CHAPTER 27 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 27 – Proximal Biceps Tenodesis
Augustus D. Mazzocca, MD
Biceps tendinopathy rarely occurs in isolation. Rather, it is usually associated with a spectrum of concomitant shoulder disorders, including subacromial impingement, rotator cuff tears, biceps instability, and SLAP tears. A diligent work-up is essential for correct identification and treatment of these associated pathologic entities.
The role of the long head of the biceps tendon has been heavily debated in the literature. Electromyography literature and biomechanical cadaver studies provide evidence of a role as a secondary humeral head depressor [7] [18]; this function appears more pronounced in the unstable shoulder.[1] Others, however, argue that the long head of the biceps tendon is a vestigial structure.
Although there is no clear consensus on the surgical treatment of symptomatic, refractory, isolated biceps tendinopathy, it is generally agreed that débridement is indicated for partial tears affecting 30% to 50% of the tendon substance. [1] [3] [19] Advocates of tenotomy base their approach on the benign natural history and good functional outcomes of traumatic biceps ruptures. However, complications such as cosmetic (“Popeye”) deformity due to distal retraction of the muscle belly, supination weakness, and muscle spasm have led to the development of numerous tenodesis techniques.[5] Recent series have reported a 70% incidence of Popeye deformity and 38% incidence of elbow flexion fatigue with tenotomy alone.[13]
Arthroscopic biceps tenodesis techniques are plentiful in the literature (
Table 27-1
). Described techniques include proximal fixation with interference screws, suture anchors, and suturing to the conjoined tendon, rotator cuff, and even transverse humeral ligament. Interference screw tenodesis demonstrated failure loads before tendon migration that were three times higher than after tenotomy alone in a cadaver model.[21] Failure of proximal stabilization has been attributed to the retention of diseased, inflamed, pain-generating tendon and synovium within the fixed confines of the intertubercular groove.[15] Securing the biceps tendon distal to the intertubercular groove with a subpectoral tenodesis approach removes the diseased tendon entirely and restores the proper biceps length-tension relationship to ensure optimal bicipital function. Biceps tenodesis is therefore recommended over biceps tenotomy for three reasons:
Multiple biomechanical cadaver and animal studies have shown increased load to failure with biotenodesis techniques over suture anchor, keyhole, and tunnel techniques.[14] Our preferred surgical technique for the treatment of isolated biceps tendinopathy is an open subpectoral tenodesis with a biotenodesis screw, [10] [11] [17] which is discussed in this chapter.
| Author | Study | Results | |
|---|---|---|---|
| Richards and Burkhart[16] (2005) | Biomechanical cadaver study | 7-mm biotenodesis screw vs. 2 | 7-mm biointerference screw: 233.5 ± 55.5 N |
| Load to failure | Mitek GII anchors | 2 Mitek G2 anchors: 135.5 ± 37.8 N | |
| Wolf et al[21] (2005) | Biomechanical cadaver study | Tenodesis vs. tenotomy | Tenotomy: 110.7 N |
| Load to failure | Tenodesis: 310.8 N | ||
| Ozalay et al[14] (2005) | Biomechanical cadaver study | Tunnel vs. interference screw vs. suture anchor vs. keyhole | Tunnel: 229 ± 44.1 N |
| Interference screw: 243.3 ± 72.4 N | |||
| Load to failure | Suture anchor: 129.0 ± 16.6 N | ||
| Keyhole: 101.4 ± 27.9 N | |||
| Jayamoorthy et al[5] (2004) | Biomechanical sheep study | Keyhole vs. biointerference screw vs. metal interference screw | Keyhole: 303 N |
| Load to failure | 8-mm biointerference screw: 234 N | ||
| Metal interference screw: 201 N | |||
| Mazzocca et al[9] (2005) | Biomechanical cadaver study | Subpectoral bone tunnel (SBT) vs. arthroscopic suture anchor (SA) vs. subpectoral interference screw (SIS) vs. arthroscopic interference screw (AIS) | Cyclic gap formation: |
| Load to failure and cyclic gap formation | SBT: 9.39 ± 2.82 mm | ||
| AIS: 5.26 ± 2.60 mm | |||
| SIS: 1.53 ± 0.60 mm | |||
| SA: 3.87 ± 2.11 mm | |||
| No differences in load to failure | |||
| Osbahr et al[13] (2002) | Retrospective review | Tenodesis vs. tenotomy | No difference in cosmesis, pain, or spasm |
| Gill et al[4] (2001) | Case series | 30 biceps tenotomy, 19 months of followup | 90% return to sports |
| 96.7% return to work | |||
| 13.3% complication rate (Popeye sign) | |||
| Boileau et al[2] (2002) | Case series | Biceps tenodesis with interference screw fixation (8 or 9 mm) | 90% strength of normal side |
| No elbow motion loss | |||
| 2 initial failures (7-mm screw) | |||
| Nord et al[12] (2005) | Case series | Tenodesis with anchor through subclavian port | 11 patients, 2-year followup: 90% good–excellent results |
| Kelly et al[6] (2005) | Case series | Tenotomy | 68% good, very good, or excellent result |
| 70% Popeye sign | |||
| 38% fatigue with resisted elbow flexion |
A typical history includes the following:
| • | Pain in intertubercular groove that moves laterally with external rotation | |
| • | No pain with cross-arm adduction or acromioclavicular joint palpation | |
| • | Positive result of O’Brien, Speed, and Yergason tests | |
| • | Positive result of subpectoral biceps tenderness test[5]: pain with palpation of the biceps tendon under the inferior border of the pectoralis major tendon. With the arm in neutral rotation, resisted internal rotation tensions the pectoralis major tendon. The biceps tendon can be palpated just distal to the inferior border of the pectoralis major, pressing laterally. Specificity of the subpectoral biceps tenderness test can be improved if a glenohumeral lidocaine injection provides symptomatic relief. |
| • | Anteroposterior, scapular oblique, and axillary views | |
| • | Magnetic resonance arthrography, if indicated | |
| • | Ultrasonography, if available |
Indications and Contraindications
The decision to treat biceps disease surgically is predicated on a clinical presentation of bicipital groove pain, provocative test results, response to injection, and failed nonoperative management. Findings on arthroscopic examination may include biceps tendinosis occurring with or without concurrent rotator cuff disease, biceps tendinosis in association with superior labral anterior-posterior (SLAP) lesions, and tendinosis secondary to instability of the biceps tendon. Instability of the biceps tendon can occur with disruption of the lateral aspect of the superior glenohumeral ligament and coracohumeral ligament, as observed in association with anterior supraspinatus tendon tears, or with disruption of the medial aspect of the coracohumeral ligament, often seen with a subscapularis tear. Instability of the biceps tendon is generally treated with a biceps tenodesis because reconstruction of the coracohumeral ligament attachment on the humerus has generally not been satisfactory.
Absolute contraindications to biceps tenodesis include any medical condition that precludes the safe administration of anesthesia or renders the patient unstable for operative intervention.
The senior author prefers beach chair positioning with interscalene block plus general anesthesia; the regional block alone is insufficient to anesthetize the axillary incision adequately. A complete examination under anesthesia is performed on both upper extremities to examine for concurrent pathologic processes of the shoulder or elbow.
Surgical Landmarks, Incisions, and Portals
| • | Coracoid | |
| • | Acromion | |
| • | Clavicle | |
| • | Pectoralis major tendon |
| • | Posterior portal | |
| • | Anterior portal | |
| • | Axillary fold incision at inferior border of pectoralis major tendon |
| • | Axillary fold incision at inferior border of pectoralis major tendon: cephalic vein, musculocutaneous nerve (overzealous retraction), pectoralis major insertion (retraction) |
Examination Under Anesthesia and Diagnostic Arthroscopy
Examination under anesthesia is performed to ensure full range of motion and glenohumeral stability.
Diagnostic arthroscopy evaluates the intraarticular biceps tendon, rotator cuff, glenoid labrum, glenohumeral ligaments, and chondral surface.
Specific Steps (
Box 27-1
)
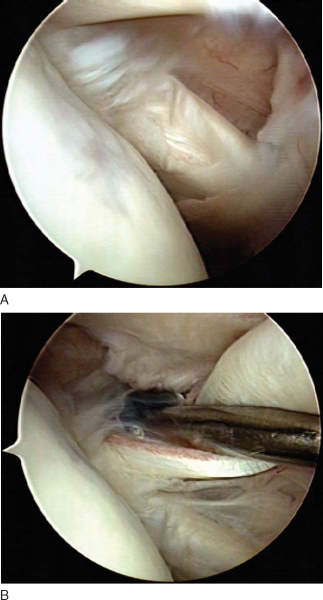
Glenohumeral arthroscopy is begun with a standard posterior viewing portal (
Fig. 27-1
). A dry inspection of the intraarticular biceps tendon is performed initially because the pump pressure will result in vascular compression, causing the tenosynovitis to be “washed out.” Injection or tendon fraying is indicative of bicipital disease. It is unknown how much biceps fraying can be accepted without the need for intervention, but some authors have proposed up to 30% to 50%. Additional inspection of the more distal tendon portions is accomplished by pulling the biceps tendon into the glenohumeral joint with a probe.
| Surgical Steps | |||||||||||||||||||||
|
|
|
|
|
Figure 27-1 |
A basket forceps is inserted through the anterior cannulated portal to transect the biceps tendon at the superior labral junction (
Fig. 27-2
). Care is taken to avoid inadvertent damage to the superior glenoid labrum.
|
|
|
|
Figure 27-2 |
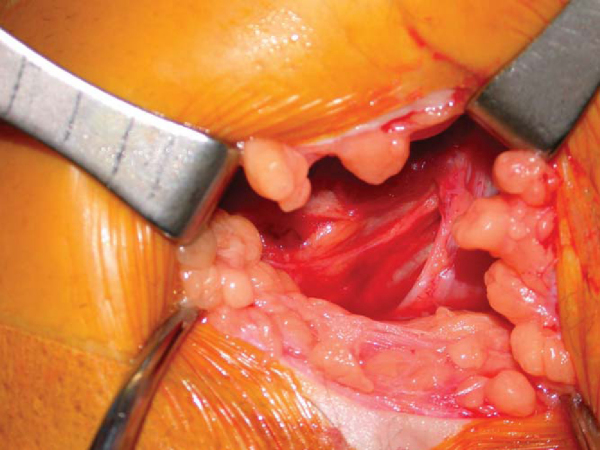
With the arm slightly abducted and externally rotated, the inferior border of the pectoralis major tendon is palpated. A 3- to 4-cm incision is performed in line with the axillary fold, with one quarter of the incision above and three quarters of the incision below the inferior border of the pectoralis major tendon. A No. 15 blade scalpel is used to incise the subcuticular tissues. After hemostasis has been achieved with the electrocautery, Gelpi or Weitlaner self-retaining retractors are inserted to improve exposure. The overlying fatty tissue is cleared until the fascia overlying the pectoralis major, coracobrachialis, and biceps is identified (
Fig. 27-3
). Once the inferior border of the pectoralis major has been identified, the fascia overlying the coracobrachialis and biceps is incised in line with the incision. If these anatomic landmarks are not easily identified, the dissection is probably too lateral, especially if the cephalic vein is seen in the deltopectoral groove, in which case the dissection is also too proximal.
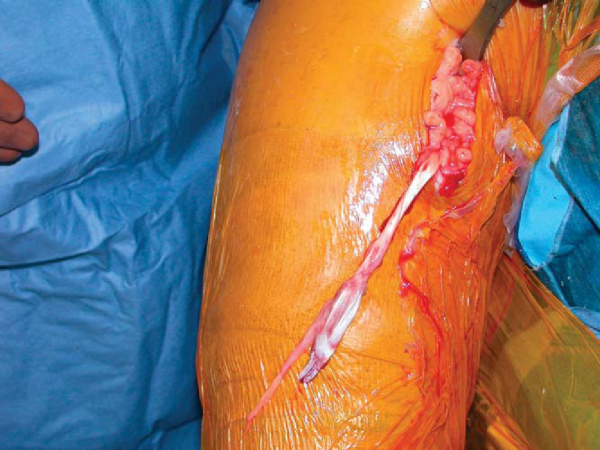
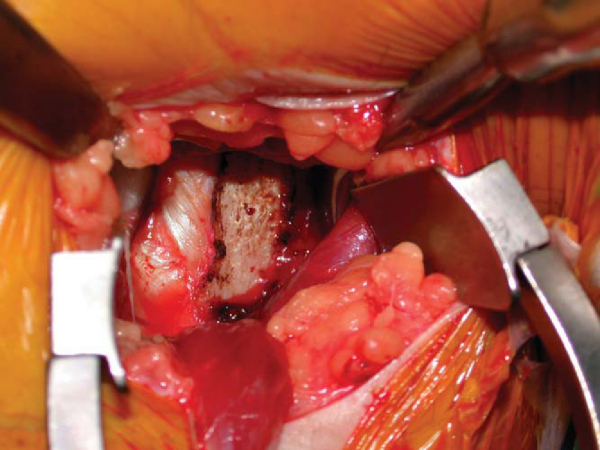
Blunt dissection with Mayo scissors and finger dissection sweep posterior to the pectoralis major tendon. The biceps tendon can be palpated in the intertubercular groove behind the pectoralis major tendon. A pointed curved Hohman retractor is placed on the lateral humeral cortex to retract the pectoralis tendon insertion superior and lateral. A blunt Chandler retractor is positioned on the medial cortex to retract the coracobrachialis and short head of the biceps. Vigorous medial retraction should be avoided to prevent injury to the musculocutaneous nerve. The long head of the biceps musculotendinous junction should be visualized. A right-angled clamp is then used to bluntly open the biceps sheath and deliver the tendon into the wound (
Fig. 27-4
).
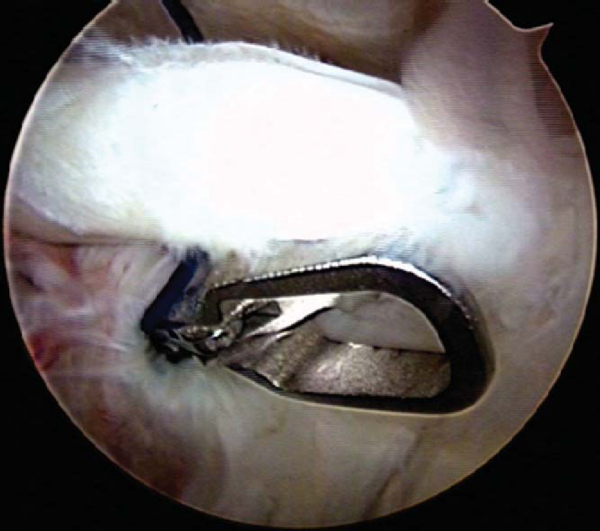
A No. 2 FiberWire (Arthrex, Inc., Naples, Fla) is used to sew a modified Krakow stitch starting 2.5 cm proximal to the musculotendinous junction (
Fig. 27-5
). The remaining tendon is removed sharply with a No. 15 blade scalpel. The two ends of FiberWire exiting the biceps tendon are tied together with a square knot.
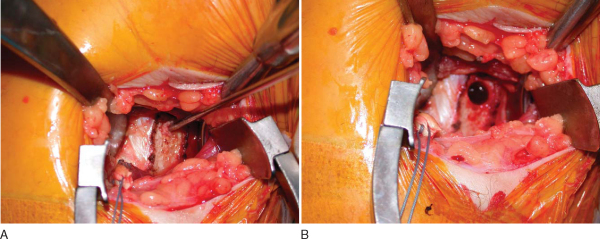
The periosteum 1 cm proximal to the pectoralis major tendon is reflected sharply off the humerus, forming a rectangle measuring approximately 2 × 1 cm (
Fig. 27-6
). A 2.4-mm threaded guide pin is drilled up to but not penetrating the far cortex. The starting point is just proximal to the inferior edge of the pectoralis major tendon and situated in the intertubercular groove, centered in the medial to lateral direction on the humerus (
Fig. 27-7A
). Subsequently, an 8-mm reamer is used to overream the guide pin without violating the posterior cortex. The reamer is then carefully backed out by hand to avoid tunnel widening on exiting (
Fig. 27-7B
). A headlight may be used to assist with illumination. An Arthrex 8- × 12-mm biotenodesis screw is loaded on the tip of the cannulated tenodesis screwdriver. A nitinol loop retrieves a strand of FiberWire through the cannulated screwdriver. The retrieved FiberWire tensions the biceps tendon to the screwdriver tip, and a needle driver secures the FiberWire tightly against the handle of the screwdriver.
|
|
|
|
Figure 27-7 |
The biceps tendon is pushed into the humeral tunnel and secured in place by the advancing biotenodesis screw until the screw head is countersunk. The tunnel may be tapped before screw insertion if dense cortical bone is encountered. After screw insertion, the biceps tendon should be draped over and covering the tenodesis screw. A right-angled clamp can be used to elevate the biceps tendon to ensure complete seating of the screw.
After copious irrigation, 3-0 Monocryl buried sutures close the deep subcutaneous tissue. Steri-Strips are applied to the skin. The wound is injected with 5 mL of 0.25% bupivacaine (Marcaine).
Sutures are removed on the seventh postoperative day. The three-view radiographic examination is repeated to assess tunnel placement.
Postoperative management is dictated by concomitant procedures.
| • | Passive range of motion first 6 weeks, then progression from active-assisted to active range of motion | |
| • | Immediate elbow range of motion and grip strengthening |
| • | Passive range of motion with rapid progression to active-assisted and active range of motion | |
| • | Immediate elbow range of motion and grip strengthening | |
| • | Follow isolated biceps tenodesis protocol |
Our experience includes 20 patients with more than 2 years of followup. The preoperative to postoperative scores averaged the following increases: Rowe score, 57 to 91; American Shoulder and Elbow Surgeons score, 42 to 86; Simple Shoulder Test score, 5 of 12 to 10 of 12; Constant-Murley score, 45 of 75 to 67 of 75.
1.
Barber FA, Byrd JW, Wolf EM, Burkhart SS: How would you treat the partially torn biceps tendon?.
Arthroscopy 2001; 17:636-639.
2.
Boileau P, Krishnan SG, Coste JS, Walch G: Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw.
Arthroscopy 2002; 18:1002-1012.
3.
Eakin CL, Faber KJ, Hawkins RJ, Hovis WD: Biceps tendon disorders in athletes.
J Am Acad Orthop Surg 1999; 7:300-310.
4.
Gill TJ, McIrvin E, Mair S, Hawkins RJ: Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii.
J Shoulder Elbow Surg 2001; 10:247-249.
5.
Jayamoorthy T, Field JR, Costi JR, et al: Biceps tenodesis: a biomechanical study of fixation methods.
J Shoulder Elbow Surg 2004; 3:160-164.
6.
Kelly AM, Drakos MC, Fealy S, et al: Arthroscopic release of the long head of the biceps tendon.
Am J Sports Med 2005; 33:208-213.
7.
Kilicoglu O, Koyuncu O, Demirhan M, et al: Time-dependent changes in failure loads of 3 biceps tenodesis techniques.
Am J Sports Med 2005; 33:1536-1544.
8.
Kim SH, Ha KI, Kim HS, Kim SW: Electromyographic activity of the biceps branchii muscle in shoulders with anterior instability.
Arthroscopy 2001; 17:864-868.
9.
Mazzocca AD, Bicos J, Santangelo S, et al: The biomechanical evaluation of four fixation techniques for proximal biceps tenodesis.
Arthroscopy 2005; 21:1296-1306.
10.
Mazzocca AD, Rios CG, Romeo AA, Arciero RA: Subpectoral biceps tenodesis with interference screw fixation.
Arthroscopy 2005; 21:896.
11.
Mazzocca AD, Romeo AA: Arthroscopic biceps tenodesis in the beach chair position.
Oper Tech Sports Med 2003; 11:6-14.
12.
Nord KD, Smith GB, Mauck BM: Arthroscopic biceps tenodesis using suture anchors through the subclavian port.
Arthroscopy 2005; 21:248-252.
13.
Osbahr DC, Diamond AB, Speer KP: The cosmetic appearance of the biceps muscle after long-head tenotomy versus tenodesis.
Arthroscopy 2002; 18:483-487.
14.
Ozalay M, Akpinar S, Karaeminogullari O, et al: Mechanical strength of four biceps tenodesis techniques.
Arthroscopy 2005; 21:992-998.
15.
Pfahler M, Branner S, Refior HJ: The role of the bicipital groove in tendopathy of the long biceps tendon.
J Shoulder Elbow Surg 1999; 8:419.414
16.
Richards DP, Burkhart SS: A biomechanical analysis of two biceps tenodesis fixation techniques.
Arthroscopy 2005; 21:861-866.
17.
Romeo A, Mazzocca AD, Tauro JC: Arthroscopic biceps tenodesis.
Arthroscopy 2004; 20:206-213.
18.
Sakurai G, Ozaki J, Tomita Y, et al: Electromyographic analysis of shoulder joint function of biceps brachii muscle during isometric contraction.
Clin Orthop 1998; 354:123-131.
19.
Sethi N, Wright R, Yamaguchi K: Disorders of the long head of the biceps tendon.
J Shoulder Elbow Surg 1999; 8:644-654.
20.
Verma NN, Drakos M, O’Brien SJ: Arthroscopic transfer of the long head biceps to the conjoint tendon.
Arthroscopy 2005; 21:764.
21.
Wolf RS, Zheng N, Weichel D: Long head biceps tenotomy versus tenodesis: a cadaveric biomechanical analysis.
Arthroscopy 2005; 21:182-185.