CHAPTER 8 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 8 – Arthroscopic Repair of Posterior Shoulder Instability
James P. Bradley, MD
Posterior instability is relatively uncommon compared with anterior instability of the shoulder. Most authors agree that posterior shoulder instability represents approximately 2% to 10% of shoulder instability cases. [4] [8] [13] Initial attempts to clarify the distinctions of posterior instability were made in 1962, when McLaughlin recognized that differences exist between “fixed and recurrent subluxations of the shoulder,” suggesting that the etiology and treatment of the two are distinctly different.[15] More than 20 years later, in the early 1980s, Hawkins[8] reviewed the difference between true dislocations and subluxations and noted that true recurrent posterior dislocations are rare compared with subluxation episodes. Since that time, additional knowledge has been gained in the differences between unidirectional and multidirectional, traumatic and atraumatic, acute and chronic, and voluntary and involuntary posterior instability. In many respects, each of these may represent a distinct form of posterior instability with its own underlying predispositions, anatomic abnormalities, and treatment algorithms. [16] [18] Our collective understanding of posterior shoulder instability continues to evolve.
Recent advances in our understanding of the spectrum of posterior instability have been gained through the study of shoulder injuries in athletes, patients with generalized ligamentous laxity, and patients with posttraumatic injuries. Acute posterior dislocations typically result from a direct blow to the anterior shoulder or indirect forces that couple shoulder flexion, internal rotation, and adduction. [4] [8] The most common indirect causes are accidental electric shock and convulsive seizures. Because of incomplete radiographic studies and a failure to recognize the posterior shoulder prominence and mechanical block to external rotation, 60% to 80% of locked posterior dislocations are missed on initial presentation. Additional pathologic processes are frequently associated with posterior instability and include the reverse Hill-Sachs lesion, the reverse bony Bankart lesion, posterior capsular laxity, excessive humeral head retroversion or chondrolabral retroversion, and glenoid hypoplasia.
To diagnose posterior instability, the clinician must perform a thorough history and physical examination as well as maintain a high index of suspicion. A history of a posterior dislocation requiring formal reduction is more obvious; however, patients with recurrent posterior subluxation may present with more subtle findings. The majority of patients with recurrent posterior subluxation complain primarily of pain with specific activities, particularly in the provocative position (90-degree forward flexion, adduction, and internal rotation), [4] [8] more so than of instability.
| • | Active and passive range of motion | |
| • | Palpation for tenderness | |
| • | Strength testing | |
| • | Evaluation for impingement | |
| • | Assessment for generalized ligamentous laxity |
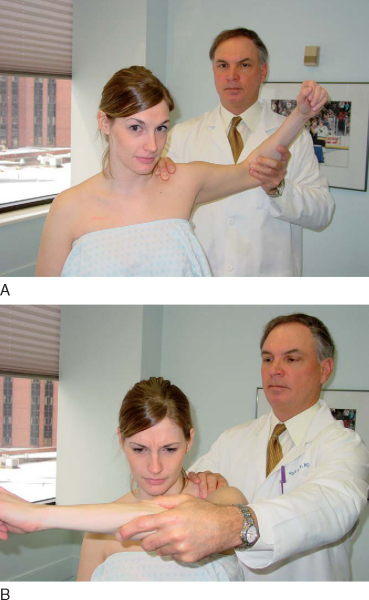
| • | Load and shift test for anterior and posterior translation ( Fig. 8-1 ) |
|
| • | Sulcus sign (in both neutral and external rotation) for inferior translation | |
| • | Sulcus sign graded as 3+ that remains 2+ in external rotation is pathognomonic for multidirectional instability |
|
|
|
|
Figure 8-1 |
| • | Jerk test ( Fig. 8-2 ) |
|
| • | Kim test ( Fig. 8-3 ) |
|
| • | Circumduction test |
|
|
|
|
Figure 8-2 |
|
|
|
|
Figure 8-3 |
| • | Including axillary view | |
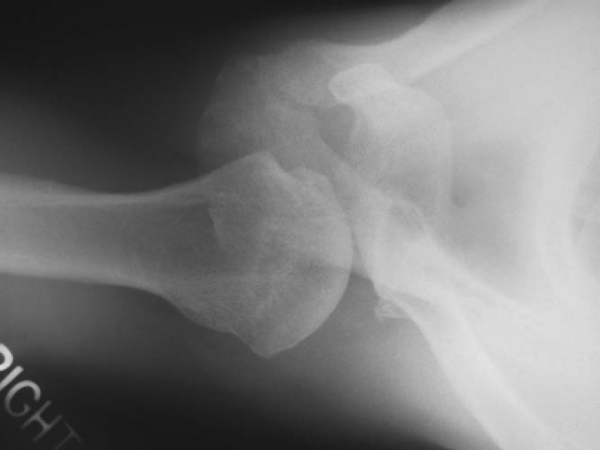
| • | Evaluate for reverse Hill-Sachs lesions ( Fig. 8-4 ), glenoid pathologic changes (retroversion, fractures, and hypoplasia), bony humeral avulsion of the glenohumeral ligaments |
Magnetic Resonance Arthrography
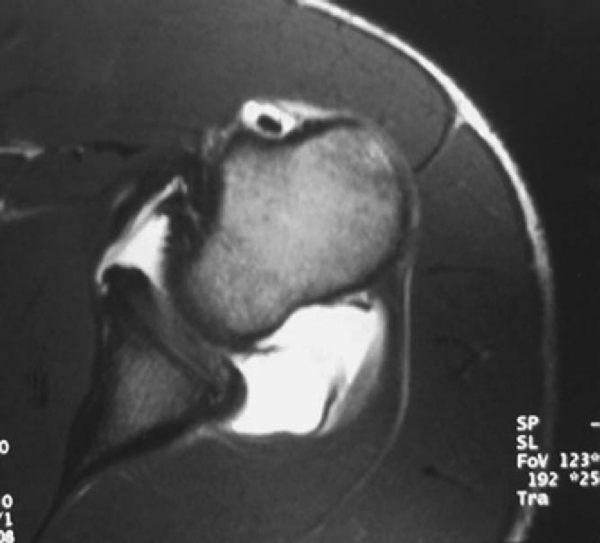
| • | Evaluate labrum, capsule, biceps tendon, subscapularis integrity ( Fig. 8-5 ) |
|
|
|
|
Figure 8-5 |
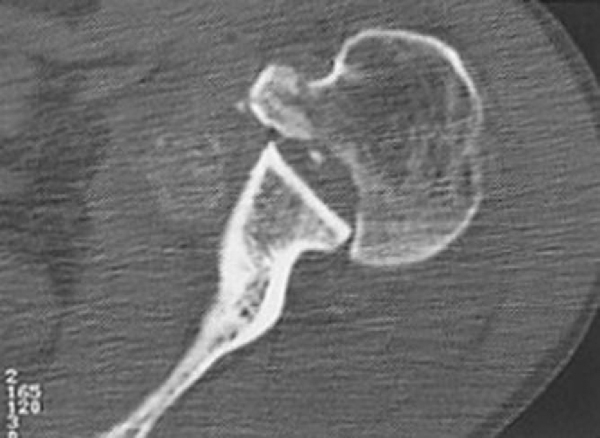
| • | Evaluate for glenoid version, locked dislocation ( Fig. 8-6 ) |
|
|
|
|
Figure 8-6 |
Indications and Contraindications
Many patients with recurrent posterior subluxation can be managed successfully without surgery. Numerous authors have proposed a period of no less than 6 months of physical therapy before surgical treatment is considered. Effect ive rehabilitation includes avoidance of aggravating activities, restoration of a full range of motion, and shoulder strengthening. Strengthening of the rotator cuff, posterior deltoid, and periscapular musculature is critical. The premise of such directed physical therapy is to enable the dynamic muscle stabilizers to offset the deficient static capsulolabral restraints. Nearly 70% of patients will improve after an appropriate rehabilitation protocol. The recurrent subluxation, however, is generally not eliminated, but the functional disability is diminished enough that it does not prevent activities. If the disability fails to improve with an extended 6-month period of directed rehabilitation, or in select cases of posterior instability resulting from a macrotraumatic event, surgical intervention should be considered.
Relative indications include patients with an antecedent macrotraumatic injury.
Relative contraindications may include chronic instability resulting in compromised capsulolabral tissue and patients who have undergone previous open surgery.
Because successful results have been achieved after arthroscopic treatment of posterior labral tears in contact athletes, arthroscopic reconstruction is not contraindicated in that population.
The procedure can be performed under interscalene block or general endotracheal anesthesia with an interscalene block for postoperative pain control.
The examination under anesthesia is performed on a firm surface with the scapula relatively fixed and the humeral head free to rotate. A load-and-shift maneuver, as described by Murrell and Warren, is performed with the patient supine.[12] The arm is held in 90 degrees of abduction and neutral rotation while a posterior force is applied in an attempt to translate the humeral head over the posterior glenoid. A sulcus sign test is performed with the arm adducted and in neutral rotation to assess whether the instability has an inferior component. A 3+ sulcus sign that remains 2+ or greater in external rotation is considered pathognomonic for multidirectional instability. Testing is completed on both the affected and unaffected shoulders, and differences between the two are documented.
Patient Positioning, Landmarks, and Portals
The patient is then placed in the lateral decubitus position with the affected shoulder positioned superior. An inflatable beanbag and kidney rests hold the patient in position. Foam cushions are placed to protect the peroneal nerve at the neck of the fibula on the down leg. An axillary roll is placed. The operating table is placed in a slight reverse-Trendelenburg position. The full upper extremity is prepared to the level of the sternum anteriorly and the medial border of the scapula posteriorly. The operative shoulder is placed in 10 pounds of traction and positioned in 45 degrees of abduction and 20 degrees of forward flexion. The bone landmarks, including the acromion, distal clavicle, and coracoid process, are demarcated with a marking pen.
After preparation and draping, the glenohumeral joint is injected with 50 mL of sterile saline through an 18-gauge spinal needle to inflate the joint. A posterior portal is established 1 cm distal and 1 cm lateral to the standard posterior portal to allow access to the rim of the glenoid for anchor placement (
Fig. 8-7
). An anterior portal is then established high in the rotator interval by an inside-to-outside technique with a switching stick. Alternatively, it can also be established by an outside-to-inside technique with the assistance of a spinal needle. Typically, only anterior and posterior portals are required to perform the procedure. An accessory 7-o’clock portal has been described but is not frequently used in our technique.
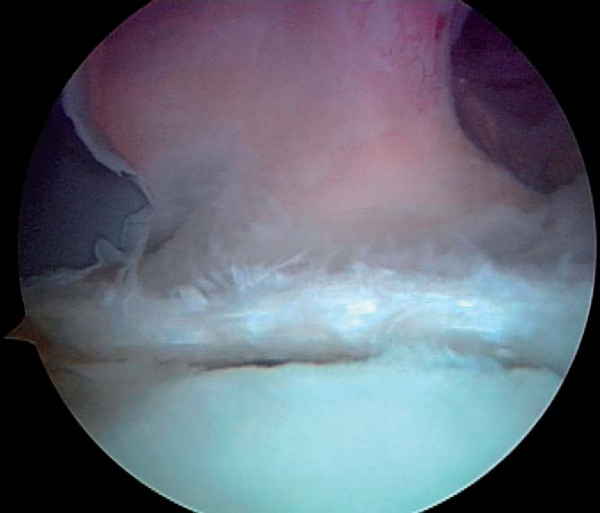
A diagnostic arthroscopy of the glenohumeral joint is then undertaken. The labrum, capsule, biceps tendon, subscapularis, rotator interval, rotator cuff, and articular surfaces are visualized in systematic fashion. This ensures that no associated lesions will be overlooked by poorly directed tunnel vision. Lesions typically seen in posterior instability include a patulous posterior capsule, posterior labral tear, labral fraying and splitting, widening of the rotator interval, and undersurface partial-thickness rotator cuff tears. After the glenohumeral joint is viewed from the posterior portal, the arthroscope is switched to the anterior portal to allow improved visualization of the posterior capsule and labrum. A switching stick can then be used in replacing the posterior cannula with an 8.25-mm distally threaded clear cannula (Arthrex, Inc., Naples, Fla), thus allowing passage of an arthroscopic probe and other instruments through the clear cannula to explore the posterior labrum for evidence of tears.
Specific Steps (
Box 8-1
)
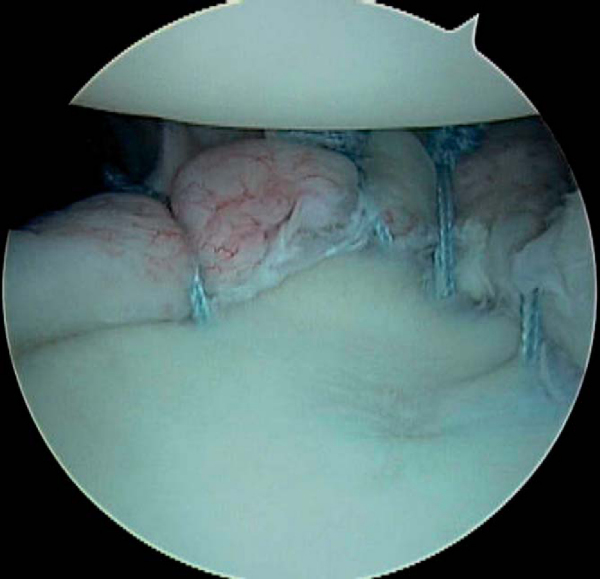
When the posterior labrum is detached, suture anchors are employed in performing the repair. The posterior labrum is visualized from both the posterior and anterior portals to appreciate the full extent of the tear (
Fig. 8-8
| • | The arthroscope then remains in the anterior portal, and the posterior portal serves as the working portal for the repair. | |
| • | An arthroscopic rasp or chisel is used to mobilize the torn labrum from the glenoid rim ( Fig. 8-9 ). |
|
| • | A motorized synovial shaver or meniscal rasp is used to abrade the capsule adjacent to the labral tear and to débride and decorticate the glenoid rim to achieve a bleeding surface. |
| Surgical Steps | |||||||||||||||||||||
|
|
|
|
|
Figure 8-8 |
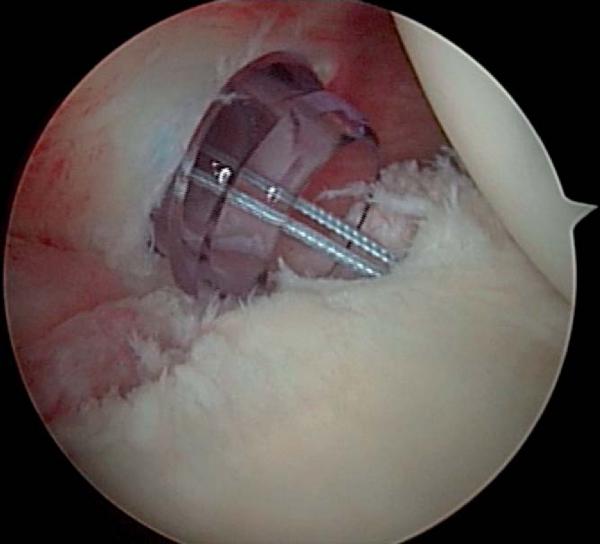
2. Placement of Suture Anchors
| • | Suture anchors are then placed at the articular margin of the glenoid rim, rather than down on the glenoid neck, to perform the labral repair ( Fig. 8-10 ). |
|
| • | A posterior labral tear extending from 6-o’clock to 9-o’clock on a right shoulder is typically repaired with suture anchors at the 6:30, 7:30, and 8:30 positions. | |
| • | We prefer the 3.0-mm Bio-Suture Tak suture anchor with No. 2 FiberWire (Arthrex, Inc., Naples, Fla) because of the ease of placing the anchor on the glenoid surface, but a number of other commercially available anchors are also adequate. | |
| • | The suture anchor is placed with the sutures oriented perpendicular to the glenoid rim to facilitate passage of the most posterior suture through the torn labrum. | |
| • | Avoid inadvertent injury to the articular cartilage. |
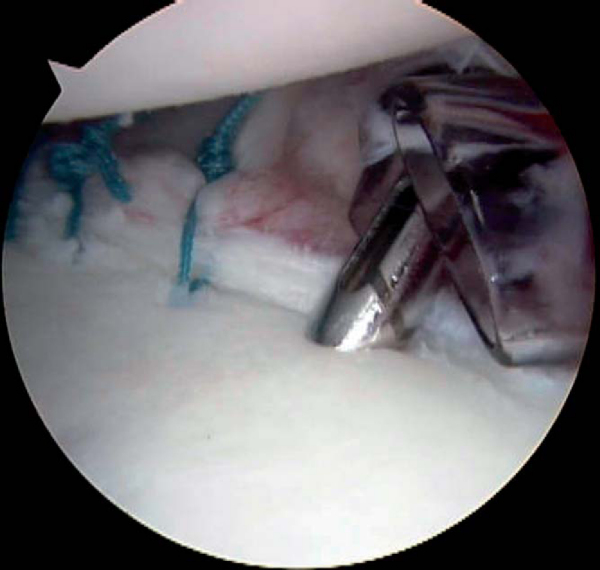
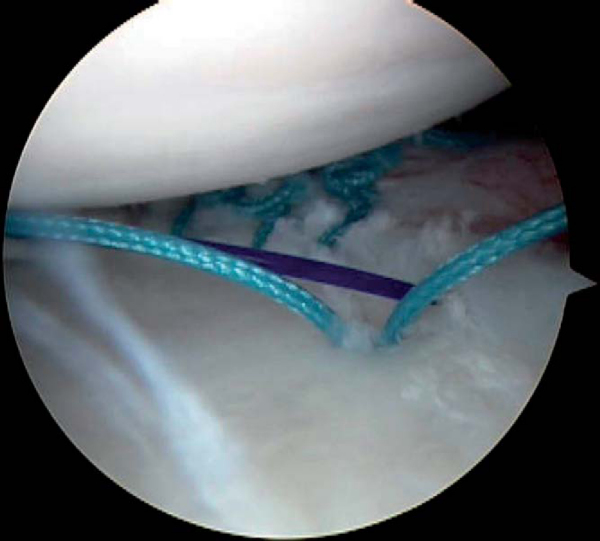
| • | After placement of the suture anchors, a 45-degree Spectrum suture hook (Linvatec, Largo, Fla) is loaded with a No. 0 polydioxanone (PDS) suture (Ethicon, Inc., Somerville, NJ). The contralateral side hook is chosen (i.e., a left 45-degree hook for a right shoulder when it is introduced from the posterior portal). Alternatively, there are other commercially available suture passers and suture relays that will also suffice. | |
| • | The suture passer is delivered through the torn labrum and advanced superiorly, reentering the joint at the edge of the glenoid articular cartilage ( Fig. 8-11 ). |
|
| • | Tension must be restored into the posterior band of the inferior glenohumeral ligament to re-establish posterior stability. | |
| • | Patients with acute injuries and less evidence of capsular stretching do not require the same degree of capsular advancement as do those with more chronic instability. | |
| • | In the setting of a labral tear with some capsular laxity, the suture passer is advanced through the posterior capsule approximately 1 cm lateral to the edge of the labral tear and then underneath the labral tear, to the edge of the articular cartilage, the so-called pleat stitch ( Fig. 8-12 ). |
|
| • | Placement of as many pleat stitches as necessary in a patulous shoulder capsule can reduce capsular redundancy. | |
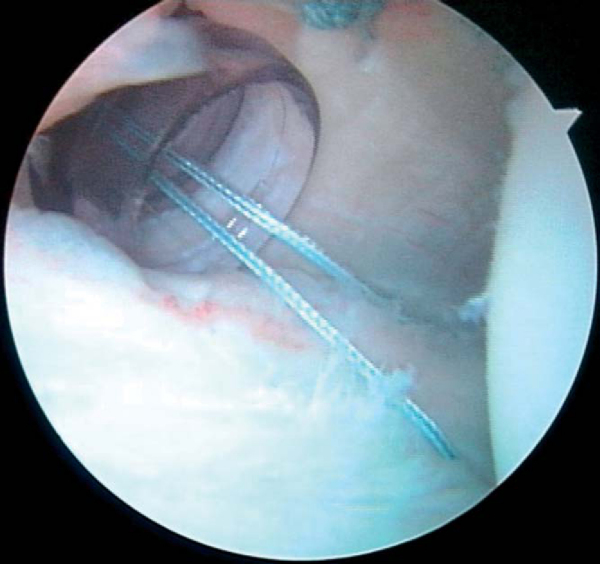
| • | The PDS suture is then fed into the glenohumeral joint, and the suture passer is withdrawn through the posterior clear cannula. | |
| • | An arthroscopic suture grasper is used to withdraw both the most posterior suture in the suture anchor and the end of the PDS suture that has been advanced through the torn labrum. This move detangles the sutures in the cannula. | |
| • | The PDS suture is then fashioned into a single loop and tightly tied over the end of the braided suture. | |
| • | The most lateral PDS suture, which has not been tied to the braided suture, is then pulled through the clear cannula ( Fig. 8-13 ). |
|
| • | This advances the most posterior suture in the suture anchor behind the labral tear ( Fig. 8-14 ). |
|
| • | A labral tear at the 7-o’clock position is advanced to the 7:30 suture anchor, and the 8-o’clock labral tear position is advanced to the 8:30 suture anchor. Additional sutures are then placed in similar fashion to complete the labral repair. | |
| • | If the capsule requires further tension, suture capsulorrhaphies can be performed in the intervals between the suture anchors directly to the newly secured labrum. | |
| • | Knots are tied after the passage of each suture, which allows continued assessment of the repair and the degree of the capsular shift achieved by each suture |
|
|
|
|
Figure 8-12 |
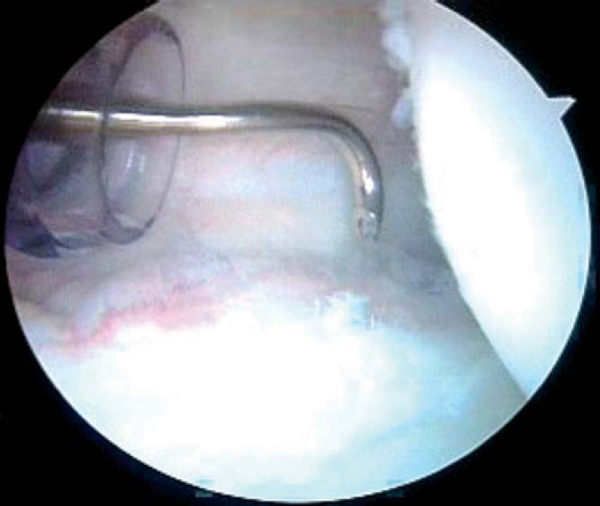
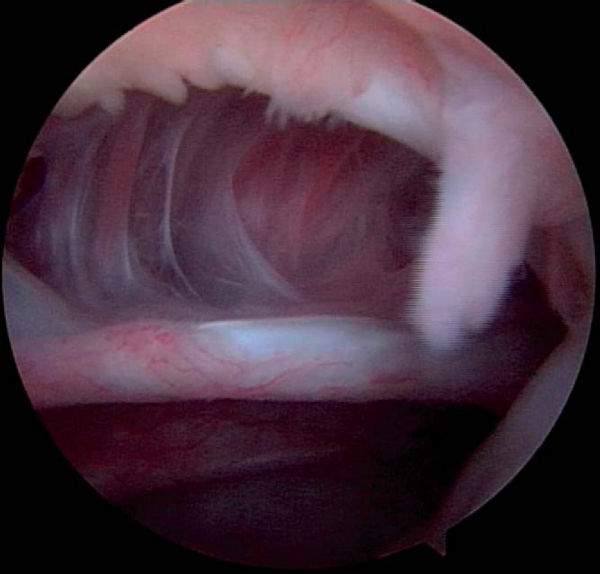
| • | The majority of patients with unidirectional posterior instability and primary posterior multidirectional instability do not have a posterior labral tear and typically display significant capsular laxity at arthroscopy ( Fig. 8-15 ). An isolated posterior capsulorrhaphy is performed. |
|
| • | Suture capsulorrhaphies are placed from inferior (6-o’clock) to superior (10-o’clock). | |
| • | The 6:30 capsular suture is typically advanced to the 7:30 position, and the reduction in capsular volume is assessed. | |
| • | Restoration of adequate tension in the posterior band of the inferior glenohumeral ligament is critical. | |
| • | Additional sutures are then placed at the 7:30, 8:30, and 9:30 positions on the capsule, advancing to the 8:30, 9:30, and 10:30 positions on the glenoid ( Fig. 8-16 ). |
|
| • | Sutures are tied after each is passed. If the sutures are not tied until the end, one errant suture may necessitate removal of all other sutures to achieve correction. |
| • | An arthroscopic awl is employed to penetrate the bare area of the humerus, under the infraspinatus tendon, in an effort to achieve some punctate bleeding to augment the healing response. | |
| • | The posterior capsular portal incision is then closed by passage of a PDS suture through the crescent Spectrum suture passer and retrieval of the suture with an arthroscopic penetrator. | |
| • | Varying the distance of the suture from the portal incision allows titration of the capsulorrhaphy. | |
| • | The PDS suture is then tied blindly in the cannula, closing the posterior capsular incision ( Fig. 8-17 ) |
Rehabilitation and Return to Play Recommendations
The rehabilitation program consists of a series of phases. Initially, the posterior capsule must be protected by avoiding extremes of internal rotation.
The complications include general risks of surgery, such as infection and hematoma formation, as well as risks particular to arthroscopic posterior shoulder stabilization, such as recurrent instability and stiffness.
| PEARLS AND PITFALLS | |||||||||||||||
|
Results of studies of arthroscopic repair of posterior shoulder instability are presented in
Table 8-1
.
| Author | Followup | Outcome |
|---|---|---|
| Papendick and Savoie[13] (1995) | 10 months | 39 of 41 (95%) successful |
| McIntyre et al[11] (1997) | 31 months | 15 of 20 (75%) successful |
| Savoie and Field[15] (1997) | 34 months | 55 of 61 (90%) successful |
| Wolf and Eakin[18] (1998) | 33 months | 12 of 14 (86%) successful |
| Mair et al[10] (1998) | 2-year minimum | 9 of 9 (100%) successful |
| Antoniou et al[1] (2000) | 28 months | 35 of 41 (85%) successful |
| Williams et al[17] (2003) | 5.1 years | 24 of 26 (92%) successful |
| Kim et al[9] (2003) | 39 months | 26 of 27 (96%) successful |
| Fluhme et al[6] (2004) | 34 months | 15 of 18 (83%) successful |
| Bottoni et al[2] (2005) | 40 months | 16 of 18 (88%) successful |
| Provencher et al[14] (2005) | 39 months | 26 of 33 (79%) successful |
| Bradley et al[3] (2006) | 27 months | 91 of 100 (91%) successful |
1.
Antoniou J, Duckworth DT, Harryman II DT: Capsulolabral augmentation for the management of posteroinferior instability of the shoulder.
J Bone Joint Surg Am 2000; 82:1220-1230.
2.
Bottoni CR, Franks BR, Moore JH, et al: Operative stabilization of posterior shoulder instability.
Am J Sports Med 2005; 33:996-1002.
3.
Bradley JP, Baker CL, Kline AJ, et al: Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders.
Am J Sports Med 2006; 34:1061-1071.
4.
Burkhead Jr WZ, Rockwood Jr CA: Treatment of instability of the shoulder with an exercise program.
J Bone Joint Surg Am 1992; 74:890-896.
5.
Davidson PA, Rivenburgh DW: The 7-o’clock posteroinferior portal for shoulder arthroscopy.
Am J Sports Med 2002; 30:693-696.
6.
Fluhme DJ, Bradley JP, Burke CJ, et al. Open versus arthroscopic treatment for posterior glenohumeral instability. Presented at the American Orthopaedic Society for Sports Medicine annual meeting; Quebec City, Canada; June 24–27, 2004.
7.
Harryman DT, Sidles JA, Harris SL, et al: The role of the rotator interval capsule in passive motion and stability of the shoulder.
J Bone Joint Surg Am 1992; 74:53-66.
8.
Hawkins RJ, Koppert G, Johnston G: Recurrent posterior instability (subluxation) of the shoulder.
J Bone Joint Surg Am 1984; 66:169.
9.
Kim SH, Ha KI, Park JH, et al: Arthroscopic posterior labral repair and capsular shift for traumatic unidirectional recurrent posterior subluxation of the shoulder.
J Bone Joint Surg Am 2003; 85:1479-1487.
10.
Mair SD, Zarzour RH, Speer KP: Posterior labral injury in contact athletes.
Am J Sports Med 1998; 26:753-758.
11.
McIntyre LF, Caspari RB, Savoie III FH: The arthroscopic treatment of posterior shoulder instability: two-year results of a multiple suture technique.
Arthroscopy 1997; 13:426-432.
12.
Murrell GA, Warren RF: The surgical treatment of posterior shoulder instability.
Clin Sports Med 1995; 14(4):903-915.
13.
Papendick LW, Savoie III FH: Anatomy-specific repair techniques for posterior shoulder instability.
J South Orthop Assoc 1995; 4:169-176.
14.
Provencher MT, Bell SJ, Menzel KA, Mologne TS: Arthroscopic treatment of posterior instability: results in 33 patients.
Am J Sports Med 2005; 33:1463-1471.
15.
Savoie III FH, Field LD: Arthroscopic management of posterior shoulder instability.
Oper Tech Sports Med 1997; 5:226-232.
16.
Tibone JE, Bradley JP: The treatment of posterior subluxation in athletes.
Clin Orthop 1993; 291:124-137.
17.
Williams III RJ, Strickland S, Cohen M, et al: Arthroscopic repair for traumatic posterior shoulder instability.
Am J Sports Med 2003; 31:203-209.
18.
Wolf EM, Eakin CL: Arthroscopic capsular plication for posterior shoulder instability.
Arthroscopy 1998; 14:153-163.