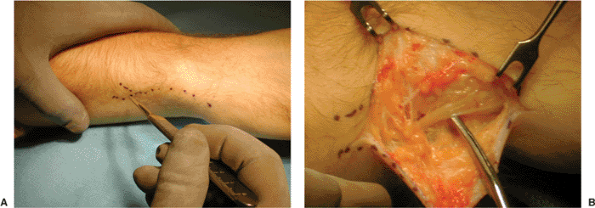
extra-articular, volar, displaced Smith’s and many dorsally displaced
fractures may be approached through the standard distal limb of the
Henry exposure. The interval is created between the radial artery and
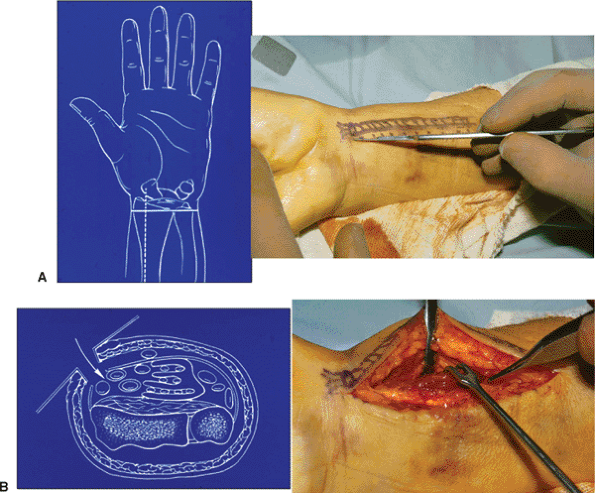
flexor carpi radialis tendon. (Fig. 13.6).
trauma or those involving a small, displaced, volar, lunate-facet
fragment are better exposed through an extended ulnar-based incision
that creates an interval between the ulnar nerve and artery and flexor
tendons. Extending this incision distally to release the transverse
carpal ligament will further facilitate exposure (Fig. 13.7).
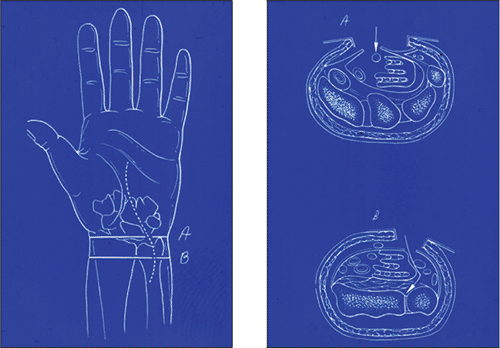
additional, extensile, volar, radial approach. By extending the Henry
approach more distally, the surgeon releases the fibrous septum
overlying the flexor carpi radialis and step cuts the insertion of the
brachioradialis tendon, which will permit further displacement of the
distal fragment and thus allow for exposure of the dorsal surface of
the distal fragment (Fig. 13.8).
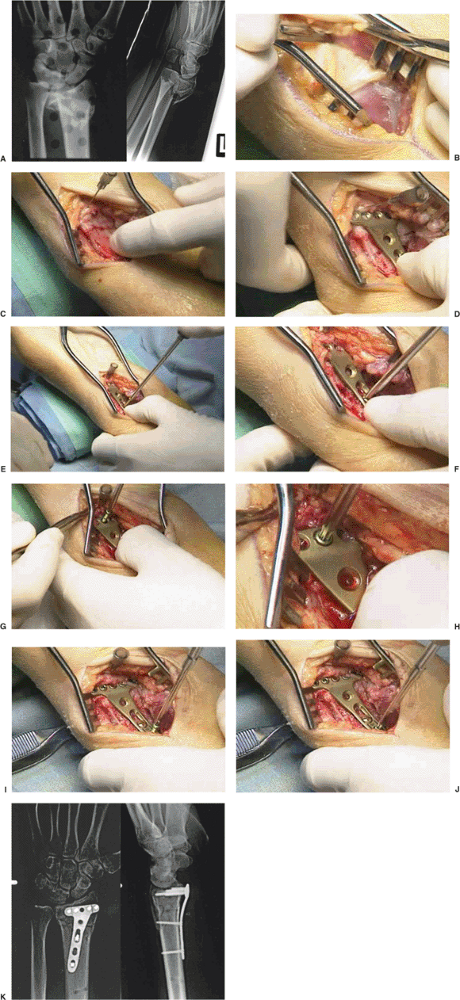
surgeon must take care to retract the muscle belly of the flexor
pollicis longus exposing the pronator quadratus. The pronator is
necessarily and sharply elevated in L fashion either from the radial
aspect of the radius or from its ulnar attachment. Whenever possible,
the proximal pedicle of the anterior interosseous artery should be
preserved to maintain muscle viability and limit the potential for a
pronation contracture that develops due to ischemia of the pronator
quadratus (Fig. 13.9).
reduction using longitudinal traction and direct digital manipulation
of the distal fracture fragment(s). Another advantage of the anterior
approach is the surgeon’s ability to judge rotational alignment as well
as length by reducing the volar, cortical fracture lines; this area is
less likely to be comminuted even in impacted, dorsally displaced
fractures (see Fig. 13.9C).
the specific anatomy of the volar surface increase stability of
fixation. The distal screws, if placed in the subchondral position
further enhance the stability of fixation, especially in osteopenic
bone (see Fig 13.9D–K).
 |
|
Figure 13.6. The volar approach of Henry creates an interval between the flexor carpi radialis and radial artery.
|
 |
|
Figure 13.7.
More extensile exposure of the volar aspect of the distal radius is achieved through a volar ulnar incision that creates an interval between the ulnar artery and nerve and flexor tendons. |
 |
|
Figure 13.8.
The extensile flexor carpi-radialis exposure developed by Orbay involves distal release of the flexor carpi radialis septum, which permits wide exposure of the anterior surface as well as the ability to gain access to the dorsal surface of the distal fragment. (Courtesy of Jorge Orbay, MD.) |
the beam 20 degrees inclined from distal to proximal to ascertain both
the articular reduction. X-rays also ensure that distal screws have not
penetrated into the radiocarpal joint (Fig 13.10).
quadratus to serve as a covering over the implant. The postoperative
wrist is kept in a splint for 7 to 10 days after which sutures are
removed and active wrist motion is initiated.
pitfalls that may lead to loss of reduction or problems with internal
fixation:
-
When approaching the displaced volar
fracture in the older patient, one must suspect an element of dorsal
cortical comminution even if it is not apparent on the lateral x-ray.
An implant applied as a buttress pushing up the displaced, volar,
distal fragment has the potential of dorsally translating the fragment.
This will cause loss of the normal volar tilt of the distal articular
surface (Fig. 13.11). -
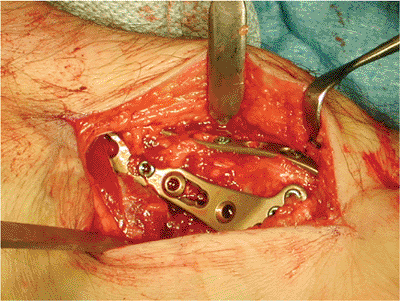
The volar, shearing, radiocarpal
fracture-subluxation (Barton’s fracture) most often will have two or
more distal-radius fragments. In some, the volar ulnar component may be
relatively small. Failure to support this fragment can result in
postoperative volar subluxation of both the small fragment as well as
the carpus (Fig 13.12). The very distal,
articular rim of the radius dips anteriorly both at the radial styloid
as well as at its most ulnar aspect. Therefore, one implant may be
unable to support the entire, distal, articular rim adequately (30). -
When stabilizing a three- or four-part
articular fracture through an anterior approach, the radial styloid
(column) component may not be protected against displacing shearing
forces when a single volar implant is used. In these instances, an
additional, small, contoured radial implant can be applied through the
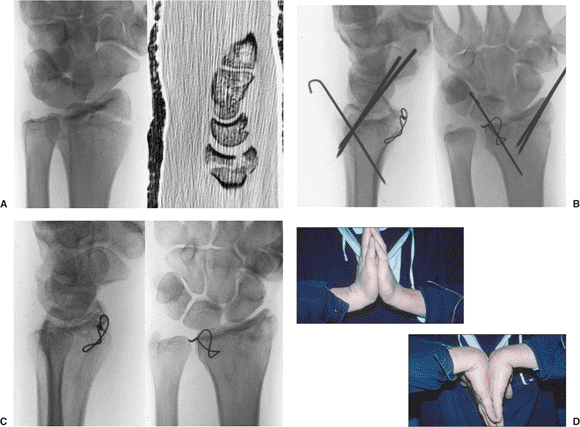
same exposure by step-cutting the brachioradialis insertion (Fig. 13.13). In addition, the volar lunate-articular facet fragment may be found to be rotated with minimal subchondral bony support (31).
We loop a wire through the volar capsular attachments to the fragment
and through a hole drilled transversely in the distal radius metaphysis
(Fig. 13.14) (32).
 |
|
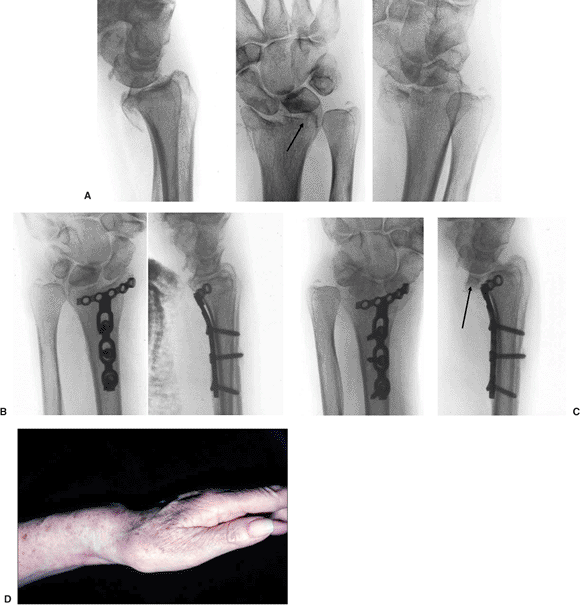
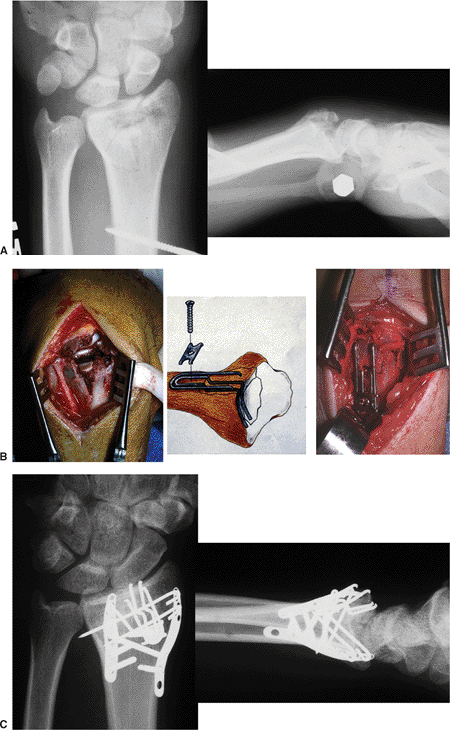
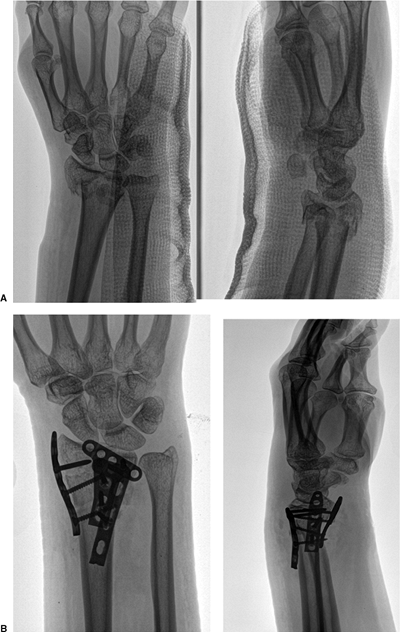
Figure 13.9. An unstable fracture in 56-year-old woman. A. The fracture x-rays. B. Exposure of the pronator quadratus. C.
Following elevation of the pronator quadratus, a needle is placed into the radiocarpal joint marking the distal volar cortical rim. The fracture is reduced. D. The 2.4-mm plate is placed and checked using intraoperative fluoroscopy. E,F. The initial screw is placed in a proximal oval hole that will allow additional stability. G,H. The distal screws with threaded heads permit locking into the plate and angular stable fixation. I,J. Final screw insertion. K. Postoperative x-rays. |
 |
|
Figure 13.10.
Volar implants with locked head screws provide angular stability even in osteoporotic patients. Stability is enhanced by placing the distal screws in a subchondral position especially when stabilizing a dorsally displaced fracture from a volar approach. |
 |
|
Figure 13.11.
Dorsal translation of the distal fragment is a potential fixation problem of an unstable extra-articular fracture from a volar approach. The result is loss of normal volar angulation of the distal articular fragment. |
 |
|
Figure 13.12. Postoperative volar subluxation of the radiocarpal joint. A. Shearing radiocarpal-fracture subluxation with small lunate-facet fracture. B. Immediate postoperative radiographs. C. Subluxation of the radiocarpal joint noted at 2 weeks caused by failure to support lunate-facet fragment. D. Clinical appearance.
|
 |
|
Figure 13.13.
Complex articular fractures involving both the radial column and intermediate column can be stabilized from the volar approach using a radial column plate and volar surface plate. |
 |
|
Figure 13.14.
Fixation of a displaced, rotated, volar, ulnar, lunate-facet fragment can be done using a small gauge wire looped through the volar capsule and radius in a figure-of-eight fashion. A. Preoperative x-ray and CT scan reveal a displaced, volar, lunate facet. B. The radial styloid and dorsal lunate facet could be reduced and held with K wires, but the volar lunate facet required open reduction and wire loop fixation. C. Healed fracture at 1 year. D. Clinical wrist motion. |
 |
|
Figure 13.15. The surgical approach to the dorsal aspect of the radial styloid is through the first and second dorsal extensor compartment.
|
indications for a dorsal approach to the reduction and internal
fixation of the distal radius fracture. These include radial, styloid,
shearing fractures with associated impaction of the articular surface;
some complex four-part articular fractures in which the dorsal, lunate,
facet component cannot be reduced from a volar approach; complex
fractures associated with intercarpal ligament descriptions; and some
dorsally displaced fractures seen 3 weeks or more postinjury.
dorsal aspect of the distal radius. When approaching a radial styloid
fracture, the surgeon can make the incision on the dorsal radial
aspect, creating exposure between the first and second extensor
compartments. Care is always taken to avoid traction injuries to the
branches of the radial sensory nerve (Fig. 13.15).
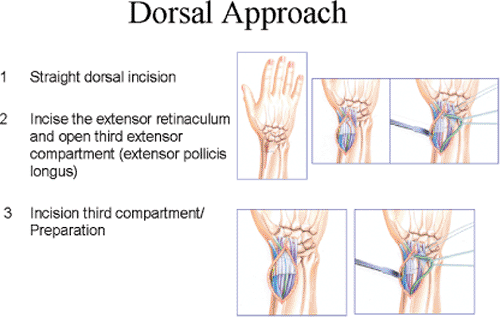
incision more dorsally and has several options for exposure of the
distal radius. The extensor retinaculum can be opened between the third
and fourth extensor compartments and the fourth extensor compartment
can be elevated subperiosteally toward the ulnar fragment. The second
extensor compartment can also be elevated subperiosteally (Fig. 13.16).
can also be made through two exposures through the extensor
retinaculum. One is between the first and second compartments, and
another is between the fourth and fifth compartments (Fig. 13.17A–E).
 |
|
Figure 13.16.
An extensile approach to the dorsal aspect of the distal radius is between the third and fourth extensor compartments. The fourth compartment and second extensor compartments are elevated subperiosteally. |
|
Figure 13.17. A complex intra-articular fracture treated with a fragment-specific plate through a dorsal approach. A,B. Anterior and lateral CT scans demonstrate clearly the articular and metaphyseal injury. C. A dorsal radial incision with a temporary external fixator on the limb. D. The extensor pollicis longus is elevated from its third extensor retinacular compartment. E. Exposure of the radial column can be made through the first and second extensor retinacular compartments. F. The radial column plate is placed in this interval. G,H. The position of the radial column plate is placed and checked via intraoperative fluoroscopy. I. The intermediate column is reached by elevating the fourth extensor compartment subperiosteally. J. A 2.4-mm L plate is placed over a K wire. K. Using a small clamp to hold both plates, the initial proximal screw is placed. L,M. The position of both plates and fracture reduction is controlled through use of intraoperative fluoroscopy. N. A special drill guide permits the locking head screws to be placed directly in the center of the hole. O. The distal screws are placed and locked into the plate. P. Postoperative radiographs of the internal fixation.
|
 |
|
Figure 13.18. A dorsoulnar approach to the distal ulna and ulna styloid. A. The incision is marked out. B. Identification and protection of the branches of the dorsal ulnar sensory nerve.
|
accomplished by longitudinal traction and direct manipulation of the
fracture fragments (see Fig. 13.17F–O). A
central articular impaction, which may be ineffectively reduced with
traction alone, will require direct elevation through the fracture site
and control of the articular reduction that is judged after an
arthrotomy of the radiocarpal joint. Direct evaluation is also
advisable when concern exists regarding intercarpal ligament injury.
traction can be considered. It is especially useful for fractures seen
late or associated with soft-tissue swelling.
of importance with unstable articular fractures. It will help control
the reduction when using intraoperative image intensification.
problems involving the distal ulna. A longitudinal incision is created
along the diaphysis. The surgeon notes that the ulnar styloid lies
relatively anterior to the ulnar diaphysis (Fig. 13.18).
dependent upon the fracture pattern and available implants. The concept
of “fracture-specific fixation” espoused independently by Medoff as
well as Rikli and Regazzoni (26) has led to the
use of small strategically placed implants to support the specific
fracture fragments. These include anatomically shaped plates, pins, and
wire forms (Figs. 13.19 and 13.20).
autogenous bone graft, bone substitute, or allograft, will be based
upon whether a defect exists under an articular fragment and/or the
stability of the internal fixation. The development of implants with
locked screw heads, which creates angular stable fixation, has
substantially decreased the requirement for bone graft.
This leaves the extensor pollicis longus outside of the retinacular
closure.
injury to the distal radioulnar joint. While most do not result in
instability, they are best recognized and treated concomitantly with
the radius fracture.
 |
|
Figure 13.19. A complex intra-articular fracture treated with fragment specific fixation using wire forms and pin plate. A. The x-rays of the fracture. B. The use of the wire form to support the impacted articular fracture. C. X-rays of the healed fracture. (Case courtesy of Dr. Robert Medoff).
|
 |
|
Figure 13.20. A complex intra-articular fracture treated with fragment-specific volar and dorsal plates. A. The initial fracture x-rays. B. X-ray of the three plates at 3 months postsurgery.
|
stability of the distal radioulnar joint should be assessed in every
patient. This is best performed by attempting to displace the distal
ulna from the sigmoid notch of the radius in forearm pronation,
neutral, and supination. If the ulna head can be displaced completely,
the possibility of instability should be considered.
especially those occurring at the base of the styloid, stability will
be restored following internal fixation of the styloid. This is best
accomplished through a separate incision along the diaphysis of the
distal ulna; the surgeon should keep in mind the more anterior location
of the styloid process. Also, the surgeon should identify and protect
the dorsal sensory branch of the ulnar nerve, which divides into three
branches at or about the level of the ulnar styloid. Internal fixation
can be accomplished in several ways, including via K wires along with a
tension band, a small screw, or combination of screw and tension band. (Fig. 13.21).
associated ulna-styloid fracture, alternative treatment options include
postoperative immobilization of the wrist and forearm in an above-elbow
splint for 4 weeks, cross pinning the ulna to radius for a similar
period and application of an above elbow splint; or open repair of the
triangular fibrocartilage complex also followed by forearm
immobilization for 4 to 6 weeks.
ulna-neck fracture, which may also require internal fixation.
Alternatives will include an intramedullary smooth pin placed
percutaneously or an ORIF with a small plate (33).
 |
|
Figure 13.21. The ulna styloid and/or neck fracture can be stabilized with a screw, tension band wire, or plate.
|
dressing combined with a volar plaster splint for the initial 7 to 10
days postsurgery. During this period, the patient is encouraged to
mobilize their upper limb, regain digital mobility, and incorporate
their hand and limb in activities of daily living. In those patients in
whom distal radioulnar-joint instability was present, the forearm is
also immobilized for 14 to 21 days. During this initial recovery
period, anti-edema measures should be encouraged including elevation,
digital mobilization, and elastic wrapping if indicated.
evaluation and instruction by an occupational or physical therapist,
active wrist and forearm range of motion is initiated. Resistive
activities are withheld until healing is assured (ordinarily after 6 to
8 weeks). Patients often need exercises for strength and motion for at
least 3 months postsurgery with a functional end point often reached
only after 12 to 18 months.
distal radius fractures are well recognized. They include loss of
fixation, infection, nerve compression, complex regional-pain syndrome,
digital and/or wrist stiffness among others (34,35,36).
Careful patient selection, pre-operative planning, technical care in
fixation and careful postoperative management will help minimize these
adverse outcomes.
JK, Amadio PC, Cooney WP. Open reduction and internal fixation of
displaced, comminuted intra-articular fractures of the distal end of
the radius. J Bone Joint Surg Am 1989;71(6):839–847.
PR, Frederick HA, Laseter GF. Open reduction and internal fixation of
unstable distal radius fractures with a low-profile plate: a
multicenter study of 73 fractures. J Hand Surg [Am] 1998;23(2):300–307.
LW III, Cole RJ, Gelberman RH, et al. Displaced intra-articular
fractures of the distal aspect of the radius: long-term results in
young adults after open reduction and internal fixation. J Bone Joint Surg Am 1997;79(9):1290–1302.
RJ, Bindra RR, Evanoff BA, et al. Radiographic evaluation of osseous
displacement following intra-articular fractures of the distal radius:
reliability of plain radiography versus computer tomography. J Hand Surg [Am] 1997;22(5):792–800.
D, Jupiter JB, Brennwald J, et al. Prospective multicenter trial of a
plate for dorsal fixation of distal radius fractures. J Hand Surg Am 1997;22(5):777–784.
RA, Lipson SR, Applegate B, et al. Treatment of severely comminuted
intra-articular fractures of the distal end of the radius by open
reduction and combined internal and external fixation. J Bone Joint Surg Am 2001;83(4):509–519.
AG, Ip WY, Poon TL, et al. Open reduction and plate fixation of
displaced AO Type C3 fractures of the distal radius: restoration of
articular congruity in eighteen cases. J Orthop Trauma 2001;15(5):350–357.
DM, Dowdle J, Glickel SZ, et al. Tomography versus computed tomography
for assessing step off in intraarticular distal radial fractures. Clin Ortho 1999;361:199–204.
JB, Fernandez DL, Toh CL, et al. Operative treatment of volar
intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am 1996;78(12):1817–1828.
DA, Regazzoni P. Fractures of the distal end of the radius treated by
internal fixation and early function: a preliminary report of 20 cases.
J Bone Joint Surg Br 1996;78(4):588–592.
WK II, Velazquez PA. The application of indirect reduction techniques
in the distal radius: the role of adjuvant arthroscopy. Arthroscopy 2000;6(8):830–835.
N, Jupiter J, Fernandez D, et al. Loss of fixation of the volar lunate
facet after volar plating of distal radius fracture. J Bone Joint Surg Am 2004;86:1900–1908.
D, McCarty P, Campbell D, et al. Condylar blade plate fixation of
unstable fractures of the distal ulna associated with fracture of the
distal radius. J Hand Surg 2004;29:103–109.
G. Fracture of the distal radius including
sequelae—shoulder-hand-finger syndrome, disturbance in the distal
radio-ulnar joint and impairment of nerve function: a clinical and
experimental study. Acta Orthop Scand 1967;108:5–153.
