CHAPTER 17 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 17 – Arthroscopic Rotator Cuff Repair: Double-Row Techniques
Neal S. ElAttrache, MD
The persistent tear rate after open and arthroscopic rotator cuff repair is concerning [3] [4] [5] [6] [7] and has stimulated development of improved rotator cuff repair techniques. Arthroscopic repair techniques currently emphasize proper recognition of tear pattern, adequate mobilization of retracted tendons, restoration of the native insertional footprint, and adequate repair strength. The techniques for arthroscopic rotator cuff repair have evolved from single-row suture anchors to double rows of suture anchors in the greater tuberosity. Studies have also shown that transosseous tunnel repair techniques provide improved footprint coverage,[2] pressurized contact area at the footprint,[11] and reduced motion at the footprint tendon-bone interface.[1] It is believed that improved contact characteristics will help maximize healing potential between repaired tendons and the greater tuberosity. The most recent techniques developed in double-row rotator cuff repair now replicate transosseous tunnel techniques and create tissue compression against the tuberosity to enhance healing.[10] These new techniques have been referred to as suture bridge techniques.
| • | Anterolateral shoulder pain exacerbated with overhead activity | |
| • | Patients may report specific trauma | |
| • | Night pain when sleeping on the affected side | |
| • | Weakness with overhead activity |
Indications and Contraindications
The surgeon’s, anesthesiologist’s, and patient’s preferences determine the type of anesthesia administered. The procedure may be performed under regional anesthesia, general anesthesia, or a combination. The patient may be positioned in either the beach chair or the lateral decubitus position. The beach chair position is more familiar to many surgeons and is often easier to convert to an open procedure. The lateral decubitus position provides traction on the arm, which enhances visualization in the subacromial space.
Surgical Landmarks and Portals
| • | Clavicle | |
| • | Acromion | |
| • | Scapular spine | |
| • | Acromioclavicular joint | |
| • | Coracoid process |
| • | Posterior portal | |
| • | Posterolateral portal | |
| • | Lateral portal | |
| • | Anterior portal | |
| • | Neviaser portal |
Examination Under Anesthesia and Diagnostic Arthroscopy
Examination under anesthesia confirms passive range of motion. Diagnostic arthroscopy is performed in a stepwise fashion to evaluate the following:
| • | Anterior, posterior, and superior labrum | |
| • | Proximal biceps tendon | |
| • | Rotator cuff, including subscapularis | |
| • | Cartilage surfaces of the humeral head and glenoid |
Specific Steps (
Box 17-1
)
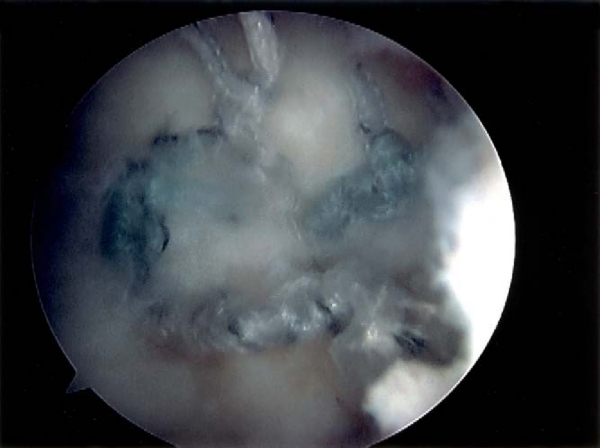
A standard posterior portal is established, and glenohumeral diagnostic arthroscopy is performed with appropriate intraarticular procedures carried out. The camera is then introduced into the subacromial space, and a lateral working portal is made 2 cm lateral to the midanterior acromion. A bursectomy is performed, and the tear pattern is identified (crescent-shaped, L-shaped, U-shaped, combined). An acromioplasty is performed as necessary.
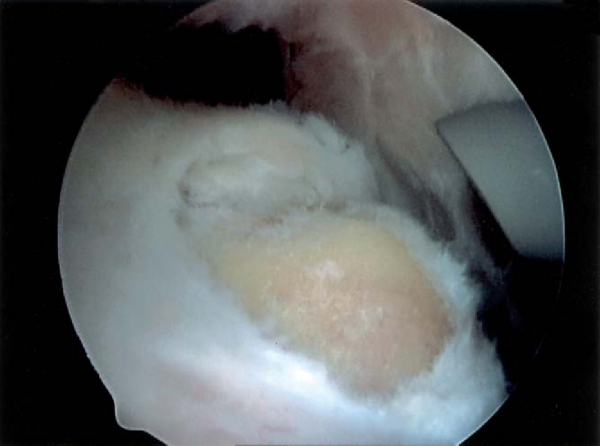
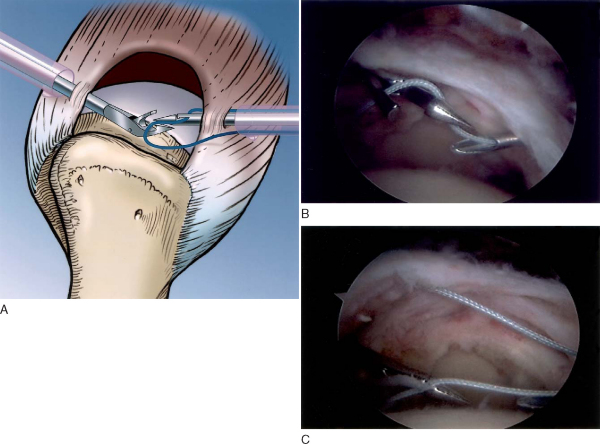
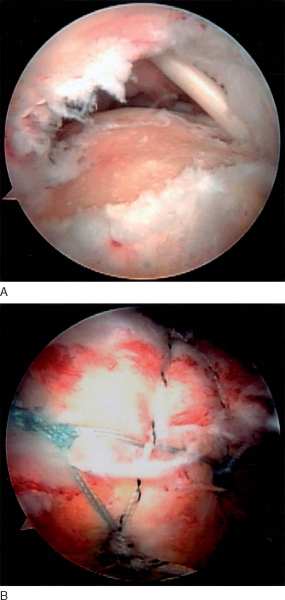
The lateral mobility of the tear is assessed by grasping the tear edge and pulling laterally. Crescent-shaped tears mobilize easily to the lateral aspect of the greater tuberosity footprint with minimal tension and do not require releases or mobilization techniques (Figs. 17-1 to 17-3 [1] [2] [3]). With the camera in the lateral portal, anterior and posterior tear mobility is assessed by pulling the anterior rotator cuff tear limb posterior and the posterior rotator cuff tear limb anterior. For U-shaped tears, the anterior and posterior tear limbs both have mobility. L-shaped tears have asymmetric limb mobility; typically, the posterior limb is more mobile than the anterior limb.
|
|
|
|
Figure 17-3 |
Many chronic tears are immobile, and mobilization techniques are performed as necessary, including anterior interval slide, posterior interval slide, and capsular releases. A double-row repair requires adequate lateral mobilization of the tendon so that it may cover the entire footprint in the lateral direction (see
Fig. 17-3
).
3. Greater Tuberosity Preparation
The greater tuberosity footprint is débrided with removal of soft tissue, and the cortical bone is abraded to stimulate healing. Decortication is avoided because it may compromise suture anchor fixation strength (see
Fig. 17-1
).
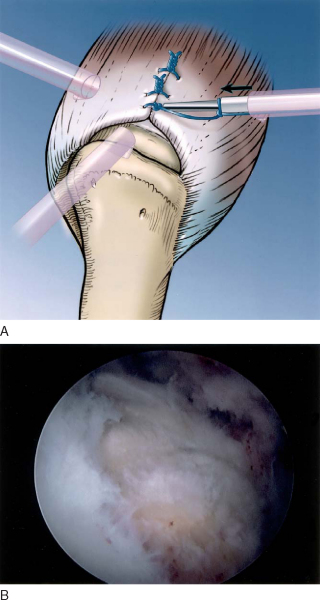
U- and L-shaped tears often have poor lateral mobility, and margin convergence sutures are necessary (Figs. 17-4 and 17-5 [4] [5]). While viewing from the lateral portal, free No. 2 sutures are passed through the anterior limb of rotator cuff and then the posterior limb to form a simple suture configuration (
Fig. 17-6
). The suture-passing sequence is repeated for the necessary number of sutures to convert the U- or L-shaped component to a crescent-shaped tear. Two to four sutures are typically placed. Knot tying for these sutures is delayed until after the medial row of suture anchors is placed to avoid restricting exposure to the medial tuberosity. Tying of the margin convergence sutures converts the U-shaped tear to a crescent-shaped tear, and the techniques for crescent-shaped tear repair are then carried out (
Fig. 17-7
).
|
|
|
|
Figure 17-6 |
|
|
|
|
Figure 17-7 |
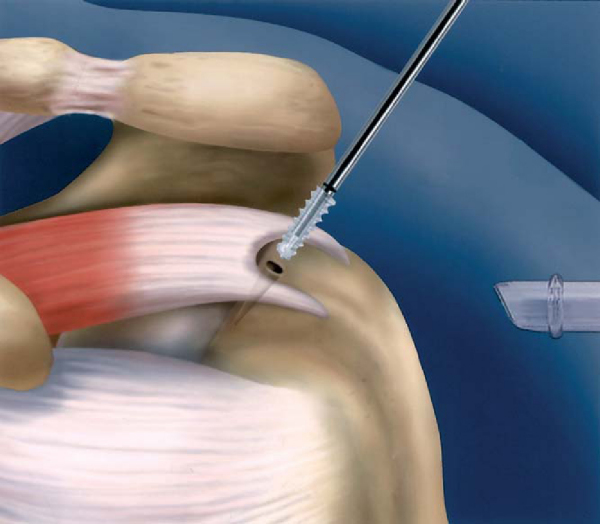
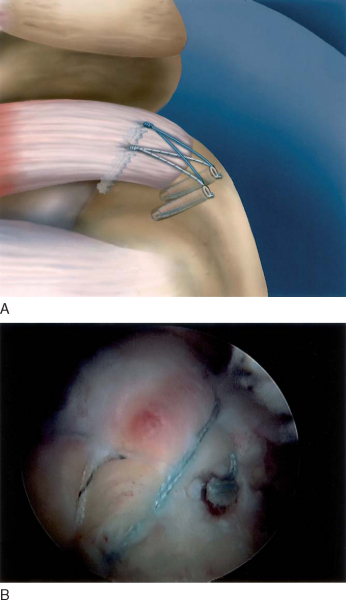
5. Medial-Row Suture Anchor Placement
The repair sequence involves placement of a medial row of suture anchors followed by suture passing through the tendon in a mattress fashion. The medial-row anchors are positioned as medial as possible adjacent to the articular surface of the humeral head (
Fig. 17-8
). For a typical crescent-shaped supraspinatus tear, two anchors are placed, one in the anterior third and one in the posterior third of the footprint (
Fig. 17-9
). For larger tears, more anchors are placed as necessary. Suture anchors that are double loaded with two sutures are preferred.
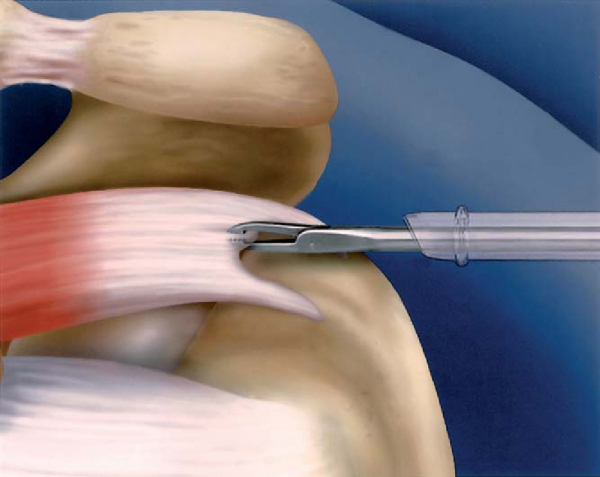
If margin convergence sutures are placed, they are tied before medial anchor suture passing. Medial suture anchor passing is then performed, creating medial mattress suture configurations, ideally 10 to 12 mm medial to the lateral edge of the rotator cuff tear. This requires suture-passing instrumentation that will facilitate medial placement of the suture (
Fig. 17-10
). This maximizes the tendon available for contact with the footprint. The sutures are passed with the surgeon’s preferred suture-passing device. The second suture from the anchor, if it is double loaded, may also be placed as a second mattress suture.
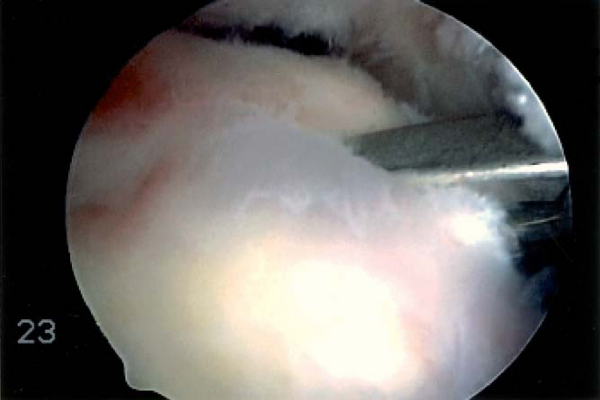
7. Lateral-Row Suture Anchor Placement
Next, the lateral row of suture anchors is placed. On the basis of the size of the footprint repair site, one or two lateral suture anchors are placed. The anchors are placed lateral to the lateral edge of the footprint to fully maximize the tendon-to-footprint contact.
For non–suture bridge double-row repair, the lateral sutures are placed in a simple fashion with the surgeon’s preferred suture-passing devices. Typically, 5 to 8 mm of tissue is captured in the simple sutures.
Knot tying is typically performed in the following sequence: lateral sutures working from posterior to anterior; medial sutures working from posterior to anterior.
Figure 17-11
demonstrates a completed double-row repair.
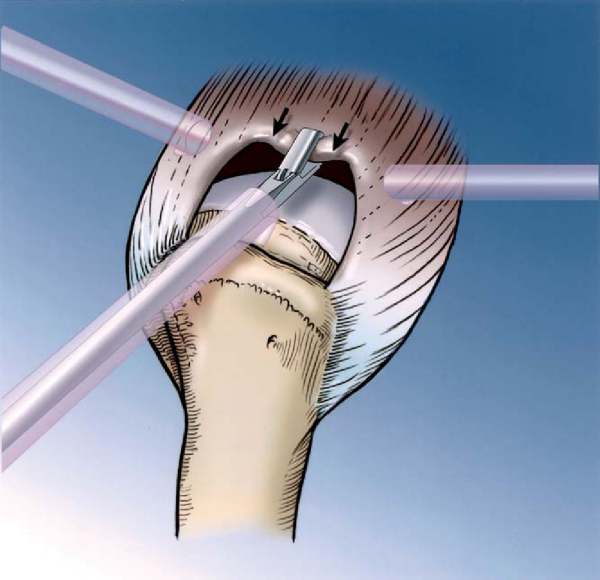
Alternative Techniques: Suture Bridge Methods
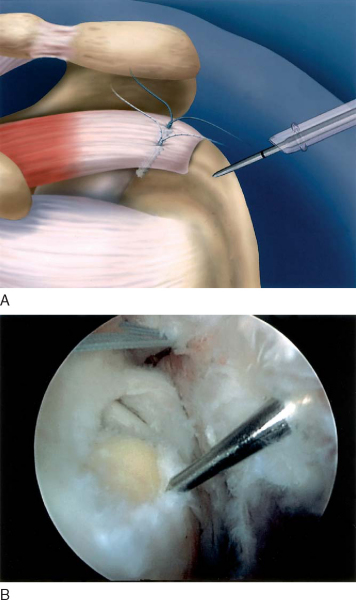
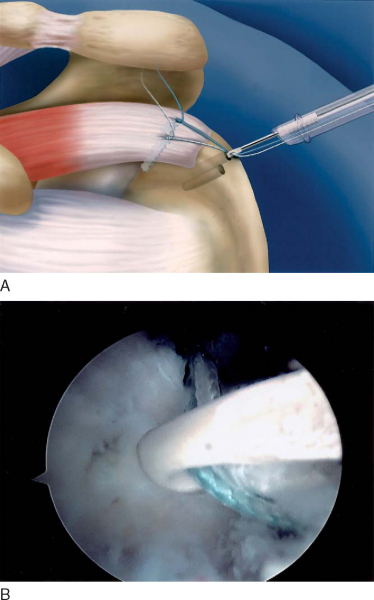
Suture Shuttle Through Lateral Anchor
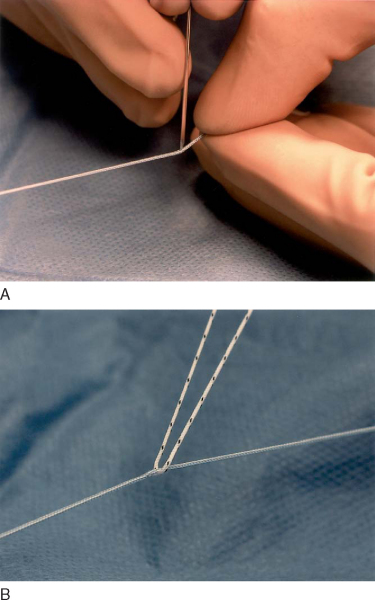
Techniques have been developed to make suture bridges that are equivalent to transosseous tunnel compression stitches. Several variations exist to form a suture bridge, and early methods made use of existing implants and instruments. The medial suture anchors are placed as previously described for a double-row technique. One suture from each anchor is placed in a horizontal mattress fashion. The second suture limbs from each anchor are then passed together just medial to the horizontal mattress sutures. This not only makes a suture bridge but also approximates a modified Mason-Allen suture construct. Either one or two lateral suture anchors may be placed just lateral to the edge of the greater tuberosity (
Fig. 17-12
). After all sutures are passed, the horizontal mattress sutures are tied. One limb from the medial compression suture and one suture from the lateral anchor are retrieved outside the lateral cannula. The suture from the medial anchor is then sewn through the lateral suture with a free needle (
Fig. 17-13
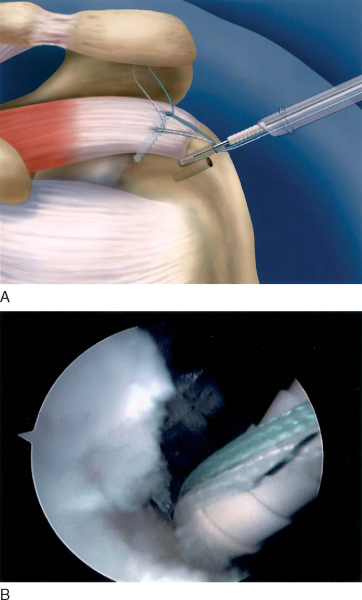
). The lateral suture, acting as a shuttle with the medial suture attached to it, is pulled through the eyelet. A second suture may be shuttled through each anchor to make a cruciate-type suture bridge, if desired, to enhance the repair (
Fig. 17-14
). After the sutures are shuttled, knot tying is performed (
Fig. 17-15
).
|
|
|
|
Figure 17-12 |
|
|
|
|
Figure 17-13 |
|
|
|
|
Figure 17-15 |
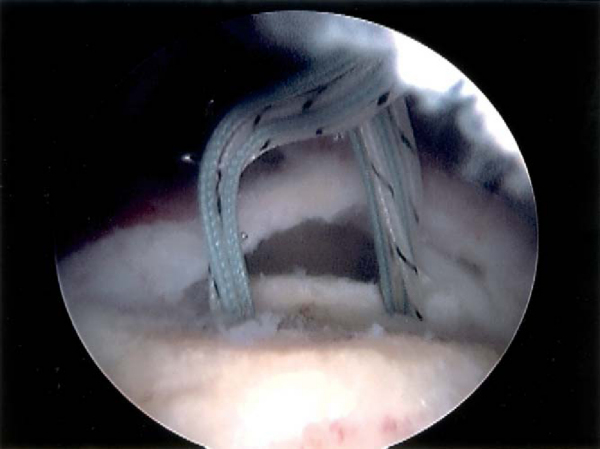
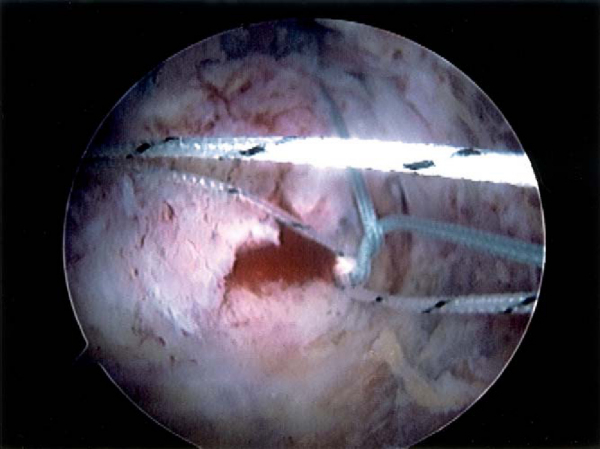
A new implant has been developed to facilitate placement of compression sutures and to reduce knot tying. For the PushLock (Arthrex, Naples, Fla) device, medial suture anchor placement and suture passing are performed as previously described for the double-row repair technique. A hole is then punched at the intended site for the lateral implant, just lateral to the lateral edge of the tuberosity. The medial sutures to be used for compression (one suture from the anterior medial anchor and one suture from the posterior medial anchor) are then passed through the eyelet of the implant outside the cannula (
Fig. 17-16
). Manual tension is applied to the suture bridge sutures as they are delivered into the tunnel to achieve the desired compression (
Fig. 17-17
). The implant is advanced over the inserter and captures the eyelet, which fixes the sutures in place and eliminates the need for knot tying. The sutures are then cut. Cruciate suture configurations can be made with a second PushLock anchor to further enhance the repair (
Fig. 17-18
).
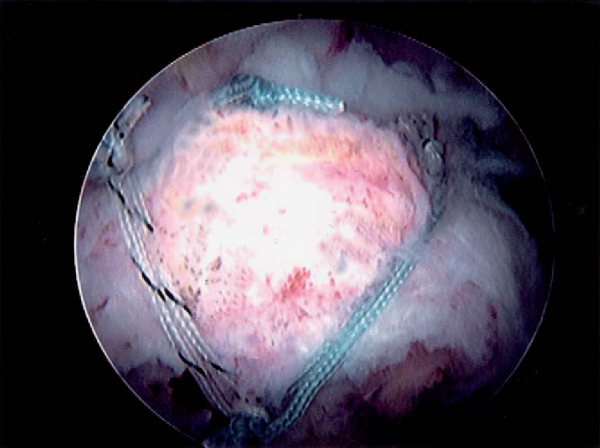
Figure 17-19
demonstrates a case example of a crescent-shaped tear repaired with a four–suture bridge technique.
|
|
|
|
Figure 17-16 |
|
|
|
|
Figure 17-17 |
|
|
|
|
Figure 17-18 |
|
|
|
|
Figure 17-19 |
Patients are placed in a sling with a small abduction pillow. The sling is worn continuously for 6 weeks except for bathing. During the first 6 weeks, active elbow, wrist, and hand exercises are performed. From 6 to 12 weeks, passive and active-assisted range of motion is initiated. After 12 weeks, active motion and gentle strengthening are initiated. More aggressive strengthening is initiated at 4 months.
| • | Failure of tendon to heal | |
| • | Stiffness | |
| • | Missed pathologic changes: acromioclavicular joint arthritis, biceps tendinitis | |
| • | Infection |
| PEARLS AND PITFALLS | |||||||||||||||
|
To date, no clinical studies specifically report the outcome of double-row suture anchor repair techniques or suture bridge repair techniques for management of rotator cuff tears. Several laboratory studies indicate improved strength of fixation to cyclic loading for double-row rotator cuff repairs compared with single-row rotator cuff repairs. [8] [9] Other studies have demonstrated that traditional transosseous repair techniques have superior restoration of footprint coverage,[2] pressurized footprint contact area,[11] and decreased motion at the footprint tendon-bone interface.[1] In the laboratory, we have compared suture bridge rotator cuff repairs with double-row rotator cuff repairs that are currently employed clinically.[10] For strength of fixation, the four–suture bridge technique had significantly higher ultimate load to failure with no difference in gap formation to cyclic loading. Furthermore, the suture bridge rotator cuff repair provided more pressurized contact area and mean pressure over the repaired rotator cuff tendon insertion compared with a double-row technique.
1.
Ahmad CS, Stewart AM, Izquierdo R, Bigliani LU: Tendon-bone interface motion in transosseous suture and suture anchor rotator cuff repair techniques.
Am J Sports Med 2005; 33:1667-1671.
2.
Apreleva M, Ozbaydar M, Fitzgibbons PG, Warner JJ: Rotator cuff tears: the effect of the reconstruction method on three-dimensional repair site area.
Arthroscopy 2002; 18:519-526.
3.
Bishop J, Lo I, Klepps S, et al. Cuff integrity following arthroscopic versus open rotator cuff repair: a prospective study. Proceedings, American Academy of Orthopaedic Surgeons 71st annual meeting; San Francisco, Calif; 2004.
4.
Galatz LM, Ball CM, Teefey SA, et al: The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears.
J Bone Joint Surg Am 2004; 86:219-224.
5.
Gazielly DF, Gleyze P, Montagnon C: Functional and anatomical results after rotator cuff repair.
Clin Orthop 1994; 304:43-53.
6.
Harryman DT, Mack LA, Wang KY, et al: Repairs of the rotator cuff. Correlations of functional results with integrity of the cuff.
J Bone Joint Surg Am 1991; 73:982-989.
7.
Jost B, Pfirrmann CWA, Gerber C: Clinical outcome after structural failure of rotator cuff repairs.
J Bone Joint Surg Am 2000; 82:304-314.
8.
Kim DH, ElAttrache NS, Tibone JE, et al: Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair.
Am J Sports Med 2006; 34:407-414.
9.
Ma CB, Comerford L, Wilson J, Puttlitz CM: Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation.
J Bone Joint Surg Am 2006; 88:403-410.
10.
Park M, ElAttrache N, Tibone J, et al. Footprint contact biomechanics for a new arthroscopic transosseous-equivalent rotator cuff repair technique compared to a double-row technique arthroscopic rotator cuff repair. American Shoulder and Elbow Surgeons Specialty Day meeting; Chicago, Ill; 2006.
11.
Park MC, Cadet ER, Levine WN, et al: Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques.
Am J Sports Med 2005; 33:1154-1159.