Humeral Shaft Fracture
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Humeral Shaft Fracture
Humeral Shaft Fracture
Simon C. Mears MD, PhD
Chris Hutchins MD
Description
-
Fractures of the diaphysis (shaft) of the humerus
-
Occur at all ages
-
Classification:
-
AO classification method (1)
-
Anatomic location:
-
Proximal 1/3 of the shaft
-
Medial 1/3 of the shaft
-
Distal 1/3 of the shaft
-
-
-
Fracture characteristics:
-
Fracture pattern (transverse versus oblique versus comminuted)
-
Fractures may be open or closed.
-
Pathologic (secondary to underlying bone disease)
-
Spiral fractures of the distal 1/3 have been termed “Holstein-Lewis” fractures and are associated with radial nerve injury.
-
Epidemiology
Incidence
-
Fracture rate is 0–2 per 10,000 per year with no gender differences (2).
-
Midshaft fractures comprise ~40% of all humerus fractures (3).
-
In children, humerus fractures cause 17% of admissions for fracture (4).
-
Fracture incidence peaks in the 3rd decade, but a 2nd peak occurs in females in their 7th decade (5).
Risk Factors
-
Osteoporosis in the elderly
-
High-energy trauma, such as motor vehicle accidents or falls from heights, in younger patients
-
Sports with rotational forces, such as wrestling or baseball
Etiology
-
Usually results from direct force to the upper extremity
-
May occur:
-
From violent muscle contractions and twisting arm injuries
-
After relatively minor trauma in patients with underlying bone disease
-
In young adults when throwing balls while playing softball or baseball
-
Associated Conditions
-
Look for other associated upper extremity fractures or injuries.
-
Carefully examine the neurovascular status.
Signs and Symptoms
-
Pain
-
Deformity
-
Bruising
-
Crepitus
-
Swelling
Physical Exam
-
Assess for skin integrity (ensure that no open fracture exists).
-
Examine the shoulder and elbow joints and the forearm, hand, and clavicle for associated trauma.
-
Check the function of the median, ulnar, and, particularly, the radial nerves.
-
Assess for the presence of the radial pulse.
Tests
Lab
No serum or laboratory test is diagnostic.
Imaging
AP and lateral views of the humerus, including the joints below and above the injury, are obtained.
Differential Diagnosis
-
Pathologic fractures through abnormal bone
-
Muscular contusions
-
Muscle tear or strain
-
Most closed fractures of the humeral shaft may be managed nonoperatively.
-
Reduction should be attempted if there is >20–30° of angulation, >3 cm of shortening, or >15° of rotational deformity.
-
Lesser degrees of shortening or angulation are tolerated satisfactorily.
-
-
Splinting:
-
Fractures are splinted with a “U” splint, which is from the axilla, under the elbow, postioned to the top of the shoulder (Fig. 1).
-
The U splint is supplemented by a
posterior splint, which originates at the proximal humerus and extends
behind the elbow to the forearm. -
The splinted extremity is supported by a sling.
-
-
Fracture brace:
-
After 1–2 weeks, swelling will have subsided, and the extremity is placed in a fracture brace.
-
Immobilization by fracture bracing is
continued for at least 2 months or until clinical and radiographic
evidence of fracture healing is observed.
-
-
With this treatment regimen, union rates of ~90% can be attained (6,7).
-
Occasionally, humeral shaft fractures require operative fixation; indications include:
-
Open fractures
-
Articular injury
-
Neurovascular injury
-
Ipsilateral forearm fractures
-
Impending pathologic fractures
-
Segmental fractures
-
Multiple extremity fractures
-
Fractures in which reduction is unable to be achieved or maintained
-
Fractures with nerve palsy after reduction maneuvers
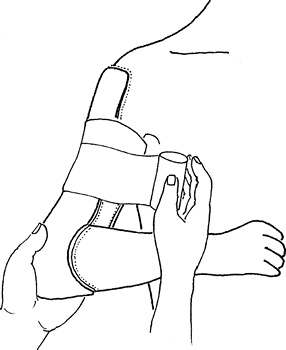 Fig. 1. Applying a sugar tong splint for humeral shaft fractures.
Fig. 1. Applying a sugar tong splint for humeral shaft fractures.
-
P.197
General Measures
Activity
Support the arm in a sling.
Nursing
-
In the acute period, apply ice to the region for 20 min every 3–4 hours to help decrease swelling.
-
Sensation of movement of the fracture ends is common.
-
The axillary area must be cleaned after splinting.
Special Therapy
Physical Therapy
-
None is required in the initial period.
-
When pain has subsided (~1–2 weeks), gentle ROM of the shoulder and elbow should be started.
Medication
First Line
Narcotic analgesics may be required for pain control.
Surgery
-
Surgery involves fixation of the bone fragments with a plate and screws or intramedullary fixation with a metal nail.
-
Plating with a 4.5-mm dynamic compression plate or a locking plate
-
Intramedullary fixation with an anterograde or a retrograde starting point
-
Anterograde starting points are associated with a higher rate of late shoulder pain than are retrograde starting points (8).
-
-
-
If severe soft-tissue injury exists, external fixation may be necessary.
Prognosis
~90% of humeral shaft fractures treated without surgery heal (6,7).
Complications
-
Injury to the radial nerve:
-
Occurs in ~11% of humerus fractures
-
Can occur at the time of initial injury, during closed reduction, or during operative repair (9)
-
If radial nerve palsy is identified after fracture reduction, operative exploration with plate fixation usually is recommended.
-
~70% of these injuries are neurapraxias (contusions to the nerve fibers) that improve over time (9).
-
-
Nonunion rates are thought to be higher when fractures are treated with intramedullary nailing (10).
-
Malunion is thought be well tolerated.
-
Shoulder pain has been reported when fractures are treated with nails and with plates (11).
-
Elbow or shoulder stiffness
Patient Monitoring
-
Serial radiographs are obtained at 4–6-week intervals to ensure progressive healing and angulation of <30°.
-
ROM of the shoulder and elbow must be checked so that adjustments can be made in the physical therapy program.
References
1. Muller
ME. Appendix A to chapter 1: The comprehensive classification of long
bones. In: Muller ME, Allgower M, Schneider R, et al., eds. Manual of
Internal Fixation. Techniques Recommended by the AO-ASIF Group, 3rd ed.
New York: Springer-Verlag,1991:118–150.
ME. Appendix A to chapter 1: The comprehensive classification of long
bones. In: Muller ME, Allgower M, Schneider R, et al., eds. Manual of
Internal Fixation. Techniques Recommended by the AO-ASIF Group, 3rd ed.
New York: Springer-Verlag,1991:118–150.
2. Singer BR, McLauchlan GJ, Robinson CM, et al. Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg 1998;80B:243–248.
3. Igbigbi PS, Manda K. Epidemiology of humeral fractures in Malawi. Int Orthop 2004;28: 338–341.
4. Galano
GJ, Vitale MA, Kessler MW, et al. The most frequent traumatic
orthopaedic injuries from a national pediatric inpatient population. J Pediatr Orthop 2005;25:39–44.
GJ, Vitale MA, Kessler MW, et al. The most frequent traumatic
orthopaedic injuries from a national pediatric inpatient population. J Pediatr Orthop 2005;25:39–44.
5. Tytherleigh-Strong G, Walls N, McQueen MM. The epidemiology of humeral shaft fractures. J Bone Joint Surg 1998;80B:249–253.
6. Koch PP, Gross DFL, Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg 2002;11: 143–150.
7. Sarmiento A, Zagorski JB, Zych GA, et al. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg 2000;82A:478–486.
8. Scheerlinck
T, Handelberg F. Functional outcome after intramedullary nailing of
humeral shaft fractures: comparison between retrograde
Marchetti-Vicenzi and unreamed AO antegrade nailing. J Trauma 2002;52:60–71.
T, Handelberg F. Functional outcome after intramedullary nailing of
humeral shaft fractures: comparison between retrograde
Marchetti-Vicenzi and unreamed AO antegrade nailing. J Trauma 2002;52:60–71.
9. Shao
YC, Harwood P, Grotz MRW, et al. Radial nerve palsy associated with
fractures of the shaft of the humerus: a systematic review. J Bone Joint Surg 2005;87B:1647–1652.
YC, Harwood P, Grotz MRW, et al. Radial nerve palsy associated with
fractures of the shaft of the humerus: a systematic review. J Bone Joint Surg 2005;87B:1647–1652.
10. McCormack
RG, Brien D, Buckley RE, et al. Fixation of fractures of the shaft of
the humerus by dynamic compression plate or intramedullary nail. A
prospective, randomised trial. J Bone Joint Surg 2000;82B:336–339.
RG, Brien D, Buckley RE, et al. Fixation of fractures of the shaft of
the humerus by dynamic compression plate or intramedullary nail. A
prospective, randomised trial. J Bone Joint Surg 2000;82B:336–339.
11. Flinkkila
T, Hyvonen P, Siira P, et al. Recovery of shoulder joint function after
humeral shaft fracture: a comparative study between antegrade
intramedullary nailing and plate fixation. Arch Orthop Trauma Surg 2004;124:537–541.
T, Hyvonen P, Siira P, et al. Recovery of shoulder joint function after
humeral shaft fracture: a comparative study between antegrade
intramedullary nailing and plate fixation. Arch Orthop Trauma Surg 2004;124:537–541.
Additional Reading
Caviglia H, Garrido CP, Palazzi FF, et al. Pediatric fractures of the humerus. Clin Orthop Relat Res 2005;432:49–56.
DeFranco MJ, Lawton JN. Radial nerve injuries associated with humeral fractures. J Hand Surg 2006;31A:655–663.
Sarmiento A, Waddell JP, Latta LL. Diaphyseal humeral fractures: treatment options. Instr Course Lect 2002;51:257–269.
Codes
ICD9-CM
812.21 Humeral shaft fracture
Patient Teaching
-
Once in a fracture brace, the patient may commence gentle active ROM of the shoulder and the elbow.
-
Activities of daily living are encouraged.
-
During the initial healing period, many patients find that sleeping in a chair is more comfortable than sleeping in a bed.
Activity
Patients treated with open plating may bear weight on the affected arm.
FAQ
Q: How long does it take to heal a humerus fracture?
A:
Most fractures are treated without surgery and take ~3–4 months to
heal. After healing, continued work is needed to improve arm motion and
strength.
Most fractures are treated without surgery and take ~3–4 months to
heal. After healing, continued work is needed to improve arm motion and
strength.
