Carpal Fractures
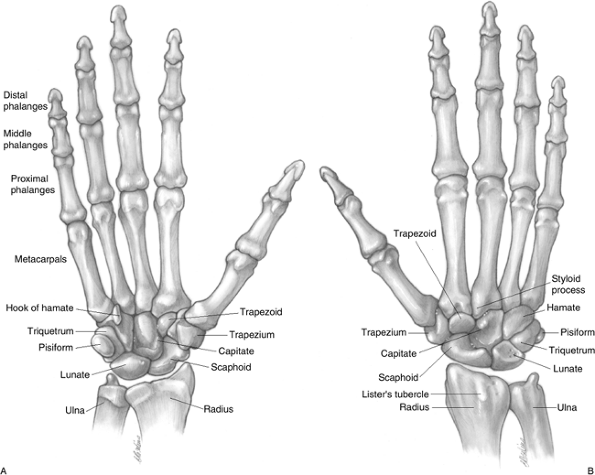
proximal and a distal row, with each row containing four bones. The
proximal row includes (from radial to ulnar) the scaphoid, lunate,
triquetrum, and pisiform. The pisiform is located palmar to the plane
of the remaining three carpal bones of the proximal row, and the
pisotriquetral joint is separated from the adjacent articulations. The
distal row includes (from radial to ulnar) the trapezium, trapezoid,
capitate, and hamate. The carpus is divided into the radiocarpal joint and the midcarpal joints.
The proximal row is convex proximally and concave distally. The
proximal row articulates proximally with the distal radius and with the
triangular fibrocartilage complex, forming the radiocarpal and
ulnocarpal joint. The proximal row articulates distally with the distal
carpal row forming the midcarpal joint.
with the five metacarpal bones and with each other. The bones of the
distal carpal row are straighter in alignment across the wrist than the
proximal row, especially at their distal articulations with the
metacarpal bones.
arch is formed by the arrangement of the proximal and distal rows. On
the palmar surface, however, a deep concavity is formed, designated as
the carpal groove. The carpal groove is
accentuated by the palmar projection of the pisiform and hook of the
hamate ulnarly, and by the projection of the scaphoid tuberosity and
trapezial ridge radially. The midcarpal joint and the radiocarpal joint
usually do not communicate with each other; if communication does
occur, as seen through the flow of dye from an arthrogram, there is a
tear or rent in the scapholunate or lunotriquetral ligaments.
the ulnar side of Lister’s tubercle on its way from the wrist to the
distal phalanx of the thumb. The extensor carpi radial brevis (ECRB) is
to the radial side of this tubercle. Lister’s tubercle is located 0.5
cm from the radiocarpal joint and is in line with the cleft between the
index and middle finger metacarpals. The interval between the proximal
pole of the scaphoid and its articulation with the lunate and the
scapho-lunate ligament is just ulnar and distal to Lister’s tubercle.
the middle finger metacarpal, points to the articular interface between
the capitate and trapezoid, and is just proximal to the insertion of
the ECRB tendon.
wrist is in line with the middle finger metacarpal, is just distal and
ulnar to Lister’s tubercle, and marks the location of the carpal lunate.
and dorsal to the abductor pollicis longus (APL) and extensor pollicis
brevis (EPB) tendons that course across its apex.
 |
|
Figure 11.1-1 A. Skeletal anatomy of the wrist, palmar aspect. B. Skeletal anatomy of the wrist, dorsal aspect.
|
and styloid process. The head is most visible and palpable when the
forearm is in pronation; the posteroulnar styloid is most readily palpable in supination and is approximately 1 cm proximal to the plane of the radial styloid.
aspect of the base of the hand, provides a visible and palpable
landmark that aids in the identification and location of the flexor
carpi ulnaris (FCU) tendon, the underlying ulnar neurovascular bundle,
and the hook process of the hamate.
aspect of the distal carpus, can be palpated approximately 1 cm radial
and distal to the pisiform. Because of its deep location, it may be
difficult to palpate in some individuals. The hook of the hamate lies
between the ulnar tunnel (Guyon’s canal) and the carpal tunnel. It thus
provides a landmark for the ulnar nerve and artery (located just ulnar
to the hook), and the ulnar boundary of the carpal tunnel. Point
tenderness in this area may indicate a fracture of the hook process, a
somewhat common injury in sports that use racquets, clubs, or bats,
such as tennis, golf, or baseball.
the scaphoid. It projects into the palm, and the tubercle is palpable
on the radial aspect of the base of the hand, usually just distal to
the distal palmar wrist crease. It becomes
more prominent with the wrist positioned in radial deviation, since the
scaphoid assumes a position of more palmar flexion in this position.
Conversely, the scaphoid tubercle is less prominent and possibly not
palpable when the wrist is in ulnar deviation, since the scaphoid
assumes a position of decreased palmar flexion and lies more in the
plane of the radius and ulna.
 |
|
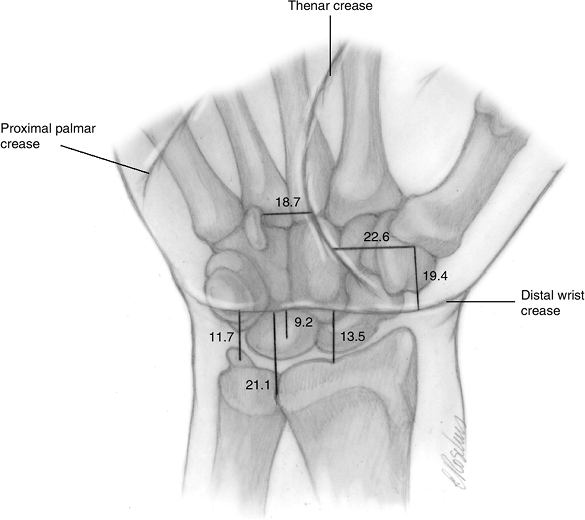
Figure 11.1-2
Flexion crease landmarks. Relationship of the carpal bones and other bony landmarks to the thenar and distal wrist creases. The number indicate the mean distance (in mm) of the structures depicted from the respective creases. |
carpal row and passes over the waist of the scaphoid and, 80% of the
time, over the pisiform bone. The lunate is proximal to the distal
wrist crease with its center an average of 9.2 mm from the crease. The
radiocarpal joint is 13.5 mm proximal to the crease and the center
point of the distal radioulnar joint (DRUJ) is 21.1 mm proximal to the
wrist crease. The base of the ulnar styloid is on average 11.7 mm
proximal to the wrist crease.
apex distal, that is bounded dorsoulnarly by the EPL, radially by the
APL and EPB tendons, and proximally by the distal margin of the
extensor retinaculum. It contains the dorsal branch of the radial
artery in the dorsoulnar corner, the tendon of the extensor carpi
radialis longus (ECRL) and one or more branches of the superficial
branch of the radial nerve. Tenderness in the anatomical snuffbox is
associated with fractures of the scaphoid.
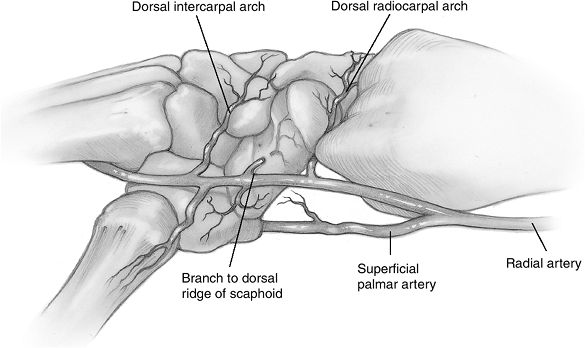
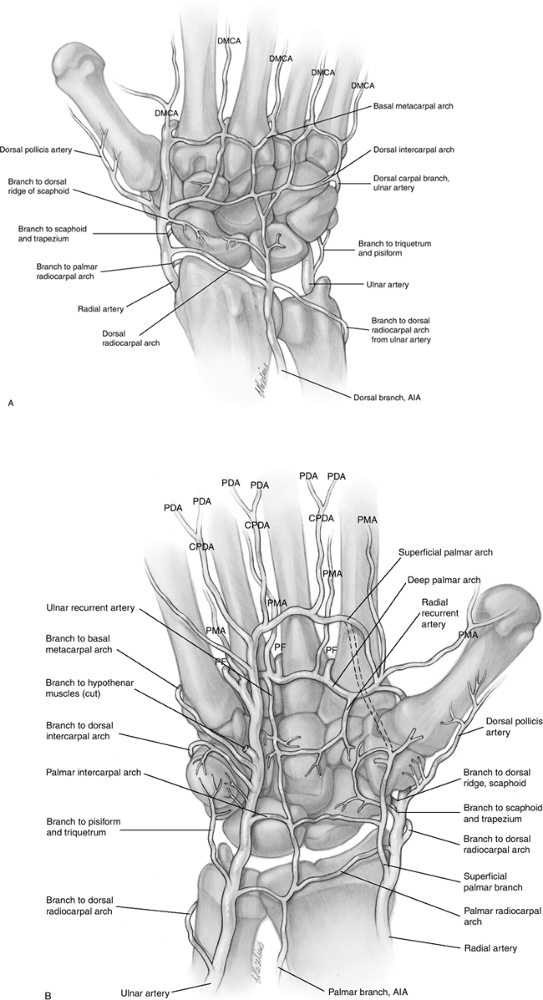
The dorsal and palmar systems consist of a series of dorsal and palmar
transverse arches that are connected by anastomoses formed by the
radial, ulnar, and anterior interosseous arteries.
Vessels enter the scaphoid in limited areas dorsally and palmarly at
nonarticular zones of ligamentous attachment. The dorsal vascular
supply to the scaphoid accounts for 70% to 80% of the internal
vascularity of the bone, all in the proximal region. The major dorsal vessels enter the bone through small foramina located at a dorsal ridge in the region of the scaphoid waist.
gives off the intercarpal artery, which immediately divides into two
branches. One branch runs transverse to the dorsum of the wrist. The
other branch runs vertically and distally over the index metacarpal.
Approximately 5 mm proximal to the origin of the intercarpal vessel at
the level of the styloid process of the radius, another vessel is given
off that runs over the radiocarpal ligament to enter the scaphoid
through its waist along the dorsal ridge.
dorsal scaphoid branch of the radial artery and the dorsal branch of
the anterior interosseous artery. No vessels enter the proximal dorsal
region of the scaphoid through the dorsal scapholunate ligament, and no
vessels enter through the dorsal cartilaginous areas. The dorsal
vessels usually divide into two or three branches soon after entering
the scaphoid. These branches run palmarly and proximally, dividing into
smaller branches to supply the proximal pole as far as the subchondral
region.
the level of the radioscaphoid joint, the radial artery gives off the
superficial palmar branch. Just distal to the origin of the superficial
palmar branch, several smaller branches course obliquely and distally
over the palmar aspect of the scaphoid to enter through the region of
the tubercle. These branches, the palmar scaphoid branches, divide into
several smaller branches just before penetrating the bone. In 75% of
specimens, these arteries arise directly from the radial artery.
 |
|
Figure 11.1-3 A, B. Anatomy of the arterial supply to the dorsal and palmar aspect of the wrist.
|
scaphoid, followed by (in descending order of incidence) the
triquetrum, trapezium, hamate, lunate, pisiform, capitate, and
trapezoid.
Experimental studies have shown that fractures of the scaphoid can be
produced consistently by forces applied to a hyperextended (90 degrees or more) and radially deviated wrist. Progressively less extension resulted in fractures of the distal radius and forearm.
-
Initial findings include a history of a
fall, complaints of persistent discomfort or pain in the wrist, and
tenderness on palpation in the anatomical snuffbox. -
X-rays are taken in four views: one posterior-anterior (PA), one lateral, and two oblique views.
-
The PA radiograph is best performed with the patient making a fist.
-
The fist posture results in slight wrist
extension, and promotes ulnar deviation of the wrist that may be useful
in opening up the fracture interface. -
This position also places the longitudinal axis of the scaphoid parallel to the plane of the x-ray plate. Figure 11.1-5 demonstrates a fracture of the carpal scaphoid.
-
-
If radiograph studies do not demonstrate
a definite fracture, the wrist is immobilized in a short-arm thumb
spica cast, and repeat radiographs made in 2 to 3 weeks. -
If radiograph studies at 2 to 3 weeks are
inconclusive, and positive physical findings are present, a bone scan
may be used to further assist in the diagnosis. -
Some surgeons may use magnetic resonance
imaging (MRI) rather than a bone scan, because MRI may detect an occult
fracture sooner than a bone scan.-
MRI with gadolinium is useful for evaluating vascularity of the scaphoid.
-
-
Computerized tomography (CT) is a useful
method to define bone anatomy, and may aid in the diagnosis of an
angular deformity that may require surgical correction.
-
Treatment options may be based on a
number of different classification systems that in turn are based on
the location of the fracture (distal, middle, or proximal pole),
stability, whether the fracture is displaced or nondisplaced,
P.163whether it is angulated or nonangulated, and the plane of the fracture relative to the long axis of the scaphoid.
![]() Figure 11.1-4 Anatomy of the arterial supply to the scaphoid and the radial aspect of the wrist.
Figure 11.1-4 Anatomy of the arterial supply to the scaphoid and the radial aspect of the wrist. -
The simplest treatment related classification is based on the location of the fracture.
-
Fractures of the tuberosity and distal
third may be treated with a short-arm thumb spica cast until union is
evident by radiograph or other studies. -
If the fracture is intra-articular and displaced, an open reduction and internal fixation may be considered.
 |
|
Figure 11.1-5 X-ray view of a fracture of the carpal scaphoid. (Courtesy of H. Relton McCarroll, Jr., MD, San Francisco)
|
-
Recent, stable, and undisplaced fractures are managed with a short-arm thumb spica cast.
-
Recent undisplaced but potentially unstable
fractures, including vertical oblique or reduced trans-scaphoid
perilunate fracture dislocations, should be managed with a long-arm
(above the elbow) thumb spica cast. Some surgeons consider a reduced
trans-scaphoid perilunate dislocation to be inherently unstable, and
advise internal fixation. -
Displaced or angulated fractures require
open reduction and internal fixation by techniques based on the
surgeon’s experience and choice, including K-wires and or Herbert
screws.
-
Recent fractures are treated with a Herbert screw followed by a long-arm thumb spica cast.
-
Delayed or nonunion and avascular
necrosis is highly likely in spite of the above-recommended treatment,
and may require one or more secondary operations including bone
grafting, vascularized bone grafting, excision of the proximal pole, or
proximal row carpectomy.
-
-
The length of immobilization will vary
from injury to injury, and is based on the experience of the surgeon,
clinical findings, and suitable diagnostic studies.
-
Fractures of the scaphoid treated more than 4 weeks after injury are less successfully treated by cast immobilization.
-
Percutaneous fixation may be a useful technique for fixation of undisplaced fractures.
-
Stable and nondisplaced fractures will
most likely heal with cast immobilization; unstable and displaced
fractures are best treated with some form of internal fixation. -
A gap or fracture offset of 1 mm or greater is considered to be a reliable indicator of instability, and is associated with a higher incidence of nonunion and malunion.P.164
-
Open reduction and internal fixation are indicated in these fractures.
-
-
Internal fixation of the surgeon’s choice
is usually indicated in fractures involving the proximal pole due to
their propensity for delayed and nonunion. -
The initial determination of stability status may not always be correct.
-
Differences of opinion exist regarding
the necessity for immobilization of the thumb and elbow in scaphoid
fractures, and may vary with the experience and preference of the
surgeon.
-
The major blood supply to the scaphoid enters at the dorsal and distal aspect of the bone; based on this fact, palmar or anterior surgical approaches to this bone are favored for management of distal pole and waist fractures.
-
The blood supply to the distal and middle
aspects of the bone is abundant in comparison to the proximal pole
whose blood supply is precarious.-
This poor blood supply is a significant factor in the high rate of nonunion in scaphoid fractures of the proximal pole.
-
-
The palmar approach is recommended for correction of the “humpback” deformity (dorsal angulation and collapse of the scaphoid).
-
The dorsal approach
is preferred for ease of screw placement in proximal pole fractures,
and does not compromise the dorsal blood supply if dissection is
confined to the proximal pole.-
It is also the approach of choice for insertion of vascularized bone grafts.
-
-
The treatment of established nonunion
(including bone graft techniques), the use of electrical stimulation
for delayed or nonunion, and procedures for secondary reconstruction of
nonunion or malunion of the scaphoid is beyond the scope of this
chapter.
-
If untreated, scaphoid nonunions lead to a predictable pattern of arthrosis in the wrist.
-
Scaphoid nonunion may exist with or
without avascular necrosis (AVN) of the proximal aspect of the
scaphoid; if present, AVN lessens the chances of success in
reconstructive procedures. -
Fractures of the waist may collapse, and dorsally angulate to produce the humpback deformity.
-
Four progressive stages of scaphoid nonunion and advanced collapse
(SNAC) have been identified: (1) arthritis of the radial styloid, (2)
spread of the arthritis to include the scaphoid fossa of the radius,
(3) the addition of capitolunate arthritis, and (4) diffuse carpal
arthritis.
fractures exclusive of the scaphoid. Two types have been identified:
dorsal rim chip fractures (the most common) and fractures of the body.
injuries may be due to avulsion of the conjoined insertion of the
dorsal radiocarpal (dorsal radiotriquetral) and dorsal intercarpal
ligaments during hyperflexion and radial deviation of the wrist, or due
to impaction from the ulnar styloid or hamate during axial loading and
hyperextension of the wrist.
to the ulnar aspect of the wrist, which results in a medial tuberosity
fracture. Triquetral fractures are often associated with other carpal
injuries such as a perilunate dislocation. An anteroposterior crushing
injury may result in sagittal fracture. Lunate or perilunate
dislocation may cause proximal pole fracture, as the palmar
lunotriquetral ligament avulses the proximal pole of the triquetrum.
Transverse fractures are usually the result of shear force, and often
are associated with scaphoid fractures.
-
Small nondisplaced or even displaced chip
fractures are usually treated symptomatically with a short period of
immobilization as needed. -
Larger chip fractures, due to their potential for nonunion or instability if untreated, are immobilized in a cast.
-
Open reduction and fixation may be
required to restore the insertions of the DRC and DIC ligaments to
prevent persistent pain and instability that is sometimes seen in
injuries with larger fragments. -
Fractures of the triquetral body or
palmar radial fractures are usually minimally displaced, and are
treated by cast immobilization—but they may be associated with
lunotriquetral or other ligament tears. -
Palmar radial fractures have been
associated with volar intercalated segment instability (VISI) collapse,
and may warrant fixation and repair or reconstruction of the
lunotriquetral ligament complex.
nonscaphoid fracture. Five types have been identified, including
vertical transarticular (the most common), horizontal, dorsoradial
tuberosity, anteromedial ridge, and comminuted. Fractures of the
trapezium often occur in combination with thumb metacarpal or distal
radius fractures.
longitudinal axial force transmitted by the thumb metacarpal.
Horizontal fractures are due to direct shearing forces, and dorsoradial
fractures are the result of vertical shearing as the metacarpal impacts
the trapezium into the radial styloid. An object held in the web space
(such as the handlebars of a bicycle or motorcycle) may produce a
similar injury. Anteromedial ridge fractures result from an
anteroposterior force that
flattens
the transverse carpal arch and causes an avulsion through the
transverse carpal ligament of the anteromedial ridge. This fracture may
occur in conjunction with a fracture of the hook process of the hamate.
-
Displaced intra-articular fractures are
best treated by open reduction and fixation, but most other fractures
are treated by 4 to 6 weeks of cast immobilization. -
The articulation with the adjacent thumb
metacarpal is very critical for thumb function, and post-injury
arthrosis may be avoided by anatomic reduction of intra-articular
fractures.
sports such as golf, baseball, or tennis. Fracture of the hamate hook
presents with pain (and often, point tenderness) distal and radial to
the pisiform. Nonunion and the resultant irregularity of the fracture
interface may cause attritional rupture of the flexors, and this loss
of flexion in the little and ring fingers may be the presenting
complaint (Figure 11.1-6).
involve the hook process and the body of the hamate. Hook fractures may
involve the tip, waist, or base. Fractures of the body may involve the
proximal pole, medial tuberosity, or (in the body), be oriented in the
sagittal oblique plane or dorsal coronal plane.
or from repetitive impacts that may cause a stress fracture. An
avulsion fracture may occur by means of traction from the FCU tendon
and its extension through the pisohamate ligament. A crush injury in
the AP plane may result in an avulsion–type
fracture mediated through the transverse carpal ligament. Fractures of
the body of the hamate may result from direct blows to the ulnar aspect
of the hand (medial tuberosity fracture), anteroposterior crush injury
(sagittal oblique fracture), or carpometacarpal dislocation of the ring
and little fingers that results in a dorsal coronal fracture.
 |
|
Figure 11.1-6 Attritional rupture of flexor tendons due to fracture of the hook process of hamate. A. Loss of flexion in the left little finger. B. Fracture of the base of the hook process (open arrows) and frayed margin (solid arrow) of the flexor tendon.
|
-
Hook fractures may be treated based on location, degree of displacement, and time from injury.
-
Recent nondisplaced fractures, regardless
of location, may be treated with immobilization, with the wrist in
radial deviation to lessen the possible deforming force of the ulnar
finger flexors. -
Displaced avulsion fractures that involve only the superficial tip of the hook may be treated symptomatically.
-
The fragment may be excised if it remains symptomatic after several weeks.
-
-
Fractures of the waist or base of the
hook may be excised. Some surgeons advise preservation of the hook by
means of ORIF and bone grafting, believing that the hook is important
as a mechanical pulley that maintains flexor tendon function. -
Nondisplaced body fractures may be
treated by cast immobilization, but displaced fractures, especially
those seen with metacarpal subluxation or instability, should be
anatomically reduced and fixed. -
The motor branch of the ulnar nerve courses around the base of the hook process, and is at risk during surgery in this region.
Twenty percent of lunate bones are vascularized by a single palmar
supply, and in the remaining 80%, the vascular supply arises from both
palmar and dorsal vessels that anastomose in the body of the lunate.
are based on their location and vascular supply: (1) palmar pole
fractures (the most common) affecting the palmar nutrient artery, (2)
osteochondral (chip) fractures of the proximal articular surface but
not affecting vascularity, (3) dorsal pole fractures possibly affecting
the dorsal nutrient artery, (4) sagittal-oblique fractures through the
body, and (5) coronal split of the body.
-
Type I palmar pole fractures are due to
wrist hyperextension and compression from the capitate and radius,
combined with tension on the radiolunate and lunotriquetral ligaments.
The palmar pole is avulsed by the lunotriquetral ligaments, and this
may produce flexion of the lunate. -
Type II osteochondral fractures may occur
following shear-related injuries, as seen in lunate dislocations,
subluxations, or in patients with Kienbock’s disease. -
Type III dorsal pole fractures result
from shear forces in perilunate dislocations (as the capitate displaces
dorsally) or from avulsion of the scapholunate ligament in acute
rotatory subluxation of the scaphoid. -
Type IV sagittal-oblique fractures
between the proximal and distal articular surfaces result from shear
forces produced by radiocarpal fracture-dislocation. -
Type V coronal fractures result from
wrist hyperextension, which produces tension on the short radiolunate
ligament that avulses the palmar pole. This fracture may also be seen
following a palmar perilunate dislocation of the capitate.
-
Most lunate fractures require surgical treatment based on the fracture and its associated ligamentous injury.
-
Type I fractures may require correction of a lunate rotatory component if present.
-
Type II injuries may require debridement if symptomatic. The specific treatment recommendations are outlined above.
-
Type III fractures associated with acute
scapholunate dissociation may require operative stabilization of the
scapholunate joint. -
Type IV fractures that are displaced require fixation.
-
Type V fractures may require surgical
intervention, depending on the degree of displacement and the
associated carpal instability. -
Kienbock’s disease of the lunate should be considered in the absence of significant trauma.
have been identified: transverse (the most common), parasagittal,
comminuted, and pisotriquetral impaction.
impaction on the pisiform, with the wrist extended. Active contraction
of the FCU muscle-tendon unit may play a role in separation of the
fracture interface. Incongruity of the pisiform may result in
pisotriquetral incongruity and degenerative arthritis. As well, a
shearing injury may result in intra-articular loose bodies, which may
remain symptomatic.
-
Most fractures may be treated with immobilization, with the expectation that union or fibrous union will occur.
-
Wide separation of the fragments may indicate some degree of discontinuity of the FCU, and may be an indication for exploration.
-
Some surgeons prefer to excise widely
separated or comminuted fractures and restore the integrity of the FCU
by suture techniques of their choice. -
Parasagittal and comminuted fractures, as
well as pisotriquetral impaction conditions (if symptomatic) may be
treated by pisiform excision.
difficult to treat due to the fact that the proximal pole is entirely
intra-articular and without soft-tissue attachment. AVN is likely if
the fracture is displaced. Four fracture types have been reported:
transverse fracture of the body (the most common), transverse fracture
of the proximal pole, and coronal oblique and parasagittal fractures.
the hyperextended wrist, which forces the capitate against the dorsal
edge of the radius. This mechanism of injury may also produce a
concomitant fracture of the scaphoid, and is called the scaphocapitate fracture syndrome.
The scaphoid fracture may be the only injury evident on the initial
radiographs, and the wise examiner will look for clinical evidence of
injury to the capitate in addition to the scaphoid injury. Types III
and IV usually result from hyperextension and axial loading injuries.
-
CT is often required to make the diagnosis. MRI is used to evaluate the vascularity of the proximal pole.
-
The treatment of capitate fractures
requires prompt diagnosis and stabilization. If diagnosed early and it
is nondisplaced, cast immobilization may be used. -
If the fracture is displaced or part of scaphocapitate fracture syndrome, open reduction and internal fixation is indicated.
-
Vascularity of the proximal pole may be evaluated intraoperatively.
-
-
Restoration of distal carpal row height,
anatomic reduction, and careful evaluation for associated injuries are
the primary goals of treatment.
|
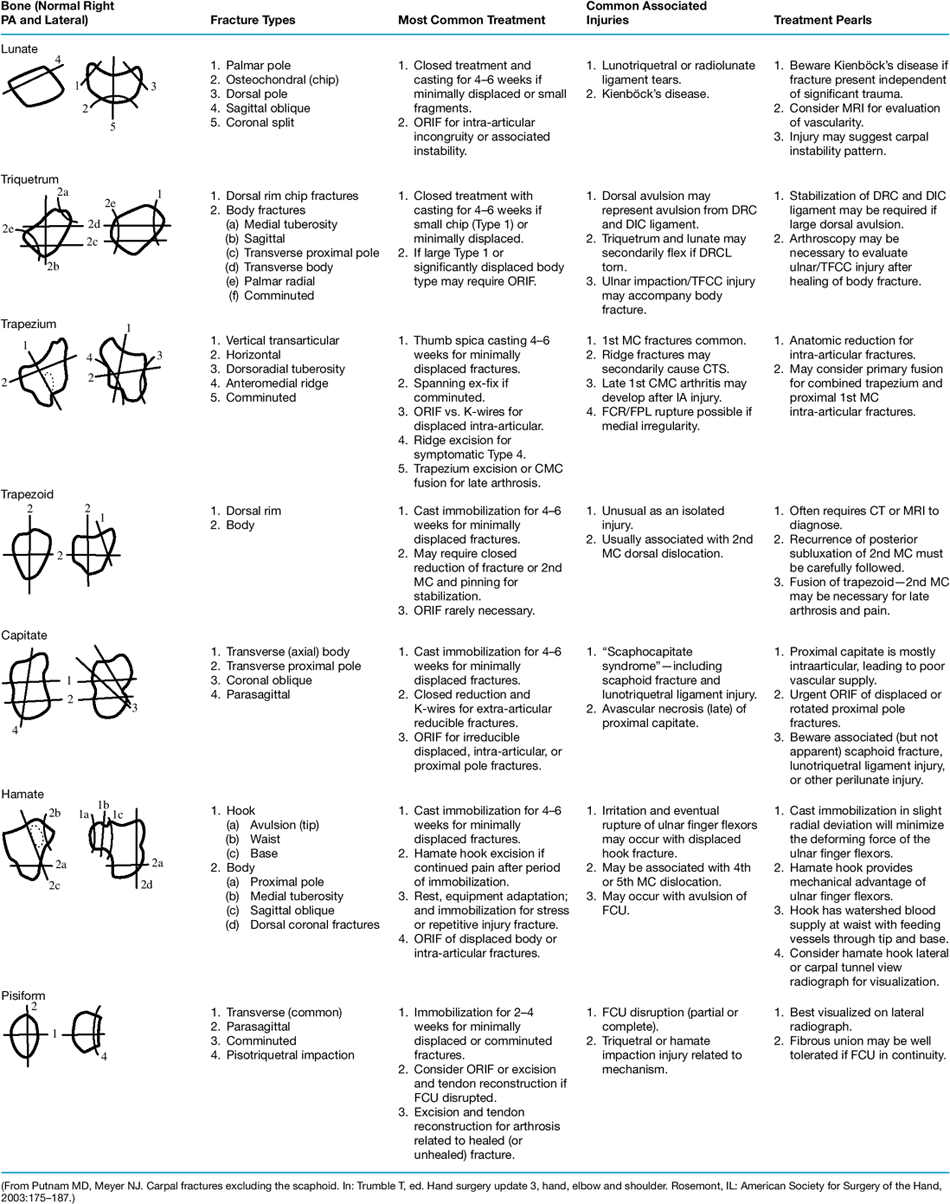
Table 11.1-1 Summary of Carpal Fractures Exclusive of the Scaphoid
|
|
|---|---|
|
vascularity. This in turn may lead to distal-row collapse, scaphoid
rotatory subluxation, and progressive carpal arthritis with persistent
pain and stiffness.
bone. Trapezoid fractures rarely occur alone, and are usually
associated with fracture-dislocations involving dislocation of the
index metacarpal or the trapezoid itself. Diagnosis may be aided by CT
or MRI, since radiographs may not show the fracture. Two types have
been identified; they include fractures of the dorsal rim and body.
force along the index metacarpal. These fractures are often difficult
to identify on plain films, and thus require a high index of suspicion.
As noted above, a CT scan or MRI will best characterize this fracture.
-
Minimally displaced trapezoid fractures
are treated with cast immobilization for 4 to 6 weeks, but displaced
fractures may require ORIF or closed reduction and immobilization. -
Osteonecrosis may occur in the trapezoid
due to its poor blood supply. Trapezoid-index metacarpal arthrodesis
may be indicated for late arthrosis. -
Table 11.1-1
depicts the fracture type, treatment, associated injuries, and
treatment “PEARLS,” and is reproduced with permission of the authors
and publisher.