Thoracic and Lumbar Trauma
spinal injuries. Most of these injuries occur in males (15 to 29 years
old) usually as the result of significant force impact, such as motor
vehicle accidents. Most injuries (52%) occur between T11 and L1,
followed by L1-5 (32%) and T1-10 (16%). Depending on the type of
fracture, associated injuries occur in 50% of patients mainly as a
result of a distraction force. Associated injuries include
intraabdominal bleeding from liver and splenic injuries, vessel
disruption, and pulmonary injuries (20% of patients). Contiguous and
noncontiguous spine injuries are present in 6% to 15% of patients.
surrounding paraspinal musculature, the vertebral elements, and the
thoracic rib cage. The sternum and the rib cage significantly limit
motion in the thoracic spine. As a result of the significant amount of
force necessary to disrupt the protective enclosure of the thoracic
spinal cord, spinal injuries in this region are associated with a high
incidence of neurologic injury. This high incidence also is a function
of the decreased spinal canal diameter to spinal cord diameter ratio,
particularly between T2 and T10. High-energy injuries in this area
usually result in a 6:1 ratio of complete to incomplete neural
deficits. The physiologic kyphosis of the thoracic spine may predispose
it to flexion/axial load injuries.
between the less mobile thoracic spine and the more flexible lumbar
spine. In this junctional region, the rib cage no longer provides
protection and support to the vertebral column. Also, the thoracic
vertebral bodies are not as large as the lumbar vertebral bodies; they
are less able to resist deformity after specific load applications.
These factors render the thoracolumbar junction more vulnerable to
injury and make it the most common location for burst-type fractures.
breathing, circulation) of trauma care. A cervical collar should be
placed and any extremity injuries splinted when the airway is secured.
The patient now can be logrolled carefully, and the spine can be
palpated for tenderness, step-offs, swelling, or visual deformities. Of
patients with persistent localized tenderness after trauma to the
thoracolumbar spine and absence of an obvious radiographic deformity,
30% may have an occult spinal fracture.
testing, dermatomal sensory testing, lumbar and sacral root motor
evaluation, and examination of reflexes. Spinal shock
refers to flaccid paralysis due to a physiologic disruption of all
spinal cord function. The presence of the bulbocavernosus reflex
heralds the end of spinal shock and allows for an accurate assessment
of the patient’s neurologic status typically 48 hours after the injury.
The bulbocavernosus reflex is tested by squeezing the glans penis or
clitoris and observing for reflex anal sphincter contracture. It also
may be tested by tugging on an indwelling catheter and observing for an
“anal wink.”
is marked by a total absence of sensory and motor function below the
anatomic level of injury in the absence of spinal shock. In an incomplete
lesion, residual spinal cord or nerve root function exists below the
anatomic level of injury. An incomplete spinal cord lesion may manifest
as one of four syndromes (Table 5-1).
must be reversed through fluid or blood replacement, with or without
the use of vasopressors. Intravenous methylprednisolone is administered
routinely within 8 hours of a spinal cord injury in the absence of
specific contraindications (Table 5-2).
of intermittent external pneumatic compression devices, static
compression stockings, and, in select patients, subcutaneous (5000 U
subcutaneously every 12 hours) or intravenous low-molecular-weight
heparin helps to minimize potentially fatal pulmonary emboli.
posterior vertebral body line should be assessed on the lateral
radiograph. Disruption of this line may signal spinal canal compromise
from a burst-type fracture. Other radiologic signs suggesting a
compression spinal injury include buckling of the cortical margins,
loss of vertebral body height, and an intravertebral vacuum sign. If
the cervicothoracic junction (C7-T1) is difficult to visualize, a
swimmer’s view (lateral view with a maximally abducted arm) or an
oblique view may help define the vertebral anatomy.
|
TABLE 5-1 SPINAL CORD INJURY SYNDROMES
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
anteroposterior view. Vertebral body cortical disruption may suggest a
lateral compression fracture. The spinous processes should be in the
midline with a relatively consistent interpedicular distance.
Displacement (i.e., spreading) may represent significant posterior
element injury and spinal instability.
may require the use of computed tomography (CT) or magnetic resonance
imaging (MRI). CT is useful in evaluating the integrity of the middle
(posterior vertebral body) and posterior (posterior elements) columns
of the vertebral body. On plain radiographs, approximately 25% of burst
fractures may be misdiagnosed as stable compression fractures owing to
lack of clear visualization of the vertebral bony anatomy. The greatest
disadvantage of CT is its limited sensitivity in showing consistently
specific soft tissue injuries (disc herniation, epidural hematoma,
ligamentous disruption, or spinal cord injury) (Table 5-3).
|
TABLE 5-2 METHYLPREDNISOLONE DOSING
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
structures of the spine is necessary. MRI is the definitive diagnostic
modality in the evaluation of spinal cord injury. It is extremely
useful in all cases with neurologic deficit to assess for intrinsic and
extrinsic spinal cord pathology. MRI can help illustrate and elucidate
the various spinal cord parenchymal findings, such as edema, hematoma,
and physical transection of the neural elements.
cord with increased signal intensity on T2-weighted images. Hematoma is
characterized by decreased signal intensity on T2-weighted images
acutely and often is surrounded by a halo of T2-weighted enhancement
from adjacent edema. Edema extending more than two vertebral levels and
the presence of hematoma within the spinal cord are considered poor
prognostic signs for potential functional motor recovery.
“black stripe sign” may indicate disruption of the posterior
longitudinal ligament or supraspinous ligament. A bright signal within
the substance of the interspinous space reliably represents ligamentous
injury. MRI is helpful in the evaluation of acute traumatic disc
disruptions, especially in the setting of a facet dislocation. MRI also
may be useful in the postinjury period in cases of late development or
worsening of a preexisting neurologic injury. In these situations, a
treatable posttraumatic cyst or syrinx often can be diagnosed.
is used commonly to define vertebral column injuries. The anatomic
spine in this system is divided into three columns. Denis divided
thoracic and lumbar spinal injuries into minor and major injuries.
Fractures of the spinous and transverse processes, the pars
interarticularis, and the facet articulations were categorized as minor
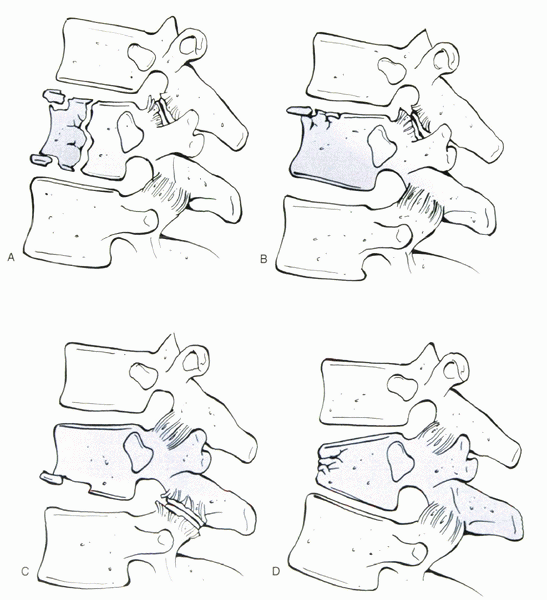
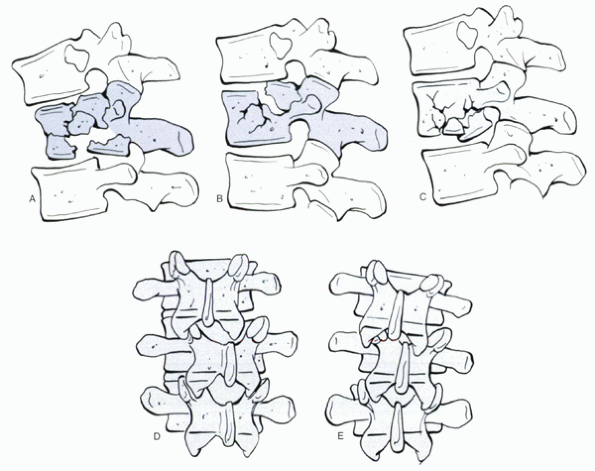
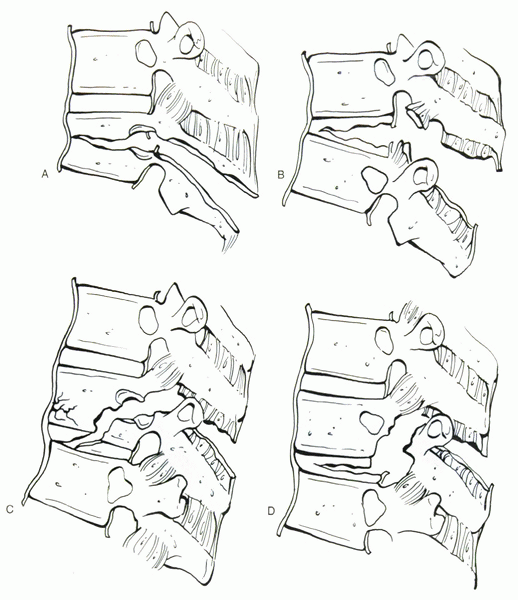
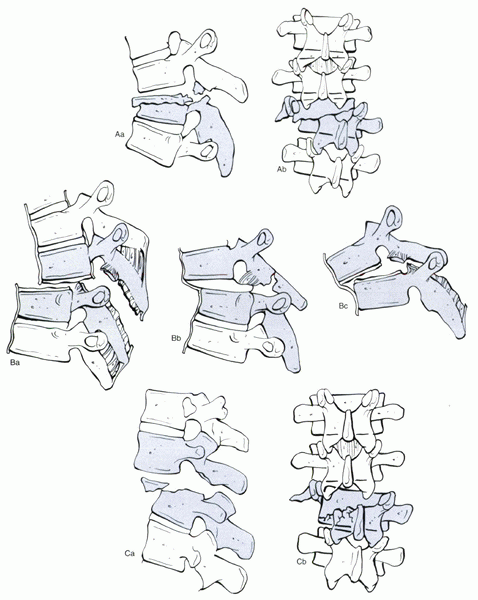
injuries. Major spinal injuries were divided into compression
fractures, burst fractures, flexion/distraction injuries, and
fracture-dislocations (Figs. 5-1, 5-2, 5-3 and 5-4).
Their system included six fracture types based on the failure mode of
the middle column: wedge-compression, stable burst, unstable burst,
Chance, flexion/distraction, and translational fractures (Table 5-4).
classification of thoracolumbar injuries. They described seven injury
patterns: compressive-flexion, distractive-flexion, lateralflexion,
translational, vertical-compression, and distractive-extension
injuries. This system categorizes injuries by the forces that create
them and is useful in guiding nonoperative and operative treatment
strategies (Table 5-5).
to shorten hospitalization; maximize function; facilitate nursing care;
and prevent deformity, instability, or pain. White and Panjabi defined
clinical instability as the “loss of the ability of the spine under
physiologic loads to maintain relationships between vertebrae in such a
way that there is neither damage nor subsequent irritation to the
spinal cord or nerve roots, and in addition, there is no development of
incapacitating deformity or pain.”
|
TABLE 5-3 DIAGNOSTIC IMAGING MODALITIES
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||
 |
|
Figure 5-1 Denis’s classification of thoracolumbar compression injuries. These fractures may involve both end plates, type A (A); the superior end plate only, type B (B); the inferior end plate only, type C (C); or a buckling of the anterior cortex with both end plates intact, type D (D).
|
 |
|
Figure 5-2 Denis’s classification of thoracolumbar burst fractures. Types A, B, and C represent fractures of both end plates (A), the superior end plate (B), and the inferior end plate (C). Type D fracture is a combination of a type A burst fracture with rotation (D),
which is best appreciated on an anteroposterior radiograph. The superior or inferior end plate, or both, may be involved with this fracture. Type E fractures are burst fractures with lateral translation or flexion (E). |
assessment of the integrity of the posterior osteoligamentous complex.
In a typical burst fracture, if there is marked widening of the
posterior spinous processes with an obvious kyphotic malalignment, this
would be considered an unstable fracture with the potential for
deformity progression. Denis defined instability
as a disruption of two or more of the three spinal columns and
categorized instability into three groups: mechanical, neurologic, and
combined. Mechanical instability included multiple column injuries in
which the posterior elements were disrupted in distraction, and late
kyphosis was a potential. Neurologic instability described a neurologic
deficit in the setting of a spinal fracture. Combined instability
described an unstable mechanical fracture in the setting of a
neurologic deficit.
(decompression and stabilization) is unclear. A critical window of
opportunity (possibly <3 hours) may exist in which the decompression
of extrinsic pressure on the spinal cord and spinal stabilization may
enhance functional neurologic outcome. Vaccaro et al
reported the only controlled, prospective, randomized study on the
timing of surgical intervention in cervical spinal cord injury. The
authors found no significant difference in functional neural recovery
when patients were operated on either early (<3 days) or late (>5
days). Progressive neurologic loss associated with an unstable fracture
pattern with significant spinal cord compression is an indication for
emergent surgical intervention.
 |
|
Figure 5-3 Denis’s classification of flexion/distraction injuries. These may occur at one level through the bone (A), at one level through the ligaments and disc (B), at two levels with the middle column injured through the bone (C), or at two levels with the middle column injured through the ligament and disc (D).
|
spinal injuries with symptomatic neural compression is unclear. Despite
varied opinions, there is no direct correlation between the percentage
of canal occlusion shown radiographically and the severity of
neurologic deficit after burst fractures. Instead the initial force
imparted to the spinal cord or the cauda equina, along with the
associated hematoma, edema, and vascular ischemia perpetuated by
various neurotrophic and vasoactive agents may be the underlying cause
of neurologic injury.
below T12 gain some return of neurologic function with nonoperative
treatment. Neurologic recovery is more predictable, however, following
an anterior decompression in spinal cord compression. Late
decompression, even several years after injury, may enhance neurologic
recovery of the spinal cord, conus medullaris, and cauda equina.
relieving canal compression via ligamentotaxis. This method is
accomplished more efficiently if performed in the early peritrauma
period. Several studies have shown that the spinal canal remodels or
enlarges with time in nonoperatively treated and operatively treated
fractures in a predictable fashion
and experience of the surgeon dictate the choice of surgical approach.
Multiple variations on the approach to the thoracolumbar spine exist
based on three methods to decompress the thecal sac: anterior,
posterior, and posterolateral (Table 5-6).
 |
|
Figure 5-4 Denis’s classification of fracture-dislocations. These injuries may occur at one level through the bone (A), at one level through the ligaments and disc (B), or at two levels with the middle column injured through the ligament and disc (C).
|
|
TABLE 5-4 THE McAFEE CLASSIFICATION SYSTEM
|
|||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 5-5 THE FERGUSON AND ALLEN CLASSIFICATION SYSTEM FOR SPINAL FRACTURES
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
TABLE 5-6 SURGICAL APPROACHES TO SPINAL DECOMPRESSION
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
fixation, there has been progressive development of various spinal
fixation systems based on segmental fixation of the spine. The choice
of spinal implant is determined by the nature, degree, or biomechanics
of the existing instability; the quality (bone density) of the spinal
elements; and the medical condition of the patient.
the spine is through the intact anterior column. Direct restoration of
the load-bearing function of the anterior spine is paramount in
addressing spinal instability secondary to thoracolumbar trauma.
Indications for anterior spinal surgery in patients with thoracolumbar
injuries include unstable fractures requiring anterior column support,
bony or discal compression of the thecal sac in the setting of a
neurologic injury best addressed anteriorly, and unstable fractures
(select burst injuries) that require stabilization best achieved
through an anterior approach to preserve spinal motion segments (Fig. 5-5).
act as a load-sharing device restoring axial stability until
arthrodesis is obtained. With a deficient anterior column and no
structural interbody spacer, a posterior spinal construct bears most of
the axially applied loads leading to the potential for nonunion and
instrument failure.
 |
|
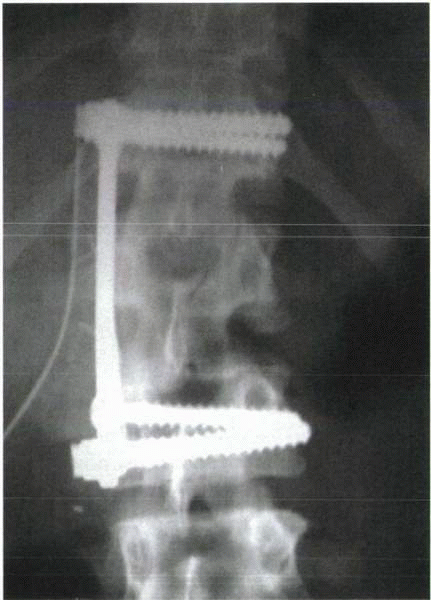
Figure 5-5
Postoperative radiograph after completion of an anterior thoracolumbar decompression and stabilization procedure using autologous iliac crest bone graft and an anterior thoracolumbar plate and screws. |
tricortical iliac crest, although allograft sources, such as a tibial
or femoral shaft or metallic mesh cages, are gaining popularity. Iliac
crest interbody grafts allow for a faster rate of bony incorporation
owing to their biocompatibility than do allograft strut grafts.
Allograft strut grafts are able to withstand greater physiologic loads,
however, in the erect spine in the early reconstruction and healing
period. Several authors have reported successful results using anterior
cortical allograft strut grafts in thoracolumbar fractures with fusion
rates approaching greater than 90% at greater than 5-year follow-up
with minimal graft subsidence and change in sagittal alignment.
crucial to the success of an anterior spinal construct. In the presence
of posterior ligamentous injury, an anterior stand-alone procedure
using a structural interbody graft followed by adjunctive internal
fixation (i.e., a dual rod or plating fixation device) may be adequate
in restoring enough stability until bone healing occurs. If significant
posterior instability still exists, however, a staged posterior
stabilization procedure should be done.
by reconstruction are technically demanding procedures not without
significant potential complications. Vascular complication rates of
5.8% have been reported, accompanied by a 2.4% rate of deep venous
thrombosis and a 10% rate of dural laceration.
realignment of the spine, direct and indirect decompression of the
neural elements, and protection against late deformity and instability
through the application of spinal instrumentation and subsequent
fusion. Posterior spinal instrumentation allows for application of
specific vector forces to the spine to correct or improve spinal
alignment. The most commonly applied vector forces are cantilever
bending and distraction. With a prudent distraction force, restoration
of vertebral body height and partial clearance of bone or discal
fragments from within the spinal canal by ligamentotaxis can be
achieved. Spinal canal clearance through ligamentotaxis optimally is
achieved within the first 2 to 3 days after injury. Posterior
distraction techniques may enlarge the compromised canal 40% to 75%.
(rod) reduces the risk of terminal implant cutout or dislodgment by
increasing the distance from the fracture site, decreasing the forces
on the hook. Especially with hook-based systems, this often requires
the immobilization of five or six motion segments that may contribute
to increased global spinal stiffness and subsequent junctional
degeneration. Historically, in an attempt to preserve the motion of
uninjured motion segments, the “rod long-fuse short” technique was
introduced. With this method, only one level above and one level below
the fracture were fused, and three levels above and below the injury
were spanned by instrumentation, which was removed at 1 year after
surgery. This technique eventually lost popularity as gross and
histologic findings of osteoarthritis were noted along the unfused
but instrumented spinal segments at the time of implant removal.
fracture reduction and stabilization include hook dislodgment, late
vertebral collapse, and progressive kyphosis after rod removal.
Overdistraction with long rods may lead to iatrogenic loss of lumbar
lordosis and the development of a painful flat back deformity. Various
modifications of hook-rod constructs were initiated to address these
issues. More square hooks, which prevented rod rotation, allowed for
gentle contouring of the rod and as such decreased hook cutout. Edward
sleeves, made of high-density polyethylene, which were placed along the
rod, were developed to provide an anterior vector moment to the spine
through three-point or four-point bending strategies.
additional method of stabilizing an unstable three-column spinal injury
through three-column bone fixation. Pedicle screw implants potentially,
in nonosteoporotic patients, allow for shorter posterior fixation
lengths, while conferring adequate spinal stability. Experimental data
confirmed that short-segment pedicle screw constructs provide
torsional, flexural, and compressive rigidity comparable to longer
hook-rod constructs. Despite the increased rigidity of pedicle screw
systems, posterior short-segment fixation of unstable thoracolumbar
fractures has resulted in high failure rates.
screw fixation (one level above and one level below the fracture level)
seem to be patients with flexion/distraction injuries or lower lumbar
burst fractures in which the weight-bearing line is posterior to the
posterior vertebral body wall. Transpedicular intracorporeal grafting
combined with short-segment instrumentation has been offered as an
alternative to a staged anterior column reconstruction procedure. This
technique has not been shown to decrease the incidence of loss of
sagittal plane alignment or instrumentation failure, however, compared
with nonintracorporeal grafted cases at long-term follow-up.
based on their biomechanical and anatomic characteristics and the
patient’s neurologic status (Table 5-7).
process fractures resulting from direct trauma or severe muscular
contractions may be treated symptomatically with or without a brace for
comfort. The importance of assessing for spinal stability after an
initial immobilization period, if deemed necessary, with
flexion/extension plain radiographs cannot be overemphasized. Care must
be taken to avoid undertreatment and missing a potentially unstable
spinal injury. An acute isolated fracture of the pars interarticularis
should be immobilized in a well-molded total contact thoracolumbosacral
orthosis. If the fracture is below L3, a unilateral thigh extension
usually is recommended.
(wedge) fractures if there is greater than 20 to 30 degrees of initial
kyphosis (significant posterior osteoligamentous disruption) and
greater than 50% loss of anterior vertebral body height (Fig. 5-6).
Ferguson-Allen type I compressive flexion injuries typically can be
treated with an extension cast or orthosis and early ambulation. If the
fracture is proximal to T7, a cervical extension to the brace or cast
is recommended. Type II and type III compressive flexion injuries
without a neurologic deficit generally are stabilized with posterior
nonsegmental or segmental instrumentation. Ferguson-Allen type II
compressive flexion injuries at the thoracolumbar junction often are
treated with posterior compression instrumentation, with the intact
middle column being used as a hinge to restore lordosis. Type III
injuries (which are burst fractures) without significant canal
compromise and evidence of significant posterior osteoligamentous
disruption (i.e., kyphosis >20 to 30 degrees or anterior loss of
vertebral body height >50% or both) may be treated with the use of
distraction-lordosis instrumentation to restore anterior and middle
column height. Care must be taken to avoid overdistraction in patients
with posterior column. A tension force placed on the neural elements
from overdistraction can result in significant neurologic injury. Often
a posterior interspinous wire is placed at the level of the posterior
ligamentous injury, preventing overdistraction, while accomplishing
fracture realignment through subsequent spinal distraction. If
short-segment fixation strategies are chosen, strict postoperative
immobilization in a custom-molded hyperextension orthosis or body cast
for a minimum of 3 months is recommended to decrease the potential for
spinal deformity recurrence and internal fixation failure.
of segmental fixation using sublaminar wires (Luque rods [rectangle]
and sublaminar wires). This procedure rarely is performed in the
setting of an intact or incomplete neurologic examination. If this
technique is chosen, the Luque rectangle is prebent in mild
hyphokyphosis to reduce the segmental kyphosis at the level of injury.
This technique generally incorporates three levels above and two to
three levels below the level of injury.
augmentation in symptomatic osteoporotic compression fractures has been
reported (vertebroplasty or kyphoplasty, which uses balloon elevation
of the vertebral end plates before cement insertion). Currently the
indications of these techniques for traumatic fractures of the thoracic
and lumbar spine are unclear.
involves a period of bed rest until resolution of initial symptoms,
followed by progressive ambulation in a full contact orthosis or cast
for 12 to 24 weeks with or without a unilateral thigh extension for the
initial 6 weeks of treatment. Several studies have evaluated back pain
associated with burst fractures and nonoperative management. Most
studies have concluded
that
the back pain is due to progressive degenerative changes as a result of
the initial injury. Residual symptomatic foraminal stenosis, segmental
instability, or sagittal plane deformity is a rare late manifestation
of a healed thoracolumbar burst fracture.
|
TABLE 5-7 MANAGEMENT OF THORACOLUMBAR FRACTURES
|
||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||
disruption of the posterior osteoligamentous complex (i.e., initial
kyphosis >20 degrees), the presence of facet subluxation or
spreading of the interspinous process distance, or greater than 50%
loss of anterior vertebral body height, surgical stabilization may help
to restore and maintain adequate spinal alignment. Surgical
intervention also is performed in an acute burst fracture with imaging
documentation of significant neural compression in the setting of an
incomplete neurologic deficit. Neurologic improvement has been seen 2
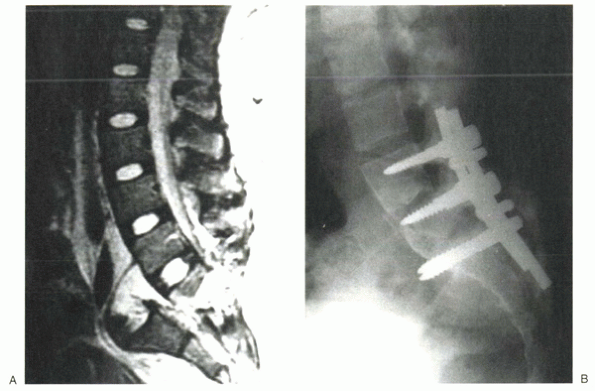
years after an injury following a late decompression (Fig. 5-7)
direct relationship between preinjury canal size and the force imparted
to the spine at the time of trauma and a
patient’s
resulting neurologic status. The degree of canal diameter and area is
significantly more compromised at the time of trauma than that noted on
postinjury MRI or CT evaluation.
 |
|
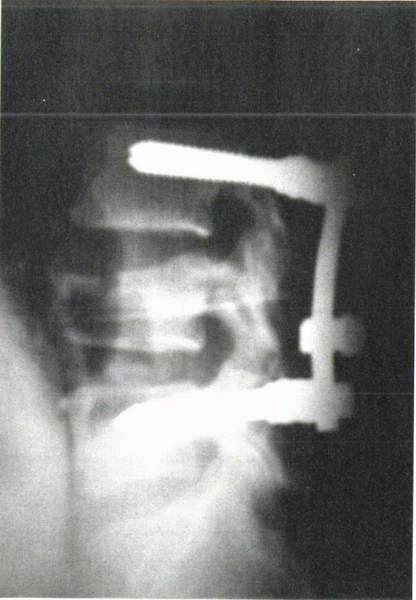
Figure 5-6
Segmental pedicle screw construct used to treat a compression fracture that involved loss of greater than 50% of anterior vertebral height and disruption of the posterior interspinous ligaments. |
interspinous ligaments and posterior longitudinal ligament (and
possibly disc space) heal slowly and unpredictably and often benefit
from surgical stabilization. Most posterior spinal implant techniques
immobilize the vertebral level above and below the injury or at the
vertebral level of injury and the level below if the injury is located
anatomically below the pedicle of the cephalad vertebrae. Caution in
the use of this reduction maneuver must be exercised if the middle
column is comminuted for the fear of retropulsion of bone or disc
material into the spinal canal or if the posterior facets are
incompetent, which may prevent a controlled anatomic reduction. If the
axis of rotation is posterior to the anterior spinal column and
anterior column compression failure is present, a distraction maneuver
may be applied at levels above and below the injury level when the
posterior elements at the fracture site are stabilized to prevent
posterior element distraction. The anterior longitudinal ligament in
this case serves as a stabilizing tension band.
rotational instability, or a translational shear injury in the absence
of a neurologic deficit requires an initial posterior segmental
reduction and stabilization procedure before considering the need for
an anterior decompressive and stabilization procedure. When reduction
is complete, a neutralization spinal implant strategy may be employed
to confer optimal stability and to prevent future fracture displacement
(Fig. 5-8). An awake intubation followed by
awake patient positioning is helpful in the absence of a complete
spinal cord injury to help protect the neural elements from further
injury due to voluntary patient splinting and afford real-time
surveillance of the neurologic exam.
 |
|
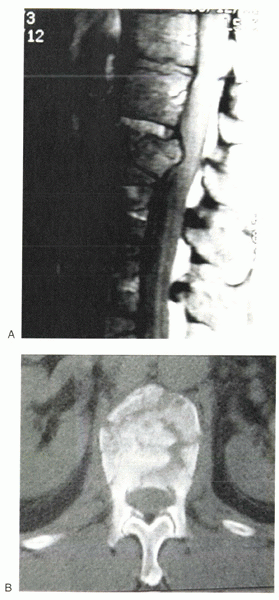
Figure 5-7 (A)
Sagittal MRI of a 34-year-old man who sustained a burst fracture to the T12 vertebral body. Note the retropulsion of the posterior vertebral body with compression of the anterior thecal sac. (B) Axial CT scan of the T12 burst fracture shows middle column failure with approximately 25% to 30% canal occlusion. |
 |
|
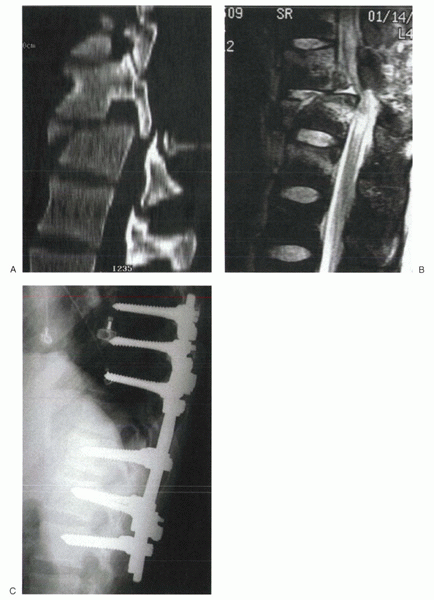
Figure 5-8 (A)
Sagittal CT reconstruction of a fracture-dislocation of the thoracolumbar spine shows marked vertebral body displacement and canal narrowing. (B) Sagittal MRI of the injury shows marked canal narrowing. Note the draping of the spinal cord over the posterosuperior edge of the caudal thoracic vertebrae. (C) Postoperative lateral radiograph shows reduction of the spinal deformity followed by a fusion and stabilization with segmental pedicle screw anchors spanning three levels above and below the level of injury. |
typically have an underlying metabolic bone disease and a preexisting
spinal deformity (i.e., ankylosing spondylitis or diffuse idiopathic
skeletal hyperostosis). Immobilization alone is inadequate because
these are highly unstable injuries with a high likelihood of
progression and neurologic worsening. Supine positioning may exacerbate
the spinal deformity and cause neurologic decline due to the existence
of a preinjury kyphotic spinal deformity. A principle of emergency
management of this spinal injury is to attempt to reproduce the
preinjury sagittal profile of the patient regardless of neurologic
status through bedding supplements or skeletal traction. When
reduced, surgical stabilization with segmental internal fixation may be performed (Fig. 5-9).
 |
|
Figure 5-9 (A) Sagittal T2-weighted MRI of a complete fracture-dislocation through the L5 vertebral body. (B)
Lateral postoperative radiograph shows adequate reduction of the fracture-dislocation stabilized with pedicle screw instrumentation from L4-S1. |
imaging, controversy continues regarding the indications for surgical
intervention, the timing of intervention, and the approach with which
to correct any existing spinal deformity. Nevertheless, the basic
tenets of trauma surgery should be strictly adhered to. When the
patient is medically stabilized, a detailed neurologic exam and careful
radiographic evaluation should be performed. The surgeon should be
aware of the biomechanics of the thoracolumbar spine, the mechanism of
injury, and the various implants available for treatment. Most
thoracolumbar injuries, in the absence of a neurologic deficit, are
stable and can be treated successfully nonoperatively. For the rare
unstable spinal fracture, with or without a neurologic deficit,
surgical treatment often is beneficial in improving patient
mobilization and early functional return to society. The ultimate goals
in managing thoracolumbar injuries are to maximize neurologic recovery
and to stabilize the spine expeditiously for early rehabilitation and
an early return to a productive lifestyle.
E, Sato K, Shimada Y, et al. Thoracolumbar burst fracture with
horizontal fracture of the posterior column. Spine 1997;22:83-87.
HH, Kirkpatrick JS, Delamarter RB. Anterior decompression for late pain
and paralysis after fractures of the thoracolumbar spine. Clin Orthop
1994;300:24-29.
GD, Minato Y, Okada A. Early time-dependent decompression for spinal
cord injury: vascular mechanisms of recovery. J Neurotrauma
1997;14:951-962.
PC, Yuan HA, Fredrickson BE, Lubicky JP. The value of computed
tomography in thoracolumbar fractures: an analysis of one hundred cases
and a new classification. J Bone Joint Surg Am 1983; 65:461-473.
RJ, Johnson JP. Vascular complications in anterior thoracolumbar spinal
reconstruction. J Neurosurg 2002;96(1 Suppl): 1-5.
AR, Daugherty RJ, Sheehan TP. Neurologic outcome of early versus late
surgery for cervical spinal cord injury. Spine 1997;22: 2609-2613.
