Agnosia, Apraxia, and Related Disorders of Higher Cortical Function
– Mental Status Examination and Higher Cortical Functions > Chapter
7 – Agnosia, Apraxia, and Related Disorders of Higher Cortical Function
knowledge) refers to the higher synthesis of sensory impulses, with
resulting perception, appreciation, and recognition of stimuli. Agnosia
refers to the loss or impairment of the ability to know or recognize
the meaning or import of a sensory stimulus, even though it has been
perceived. Agnosia occurs in the absence of any impairment of
cognition, attention, or alertness. The patients are not aphasic and do
not have word finding or a generalized naming impairment.
Hughlings-Jackson saw agnosia as a non-language form of aphasia.
Agnosias are usually specific for a given sensory modality and can
occur with any type of sensory stimulus. Agnosias that involve the
primary sensory modalities may represent disconnection syndromes that
disrupt communication between a specific cortical sensory area and the
language areas, causing a restricted anomia. Tactile agnosia refers to
the inability to recognize stimuli by feel, visual agnosia the
inability to recognize visually, and auditory (acoustic) agnosia the
inability to know or recognize by audition. Body-image agnosia
(autotopagnosia) is loss or impairment of the ability to name and
recognize body parts. Finger agnosia is a type of autotopagnosia
involving the fingers. Auditory agnosia is the loss of recognition of
sounds; phonagnosia is the loss of recognition of familiar voices. Time
agnosia refers to loss of time sense without disorientation in other
spheres. Visuospatial agnosia is loss or impairment in the ability to
judge direction, distance, and motion and to understand three
dimensional spatial relationships. Because of the impaired spatial
judgment and visual disorientation, the patient cannot find his way in
familiar surroundings. Multimodal agnosias may occur with dysfunction
of the association areas in the parietal and temporal lobes that
assimilate sensory information from more than one domain.
to recognize and identify an object by touch despite intact primary
sensory modalities. There is no loss of perceptual ability. The patient
can feel the object, sensing its dimensions, texture, and other
relevant information. However, he is unable to synthesize this
information and correlate it with past experience and stored
information about similar objects in order to recognize and identify
it. Stereognosis is tested by asking the patient to identify, with eyes
closed, common objects placed into their hand (coin, key, button,
safety pin, paper clip). The most convincing deficit is when the
patient is able to identify with the other hand an object they were
unable to identify with the tested hand. When primary sensory
modalities in the hand are impaired, as by radiculopathy or neuropathy,
failure to identify an object by touch is not astereognosis.
Astereognosis usually indicates a lesion involving the contralateral
parietal lobe. Rarely, a lesion of either parietal lobe can produce
astereognosis bilaterally. It has also
been
reported to occur with lesions involving the anterior corpus callosum
and the thalamic radiations. If there is hand weakness, the examiner
may hold and move the object between the patient’s fingers. It is
striking to see a patient with a paralyzed hand from a pure motor
capsular stroke demonstrate exquisitely intact stereognosis when tested
in this fashion. In tactile agnosia, the patient is unable to identify
the object with either hand, but can identify it visually.
Graphesthesia is a similar function. It is tested by writing numbers on
the patient’s palm or fingertips. The inability to recognize the
numbers is referred to as agraphesthesia; in the presence of intact
primary sensory modalities, it usually indicates a lesion involving the
contralateral parietal lobe.
ability to recognize, name, or select individual fingers of the
patient’s own hands or the hands of the examiner. The patient loses the
ability to name individual fingers, point to fingers named by the
examiner, or move named fingers on request, in the absence of any other
naming deficit. Testing for finger agnosia may be conveniently combined
with assessment of right-left orientation. The simplest test of
right-left orientation is to ask the patient to raise a specific hand.
More challenging is to have the patient touch a body part on one side,
e.g., the right ear, with a specific digit of the other side, e.g., the
left thumb. Even more strenuous is when the examiner faces the patient,
crosses his forearms with hands and fingers extended, and requests the
patient to touch one of the examiner’s fingers on a specific side, e.g,
the left index. A very challenging test is to ask the patient to touch
a specific finger as the examiner faces away from the patient with
forearms crossed behind his back, using a confusing syntax, e.g., “with
your left hand touch my right index finger.” Finger agnosia and
right-left confusion, along with agraphia and acalculia, make up
Gerstmann syndrome. Finger agnosia alone is not highly localizing, but
when all components of the syndrome are present the lesion is likely to
lie in the region of the dominant angular gyrus.
the ability to recognize things visually, despite intact vision
(psychic blindness or mindblindness). Areas 18 and 19 are particularly
important for visual gnostic functions. Visual agnosia is not a sensory
defect but a problem in recognition. There is impairment in the higher
visual association processes necessary for recognition and naming, not
explicable by any deficit in visual perception. Patients can see but
cannot make sense of the visual world. Teuber said visual agnosia was a
“percept stripped of its meaning.” Oliver Sacks provided an
entertaining and informative description of the clinical picture of
visual agnosia in The Man Who Mistook His Wife For a Hat (Touchstone Books, 1985).
visual cortex, cause color blindness (central achromatopsia). Lesions
of the association areas may cause color agnosia. In color agnosia, the
patient cannot name or identify colors, although he is not color blind
and can discern the numbers on color plates. Patients may not be able
to remember the color of common things, e.g., the sky. In prosopagnosia
(face or facial agnosia, face blindness), there is an inability to
recognize familiar faces. The patient may not be able to identify
people by looking at their faces, even close family members, but may
immediately identify the person by the sound of their voice. The
patient may recognize a face as a face but cannot associate it with a
particular individual. They learn to identify people using other cues.
In extreme examples, the patient is unable to recognize himself in a
mirror or photograph. Patients with prosopagnosia, and other visual
agnosias, usually have bilateral lesions of the occipitotemporal area
involving the lingual, fusiform, and parahippocampal gyri.
Prosopagnosia can occur with unilateral right posterior hemispheric
lesions.
is the inability to carry out on request a high-level, familiar,
purposeful motor act in the absence of any weakness, sensory loss, or
other deficit involving the affected part. The patient must have intact
comprehension and be cooperative and attentive to the task. Another
definition of apraxia is the inability to perform an act on command
that the patient is able to perform spontaneously. There are many
varieties of apraxia. The ones seen most often are ideomotor,
buccofacial, constructional, and dressing apraxia. Some of the other
apraxias include apraxia of eyelid opening, eyelid closure, gaze, and
gait.
probably should not exist. These patients have difficulty with fine
motor control. They typically have very mild lesions involving the
corticospinal tract that are not severe enough to cause detectable
weakness, but are severe enough to impair coordination and dexterity.
Limb kinetic apraxia is due to dysfunction of the primary motor
pathways. In other forms of apraxia the primary motor and sensory
cortical areas are intact.
perform a complex command (salute, wave goodbye, snap the fingers, make
a fist, show how to hitchhike) with the involved extremity, sometimes
with either extremity. The patient may be unable to pantomime how to
use common implements (hammer, toothbrush, comb) or how to kick or
throw a ball. They may substitute a hand or finger for the imagined
object, e.g., raking the fingers through the hair instead of showing
how to use a comb, snapping fingers together as the blades when asked
to show how to use scissors. The patient may be unable to carry out the
act on command but be able to imitate it. Rarely, the patient may be
unable to carry out an act on command or imitation, such as showing how
to use a comb, but be able to use the actual object. In ideomotor
apraxia, there may be a disconnection between the language or visual
centers that understand the command and the motor areas tasked with
carrying it out. Patients may have apraxia for whole body movements.
They are unable to, on command, do such things as stand up, take a bow,
or stand like a boxer.
perform a complex motor act with the non-paretic limb in the presence
of a unilateral dominant hemisphere lesion. For instance, a patient
with a left hemisphere lesion causing Broca aphasia may be unable to
show how to wave goodbye using the left hand. This is because the
fibers connecting the language areas of the left hemisphere with the
motor areas of the right hemisphere are disrupted. The patient
understands the request, has no weakness of the left hand, but is
unable to execute because the right hemisphere never receives the
command.
to carry out individual components of a complex motor act, but cannot
perform the entire sequence properly. Patients may perform each step
correctly, but in attempting the sequence they omit steps or get the
steps out of order. Ideational apraxia seems to be an impairment in
conceptualizing the overall goal of the activity sequence or an
inability to plan the series of steps. For instance, in showing how to
drive a car, the patient might try to put the car in drive before
starting the engine. When asked to demonstrate how to mail a letter,
the patient may seal the envelope before inserting the letter, or mail
the letter before affixing the stamp. Ideational apraxia may occur with
damage to the left posterior temporoparietal junction or in patients
with generalized cognitive impairment.
on request complex acts involving the lips, mouth, and face, such as
whistling, coughing, pursing the lips, sticking out the tongue, or
blowing a kiss or pantomime blowing out a match or sniffing a flower.
There is no weakness of the mouth, lips, or face, but the patient is
unable to make the requested movement. The patient may spontaneously
lick his lips, but is unable to do so on command. Apraxia of such
midline functions is common in patients with lesions involving either
hemisphere. Failure to execute such acts should not necessarily be
construed as evidence of impaired comprehension in aphasic patients.
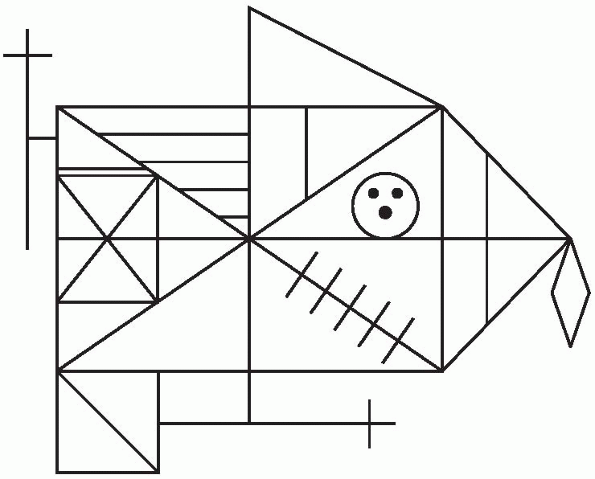
constructional. Constructional or dressing apraxia may occur with
parietal lobe lesions which interfere with the patient’s ability to
comprehend spatial relationships. In constructional apraxia, the
patient is unable to copy geometric forms of any complexity because of
impaired visuospatial skills. They may be able to draw a square but not
a three dimensional cube. They may be able to draw individual shapes,
but cannot synthesize them into a more complex geometric figure, e.g.,
a square with a triangle perched on its upper right corner and a circle
attached to the lower right corner, all touching. The patient may also
be asked to draw actual things, such as a three dimensional house with
a roof and chimney, a clock, or a daisy. Patients with hemineglect may
fail to put petals on one side of the daisy. A test
for
both praxis and cognition is to have the patient draw a clock face,
insert the numbers, and draw the hands at a specific time, e.g., 3:10,
or “10 minutes past 3).” Patients with hemineglect may fail to put the
numbers on one side of the clock. Patients with frontal lobe
dysfunction or a confusional state may have a disorganized and confused
approach to the task, making multiple errors. A patient with cognitive
impairment may forget the proper arrangement of numbers or how to
indicate a specific time. Some patients cannot interpret 3:10 and will
put one hand on the 10 and the other on the 3, indicating 2:50 or
10:15. The Rey-Osterrieth figure is very complex and can bring out
subtle constructional apraxia (Fig. 7.1).
Constructional tasks are particularly useful for differentiating
psychiatric from neurologic disease. Impaired constructional ability is
a sensitive indicator of lesions involving various parts of the brain,
but in patients with psychiatric disease constructional ability is
preserved.
 |
|
FIGURE 7.1 • The Rey-Osterrieth Complex Figure for evaluating constructional ability.
|
don clothing correctly. There is loss of the ability to manipulate the
clothing in space and to understand its three dimensional
relationships. Patients with hemineglect may fail to dress one side of
the body. A useful test for dressing apraxia is to turn one sleeve of
the hospital gown or robe inside out, then have the patient try to put
it on. Patients with dressing apraxia are often baffled. Dressing
apraxia can be particularly disabling, as the patient struggles for a
long period of time each morning simply to get dressed. Constructional
apraxia would be very disabling for a patient who was an artist or
craftsman.
tracts that interconnect primary cortical areas are disrupted, with
preservation of the cortical areas of origin. Neurologic dysfunction
occurs not because of destruction of cortex but because of defects in
intrahemispheric or interhemispheric communication. Some of the
disconnection syndromes include alexia without agraphia, ideomotor
apraxia, sympathetic apraxia, pure word deafness, conduction aphasia,
and the transcortical aphasias. The modality specific agnosias may be
disconnection syndromes in which the primary sensory area for a given
modality is disconnected from the language and memory areas of the
brain
that are responsible for recognition and naming. Disconnection
syndromes may result from any process that disrupts subcortical white
matter, including infarction, hemorrhage, neoplasm, and trauma.
in patients with altered mental status and other diffuse cerebral
disturbances, there may be selective defects of attention in patients
with focal cerebral lesions. These are seen primarily in right handed
patients with right (non-dominant) hemisphere lesions, especially those
that involve the inferior parietal lobule. A variety of terms have been
used to describe the phenomenon: extinction, neglect, hemi-neglect,
hemi-inattention, denial, spatial inattention. Hemi-attention may be
modality specific. The mildest manifestation of a right parietal lesion
is extinction of the contralateral stimulus with double simultaneous
stimulation on visual field or somatosensory testing. Although primary
sensory modalities are intact, when touched simultaneously on both
sides the patient fails to appreciate the stimulus on the involved side
or fails to see the stimulus in the involved visual hemifield. Patients
with multimodal hemineglect may extinguish all types of contralesional
stimuli, and may completely ignore the left side of space. On the line
bisection test they fail to see the left half of the line. They bisect
the right half, drawing their vertical tick about one-quarter of the
way down the line from the right. If lines are drawn all over the page,
the patient may fail to bisect any of the lines on the left. When
presented with a complex drawing, such as the cookie theft picture,
they may describe what is taking place on the right side of the
picture, but fail to notice the cookie theft happening on the left. In
motor neglect (hemiakinesia), all of the patient’s motor activities are
directed to one side of space.
refer to a patient’s lack of awareness of their neurologic deficit. It
occurs particularly in patients with non-dominant parietal lesions. It
is not uncommon to see patients with a right parietal infarction on
imaging studies but no clinical history of the event, in part due to
this lack of recognition of deficits involving the left side of the
body. Occasional patients with severe left hemiplegia may deny there is
anything wrong with the involved limbs. Even when the examiner dangles
the patient’s paralyzed left hand before his face and asks if there is
anything wrong with this hand, the patient may deny it. The most severe
form of anosognosia is when the patient denies owning the hand
(asomatognosia). Occasional patients become belligerent in denying that
the hand dangling before them is theirs. They commonly say the hand
belongs to the examiner. Patients with anosognosia may refuse to remain
in the bed with this “other person.”
large right hemisphere strokes causing severe left hemisensory loss and
left spatial neglect. Anosognosia for the hemiplegia may result from
impaired proprioceptive mechanisms that leave the patient unaware of
the position and movement of the affected limbs. Anosognosia for
hemiplegia has also been reported with pontine lesions. Patients may
deny or neglect other neurologic deficits as well, particularly loss of
vision due to bilateral occipital lobe lesions (cortical blindness,
Anton syndrome).
