CHAPTER 51 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 51 – Débridement of Articular Cartilage in the Knee
Shawn Wynn, MD,
Lee Kaplan, MD
Articular cartilage injuries in the knee are a relatively common problem in today’s population. In fact, an estimated 900,000 Americans suffer cartilage injuries each year.[8] The integrity of a normally structured articular cartilage envelope is essential for proper joint function.[5] Curl et al[6] evaluated 31,516 arthroscopies and found 53,569 hyaline cartilage lesions during a 4-year period. Whereas articular cartilage injuries are common, injured cartilage has a limited ability to heal itself.[6]
The pain experienced with chondral lesions is believed to stem from the nerve endings in the exposed subchondral bone and knee effusions caused by articular debris. [20] [23] Studies have shown that loose articular cartilage flaps and exposed subchondral bone cause significant disability in the knee joint.[11] One study injecting cartilage fragments into rat knees resulted in joint effusions, articular cartilage friability, pitting, discoloration, and inflammatory arthritis.[8]
Once it is damaged, articular cartilage has a severe limitation for self-repair. Our knowledge of the pathophysiologic mechanisms of damage and repair of articular cartilage is currently in its infancy. This lack of complete understanding has stimulated a great deal of interest as well as research in this area. Multiple techniques ranging from mechanical débridement to surgical repair and cartilage transplantation exist for the treatment of articular cartilage defects.
Arthroscopic mechanical débridement with abrasion arthroplasty was first described by Johnson [14] [15] in the 1980s. Mechanical débridement of articular cartilage can remove unstable flaps, remove loose particles, and ultimately improve pain and function of the knee.
Articular cartilage defects can often be difficult to diagnose, with or without imaging. It is important to determine the possible cause of the cartilage defect. Any traumatic event in the past may be important; this may have been the inciting event that disrupted the integrity of the delicate articular cartilage. The degree of injury may be variable as well. A patient who suffered a severe knee dislocation may have larger or more extensive cartilage defects than a patient with the insidious onset of knee pain and no major trauma. An accurate history, including the duration and severity of symptoms, may be of great benefit when treatment options are considered. Associated ligamentous or meniscal injuries will also be important factors in compiling a treatment plan.
Patients with articular cartilage lesions often present with intermittent knee pain. The pain is commonly accompanied by intermittent effusions. In fact, effusions can occur in up to 70% of patients with articular cartilage lesions.[17] The presence of an effusion at the actual time of examination can be variable. Regardless, the presence of a knee effusion should not be overlooked. Patients may or may not remember a specific event or injury that is related to their symptoms. Pain, however, is the most common complaint. It may be reproduced at certain degrees of flexion or with certain positions or activities. Mechanical symptoms, such as popping, catching, and even locking, can be experienced as well.
Visual inspection, palpation, range-of-motion evaluation, joint line palpation, and ligament testing are performed in examination of the knee. A Lachman examination, pivot shift test, and anterior and posterior drawer tests are conducted, as is varus and valgus testing for lateral collateral ligament and medial collateral ligament stability. Ambulation and gait are observed. Strength testing and neurovascular examination are performed. Examination of the patellofemoral joint with squat testing, apprehension, and load testing is an important aspect as well. Specific to this type of lesion, the patient may be tender to palpation directly over the femoral condyles, in the location of the lesion. Palpation of the lesion often will produce a sharp pain in this region. Joint effusion is common and should be evaluated. Crepitation can also be felt while the knee is moved through a range of motion.
Radiographs should always be obtained in symptomatic patients but may be of limited use in narrowing the diagnosis to a cartilage lesion. Radiographs are important to eliminate other possible causes of pain. Weight-bearing anteroposterior, lateral, sunrise, 45-degree flexion posteroanterior, and alignment views are usually obtained and can help rule out degenerative joint disease, loose bodies, and fractures.
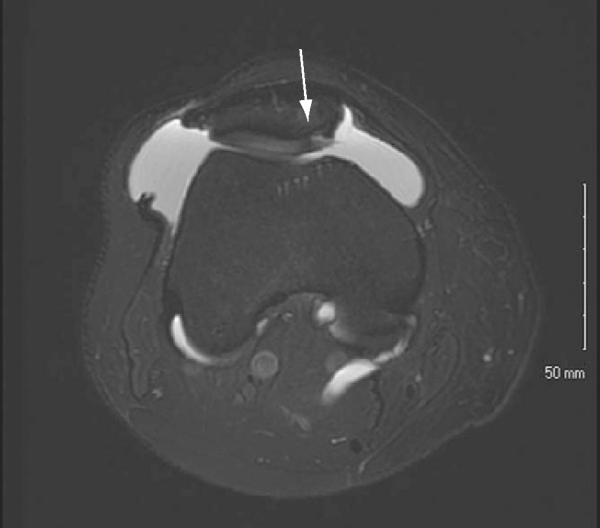
Magnetic resonance imaging (MRI) is the most useful imaging modality for the diagnosis of chondral lesions (
Fig. 51-1
); however, this is controversial. One study has shown the sensitivity of MRI for evaluation of chondral lesions to be as low as 21%.[18] Disler et al,[7] however, found a 93% sensitivity and 94% specificity for detection of cartilage lesions by three-dimensional spoiled gradient-echo MRI. The sensitivity and specificity of MRI depend on the imaging sequence as well as the grade of the cartilage lesion.[4] Ligament and meniscal pathologic processes are seen very well on MRI, as is soft tissue disease. Cartilage defects are more difficult to assess. The development of improved MRI machines, as well as new imaging sequences, may improve the sensitivity of MRI for identification of chondral lesions in the future.
|
|
|
|
Figure 51-1 |
Indications and Contraindications
Nonoperative treatment is typically the first line of treatment with these types of injuries. The duration of nonoperative treatment is surgeon and patient dependent. Treatment modalities include physical therapy, anti-inflammatory drugs, ice, rest, and closed chain muscle strengthening. Weight loss is also an important consideration. Compressive wraps or neoprene sleeves can be used to control and to minimize intermittent joint effusions.
Operative treatment is reserved for those whose course of nonoperative treatment has failed. This is often after 8 to 12 weeks of treatment but can be variable. The primary indication for operative treatment is mechanical symptoms. The goals of treatment are to stabilize loose articular cartilage, to decrease pain, and to improve function.
Mechanical débridement may be contraindicated in elderly patients with advanced degenerative changes, as the procedure may be of little benefit in advanced degenerative disease.
The choice of anesthesia is based on the preferences of the surgeon, the anesthesiologist, the patient, and the patient’s general medical condition. General endotracheal, spinal, and regional anesthesia with sedation are viable anesthetic options.
A proper time-out is performed to identify the patient, limb of surgery, and surgical procedure in the operating room. The patient is then placed in a supine position on a standard operating table. A side thigh post is used, and the foot of the bed is not dropped. Once adequate anesthesia is obtained, the patient is given preoperative prophylactic antibiotics, and a well-padded tourniquet is applied to the upper thigh. The tourniquet is placed but not inflated. The arthroscopy portal sites are preinjected with lidocaine and epinephrine.
After the patient has obtained adequate anesthesia, a standard ligamentous knee examination is performed. Range of motion, anterior cruciate ligament, posterior cruciate ligament, lateral collateral ligament, and medial collateral ligament are examined in standard fashion.
Surgical Landmarks, Incisions, and Portals
Standard arthroscopy portals are used. Landmarks include the medial and lateral joint lines, patella, and patellar tendon.
A superomedial portal is made for the inflow cannula. Next, an inferolateral camera portal is placed. An inferomedial portal is also made under direct visualization.
Specific Steps (
Box 51-1
)
A diagnostic arthroscopy is performed first. Special focus is placed on evaluation of the entire articular surface of the patella, trochlear groove, medial and lateral femoral condyles, and tibial plateaus. The inferomedial portal is placed under direct visualization.
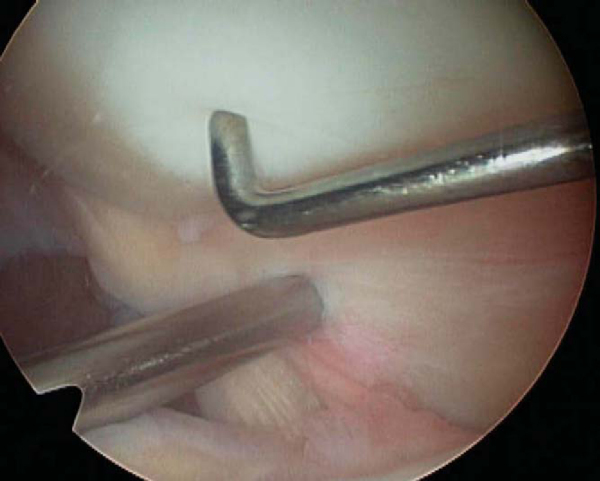
The chondral lesion is identified (
Fig. 51-2
), and the defect and its borders are carefully and systematically palpated with a blunt probe. This will expose loose flaps and any areas of delamination. It is also important to identify areas where the cartilage is softened (
Fig. 51-3
); but if the cartilage has an intact surface, it should not be débrided. Once loose flaps of cartilage are identified, a 4.5-mm aggressive shaver is placed, and the loose flaps and debris are mechanically removed until stable borders are obtained (Figs. 51-4 and 51-5 [4] [5]). A whisker-type shaver may also be used for less aggressive débridement. Care must be taken not to peel off the articular cartilage but only to remove the unstable borders. The posteromedial and posterolateral gutters are also visualized to evaluate for intraarticular loose bodies. The blunt arthroscopy obturator is placed through the notch into the posterolateral and posteromedial recess of the knee under direct visualization. Once it is in position, the camera is then placed into the obturator sleeve, and the posterolateral and posteromedial notch recesses are visualized.
|
|
|
|
Figure 51-2 |
|
|
|
|
Figure 51-3 |
|
|
|
|
Figure 51-4 |
It is helpful to document the size and location of the lesion in the operative report. On the patella, the description should include the facet on which the lesion is located as well as the flexion angle at which the lesion comes in contact with the trochlea. On the trochlea, describe whether the lesion is medial, lateral, or centrally located. If the lesion involves the medial or lateral femoral condyles, documentation of the flexion angle of the knee where the lesion becomes weight bearing is helpful for reference.
| PEARLS AND PITFALLS | ||||||||||||||||||||||||||||||
|
Sutures are removed in 7 to 10 days. Close attention is paid to obtaining postoperative range of motion. Also, postoperative effusions and any activity-related effusions are worrisome and should be addressed with repeat examination and possible MRI.
Patients are allowed to bear weight postoperatively as tolerated. Crutches are prescribed to assist with ambulation, and patients may be weaned from postoperative crutches when they no longer demonstrate a limp. Once the incisions are healed, pool therapy can also be of significant benefit.
Complications can include infection, continued pain, advancement to degenerative arthritis, and possible arthrofibrosis.
The results of treatment of chondral lesions with mechanical débridement are variable (
Table 51-1
). These are complex and often frustrating problems. Mechanical symptoms, such as catching and popping, are often alleviated with mechanical débridement. Hunt et al[12] believe that improved pain relief and longer duration of pain relief are achieved in patients who have acute onset of pain, mechanical symptoms, normal lower extremity alignment, and minimal degenerative changes on radiographic examination. Kruger et al[16] found that after an average followup of 40 months, patients with severe articular cartilage lesions who had undergone articular lavage alone showed significantly poorer results than did those treated with mechanical débridement.
| Author | Study Design | Technique | No. of Patients | Indications | Followup | Outcomes |
|---|---|---|---|---|---|---|
| Moseley et al[21] (2002) | Prospective, randomized, controlled trial | 3 groups (lavage, débridement, placebo) | 165 | Degenerative arthritis | 2 years | No difference between the 3 groups |
| Jackson et al[13] (1986) | Prospective, randomized | Lavage ± débridement | 202 total 65 lavage 137 lavage + débridement |
Degenerative arthritis | 3 years | Lavage: 45% improved Lavage + débridement: 68% improved |
| Livesley et al[19] (1991) | Prospective, controlled trial | Physiotherapy ± lavage | 61 total 37 physiotherapy+ lavage 24 physiotherapy alone |
Degenerative arthritis | 1 year | Better pain relief in lavage group, more effective in earlier stages of osteoarthritis |
| Aichroth et al[1] (1991) | Prospective review | Débridement | 254 | Degenerative arthritis | 44 months (mean) | 75% good–excellent 85% satisfied |
| Kruger et al[16] (2000) | Retrospective | Abrasion arthroplasty | 161 | Degenerative arthritis | 40 months (mean) | 29.2% improved 54.7% unchanged 16.1% worse |
| Rand[22] (1991) | Retrospective | Abrasion arthroplasty | 28 | Degenerative arthritis | 3.8 years (mean) | 39% good–excellent 29% fair 32% poor |
| Baumgaertner et al[2] (1990) | Retrospective | Abrasion arthroplasty | 46 (41 knees) | Degenerative arthritis | 33 months (mean) | 52% improved 39% no change 9% temporary improvement |
| Bert and Maschka[3] (1989) | Retrospective | Abrasion arthroplasty | 59 | Degenerative arthritis | 60 months (mean) | 51% good–excellent 16% fair 33% poor |
| Bert and Maschka[3] (1989) | Retrospective | Débridement | 67 | Degenerative arthritis | 60 months (mean) | 66% good–excellent 13% fair 21% poor |
| Johnson[14] (1986) | Retrospective | Abrasion arthroplasty | 104 | Degenerative arthritis | 2 year | 78% subjective improvement 15% no change 7% worse |
| Friedman et al[9] (1984) | Retrospective | Abrasion arthroplasty | 73 | Degenerative arthritis | >6 months (mean) | 60% good–excellent 34% fair 6% poor |