CHAPTER 21 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 21 – Tendon Transfers for Rotator Cuff Insufficiency
Scott D. Pennington, MD,
Thomas F. Holovacs, MD,
Jon J.P. Warner, MD
Direct primary repair achieves reliable pain relief and functional improvement in the majority of rotator cuff tears. [13] [22] [49] However, less commonly, very large musculotendinous defects, static superior subluxation of the humeral head, chronicity, and poor bone or tendon tissue quality may preclude successful primary repair. [3] [4] [16] [20] [22] In such cases, alternative reconstructive surgical techniques should be considered. Historically, the management of irreparable massive rotator cuff tears had encompassed a wide range of surgical procedures, including open or arthroscopic débridement, muscle or tendon transposition (upper subscapularis, teres minor, teres major, latissimus dorsi, pectoralis major, trapezius, deltoid, biceps, and triceps), tendon allografts, synthetic graft material, xenograft, and arthroplasty. [1] [2] [5] [8] [12] [36] [37] [38]
Although débridement may allow pain relief in the low-demand patient, [42] [43] function is not reliably restored. [6] [22] Bridging of tendinous gaps with allografts and xenografts has not gained widespread acceptance because of variable functional results and inability to re-establish the length-tension relationship of the rotator cuff.[11] If the coracoacromial arch is intact, hemiarthroplasty may offer some relief in the setting of rotator cuff arthropathy, [26] [30] but this treatment rarely addresses functional limitations.[25] Recently, reverse total shoulder arthroplasty has offered a promising solution for pain relief and concomitant functional improvement in older patients with irreparable tears; however, long-term data on the longevity of these prostheses are not available in the United States. Furthermore, a reverse prosthesis alone will not restore an external rotation deficit, which can be a persistent source of disability. For younger, high-demand patients, local or regional muscle and tendon transfers are viable treatment options that provide a vascularized, functional replacement of the affected musculotendinous unit when other repair methods are likely to fail.
When a musculotendinous unit has become torn and retracted from its insertion, the constituent muscle fibers undergo atrophy secondary to disuse. Concomitantly, fatty infiltration of the muscle interstitium results from macroarchitectural changes in the muscle fiber pennation angle.[32] Once these changes have occurred, the muscle may not generate the strength and excursion necessary for normal function, even after successful primary repair. [13] [18] [16] [22] [32] Even if excursion is sufficient to allow primary repair, fatty infiltration appears to be an irreversible event that may permanently compromise mechanical integrity of the musculotendinous unit.
Several donor muscles about the shoulder girdle have been shown to possess a suitable vector of pull, with adequate strength and amplitude to act as a surrogate rotator cuff tendon. [7] [9] [19] [24] [27] [28] [31] [44] [51] Empirically derived functional tendon transfers, of proven efficacy in foot and hand surgery, have been used to restore shoulder function after obstetric palsy in children. [10] [27] The analogous situation in the adult can result from brachial plexopathy and iatrogenic, inherited, or degenerative injury to the neuromusculotendinous unit of the rotator cuff. Advancement or transposition of local and regional muscles has been described to treat commonly occurring massive degenerative rotator cuff tears. [8] [16] [37] The two patterns of massive, irreparable rotator cuff tears are posterior superior and anterior superior configurations. Posterior superior rotator cuff tears are the most common type and involve the supraspinatus and infraspinatus (and occasionally the teres minor) tendons. Anterior superior rotator cuff tears involve the supraspinatus and the subscapularis. In this chapter, we review two reliable regional tendon transfers for treatment of the most commonly occurring deficits in the rotator cuff: the irreparable, massive posterior superior rotator cuff tear and the irreparable subscapularis tear (
Table 21-1
).
| Deficit | Transfer Option |
|---|---|
| Infraspinatus (posteroinferior cuff) | Latissimus ± teres major |
| Teres alone | |
| Supraspinatus | Subscapularis |
| Teres minor | |
| Anterior deltoid | |
| Subscapularis (anterosuperior cuff) | Pectoralis major (split, clavicular head or sternal head) |
| Teres major | |
| Serratus anterior | Pectoralis major (split, sternal head) |
| Trapezius | Rhomboid, levator advancement (Eden-Lange) |
Latissimus Dorsi Transfer for Posterior Superior Rotator Cuff Tears
The latissimus dorsi transfer is primarily indicated for patients with unacceptable pain and functional deficits caused by a chronic, irreparable, massive tear of the posterosuperior rotator cuff. Because there is no strict preoperative definition of an irreparable tear, the clinician must use a constellation of findings on the history, physical examination, and radiographic work-up to ascertain the feasibility of primary rotator cuff repair. Size of the tear, chronicity, and tendon and bone quality are preoperative risk factors that may mitigate the success of primary cuff repair.
| • | Atrophy of the spinati may be noted, indicating a chronic, massive tear. | |
| • | Active forward flexion and external rotation are limited compared with the contralateral side. Motor testing of the supraspinatus and infraspinatus demonstrates weakness. | |
| • | Passive motion should be well maintained in the tendon transfer candidate. | |
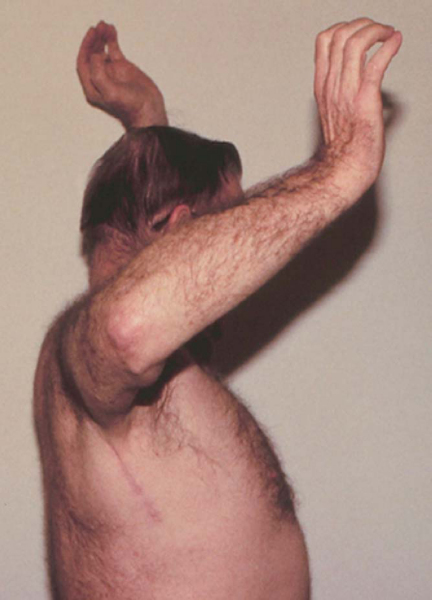
| • | External rotation lag (a difference in passive and active external rotation arc) is indicative of a massive posterior cuff tear. An external rotation lag sign that persists in abduction, termed the signe du clarion (hornblower sign), indicates extension of the tear into the teres minor[23] ( Fig. 21-1 ). |
|
| • | Subscapularis function is intact (Gerber liftoff test). | |
| • | It may be advantageous to perform an impingement test with a lidocaine injection into the subacromial space to test rotator cuff strength if the examination is limited by pain. |
| • | True anteroposterior, scapular Y, and axillary lateral views of the shoulder | |
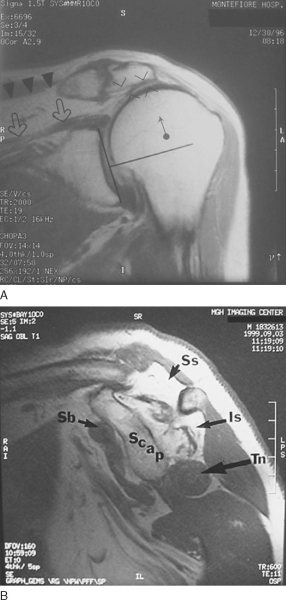
| • | Plain films may demonstrate static superior subluxation of the humeral head. An acromiohumeral distance of less than 7 mm (normal, 10.5 mm) suggests an irreparable tear of the infraspinatus ( Fig. 21-2A ). |
|
| • | Magnetic resonance imaging is performed to characterize the status of the rotator cuff tendons and to evaluate muscle atrophy and fatty infiltration. | |
| • | A massive tear, defined as a tear encompassing two or more tendons, with grade 3 or 4 fatty infiltration of the rotator cuff musculature on magnetic resonance imaging or computed tomography, portends a poor prognosis for a successful primary repair and as such is an indication for tendon transfer ( Fig. 21-2B ).[20] |
|
|
|
|
Figure 21-2 (B from Warner JJP. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instr Course Lect 2001;50:63-71.) |
Not all patients with massive, irreparable rotator cuff tears require surgery. Some patients with massive cuff tears experience minimal pain and maintain good overall shoulder function. Reconstructive efforts in such patients are unnecessary.
Patients with massive, irreparable rotator cuff tears often demonstrate pseudoparalysis, or the inability to initiate abduction. This finding is a contraindication to latissimus dorsi tendon transfer. Isolated loss of forward elevation alone is not reliably restored by this technique. In addition, patients with anterosuperior rotator cuff tears involving the subscapularis, such that the liftoff test result is positive, are not good candidates for latissimus transfer.
Prior failed attempts at primary rotator cuff repair are not necessarily contraindications to a latissimus transfer, but more limited gains in satisfaction and function should be expected.[48] Other relative contraindications include deltoid dysfunction, shoulder stiffness, severe rotator cuff tear arthropathy, and infection.
The patient is assessed by the anesthesiologist preoperatively for the use of an interscalene block and catheter. However, because the interscalene block does not extend to the axilla, general anesthesia is necessary. We have had experience in positioning one of two ways—beach chair or lateral decubitus.
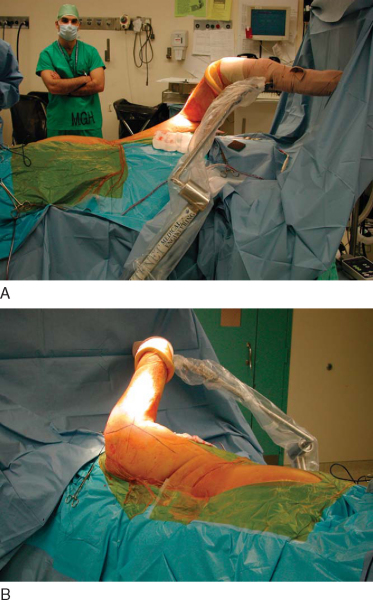
If the beach chair position is selected, the patient is placed onto a custom beach chair device with retractable kidney rests, providing maximal exposure (T-Max Shoulder Positioner; Tenet Medical Engineering, Calgary, Canada). The beach chair position is relatively contraindicated in obese patients because of difficulty with surgical field exposure in the axilla. After induction, the patient is placed as far laterally on the table as possible to facilitate positioning of the surgeon during exposure. A first-generation cephalosporin is administered for prophylaxis. The operative limb and hemi-torso are prepared and draped in the usual sterile fashion and then secured by means of a sterile pneumatic arm holder (Spider Limb Positioner; Tenet Medical Engineering, Calgary, Canada). In this position, the surgeon may easily approach the superior shoulder and the axilla without the need of an assistant to hold the extremity (
Fig. 21-3
).
Alternatively, the lateral decubitus position may be used. After induction, the patient is placed into the lateral decubitus position on the far lateral side of a standard operating table. A full-length beanbag supports the patient’s body, with an axillary roll in place on the contralateral side. The Tenet arm holder is positioned at the midportion of the bed on the ventral side of the patient. Preparation and draping proceed in the standard fashion, with care taken to provide adequate exposure superiorly and posteriorly (
Fig. 21-4
).
Surgical Landmarks and Incisions
| • | Anterosuperior exposure: acromion, acromioclavicular joint, clavicle, and coracoid process. The incision is placed in relation to these landmarks parallel to Langer’s lines over the lateral third of the acromion, beginning at the posterior edge of the acromion and extending anteriorly 1 cm lateral to the coracoid process. | |
| • | Posteroinferior exposure: anterior border of the latissimus, triceps muscle belly, posterior deltoid. The posteroinferior incision of the latissimus dorsi is drawn parallel to the anterior border of the latissimus approximately 6 to 8 cm distal to the axillary fold. Proximally, the incision is curved superiorly parallel to the posterior axillary line to allow access to the posterior aspect of the deltoid ( Fig. 21-5 ). |
| • | Latissimus transfer: axillary nerve, radial nerve, brachial artery, thoracodorsal neurovascular pedicle |
Specific Steps (
Box 21-1
)
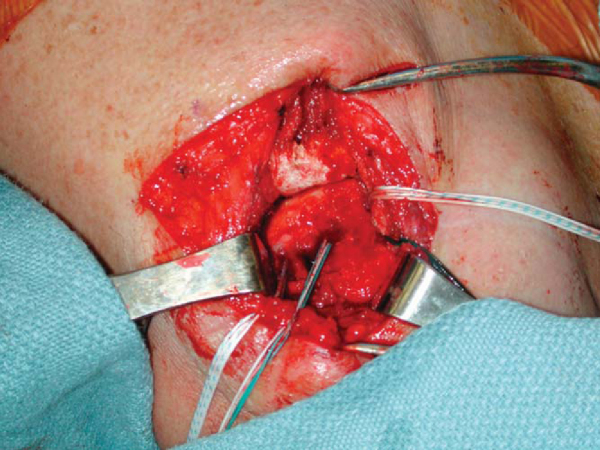
1. Superior Exposure, Cuff Assessment, and Mobilization
We approach the rotator cuff first during the procedure to allow assessment of cuff tissue and placement of anchors before harvesting of the latissimus. A No. 10 scalpel is used to incise skin and subcutaneous tissue to the level of the deltoid fascia. Sharp dissection with the scalpel is used to develop skin flaps at this level adequate to allow visualization of the lateral acromion and interval between the anterior and middle deltoid. Electrocautery is used to secure hemostasis, and self-retaining retractors are placed.
Next, the electrocautery is used to split the deltoid in line with its fibers for a distance of 4 to 5 cm between the anterior and middle heads of the deltoid. The anterior deltoid may be reflected subperiosteally off the acromion by means of the electrocautery to provide visualization of the rotator cuff, if necessary. The interval between the anterior deltoid and coracoacromial arch is identified, and the coracoacromial ligament attachment to the acromion is preserved. The subacromial bursa is excised. Placement of Army-Navy retractors or a self-retaining subacromial spreader may be useful for exposure of the rotator cuff. The torn edges of the rotator cuff are then tagged with No. 3 Ethibond, and a systematic release of the rotator cuff is performed. A No. 15 scalpel is employed to release the coracohumeral ligament, extra-articular subacromial adhesions, and the superior capsule of the glenohumeral joint just deep to the rotator cuff. Care is taken not to release more than 1.8 cm medial to the glenoid to avoid iatrogenic injury to the suprascapular nerve. If the biceps tendon is present, it is released from the supraglenoid tubercle and tenodesed in the biceps groove. Once releases have been performed, the compliance and excursion of the cuff are assessed for the possibility of primary repair (
Fig. 21-6
).
2. Greater Tuberosity Preparation (with Anchor Placement)
If primary repair is deemed to be not feasible, the rotator cuff tendon edges are freshened with a scalpel and the greater tuberosity is prepared with a rongeur on its anterolateral surface. The footprint must be placed laterally enough to allow creation of an external rotation moment for the transferred tendon. Suture anchors are then placed to allow multiple fixation points and to re-establish the rotator cuff footprint, depending on the tear pattern. A moistened saline gauze is then packed into the wound, and attention is turned to the posteroinferior exposure (
Fig. 21-7
).
|
|
|
|
Figure 21-7 |
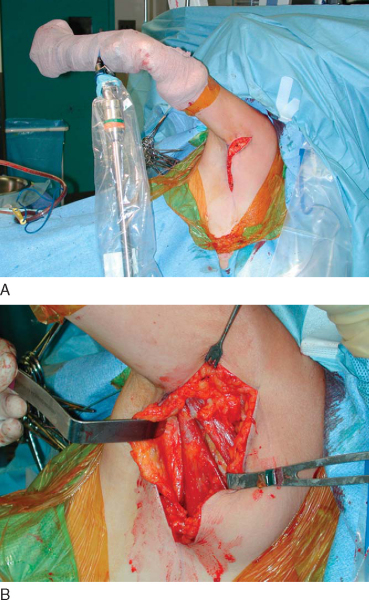
3. Posteroinferior Exposure and Mobilization of the Latissimus Tendon
With the arm holder in a position of abduction and maximal internal rotation, attention is turned to the posteroinferior incision. The skin is incised with a No. 10 scalpel, and skin flaps are developed above the level of the superficial fascia (
Fig. 21-8A
). By sharp dissection, the anterior border of the latissimus is defined. Posteriorly, the teres major, long head of the triceps, and posterior deltoid are identified. Careful dissection anteriorly will identify the neurovascular pedicle of the latissimus approximately 10 cm from the musculotendinous junction. If the muscle portion of the teres major is distinct from the latissimus posteriorly, this interval may be developed distally to further isolate the latissimus. However, the bellies of these two muscles are often confluent. In this case, dissection is carried superiorly just off the anterior border of the latissimus to its insertion, which is identified by the long, flat tendon insertion on the anterior humerus. Exposure is facilitated by maximal internal rotation and abduction of the brachium. Once the insertion has been identified, the tendon is released under direct vision with a No. 15 scalpel, with care taken to avoid the radial and axillary nerves, which are close. The rest of the muscle belly may then be liberated of any adhesions to the chest wall in a retrograde fashion (
Fig. 21-8B
).
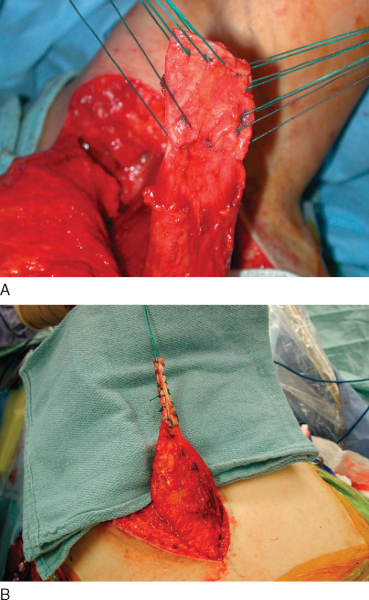
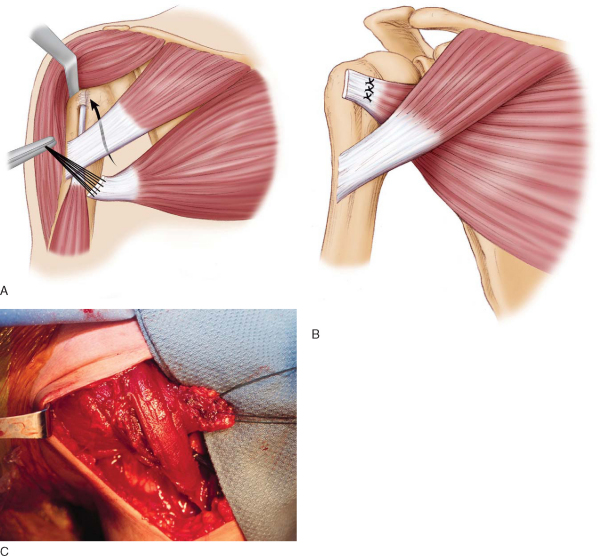
After the latissimus has been identified and mobilized, a running locking stitch of No. 3 Ethibond is placed in the tendon, and final releases are performed distally (
Fig. 21-9A
). Adequate excursion of the tendon may be tested by the ability to elevate the tendon superior to the level of the acromion (
Fig. 21-10A
). If this maneuver cannot be performed, further dissection of the thoracodorsal neurovascular pedicle may be performed as necessary, remembering that the average length of the pedicle is 8.4 cm. Alternatively, consideration may be given to augmentation of the graft with autogenous tissue (i.e., hamstring tendons) or soft tissue allografts to gain more length (
Fig. 21-9B
).
|
|
|
|
Figure 21-9 |
|
|
|
|
Figure 21-10 (B redrawn from Warner JJP. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instr Course Lect 2001;50:63-71.) |
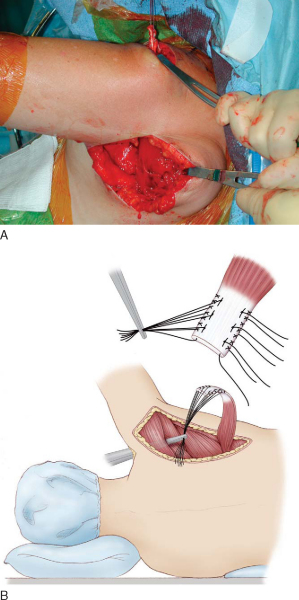
Once it has been determined that the tendon has enough length and excursion to reach the insertion site on the greater tuberosity, a subdeltoid tunnel is developed by a curved clamp inserted proximal to distal from the anterosuperior exposure to the posteroinferior exposure. The plane between the deltoid and teres minor is bluntly dissected, and the previously placed tagging sutures are drawn proximally through the soft tissue tunnel in an anterograde fashion. The axillary nerve is lateral to the passage of the tendon. Adequate excursion within the tunnel is confirmed by placing the tendon on the intended insertion site (
Fig. 21-10B
).
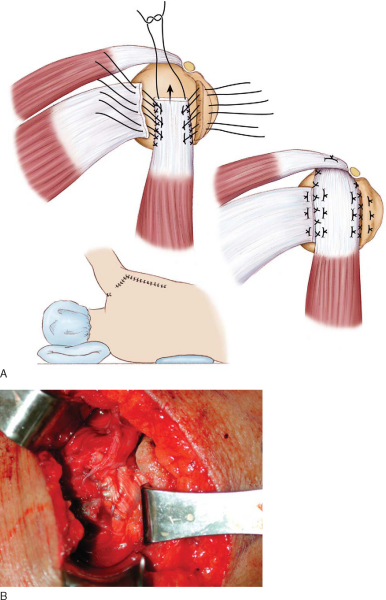
Tendon fixation is performed to the insertion site with the arm in 45 degrees of abduction and 30 degrees of external rotation by means of horizontal mattress sutures from the suture anchors. Frequently, slight external rotation may be needed to secure the tendon without too much tension. If the mobilized remnant of the rotator cuff will reach the insertion site, it may be incorporated into the fixation of the latissimus tendon or secured with No. 5 FiberWire sutures in a Mason-Allen configuration through bone tunnels to the greater tuberosity (
Fig. 21-11
).
|
|
|
|
Figure 21-11 (A [redrawn] and B from Higgins LD, Warner JJP. Massive tears of the posterosuperior rotator cuff. In Warner JJP, Iannotti JP, Flatow EL, eds. Complex and Revision Problems in Shoulder Surgery, 2nd ed. Philadelphia, Lippincott Williams & Wilkins, 2005:129-160.) |
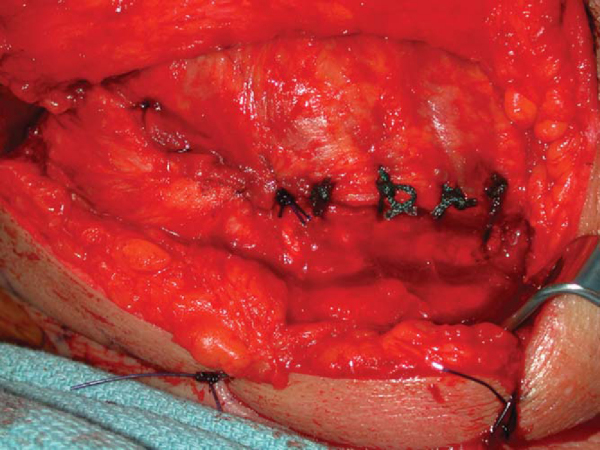
The deltoid is then repaired to the acromion through bone tunnels with No. 5 FiberWire (
Fig. 21-12
). All wounds are closed with 2-0 Vicryl sutures, followed by 3-0 Monocryl. Drains may be left in the wounds if it is deemed necessary. Before the patient is extubated, the SOBER brace (Laboratoire SOBER, Crolles, France) is fashioned to the patient in a position of 45 degrees of abduction and 45 degrees of external rotation (
Fig. 21-13
).
|
|
|
|
Figure 21-13 (From Higgins LD, Warner JJP. Massive tears of the posterosuperior rotator cuff. In Warner JJP, Iannotti JP, Flatow EL, eds. Complex and Revision Problems in Shoulder Surgery, 2nd ed. Philadelphia, Lippincott Williams & Wilkins, 2005:129-160.) |
The postoperative protocol is designed to protect tendon healing to bone while maintaining adequate excursion of the tendon through the submuscular tunnel and preventing glenohumeral stiffness and postsurgical adhesions. The patient is instructed to wear the SOBER brace continuously in abduction and external rotation for 6 weeks. During this time, passive abduction with external rotation above the plane of the brace (greater than 45 degrees) is instituted with physical therapy. Internal rotation and adduction are not permitted. At 6 weeks, the brace is removed, and gentle activities of daily living are allowed with gentle mobilization of the extremity in physical therapy.
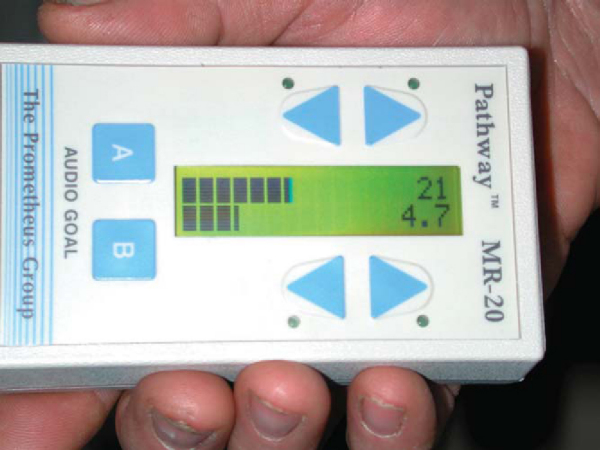
At the 3-month mark, active strengthening of the rotator cuff and tendon transfer is allowed. The normal vector of the latissimus is one of adduction, internal rotation, and extension. However, in its new position, the transfer must act out of phase as an external rotator. Therefore, muscle re-education is performed with the aid of a biofeedback device (
Fig. 21-14
). An electrode is placed on the latissimus, which senses contraction and provides auditory and visual feedback to the patient. With the shoulder positioned in the midrange of abduction, the patient is instructed to adduct the arm, causing contraction of the latissimus. The therapist then assists the arm into forward flexion and external rotation during this maneuver, making a J shape in space. With time, the patient learns how to contract the latissimus to execute abduction and external rotation. Full retraining of the muscle may take up to 12 months.
|
|
|
|
Figure 21-14 |
Complications of latissimus dorsi transfer include infection, scar tenderness (contraction of the axillary scar if it crosses perpendicular to the axilla), and pseudoparesis of the shoulder. As with any rotator cuff surgery, deltoid injury and axillary nerve injury may occur as well. Late failure of the transfer has been variably reported, but if this is an intraoperative concern, the tendon may be augmented with autogenous fascia lata.[48]
Results of the latissimus dorsi transfer have been reported by Gerber,[15] Aoki et al,[2] Miniaci and MacLeod,[35] Warner and Parsons,[49] and Habermeyer et al.[21] Good to excellent subjective results have been demonstrated in 13 of 16 patients[15] and 8 of 12 patients.[2] In Gerber’s series, pain relief at rest was satisfactory in 94% of patients, and pain with exertion was 75% at 65 months postoperatively. Functionally, average improvement has ranged from 36 to 53 degrees in flexion and 14 degrees in external rotation. Habermeyer found an increased Constant score from 46 to 76 at 32 months postoperatively with a single-incision technique.
More recent midterm results (53 months) by Gerber[17] have shown that patients maintained improvements in pain and function (subjective shoulder value increase from 28% to 66%; age- and gender-matched Constant score increase from 55 to 73).
Results in the setting of a failed prior attempt at rotator cuff repair have been less predictable. Warner and Parsons found that only 8 of 16 patients had adequate pain relief in the setting of a revision surgery, with an average gain in flexion of 44 degrees. In contrast, a satisfactory outcome was obtained in five of six patients who had the transfer as a primary procedure. Negative prognostic factors in the setting of a revision included prior deltoid injury, stiffness, and poor tendon quality of the remaining rotator cuff.
Irreparable rotator cuff tears continue to be a challenging problem for the reconstructive shoulder surgeon. For the appropriately chosen patient, latissimus dorsi transfer has been shown to provide reliable pain relief and improved function. Further study is necessary to delineate the future role of tendon transfers in the setting of prior arthroplasty or revision surgery, especially when patients have continued weakness of the external rotators (
Table 21-2
).
| Author | No. of Patients | Followup | Outcomes |
|---|---|---|---|
| Aoki et al[2] (1996) | 12 | 35 months | 66% good–excellent UCLA score |
| Forward flexion improved 36 degrees | |||
| Miniaci and MacLeod[35] (1999) | 17 revision | 51 months | 82% satisfactory UCLA score |
| Forward flexion improved 59 degrees | |||
| External rotation improved 12 degrees | |||
| Warner and Parsons[49] (2001) | 16 revision | 29 months | Postoperative score of 70% |
| Forward flexion improved 60 degrees | |||
| External rotation improved 37 degrees | |||
| 6 primary | 25 months | Postoperative score of 55% | |
| Forward flexion improved 43 degrees | |||
| External rotation improved 29 degrees | |||
| Gerber et al[19] (1988) | 4 | 14 months | 75% good–excellent results |
| Forward flexion improved 88 degrees | |||
| Abduction improved 75 degrees | |||
| External rotation improved 23 degrees | |||
| Gerber[15] (1992) | 16 | 33 months | Postoperative normal age-adjusted Constant score of 73 |
| Adequate pain relief in 94% of patients | |||
| Forward flexion improved 52 degrees | |||
| External rotation improved 13 degrees | |||
| Gerber et al[17] (2006) | 69 | 53 months | Subjective shoulder value improved from 28% to 66% |
| Age- and gender-matched Constant score improved from 55 to 73 | |||
| Pain improved from 6 to 12 (of a possible 15 points) | |||
| Forward flexion improved 19 degrees | |||
| External rotation improved 7 degrees | |||
| Habermeyer et al[21] (2006) | 14 | 32 months | Constant score improved from 46 to 74 |
| Forward flexion improved 51 degrees | |||
| External rotation improved 14 degrees |
Pectoralis Major Transfer for Subscapularis Insufficiency
The pectoralis major transfer is primarily indicated for patients with unacceptable pain and functional deficits caused by a chronic, irreparable tear of the subscapularis. Pectoralis major transfer to the lesser tuberosity has proved to be a useful salvage procedure for subscapularis insufficiency when its primary repair is precluded by subscapularis muscle atrophy, fatty infiltration, or poor tendon quality. Multiple techniques have been described for this transfer, including transfer of one or both heads of the tendon superficial or deep to the conjoined tendon to insert on the lesser tuberosity. [12] [41] [50] Our preferred method, transfer of the sternal head of the pectoralis superficial to the conjoined tendon, is described here.[46]
| • | Insidious onset of shoulder pain and loss of function | |
| • | Remote traumatic injury (external rotation) | |
| • | Prior surgical injury to the subscapularis |
| • | Positive liftoff test result, positive belly press test result | |
| • | Internal rotation weakness | |
| • | Increased passive external rotation compared with the contralateral side |
Routine studies are as described for the latissimus dorsi transfer. Pertinent positive findings are the following:
| • | Static anterior subluxation on an axillary plain film or complete anterosuperior escape of the humeral head on a true anteroposterior view may indicate subscapularis insufficiency. | |
| • | Greater than grade 2 fatty infiltration of subscapularis on computed tomography or magnetic resonance imaging |
Primary subscapularis tendon repair is preferable, if possible. If the subscapularis insufficiency is a component of a massive irreparable anterosuperior rotator cuff tear, the patient may be best served by a reverse shoulder prosthesis if he or she meets the criteria for that salvage procedure. Combined latissimus and pectoralis major tendon transfers have not yielded satisfactory results in our experience.[1] Concurrent infection, stiffness, and medical comorbidities may preclude pectoralis major transfer.
Anesthesia and beach chair positioning are as described for the latissimus dorsi transfer.
Before draping, the passive external rotation of the unaffected contralateral arm is assessed.
Surgical Landmarks and Incisions
| • | Deltopectoral approach: the lateral aspect of the coracoid and the deltoid insertion serve as the boundaries of the deltopectoral incision. |
| • | The axillary nerve courses over the belly of the subscapularis and is at risk throughout the mobilization of the subscapularis. | |
| • | The medial pectoral nerve is at risk during dissection and mobilization of the sternal head of the pectoralis if dissection is carried too medially. Injury to this nerve results in denervation of the transferred muscle. | |
| • | Axillary artery |
Specific Steps (
Box 21-2
)
With the arm in slight forward flexion, abduction, and neutral rotation, a standard deltopectoral approach, extending from the lateral aspect of the coracoid toward the insertion of the deltoid, is employed for initial exposure. Taking the cephalic vein laterally, the interval between the pectoralis major and deltoid is exposed and maintained with self-retaining retractors. The clavipectoral fascia is incised, and the conjoined tendon is retracted medially. Externally rotate the arm to expose the lesser tuberosity.
| Surgical Steps of Pectoralis Transfer | |||||||||||||||
|
2. Evaluation and Mobilization of the Subscapularis Tendon
The subscapularis tendon deficiency may initially be difficult to appreciate as the lesser tuberosity is often enveloped in scar tissue. After this scar is excised and the bone of the lesser tuberosity is exposed, identification of the torn edge of the subscapularis tendon is attempted. The remnant tendon is tagged with 3-0 braided suture and mobilized from under the conjoined tendon with a combination of blunt and sharp dissection. Care is taken to protect the axillary nerve on the anterior inferior aspect of the subscapularis during dissection. If the subscapularis tendon is of poor quality or irreparable, proceed with the pectoralis major transfer.
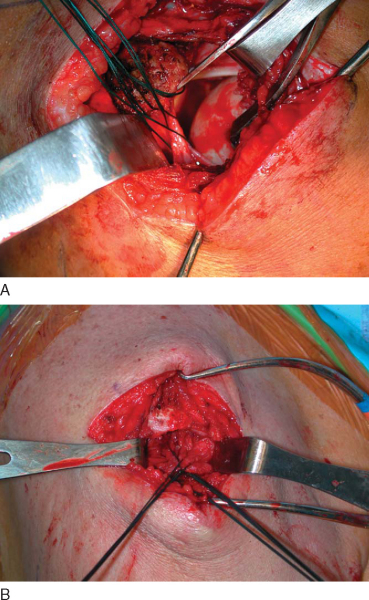
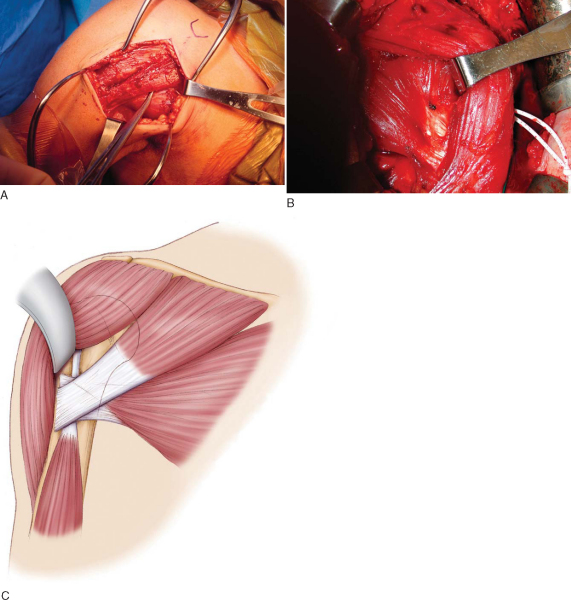
3. Harvest of Sternal Head of the Pectoralis Major Tendon
The interval between the sternal and clavicular heads of the pectoralis major tendon is best delineated at its humeral insertion. Placement of the muscle under tension by abducting and externally rotating the shoulder facilitates the differentiation of the sternal and clavicular portions of the pectoralis major. Often, a stripe of fatty tissue may be present in the plane between the two muscles (
Fig. 21-15A
). A Cobb elevator, No. 15 scalpel blade, or Metzenbaum scissors are used to isolate the tendon of the sternal head as it inserts inferior and deep to the clavicular head (
Fig. 21-15B and C
). The tendon is then detached sharply off the bone. After No. 2 braided nonabsorbable traction sutures are placed into the tendon in a Mason-Allen fashion, blunt dissection between the muscle bellies of the sternal and clavicular heads proceeds medially. The medial and lateral pectoral nerves are safe as long as one stays lateral to the pectoralis minor and less than 8.5 cm from the humeral insertion of the pectoralis major.
|
|
|
|
Figure 21-15 |
4. Transfer under the Clavicular Head
After the sternal head is sufficiently mobilized, a Kelly clamp is passed from superior to inferior, deep to the clavicular head of the pectoralis major and lateral to the conjoined tendon. The traction sutures are grasped with this clamp to transfer the sternal head under the clavicular head (
Fig. 21-16
).
|
|
|
|
Figure 21-16 (A and B redrawn from Warner JJP. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instr Course Lect 2001;50:63-71.) |
5. Fixation to the Humeral Head
The arm is then placed into the patient’s physiologic amount of passive external rotation, as determined by the nonoperative arm during the examination under anesthesia. The transferred sternal head of the pectoralis major is then fixed to the lesser tuberosity by anchors or transosseous sutures.
| • | A sling is worn for 6 weeks with only passive range of motion to protect the transfer and to limit scarring. | |
| • | Begin active-assisted range of motion after 6 weeks. | |
| • | Start active range of motion at 2 months. | |
| • | Strengthening may begin after 3 months. | |
| • | Return to sport or work after 6 months. |
| • | Recurrent instability | |
| • | Avulsion of transferred pectoralis tendon | |
| • | Infection | |
| • | Deep venous thrombosis | |
| • | Coracohumeral impingement |
After split pectoralis major tendon transfer, good to excellent results are achieved in nearly 80% of patients. Although patients usually have improvement in function and a decrease in pain, many will not have a negative liftoff test result postoperatively. Better results are obtained if the subscapularis tendon can be partially or completely repaired concomitantly with the pectoralis major transfer (
Table 21-3
).
| Author | No. of Patients | Followup | Outcomes |
|---|---|---|---|
| Warner (2004) | 11 | 38 months | ASES score improved from 42 to 61 |
| 81% of patients satisfied | |||
| Aldridge et al[1] (2004) | 11 | 31 months | Constant score improved from 21 to 36 |
| 63% of patients satisfied | |||
| Gerber et al[14] (2004) | 30 | 32 months | Constant score improved from 47 to 70 |
| 82% good–excellent results | |||
| Galatz et al[12] (2003) | 14 | 18 months | 79% of patients satisfied |
| Noerdlinger et al[39] (2002) | 15 | 64 months | Improved Rowe scores |
| Improved Constant scores | |||
| Return to preinjury activities | |||
| Resch et al[42] (2000) | 12 | 28 months | Constant score improved from 27 to 67 |
| 75% good–excellent results |
| PEARLS AND PITFALLS | |||||||||||||||
|
1.
Aldridge JM, Atkinson TS, Mallon WJ: Combined pectoralis major and latissimus dorsi tendon transfer for massive rotator cuff deficiency.
J Shoulder Elbow Surg 2004; 13:621-629.
2.
Aoki M, Okamura K, Fukushima S, et al: Transfer of latissimus dorsi for irreparable rotator cuff tears.
J Bone Joint Surg Br 1996; 78:761-766.
3.
Apoil A, Augereau B: Reparation par lambeau de deltoid des grandes pertes de substance de la coiffe des rotateurs de l’epaule.
Chirurgie 1985; 11:287-290.
4.
Arntz CT, Matsen III FA, Jackins S: Surgical management of complex irreparable rotator cuff deficiency.
J Arthroplasty 1991; 6:363-370.
5.
Beauchamp M, Beaton DE, Barnhill TA, et al: Functional outcome after L’Episcopo procedure.
J Shoulder Elbow Surg 1998; 7:90-96.
6.
Burkhart SS: Arthroscopic débridement and decompression for selected rotator cuff tears: clinical results, pathomechanics, and patient selection based on biomechanical parameters.
Orthop Clin North Am 1993; 24:111-123.
7.
Cleeman E, Hazrati Y, Auerbach JD, et al: Latissimus dorsi tendon transfer for massive rotator cuff tears: a cadaveric study.
J Shoulder Elbow Surg 2003; 12:539-543.
8.
Cofield RH: Subscapularis muscle transposition for repair of chronic shoulder cuff tears.
Surg Gynecol Obstet 1982; 154:667-672.
9.
Comtet JJ, Herzberg G, Naasan IA: Biomechanical basis of transfers for shoulder paralysis [review].
Hand Clin 1989; 5:1-14.
10.
Covey DC, Riordan DC, Milstead ME, et al: Modification of the L’Episcopo procedure for brachial plexus birth palsies.
J Bone Joint Surg Br 1992; 74:897-901.
11.
DeFranco MJ, Derwin K, Iannotti JP: New therapies in tendon reconstruction.
J Am Acad Orthop Surg 2004; 12:298-304.
12.
Galatz LM, Connor PM, Calfee RP, et al: Pectoralis major transfer for anterior-superior subluxation in massive rotator cuff insufficiency.
J Shoulder Elbow Surg 2003; 12:1-5.
13.
Gazielly DF, Gleyze P, Montagnon C: Functional and anatomical results after rotator cuff repair.
Clin Orthop 1994; 304:43-53.
14.
Gerber A, Clavert P, Millett PJ, et al: Split pectoralis major and teres major tendon transfers for reconstruction of irreparable tears of the subscapularis.
Tech Shoulder Elbow Surg 2004; 5:5-12.
15.
Gerber C: Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff.
Clin Orthop 1992; 275:152-160.
16.
Gerber C, Hersche O: Tendon transfers for the treatment of irreparable rotator cuff defects.
Orthop Clin North Am 1997; 28:195-203.
17.
Gerber C, Maquieira G, Espinosa N: Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears.
J Bone Joint Surg Am 2006; 88:113-120.
18.
Gerber C, Meyer DC, Schneeberger AG, et al: Effect of tendon release and delayed repair on the structure of the muscles of the rotator cuff: an experimental study in sheep.
J Bone Joint Surg Am 2004; 86:1973-1982.
19.
Gerber C, Vihn TS, Hertel R, et al: Latissimus dorsi transfer for treatment of massive tears of the rotator cuff: a preliminary report.
Clin Orthop 1988; 232:51-61.
20.
Goutallier D, Postel JM, Bernageau J, et al: Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan.
Clin Orthop 1994; 304:78-83.
21.
Habermeyer P, Magosch P, Rudolph T, et al: Transfer of the tendon of latissimus dorsi for the treatment of massive tears of the rotator cuff: a new single incision technique.
J Bone Joint Surg Br 2006; 88:208-212.
22.
Harryman DT, Mack LA, Wang KY: Repairs of the rotator cuff: correlation of functional results with integrity of the cuff.
J Bone Joint Surg Am 1991; 73:982-989.
23.
Hertel R, Ballmer FT, Lombert SM, et al: Lag signs in the diagnosis of rotator cuff rupture.
J Shoulder Elbow Surg 1996; 5:307-313.
24.
Herzberg G, Urien JP, Dimnet J: Potential excursion and relative tension of muscles in the shoulder girdle: relevance to tendon transfers.
J Shoulder Elbow Surg 1999; 8:430-437.
25.
Hettrich CM, Weldon 3rd E, Boorman RS, et al: Optimizing the glenoid contribution to the stability of a humeral hemiarthroplasty without a prosthetic glenoid.
J Bone Joint Surg Am 2004; 86:2022-2029.
26.
Hockman DE, Lucas GL, Roth CA: Role of the coracoacromial ligament as restraint after shoulder hemiarthroplasty.
Clin Orthop 2004; 419:80-82.
27.
Hoffer MM, Wickenden R, Roper B: Brachial plexus birth injuries: results of tendon transfer of the rotator cuff.
J Bone Joint Surg Am 1978; 60:691-695.
28.
Jonsson B, Olofsson BM, Steffner LC: Function of the teres major, latissimus dorsi, and pectoralis major muscles: a preliminary study.
Acta Morphol Neerl Scand 1971; 9:275.
29.
Jost B, Puskas GJ, Lustenberger A, et al: Outcome of pectoralis major transfer for the treatment of irreparable subscapularis tears.
J Bone Joint Surg Am 2003; 85:1944-1951.
30.
Laudicina L, D’Ambrosia R: Management of irreparable rotator cuff tears and glenohumeral arthritis.
Orthopedics 2005; 28:382.358
31.
L’Episcopo JB: Tendon transplantation in obstetrical paralysis.
Am J Surg 1934; 25:122-125.
32.
Meyer DC, Hoppeler H, von Rechenberg B, Gerber C: A pathomechanical concept explains muscle loss and fatty muscular changes following surgical tendon release.
J Orthop Res 2004; 22:1004-1007.
33.
Meyer DC, Pirkl C, Pfirrmann WA, et al: Asymmetric atrophy of the supraspinatus muscle following tendon tear.
J Orthop Res 2005; 23:254-258.
34.
Miller BS, Joseph TA, Noonan TJ, et al: Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment, and outcome.
J Shoulder Elbow Surg 2005; 14:492-496.
35.
Miniaci A, MacLeod M: Transfer of the latissimus dorsi muscle after failed repair of a massive tear of the rotator cuff.
J Bone Joint Surg Am 1999; 81:1120-1127.
36.
Neer CS, Flatow EL, Lech O: Tears of the rotator cuff: long term results of anterior acromioplasty and repair.
Orthop Trans 1988; 12:735.
37.
Neviaser JS, Neviaser RJ, Neviaser TJ: The repair of chronic massive ruptures of the rotator cuff of the shoulder by use of a freeze-dried rotator cuff.
J Bone Joint Surg Am 1978; 60:681-684.
38.
Neviaser RJ, Neviaser TJ: Transfer of the subscapularis and teres minor for massive defects of the rotator cuff.
In: Bayley IL, Kessel L, ed. Shoulder Surgery,
Berlin: Springer; 1982:60-63.
39.
Noerdlinger MA, Cole BJ, Stewart M, Post M: Results of pectoralis major transfer with fascia lata autograft augmentation for scapula winging.
J Shoulder Elbow Surg 2002; 11:345-350.
40.
Ozaki J, Fujimoto S, Masuhara K: Reconstruction of chronic massive rotator cuff tears with synthetic materials.
Clin Orthop 1986; 202:173-183.
41.
Phipps GJ, Hoffer MM: Latissimus dorsi and teres major transfer to rotator cuff for Erb’s palsy.
J Shoulder Elbow Surg 1995; 4:124-129.
42.
Resch H, Povacz P, Ritter E, et al: Transfer of the pectoralis major muscle for the treatment of irreparable rupture of the subscapularis tendon.
J Bone Joint Surg Am 2000; 82:372-382.
43.
Rockwood CA, Burkhead WZ: Management of patients with massive rotator cuff débridement.
Orthop Trans 1988; 12:12.190.
44.
Rockwood Jr CA, Williams Jr GR, Burkhead Jr WZ: Débridement of degenerative, irreparable lesions of the rotator cuff.
J Bone Joint Surg Am 1995; 77:857-866.
45.
Schoierer O, Herzberg G, Berthonnaud E, et al: Anatomical basis of latissimus dorsi and teres major transfers in rotator cuff tear surgery with particular reference to the neurovascular pedicles.
Surg Radiol Anat 2001; 23:75-80.
46.
Shiino K: Über die Bewegungen im Schultergelenk und die Arbeitsleistung der Schultermuskeln.
Arch Anat Physiol Anat 1913;1-89.
47.
Warner JJP: Management of massive irreparable rotator cuff tears: the role of tendon transfer.
AAOS Instr Course Lect 2001; 50:63-71.
48.
Warner JJP, Gerber C: Treatment of massive rotator cuff tears: posterior-superior and anterosuperior.
In: Iannotti JP, ed. The Rotator Cuff: Current Concepts and Complex Problems,
Rosemont, Ill: American Academy of Orthopaedic Surgeons; 1998:59-94.
49.
Warner JJP, Parsons M: Latissimus dorsi transfer: a comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears.
J Shoulder Elbow Surg 2001; 10:514-521.
50.
Watson M: Major ruptures of the rotator cuff: the results of surgical repair in 89 patients.
J Bone Joint Surg Br 1985; 67:618.
51.
Wirth MA, Rockwood Jr CA: Operative treatment of irreparable rupture of the subscapularis.
J Bone Joint Surg Am 1997; 79:722-731.
52.
Zachary RB: Transplantation of teres major and latissimus dorsi for loss of external rotation at shoulder.
Lancet 1947; 2:757.