Physical Examination Tests for the Shoulder and Elbow
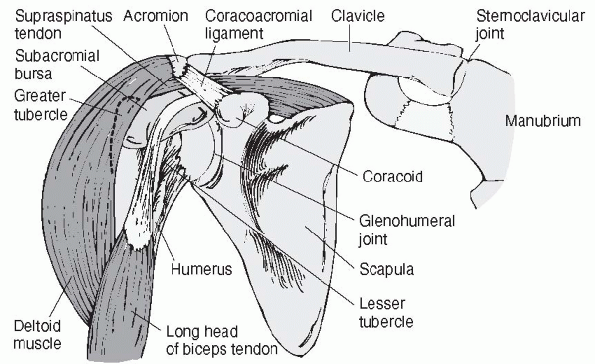
ball-and-socket joint that links the upper extremity to the axial
trunk. Due to its large range of motion, there is an inherent sacrifice
in bony stability. The shoulder complex is made up of three bones (the
scapula, clavicle, and humerus) with four articulations (the
sternoclavicular, acromioclavicular (AC), scapulothoracic, and
glenohumeral joints). Major softtissue contributors include the muscles
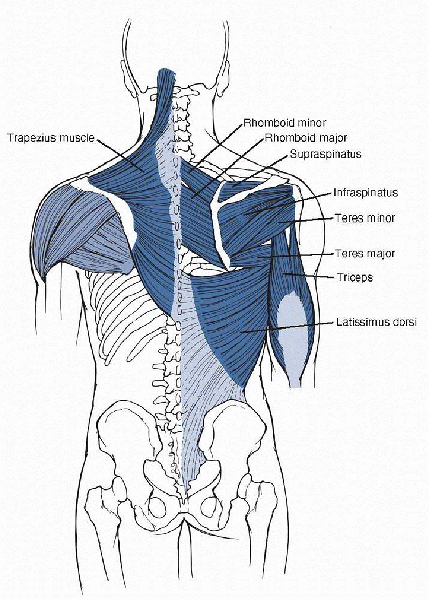
of the rotator cuff (supraspinatus, infraspinatus, teres minor, and
subscapularis), the glenoid labrum, glenohumeral ligaments,
coracoacromial and coracoclavicular (CC) ligaments, long head of the
biceps tendon, and scapulothoracic muscles (Figs. 15-1 and 15-2).
dynamic stabilizer of the glenohumeral joint and a humeral head
depressor. It contributes to the torque that is required in shoulder
elevation and internal and external rotation of the humerus. The
supraspinatus, which lies across the top of the glenohumeral joint,
provides joint compression by contraction. This counteracts the force
generated during shoulder elevation that is provided by the deltoid.
The supraspinatus also contributes to shoulder abduction along with the
deltoid. The infraspinatus and teres minor muscles both function as
external rotators of the arm. The subscapularis function is to provide
internal rotation and to act as dynamic barrier to anterior humeral
displacement. The long head of the biceps tendon is felt to contribute
to dynamic stability of the humeral head in the superior and posterior
planes. The supraspinatus arises from the supraspinatus fossa of the
scapula, passes beneath the acromion and AC joint, and inserts into the
upper portion of the greater tuberosity. It is innervated by the
suprascapular nerve. The infraspinatus originates from the
infraspinatus fossa of the scapula, inserting into the posterolateral
aspect of the greater tuberosity. It is also innervated by the
suprascapular nerve. The teres minor, innervated by the axillary nerve,
originates from the lateral border of the scapula and inserts on the
lower portion of the greater tuberosity. The subscapularis arises from
the anterior surface of the scapula, inserting on the lesser
tuberosity. It is innervated by the upper and lower subscapular nerves.
 |
|
Figure 15-1
Shoulder (right anterior view) joint. (From Weber J, Kelley J. Health Assessment in Nursing, 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 2003.) |
 |
|
Figure 15-2
Muscles of the posterior shoulder region. (From Hendrickson T. Massage for Orthopedic Conditions. Philadelphia: Lippincott Williams & Wilkins, 2003.) |
injury mechanism and arm position are important factors. The patient’s
age, dominant arm, and chief complaint play a major role in
establishing an accurate diagnosis and should not be overlooked. Within
the shoulder physical examination, numerous provocative tests have been
described. These can be thought of, in a general sense, as belonging to
two categories: tests that evaluate the rotator cuff and those that
test for shoulder stability. Within these two general categories are
numerous specific tests that attempt to isolate specific structures
within the glenohumeral joint, subacromial space, AC joint, and
surrounding supporting structures.
-
As always, physical examination of the
shoulder joint complex should take place only after a detailed and
thorough history has been performed. -
The patient should be unclothed and the entire upper extremity—including the front and back of the torso—should be visualized.
-
After careful inspection, palpation for
areas of bony and soft-tissue tenderness is performed, and
documentation of both active and passive shoulder range of motion is
noted. -
The following specific provocative
physical examination tests can then be used and are utilized to confirm
selectively suspicious findings obtained from the history. (If the test
is illustrated by a figure, the steps in performing it are in the
legend.)
encroachment on the subacromial space by bursa and spurs leading to
rotator cuff irritation (Table 15-1). The following tests are used to evaluate for rotator cuff irritation/injury in the subacromial space.
resulting from contact between the rotator cuff and biceps tendon
against the coracoacromial arch (Fig. 15-3).
This contact can cause an inflammatory response, resulting in
subacromial bursitis and reducing the space for the rotator cuff
tendons to glide underneath the acromion. Also known as the empty can
test, the supraspinatus test (or Jobe’s test) was first described in
1983. A positive finding produces pain or weakness about the involved
shoulder, implicating the supraspinatus muscle or tendon as the site of
pathology. Complaints of pain involving the anterior shoulder or
anterolateral arm involving the deltoid muscle may also be indicative
of tendonitis or impingement of the supraspinatus outlet. Itoi et al.
evaluated the empty can test in 143 shoulders of 136 patients with a
positive result documented for pain, muscle weakness, or both.
Examination results were correlated with follow-up high-resolution
magnetic resonance imaging. The empty can test was 70% accurate in
predicting a torn supraspinatus tendon when muscle weakness was used as
a positive finding. Pain was observed in 71 shoulders (50%).
|
TABLE 15-1 NEER’S THREE PHASES OF IMPINGEMENT OF THE ROTATOR CUFF
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 15-3
Jobe’s test is performed with the patient standing with both shoulders abducted to 90 degrees, horizontally adducted approximately 30 degrees, and internally rotated so the patient’s thumbs point to the floor. In this position, the examiner resists the patient’s attempt to abduct both shoulders. |
pain about the shoulder or reproduce patient-specific symptoms. The
Neer test, first described in 1972 and then further in 1983, is another
test for subacromial outlet impingement (Fig. 15-4).
A positive test will reproduce pain in patients with impingement
syndrome and may also be positive in patients with adhesive capsulitis,
calcific tendonitis, and AC arthrosis. For those with true impingement
pain, the Neer’s test can usually be relieved with subacromial local
anesthetic injection. The injection is performed under sterile
conditions with insert of local anesthetic into the subacromial space.
Patient subjective decrease in pain is felt to be indicative of
impingement. In an anatomic study evaluating the provocative position
of the Neer test, subacromial soft-tissue contact with the medial
aspect of the acromion was noted. McDonald et al. demonstrated a 75%
sensitivity of this test for subacromial bursitis and 88% for
abnormalities of the rotator cuff,
with
specificities of 48% and 51%. Furthermore, the Neer impingement test
was positive in 25% of patients with Bankart lesions and 46% of those
with superior labrum anterior and posterior (SLAP) lesions. The test
was also positive in 69% of those patients with AC arthritis.
 |
|
Figure 15-4
Neer’s test is performed with the patient seated and the examiner standing. In this position, scapular rotation is prevented by one hand as the other is used to raise the patient’s arm in forward flexion causing the greater tuberosity to impinge against the acromion. |
The maneuver brings the greater tuberosity of the humerus farther under
the coracoacromial ligament reproducing impingement pain. Shoulder pain
and apprehension in this position are felt to be indicative of
supraspinatus subacromial impingement. Analysis of this test has
demonstrated 88% and 92% sensitivity for rotator cuff abnormalities and
subacromial bursitis, respectively, with a specificity of 43% and 44%.
Of the patients with AC joint arthritis, greater than 90% had a
positive test result with the Hawkins test.
 |
|
Figure 15-5
For Hawkins’ test, the patient is either seated or standing. The examiner forward flexes the patient’s humerus to 90 degrees and then internally rotates the shoulder. |
the function of the supraspinatus tendon and appears very similar to
the Jobe supraspinatus test. This is another test for supraspinatus
outlet impingement. The test is performed with abduction of the
patient’s arm to 90 degrees, forward flexion to 30 degrees, and maximal
internal rotation. In this position, the examiner resists active
shoulder abduction, and reproduction of pain and/or weakness in this
position implicates the supraspinatus tendon as the site of injury and
is felt to be indicative of impingement tendonitis.
differentiate between intra-articular (internal impingement) and
classic outlet impingement syndromes (Fig. 15-6).
Internal impingement is commonly seen in overhead athletes with subtle
glenohumeral instability. These patients have impingement of the
posterior rotator cuff along the posterior superior labrum in the late
cocking phase of the throwing motion and pain in the region of the
infraspinatus insertion with abduction and maximal external rotation on
physical examination. If the patient with a positive impingement sign
has good strength in external rotation, this test is considered
positive and predictive of internal impingement. A negative test (more
weakness in external rotation) is suggestive of classic outlet
impingement (external impingement). A prospective study of 110 patients
yielded a sensitivity of 88% and specificity of 96% in defining these
diagnoses. The positive predictive value was 88%, and the negative
predictive value was 94%.
reproduce entrapment of the rotator cuff between the humeral head and
the coracoid
identifying those patients with a suspected diagnosis of subcoracoid impingement (Fig. 15-7).
Although uncommon, this diagnosis has been described in patients with a
long or laterally placed coracoid process and should be considered in
patients with negative classic impingement signs that describe
anterior/lateral pain with overhead activities and have subjective
complaints similar to those with classic outlet impingement. From an
anatomic standpoint, these patients have impingement of the coracoid
process on the proximal humerus with forward flexion and internal
rotation of the arm. Gerber showed that forward flexion to 90 degrees
combined with internal rotation was restricted and consistently painful
in patients with subcoracoid impingement.
 |
|
Figure 15-6
The internal rotation resistance stress test is performed with the patient standing and the arm in 90 degrees of abduction in the coronal plane and 80 degrees of external rotation. With the examiner standing behind the patient, a manual isometric muscle test is performed for external rotation and this is compared to one for internal rotation in the same position. |
 |
|
Figure 15-7
The subcoracoid impingement test is performed with the involved arm forward flexed to 120 to 130 degrees and internally rotated, reproducing the patient’s symptoms of pain. |
integrity of the musculotendinous units of the rotator cuff. The
following tests attempt to identify weaknesses or deficiencies in
rotator cuff strength that signify a tear.
test the integrity of the supraspinatus and infraspinatus tendons. The
test is performed with the patient either seated or standing. The elbow
on the side of the involved shoulder is passively flexed to 90 degrees,
and the shoulder is held at 20 degrees of elevation (in the scapular
plane) and near-maximal external rotation. In this position, the
patient is then asked to actively maintain the position of external
rotation when the examiner releases the wrist while supporting the limb
at the elbow. The sign is considered positive when a lag occurs and the
patient is unable to actively maintain the position of external
rotation. This should be recorded to the nearest 5 degrees. It is
important to take into consideration any loss of passive motion as a
result of capsular contracture or subscapularis injury, because this
may lead to false-negative or false-positive results. Also, the
involved side should be compared with the uninvolved contralateral
shoulder. Jobe’s test may be more sensitive for posterosuperior rotator
cuff tears when compared with the ERLS. Furthermore, the ERLS was more
sensitive than the drop sign (described below). There was found to be
no difference in accuracy when comparing the Jobe sign and ERLS, and
both were more accurate than the drop sign. Positive predictive value
for the Jobe sign was 84%, and the negative predictive value was 58%.
The drop sign and ERLS both had 100% positive predictive values, and
56% and 32% negative predictive values, respectively.
test the integrity of the subscapularis tendon. The test is performed
with the patient either standing or seated on the examination table.
The involved arm is held at maximal internal rotation by the examiner.
The patient’s elbow is flexed to 90 degrees, and the shoulder is held
at 20 degrees of elevation and 20 degrees of extension. The hand is
passively lifted away from the lumbar region until near full internal
rotation is accomplished. The patient is then instructed to actively
maintain this position as the examiner releases the wrist while
maintaining support at the elbow. When a lag occurs and the patient is
unable to maintain the arm position, the test is said to be positive
for injury to the subscapularis (either partial or full thickness tear)
and is recorded to the nearest 5 degrees and compared with the
contralateral side. With large tears, an obvious drop of the hand will
occur. A slight lag may indicate a partial tear of the superior portion
of the subscapularis tendon.
signs and extent of rotator cuff injury. If the rotator cuff was
intact, the IRLS, ELRS, and drop arm tests were negative. In patients
with an isolated tear of the supraspinatus tendon, a lag of 5 to 10
degrees was seen in 94% (16 of 17 patients). All patients with combined
tears of the infraspinatus and supraspinatus demonstrated a lag of 10
to 15 degrees. Eighty percent (4 of 5 patients) with partial
subscapularis tendon tears demonstrated lag signs of 5 degrees. All of
those with complete ruptures had lag signs approaching 10 degrees.
The test is considered positive for a subscapularis tear if the patient
is unable to lift the dorsum of his hand off his back.
sign for subscapularis muscle rupture. The test is performed by
bringing the patient’s arm passively behind the body into a position of
maximal internal rotation. The test is considered normal if the patient
is able to maintain maximal internal rotation after the examiner
releases the patient’s hand. In their series, a normal test was
demonstrated in 100 patients who had no shoulder complaints and in 27
patients with a rotator cuff tear that did not involve the
subscapularis tendon. Eight of nine patients (88%) tested with full
thickness subscapularis tendon tears had positive lift-off test results.
In this test, the patient is instructed to press his abdomen with the
palm of his hand while attempting to keep the arm in maximal internal
rotation. If active internal
rotation
is intact, the elbow does not drop backward signifying an intact
subscapularis. However, if strength of the subscapularis is impaired,
internal rotation cannot be maintained. Thus, the patient notes
weakness, and the elbow drops back behind the trunk. This is felt to be
an indication of either partial or complete subscapularis tear. In
Gerber’s series of patients studied in 1996, eight of eight patients
had a positive belly press test result with subscapularis tendon tears.
 |
|
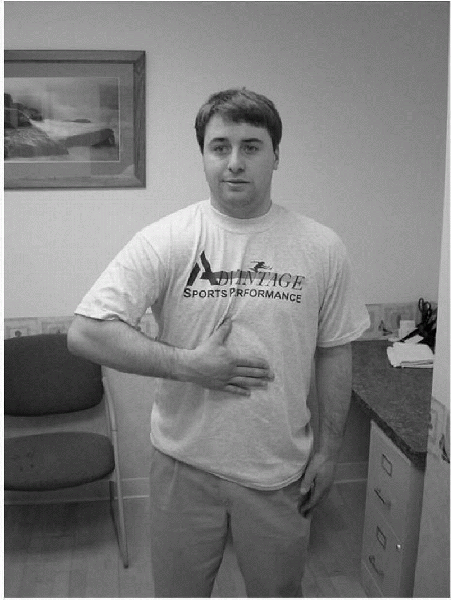
Figure 15-8
The lift-off test is performed with the patient standing and with the involved arm in a position of internal rotation placing the dorsum of the patient’s hand against his back. The patient is then asked to actively lift the hand off the back. |
 |
|
Figure 15-9
In the belly press test, the patient presses the abdomen with the palm of the hand while attempting to keep the arm in maximal internal rotation. |
integrity of the infraspinatus tendon. The test is performed with the
patient either standing or seated on the examination table. With the
elbow flexed to 90 degrees, the examiner holds the involved arm at 90
degrees of elevation in the scapular plane and near full external
rotation. In this position, external rotation is maintained primarily
by the infraspinatus. The patient is then instructed to maintain this
position as the examiner releases the wrist while supporting the elbow.
The sign is considered positive for a tear of the infraspinatus tendon
if a lag or drop occurs and is recorded to the nearest 5 degrees and
compared with the contralateral side.
head depressor and plays a role in anterior stability of the
glenohumeral joint by increasing the resistance of the shoulder to
torsional forces in the positions of abduction and external rotation.
In the presence of a rotator cuff tear, the biceps may also be torn or
become enlarged by increased functional requirements if the tear
involves the anterior superior rotator cuff or subscapularis. The
following tests attempt to identify injury to the long head of the
biceps tendon.
attempts to isolate the long head of the biceps tendon as the source of
shoulder pain (Fig. 15-10). The test is
positive if the maneuver produces tenderness or pain localized to the
bicipital groove and may represent such pathologic findings as biceps
tendonitis or SLAP lesions.
 |
|
Figure 15-10
For Speed’s test, the patient is either in the sitting or standing position. The involved shoulder is flexed to 90 degrees with the elbow fully extended and the forearm supinated. The examiner then places one hand along the volar aspect of the patient’s forearm and resists the patient’s attempt to actively forward flex the shoulder. |
 |
|
Figure 15-11
Yergason’s test is performed with the patient either sitting or standing and the elbow flexed to 90 degrees while stabilized against the side of the body. The forearm begins in a pronated position. The examiner then holds the patient’s wrist to resist active supination, then instructs the patient to attempt to actively supinate the forearm/wrist. |
The test is considered positive if the maneuver reproduces pain in the
region of the proximal bicipital groove and may indicate proximal
bicipital tendonitis.
surface of the anteromedial aspect of the acromion and the convex
surface of the distal clavicle. A fibrocartilaginous disc exists within
the AC joint. The main function of the joint is to serve as a
connection between the scapula and clavicle supporting the shoulder on
the chest wall. The AC joint is exposed to mainly compressive forces.
The stability of the AC joint is provided by two sets of ligaments: the
CC ligaments (conoid and trapezoid) and AC capsuloligamentous complex.
The superior and inferior AC ligaments act as the primary restraints to
posterior clavicular displacement. The CC ligament provides restraint
to anterior and superior displacement of the clavicle.
AC joint as the source of anterior/superior shoulder pain and is
positive in patients with AC arthritis or those with recent diagnosis
of AC separation (Fig. 15-12). When the
maneuver is performed, superior shoulder pain (specifically pain
localized at the AC joint) is indicative of AC joint pathology. Pain
not felt specifically at the AC joint and more involving the anterior
shoulder may indicate supraspinatus, long head of the biceps, or
subscapularis pathology. Complaints of posterior shoulder pain with
this maneuver may relate to posterior capsule or posterior rotator cuff
pathology. One study demonstrated a 77% sensitivity using this test to
evaluate AC joint pathology.
 |
|
Figure 15-12
For the crossover impingement test, the patient is in the sitting position with the examiner standing with one hand on the posterior aspect of the patient’s shoulder to stabilize the trunk and the other hand holding the patient’s elbow on the involved side. The examiner then maximally adducts the involved shoulder across the patient’s body. |
described as pain and/or movement of the scapula inferior to the clavicle indicating injury to the AC and or CC ligament.
 |
|
Figure 15-13
For the AC joint distraction test, the patient sits with the involved arm at the side and the elbow flexed to 90 degrees. The examiner stands on the patient’s involved side, and with one hand holds the patient’s arm just above the elbow, while the examiner’s other hand is placed over the involved AC joint. In this position, the examiner applies gentle downward pressure on the arm and notes any movement at the AC joint. |
patient in the sitting position and arm relaxed at the side. The
examiner stands on the involved side and places one hand on the
patient’s clavicle and the other on the spine of the scapula. In this
position, the examiner gently squeezes the hands together, noting any
movement at the AC joint. Pain or movement of the clavicle is felt to
represent a positive finding in AC or CC ligament injuries.
involving the AC joint. The test is used in patients suspected of
sustaining AC sprain or separation with injury to the AC joint and/or
CC ligaments. The patient sits with the involved limb relaxed at the
side. In this position, the examiner applies direct downward pressure
to the patient’s distal clavicle to depress it into its normal resting
position in a patient with AC ligament and CC ligament disruption. This
should be compared with the involved contralateral side.
evaluate the rotator cuff, biceps tendon, AC, and sternoclavicular
joints, there are special focused tests used to evaluate for shoulder
instability, laxity, and labral tears, including SLAP tears.
A positive finding is described as one in which the patient looks or
feels apprehensive or expresses feelings of pain or apprehension if the
shoulder were to be externally rotated further.
 |
|
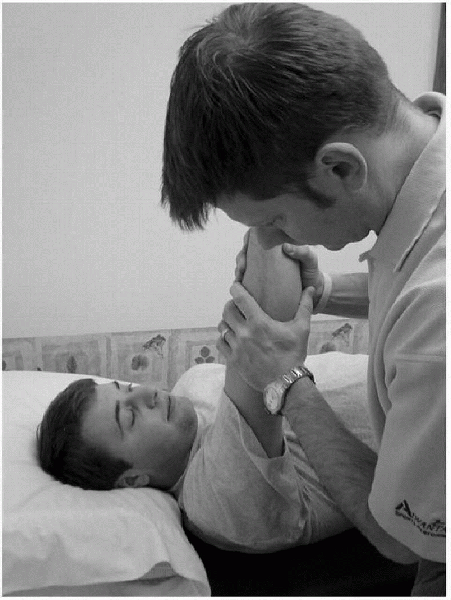
Figure 15-14
The apprehension test for glenohumeral anterior laxity/instability is performed with the patient sitting on the examination table. The involved shoulder is placed in 90 degrees of abduction with the elbow in 90 degrees of flexion. The examiner then slowly passively externally rotates the shoulder. |
 |
|
Figure 15-15
The apprehension test for posterior instability is performed with the patient lying supine on the examining table. The examiner places the patient’s involved shoulder in 90 degrees of forward flexion and internal rotation while applying a posterior force through the long axis of the humerus. |
A positive finding is felt to be present if the patient expresses
apprehension toward further movement in the posterior direction.
apprehension test. It is performed with the patient supine and the arm
in 90 degrees of abduction and external rotation. During the
apprehension portion of the test, the examiner pushes anteriorly on the
posterior aspect of the humeral head. This maneuver may produce a sense
of apprehension and at times also associated with pain in patients with
recurrent instability/dislocation. Patients with anterior subluxation
are felt to experience pain but not apprehension with this test, and
patients with a normal shoulder will be asymptomatic with the maneuver.
The relocation test is then performed (Fig. 15-16).
Patients with instability or subluxation and secondary outlet
impingement will have pain relief and can tolerate maximal external
rotation with the posteriorly directed force applied to the proximal
humerus. Patients with primary impingement alone will have no change in
their pain. Sensitivity for this test has been described at 68%;
specificity, 100%; positive predictive value, 100%; negative predictive
value, 78%; and accuracy, 85% when apprehension was the determinant of
a positive test result.
depression is observed with this maneuver between the lateral edge of
the acromion and the humeral head, the sulcus sign is said to be
positive, indicating injury to the rotator interval and contributing to
inferior glenohumeral instability. This should be compared with the
uninvolved contralateral side. The amount of depression should be
lessened with the same downward traction applied with the arm in
external rotation. The sulcus sign is graded 1+ when a gap is less than
1 cm, 2+ when the gap is between 1 and 2 cm, and 3+ when the gap is
more than 2 cm. In 1997, Henry et al. found the sulcus sign to have a
sensitivity of 97% and specificity of 99% in evaluation of inferior
glenohumeral laxity.
 |
|
Figure 15-16
The relocation test is used in conjunction with the apprehension test for posterior instability. It is performed by administering a posteriorly directed force on the humeral head with the arm in the abducted, externally rotated position. |
 |
|
Figure 15-17
Testing for the sulcus sign can be performed with the patient sitting or lying supine. The examiner applies downward traction on the involved arm with the scapula stabilized. |
The relative movement of the humerus relative to the scapula can then
be graded and compared with the contralateral side. Grading reflects
the degree of humeral head translation anterior to the glenoid rim. A
grade of 1+ is given for translation of the humeral head to the edge of
the glenoid; 2+ if the humeral head can be subluxated over the glenoid
rim but reduces spontaneously; and 3+ if a frank dislocation of the
humeral head over the glenoid rim does not reduce spontaneously.
notes the extent of posterior movement of the humeral head and compares
this to the uninvolved contralateral side. This may also be graded, as
is done with the anterior drawer test.
 |
|
Figure 15-18
For the anterior drawer test, the examiner faces the involved shoulder with the glenohumeral joint positioned at the edge of the examining table. The involved shoulder is held in 80 to 120 degrees of abduction, 0 to 20 degrees of forward flexion, and 0 to 30 degrees of lateral rotation. The examiner holds the patient’s scapula with one hand, pressing the scapular spine forward with the index and middle fingers, the thumb exerting counter pressure on the coracoid process. With the other hand, the examiner grasps the patient’s upper arm and attempts to draw it anteriorly. |
 |
|
Figure 15-19
For the posterior drawer test, the patient is supine, and the examiner stands next to the involved side, positioning the shoulder in 80 to 120 degrees of abduction and 20 to 30 degrees of forward flexion. The patient’s elbow is flexed in a relaxed position. The examiner then stabilizes the scapula by placing the other hand posterior to the shoulder joint capsule with the thumb over the coracoid process. In this position, while stabilizing the scapula, the examiner internally rotates the humerus, applying downward pressure and pushing the humeral head posteriorly. |
stresses are applied, and the amount of translation of the humerus on
the glenoid is noted (Fig. 15-20). An anterior
or posterior translation of the humeral head greater than 25% of the
diameter of the humeral head when a load is applied is considered a
positive test. This test should always be repeated bilaterally with
comparison to the contralateral shoulder. Translation between 25% and
50% has been described as being a grade I positive test. Greater than
50% translation with subsequent reduction is considered grade II. The
same amount of translation without reduction is described as grade III.
Tzannes et al. have described a 100% specificity for both the anterior
and posterior load shift tests in diagnosing anterior/posterior
instability. However, the sensitivity has been described as 50% and 14%
for the anterior and posterior tests respectively.
the glenoid articular surface through a fibrocartilaginous transition
zone. It is an anchor point for capsuloligamentous structures, thereby
deepening the glenoid concavity and reducing excessive glenohumeral
translation. The labrum functions to increase the depth and surface
area of the glenoid. It has been noted that labrum excision decreases
the depth of the glenohumeral socket by 50%, reducing resistance to
instability by 20%.
 |
|
Figure 15-20
The load and shift test is performed with the patient in the sitting position and the examiner behind him or her on the involved side. The examiner stabilizes the clavicle and scapula with one hand and with the other hand grasps the humeral head. The examiner then places an axial load along the shaft of the humerus in an attempt to compress the humeral head into the glenoid fossa. |
detect a glenoid labral tear. The test is performed with the patient
lying supine and the affected shoulder abducted 90 degrees with the
elbow flexed 90 degrees. In this position, the examiner grasps the
patient’s elbow with one hand and the proximal humerus with the other
hand and applies compression to the glenoid labrum while attempting to
circumduct the humeral head 360 degrees around the surface of the
glenoid. A positive finding of a clunking or grinding sensation may be
indicative of a glenoid labrum tear.
test. With the patient supine, the examiner places one hand on the
posterior aspect of the patient’s humeral head and the other hand
proximal to the patient’s elbow joint. In this position, the examiner
passively abducts and externally rotates the patient’s arm overhead
applying an anterior force to the humerus. The arm may also be brought
into internal rotation. The examiner then circumducts the humeral head
around the glenoid labrum. A positive finding of a clunking or grinding
sensation is felt to be indicative of a glenoid labral tear. In a study
by Stetson evaluating the test in 65 patients with shoulder pain
comparing physical examination results with findings from diagnostic
arthroscopy, the crank test was 56% specific, 46% sensitive, and had a
positive predictive value of 41% and a negative predictive value of 61%.
Since then, there have been a number of tests developed to detect this
lesion by physical examination. The following tests attempt to isolate
the superior labrum biceps anchor complex and identify injury to this
area.
shoulder flexion with the elbow extended and forearm supinated. A
positive test result (felt to be indicative of a SLAP lesion) was
defined as deep anterior shoulder pain reproduced with this maneuver.
In 1993, Field and Savoie observed the biceps tension test to be
positive in 20 consecutive patients with a diagnosis of SLAP lesion.
performed with the patient supine, shoulder abducted 90 degrees, and
the elbow flexed 90 degrees. In this position, a compression force is
applied to the humerus, which is then rotated in an attempt to trap the
suspected torn labrum. A positive test will demonstrate a catch or snap
of the torn superior labrum.
The test is considered positive for a SLAP lesion if deep shoulder pain
is present in the internally rotated position and reduced in the second
position (forearm supinated). Pain localized to the AC joint or on top
of the shoulder was considered to be diagnostic of AC joint
abnormalities. In a series of more than 300 patients, this test
demonstrated a sensitivity of 100%, a specificity of 99%, a positive
predictive value of 95%, and a negative predictive value of 100% for
labral abnormalities.
 |
|
Figure 15-21
The O’Brien active compression test is performed with the patient either sitting or standing. The involved shoulder is placed in 90 degrees of forward flexion, and 30 to 45 degrees of horizontal adduction and maximal internal rotation. The examiner then applies a downward force to the arm against the patient’s manual resistance. With the arm in the same position, the palm is then fully supinated and the maneuver repeated. |
SLAP lesions in patients with and without recurrent anterior
instability. This test is performed with the patient in the supine
position and the examiner on the side of the affected shoulder. The
involved shoulder is then abducted 120 degrees and maximally externally
rotated with elbow in 90 degrees of flexion and the forearm supinated.
The patient is then instructed to flex the elbow while this is
restricted by the examiner. The test is considered positive if the
patient complains of pain during the resisted elbow flexion. In 1999,
Kim assessed this test in 75 patients, with a reported specificity of
97%, a sensitivity of 91%, a positive predictive value of 83%, and a
negative predictive value of 98%.
examination, but not isolated to the shoulder, include tests for
thoracic outlet syndrome and the brachial plexus.
patient sitting. The examiner stands behind the patient and places one
hand on the side of the patient’s head and the other hand on the
shoulder on the same side. In this position, the examiner laterally
flexes the patient’s head while applying gentle downward pressure on
the shoulder. Pain that radiates in the patient’s arm opposite to the
laterally flexed neck is described as a positive finding. If pain is in
the neck on the side toward lateral flexion, this may represent
cervical spine facet joint impingement.
An absent or diminished radial pulse is felt to be indicative of
thoracic outlet syndrome secondary to subclavian artery compression by
the scalene muscles.
 |
|
Figure 15-22
In Adson’s maneuver, the patient is either standing or sitting, and the examiner places his fingers over the radial artery at the wrist. The examiner then externally rotates and extends the patient’s involved arm while palpating the radial pulse. The patient then extends and rotates the neck toward the involved arm and inhales. |
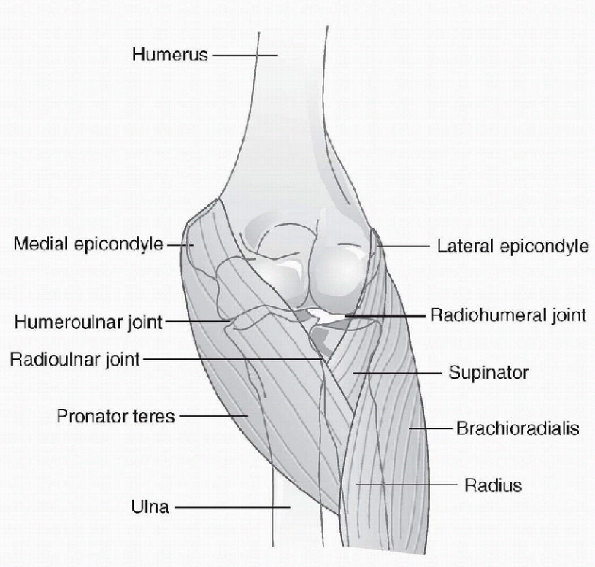
articulations: the ulnohumeral joint, humeroradial (radiocapitellar)
joint, and the radioulnar joint. The medial epicondyle of the distal
humerus serves as the attachment site of the ulnar collateral ligament
(UCL) and the flexor-pronator muscles of the forearm (flexor carpi
radialis, flexor carpi ulnaris, flexor digitorum superficialis,
pronator teres, and palmaris longus) (Fig. 15-23).
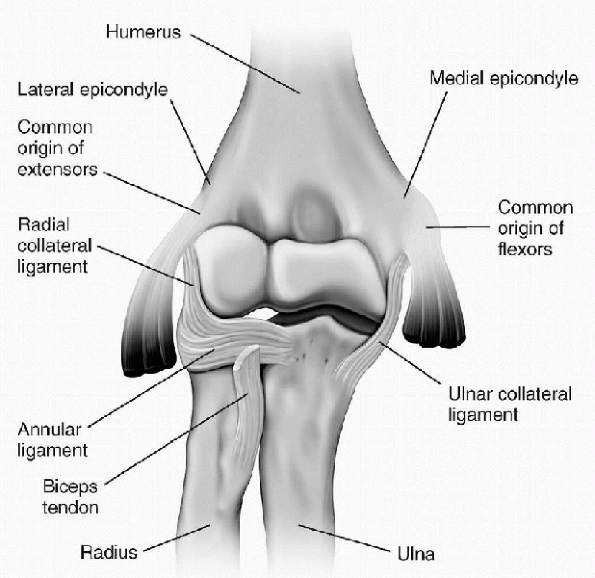
The lateral epicondyle of the distal humerus provides attachment for
the lateral UCL along with the extensor muscles of the forearm
(extensor carpi radialis longus and extensor carpi radialis brevis,
extensor carpi ulnaris, extensor digiti minimi, anconeus, and
supinator) (Fig. 15-24). The bony stability of
the joint is provided by the capsule, the UCL, the radial collateral
ligament, and the annular ligament. The elbow allows flexion and
extension along with supination and pronation. This enables the hand to
be placed in a variety of positions in space.
-
Although elbow injuries are not as common as those involving the shoulder, they may be difficult to diagnose.
-
A complete and thorough history and a full and systematic physical examination are required for correct diagnosis.
-
Along with this, knowledge of elbow anatomy and the abnormal conditions that may affect the joint are crucial.
-
A history should include a description of
the patient’s onset of symptoms (acute or chronic), location of pain,
duration of symptoms, dominant arm, and associated activities.-
Information gained will help to focus the physical examination.
-
-
Examination of the elbow joint should begin with inspection.
-
As with the shoulder, the patient should be unclothed to the waist for the examination.
-
The elbow is a superficial joint, and many of its disorders can be detected by simple inspection.
-
Inspection should involve the entire upper extremity along with comparison with the uninvolved contralateral extremity.
-
-
After inspection, the examination should
proceed with palpation of bony landmarks, including the medial and
lateral epicondyles, radiocapitellar joint, medial joint line, medial
and lateral collateral ligaments, distal biceps, and triceps tendons. -
Range of motion in the flexion/extension
and pronation/supination planes should be measured and recorded and
compared to the contralateral side. -
Information obtained from the history and
initial physical examination will provide clues toward the diagnosis
and direct the examiner to proceed further with necessary provocative
tests.
 |
|
Figure 15-23
Anterior view of the left elbow joint. (From Bickley LS, Szilagyi P. Bates’ Guide to Physical Examination and History Taking, 8th ed. Philadelphia: Lippincott Williams & Wilkins, 2003.) |
 |
|
Figure 15-24
Anterior view of the right elbow joint, radius, and ulna, showing the ligaments. (From Premkumar K. The Massage Connection Anatomy and Physiology. Baltimore: Lippincott Williams & Wilkins, 2004.) |
lateral epicondylitis or tennis elbow. There have been numerous tests
described to evaluate this entity, which involves angiofibroblastic
tendinosis of the extensor carpi radialis brevis origin at the lateral
humeral epicondyle. The following special tests are used to aid in this
diagnosis.
or radiation along the extensor-supinator muscle compartment is
considered a positive finding for lateral epicondylitis. This test can
also be performed with resisted wrist extension when the elbow is fully
extended. Pain with this maneuver along the lateral epicondyle is
considered a positive finding.
 |
|
Figure 15-25
Cozen’s test is performed with the patient sitting. The examiner stabilizes the involved elbow with one hand and places the palm of the other hand on the dorsal aspect of the subject’s hand just distal to the proximal interphalangeal joint of the patient’s long finger. The patient is then instructed to extend the long finger against the examiner’s resistance. |
The test is considered positive if pain or complaints of discomfort are
elicited along the medial aspect of the elbow (especially pain at the
medial epicondyle).
 |
|
Figure 15-26
The passive tennis elbow test is performed with the patient sitting and the involved elbow in full extension. In this position, the examiner passively pronates the patient’s forearm and flexes the patient’s wrist. |
 |
|
Figure 15-27
The golfer’s elbow test is performed with the patient either sitting or standing. The examiner faces the subject and palpates along the humeral medial epicondyle. While the patient makes a fist on the involved side, the examiner passively supinates the forearm and extends the elbow and wrist. |
caused by injury to the ulnar nerve or structural damage to the UCL. As
such, it is important to assess these structures individually. The
valgus stress test has been described to evaluate injury to the UCL (Fig. 15-28). Medial or increased
valgus movement with a diminished or absent end point is considered
indicative of damage to the UCL. During this test, it is imperative
that the humerus not be internally or externally rotated because this
may give a false-positive result. A recent study by O’Driscoll et al.
demonstrated a 100% sensitivity and 75% specificity utilizing a valgus
stress test for the diagnosis of UCL injury in the elbow.
 |
|
Figure 15-28
Valgus stress test. The test is performed with the patient sitting and the involved elbow flexed to 20 to 30 degrees. The examiner stands with the distal hand around the subject’s wrist (medially) and the proximal hand over the patient’s elbow joint (laterally). In this position, with the patient’s wrist stabilized, the examiner applies a valgus stress to the elbow with the proximal hand. |
Lateral elbow pain or increased varus movement with an absent or
diminished end point is felt to be indicative of injury to the radial
(lateral) collateral ligament.
pivot shift test, assesses laxity of the ulnar portion of the lateral
collateral ligament (Fig. 15-31). Apprehension
in the awake patient indicates a positive test—injury to the ulnar
portion of the lateral collateral ligament. However, displacement of
the ulna from the trochlea usually can only be performed with the
patient under general anesthesia.
either sitting or standing. The patient is instructed to maximally flex
the elbow and hold this position for 3 to 5 minutes. Radiating pain in
the median nerve distribution in the patient’s arm or hand (lateral
forearm or tip of thumb, index and middle finger, ulnar half of ring
finger) is considered a positive finding indicative of cubital fossa
syndrome. This test may also be indicative of ulnar nerve compression
in the ulnar groove if radiating pain extends in an ulnar nerve
distribution (the small finger and radial half of the ring finger).
In
1998, Rosati et al. evaluated the validity of this test for diagnosing
ulnar nerve compression at the cubital tunnel. The percentage of
positive tests was only 3.6% at 1 minute and increased to 16.2% at 3
minutes.
 |
|
Figure 15-29
In the milking test, the patient is seated. With the patient’s forearm fully supinated, the thumb is grasped and a valgus stress is applied to the elbow as the joint is passively flexed greater than 90 degrees. |
 |
|
Figure 15-30
In the varus stress test, the patient is sitting and the involved elbow is flexed to 20 to 30 degrees. The examiner sits facing the patient with the distal hand around the patient’s wrist (laterally) and the proximal hand around the patient’s elbow (medially). In this position with the patient’s wrist stabilized, the examiner applies a varus stress to the elbow. |
 |
|
Figure 15-31
In the lateral pivot shift test, the patient is supine. The involved arm is extended back over the patient’s head and the shoulder externally rotated. The examiner stands at the head of the table and supinates the patient’s forearm while simultaneously applying a valgus stress and axial compression and flexion of the elbow. |
 |
|
Figure 15-32
In testing for Tinel’s sign, the patient is seated with the elbow in slight flexion. The examiner grasps and stabilizes the patient’s wrist with one hand and taps the ulnar nerve between the medial epicondyle and olecranon with the other hand. |
A positive finding is described as subjective tingling along the ulnar
nerve distribution of the forearm, hand, and fingers. This test should
be repeated on the contralateral side for comparison. In 1994, a study
by Novak examined 44 extremities with cubital tunnel syndrome. Of
those, 31 had Tinel’s sign and sensitivity of 70%.
anterior interosseus nerve (a branch of the median nerve that
innervates the pronator quadratus, flexor pollicis longus, and the
first and second components of the flexor digitorum profundus). It may
be performed with the patient sitting or standing. The patient is
instructed to pinch the tips of the thumb and index finger together.
The inability to touch them together is described as a positive
finding, indicating potential pathology of the anterior interosseous
nerve between the two heads of the pronator muscle.
WF. Specificity of the Speed’s test: arthroscopic technique for
evaluating the biceps tendon at the level of the bicipital groove.
Arthroscopy 1998;14:789-796.
LU, Morrison DS, April EW. The morphology of the acromion and its
relationship to rotator cuff tears. Orthop Trans 1986;10: 228.
TS, Boeckmann RR. Interrater reliability of manual valgus stress
testing of the elbow joint and its relation to an objective stress:
radiography technique in professional baseball pitchers. J Orthop
Sports Phys Ther 1998;27:95.
LD, Savoie FH III. Arthroscopic suture repair of superior labral
detachment lesions of the shoulder. Am J Sports Med 1993;21: 783-790.
CS II. Anterior acromioplasty for the chronic impingement syndrome in
the shoulder: a preliminary report. J Bone Joint Surg 1972; 54A:41-50.
SJ, Pagnani MJ, Fealy S, et al. The active compression test: a new and
effective test for diagnosing labral tears and acromioclavicular joint
abnormality. Am J Sports Med 1998;26:610-613.
SW, Lawton, RL, Smith A. The “moving valgus stress test” for medial
collateral ligament tears of the elbow. Am J Sports Med
2005;33(2):231-239.
DT, Beach WR, Meyers JF. A review of the special tests associated with
shoulder examination. Part I: The rotator cuff tests. Am J Sports Med
2003;31:154-160.
DT, Beach WR, Meyers JF. A review of the special tests associated with
shoulder examination. Part II: laxity, instability and superior labral
anterior and posterior (SLAP) lesions. Am J Sports Med 2003;31:301-307.
