ARTHROSCOPIC TREATMENT OF THE ELBOW
Its minimally invasive nature allows for rapid postoperative
rehabilitation, which helps prevent the most common and dreaded
complication of elbow surgery, arthrofibrosis. Arthroscopy permits
better visualization of the elbow joint than does limited arthrotomy;
arthroscopy of the elbow is difficult, however, because the joint is
small and in close proximity to neurovascular structures. These reasons
limit widespread use of the procedure.
evaluation of disorders of the elbow. The timing of the injury, whether
it was acute or insidious in onset, is important. Acute trauma to the
elbow may involve capsular injury, which is a contraindication to elbow
arthroscopy.
extension can be the first sign of elbow pathology in an adolescent,
often before any complaints of pain. In older patients with
degenerative changes, a loss of both flexion and extension is typical.
Lateral pain is seen in lateral epicondylitis and osteochondritis
dissecans. Medial pain is associated with chronic valgus laxity, ulnar
nerve symptoms, and medial epicondylitis. Posterior pain is typical of
posterior impingement and triceps tendinitis. Anterior pain is less
common and is associated with biceps tendinitis, anterior coronoid
osteophytes, and arthritis.
useful to determine at which stage of the throwing motion pain occurs.
Pain that occurs just before ball release when the arm is maximally
cocked is associated with valgus laxity and ulnar collateral injuries.
Pain after ball release is more often seen with posterior impingement
injuries.
the initial treatment along with the type and duration of physical
therapy. Arthrofibrosis after elbow trauma is one of the most common
abnormalities seen. An adequate course of physical therapy to try to
restore motion and strength is necessary before surgery. Review
previous surgeries with careful attention to whether the ulnar nerve
has been transferred. A previous ulnar nerve transposition does not
allow access to the medial portal and severely limits an arthroscopic
operative procedure.
measurement of the preoperative range of motion using a long goniometer
with the forearm in the same position for each measurement. Measurement
by eye alone may not pick up flexion contracture. Compare measurements
to those on the opposite side. Measure pronation and supination.
Tenderness and crepitation over the radiocapitellar joint or posterior
ulnahumeral articulation may indicate chondral injury in these areas.
An effusion may be detected by palpation of the lateral soft spot.
instability, valgus opening may be detected with the elbow flexed about
30° as a valgus force is applied to the forearm. This test may be
easier to perform with the patient supine and the humerus maximally
externally rotated, with the arm off the side of the table.
With the patient supine and the arm overhead and forearm in supination,
apply a supination and valgus force to the elbow in an axial direction
with it flexed 20° to 30°. Posterolateral subluxation will be visible
and will decrease with further flexion of the elbow.
Perform a valgus extension overload test by extending the elbow with a
valgus force applied across the joint. This procedure forces the
posteromedial olecranon to contact the humerus with impingement and
pain. This test is also often positive with ulnar collateral ligament
injuries.
position and whether it subluxes. (The nerve can be displaced over the
medical epicondyle, or, with flexion of the elbow, the nerve will slide
anteriorly.) This can be easily missed on physical examination. It is
easier to visualize subluxation of the nerve medially with the patient
supine.
(AP), lateral, oblique, and an axial view. Radiographs alone are
adequate to diagnose degenerative changes but may be completely normal
in cases of osteochondritis dissecans and loose bodies. Magnetic
resonance imaging (MRI) is useful to evaluate osteochondritis dissecans
and ligamentous injuries (29). The ulnar
collateral ligament is more easily visualized with either a contrast
MRI or a computed tomography (CT) arthrogram. Computed tomography
arthrography is also helpful to find loose bodies, but it is not
foolproof. In one series of patients with known loose bodies, the
preoperative radiographs were negative in 71% of the patients, and the
CT-arthrogram was negative in 38% (3).
removal of loose bodies, evaluation and treatment of osteochondritis
dissecans of the capitellum, and excision of osteophytes from the
coronoid and posterior olecranon. It is also indicated in release of
posttraumatic contractures of the elbow, synovectomy in inflammatory
disorders, and debridement of degenerative changes. It is useful in
evaluation of the ulnar collateral ligament and detection of valgus
instability as well as evaluation of the painful elbow with uncertain
intraarticular pathology.
ankylosis and severe fibrous capsular contracture, which can make
introduction of the arthroscope into the elbow joint difficult. An
acute capsular tear in the elbow is also a contraindication, as fluid
extravasation may occur that can collapse the joint; this makes
visualization difficult and, additionally, presents the danger of
compartment syndrome.
derangement. If the specific disorder is not known, a preoperative
intraarticular lidocaine injection can be useful to determine if pain
is relieved. Undertake an adequate course of conservative treatment
before surgery. Specific treatment guidelines are outlined with each
diagnosis.
-
Position the patient supine or prone,
depending on your preference and the portals to be used. I prefer to
use a general anesthetic because it offers complete muscle relaxation
and avoids intraoperative patient discomfort. In addition, it allows an
immediate postoperative neurologic examination in the recovery room,
which is not possible if a block is used. Apply a tourniquet around the
proximal arm before positioning and draping. For both the supine and
prone position, place the arthroscopy equipment on the opposite side of
the table from the surgeon. -
In the supine position, a standard operating table suffices. Place the hand in a gauntlet or suspension unit
P.2235
that is used for shoulder arthroscopy (Fig. 82.1).
Then suspend the arm overhead to hold the shoulder in neutral rotation
and 90° of abduction with the elbow flexed 90°. This position provides
maximal protection of the neurovascular structures in the antecubital
fossa. Use 5 lb of traction initially; when extension of the elbow is
needed to work in the posterior compartment, add another 3 to 5 lb.
Alternatively, prep the hand and suspend it with a sterile suspension
device or finger traps if you plan a later open procedure. In general,
for elbow arthroscopy, suspend the hand first and then sterilely prep
the elbow and cover the forearm with a towel and clear sticky drape. A
split drape works well for the supine position, and the arthroscopy
drapes with bags attached are useful in collecting fluid. Sit on a
rolling stool with the patient’s elbow at a comfortable level. This
arrangement allows access to both the medial and lateral sides of the
elbow and rotation of the forearm.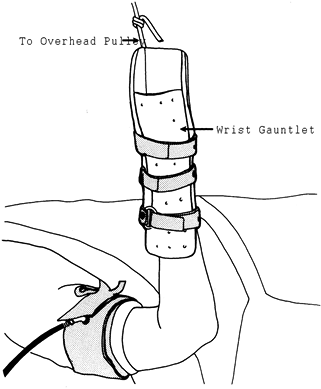 Figure 82.1.
Figure 82.1.
Setup and patient positioning for elbow arthroscopy. The affected arm
is statically suspended and positioned so that the elbow hangs freely
off the side of the table. -
If the patient is prone, support the chest and abdomen to avoid compression (20)
and place an arm board parallel to the operating table at the level of
the patient’s arm. Elevate the proximal arm and shoulder on a sandbag
placed on the arm board. No traction is required; gravity alone
distracts the elbow joint. The shoulder is in 90° abduction, and the
elbow flexed 90°, with the forearm pointed to the floor. The surgeon
then stands at the operating table with the elbow at chest level. -
There are many debates regarding the best
position for elbow arthroscopy. In general, operative arthroscopy in
the anterior compartment with release of the anterior capsule is easier
in the supine position. Advocates of the prone position cite the
greater ease of operating in the posterior compartment because the
surgeon is not fighting gravity with the arm in this position. If a
coupled videoarthroscope or “glass on glass” camera is not available,
the prone position is preferred to avoid fogging of the camera (when
the supine position is used, the fluid runs down the arthroscope and
can cause fogging of the camera). I prefer the supine position and
suggest that you select one position and develop proficiency with it.
The elbow is a very difficult joint to examine and treat
arthroscopically. It takes several cases before a reasonable level of
ease with the procedure is achieved.
elbow. The 4-mm, 30° arthroscope can be used throughout the procedure.
Visualization with the larger arthroscope is much better than with the
smaller 2.7-mm arthroscope. The 2.7-mm arthroscope is at times useful
in the tight lateral compartment. I use a standard-sized shaver
handpiece, with a 4.0-mm shaver tip; the smaller handpiece may be
needed in the lateral compartment. Other instruments needed include a
grasper for loose bodies and microfracture awls to abrade
full-thickness chondral defects. An arthroscopic system that allows the
camera and shaver to be placed through the same metal cannulas is very
helpful in preventing loss of a portal. If they are not available, use
switching sticks to change the position of the cannulas. Finally, an
arthroscopic fluid system is very useful in maintaining pressure in the
joint when the shaver is used. Two-portal arthroscopy can be used, as
the debrider can be used as outflow. A pressure setting of
approximately 30 to 35 mm Hg works well in the elbow joint. One ampule
of epipherine added to each 3,000-cc bag is also helpful in controlling
bleeding in the joint, in addition to the use of a tourniquet.
-
Outline the bony landmarks about the
elbow with a marking pen, carefully marking the location of the ulnar
nerve. With the hand covered and the elbow distended with fluid, it can
be difficult to locate the standard anatomic landmarks. Identify the
radial head as well as the medial and lateral epicondyles and the tip
of the olecranon. The most commonly used portals are the direct
lateral, anteromedial and anterolateral, posterolateral, straight
posterior, and proximal medial (used in the prone position) portals. -
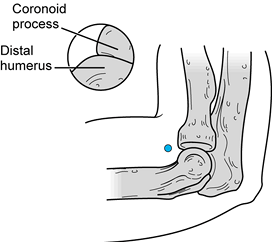
Locate the direct lateral portal among
the lateral epicondyle, olecranon tip, and the radial head in the soft
spot of the elbow (Fig. 82.2). This is a safe
portal, as instrumentation introduced through this portal traverses
only skin, a thin subcutaneous layer, the anconeus muscle, and joint
capsule (Fig. 82.3).![]() Figure 82.2.
Figure 82.2.
The direct lateral portal is located amid the lateral epicondyle,
olecranon tip, and radial head. (From Andrews JR, Carson WG.
Arthroscopy of the Elbow. Arthroscopy 1985;1:97.)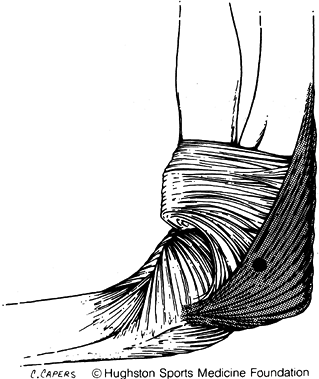 Figure 82.3. Instruments placed in the direct lateral portal penetrate the anconeus muscle before entering the joint capsule.
Figure 82.3. Instruments placed in the direct lateral portal penetrate the anconeus muscle before entering the joint capsule. -
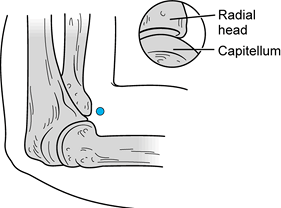
Locate the anterolateral portal approximately 2 to 3 cm distal and 1 cm anterior to the lateral epicondyle (Fig. 82.4).
Make this portal over the radiocapitellar joint just anterior to the
radial head, which is easily identified by pronating and supinating the
forearm. This portal goes through the extensor carpi radialis brevis
muscle and comes within 7 mm of the radial nerve (Fig. 82.5) (12). In an anatomic study, Lynch and associates (12)
found the radial nerve to be displaced 11 mm from the portal with 35 to
40 ml of fluid distention of the joint; without distention it is only 4
mm away.![]() Figure 82.4.
Figure 82.4.
Establish the anterolateral portal approximately 3 cm distal and 1 cm
anterior to the lateral epicondyle. Arthroscopic anatomy as seen
through this portal includes the distal humerus and the coronoid
porcess of the ulna. (From Andrews JR, Carson WG. Arthroscopy of the
Elbow. Arthroscopy 1985;1:97.) Figure 82.5.
Figure 82.5.
Instruments placed in the anterolateral portal penetrate the extensor
carpi radialis brevis muscle and pass within 7 mm of the radial nerve.
(From Chapman MW, ed. Operative Orthopaedics, 2nd ed. Philadelphia: JB Lippincott, 1993.) -
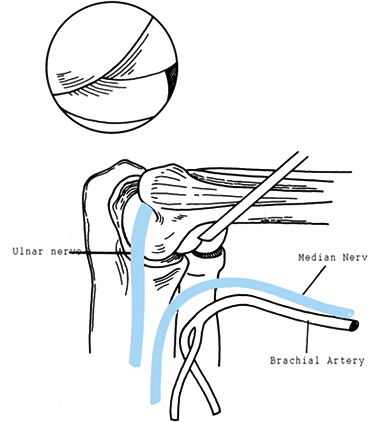
Locate the anteromedial portal approximately 2 cm distal and 2 cm anterior to the medial epicondyle (Fig. 82.6).
P.2237
Instruments in this portal pass through the tendinous portion of the
pronator teres and the radial aspect of the flexor digitorum
superficialis (Fig. 82.7). This portal comes within 1 cm of the median nerve and the brachial artery (12).
Lynch showed that the median nerve was an average of 4 mm from this
portal without distention and 14 mm with joint distention. The brachial
artery averaged 9 mm of displacement without and 17 mm with joint
distention.![]() Figure 82.6.
Figure 82.6.
The anteromedial portal. Instruments enter the skin approximately 2 cm
distal and 2 cm anterior to the medial epicondyle. The arthroscopic
view includes the capitellum and radial head. (From Andrews JR, Carson
WG. Arthroscopy of the Elbow. Arthroscopy 1985;1:97.)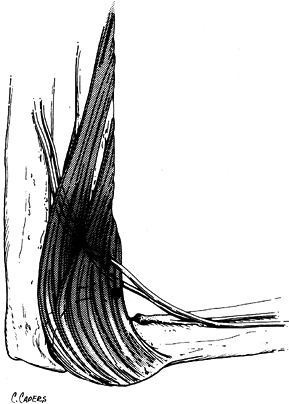 Figure 82.7.
Figure 82.7.
Instruments passed in the anteromedial portal penetrate the tendinous
portion of the pronator teres and the radial aspect of the flexor
digitorum digitalis. -
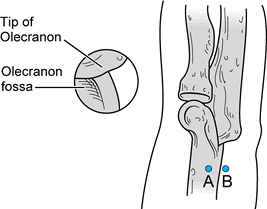
Establish the posterior portals with the
elbow in slightly more extension, which relaxes the triceps muscle and
allows the posterior joint to be distended. The posterolateral portal
is approximately 3 cm proximal to the olecranon tip, just off the
lateral epicondylar ridge posterior and proximal to the lateral
epicondyle (Fig. 82.8 and Fig. 82.9). The second posterior portal is the straight or working portal. It is used if there is need for a second
P.2238
operating portal posteriorly. Place it in the middle portion of the
triceps tendon, splitting the triceps in line with its fibers. Take
care to avoid too medial positioning of this portal, as the ulnar nerve
is close. This portal comes within 18 mm of the ulnar nerve (12). I do not incise medial to the midpoint of the triceps tendon.![]() Figure 82.8. With the elbow in 20° to 30° of flexion, (A) the posterolateral portal is established 3 cm proximal and 2 cm medial to the triceps tendon, and (B) the straight posterior portal is established 3 cm proximal to the olecranon tip and 2 cm medial to the posterolateral portal.
Figure 82.8. With the elbow in 20° to 30° of flexion, (A) the posterolateral portal is established 3 cm proximal and 2 cm medial to the triceps tendon, and (B) the straight posterior portal is established 3 cm proximal to the olecranon tip and 2 cm medial to the posterolateral portal. Figure 82.9.
Figure 82.9.
Instruments placed in the posterolateral portal pass just lateral to
the triceps tendon. Instruments in the straight posterior portal split
the triceps tendon in line with its fibers. -
Place the proximal medial or the supracondylar anteromedial portal with the patient in the prone position (20).
This portal is located 2 cm proximal to the medial epicondyle. Incise
the skin and insert the cannula anterior to the intermuscular septum,
avoiding injury to the ulnar nerve (Fig. 82.10).
With the cannula directed toward the radial head, maintain contact with
the anterior humerus, which protects the median nerve and the brachial
artery (Fig. 82.11).![]() Figure 82.10. Medial view of the left elbow. The proximal medial portal is used in the prone position.
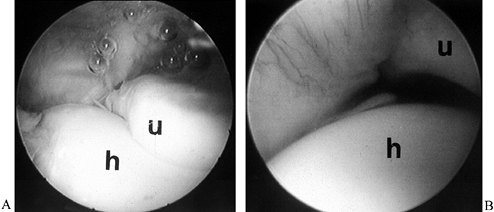
Figure 82.10. Medial view of the left elbow. The proximal medial portal is used in the prone position.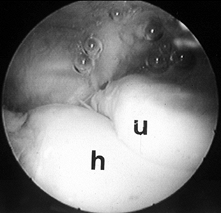 Figure 82.11. Arthroscopic view of the ulna (u) and humerus (h) in anterior compartment from the anterolateral portal.
Figure 82.11. Arthroscopic view of the ulna (u) and humerus (h) in anterior compartment from the anterolateral portal.
-
After identifying the bony landmarks,
inflate the tourniquet. I insert an 18-gauge needle into the soft spot,
in the area of the direct lateral portal, aimed directly at the center
of the joint. Then distend the elbow with approximately 30 to 40 ml of
fluid, using intravenous tubing and a 50-ml syringe. The IV tubing
allows for an easier injection. Confirm entry into the joint by the
visible distention of the joint and the free backflow of fluid from the
needle. Leave this needle in place with pressure applied to the syringe
to distend the joint. Maximal distention of the joint displaces the
antecubital neurovascular structures into a more anterior position,
providing a safety margin. -
Place a second spinal needle for the
anterolateral portal. The angle of this needle is then used as a guide
for directing the cannula into the joint. Incise the skin only with a
#11 blade; do not penetrate deeper to avoid damage to subcutaneous
nerves. Use a staight hemostat to spread the tissues to the level of
the joint capsule. Enter the joint with a blunt trocar. Because the
capsule is trapped between the radial head and the capitellum, a change
in angle is required toward the center of the joint once the trocar has
passed over the radial head. Otherwise, the trocar has a tendency to
track across the joint and enter in a more medial position, which makes
visualization difficult. Direct the blunt trocar down toward the
humerus. Palpate the medial epicondyle as the cannula is introduced; it
stabilizes the arm and also serves as a point of reference. Once the
cannula is in the joint, insert the arthroscope into the sheath without
the fluid flowing in order to confirm an intraarticular location. -
With the arthroscope in the anterolateral portal, visualize the coronoid, humerus, and a portion of the radial head (Fig. 82.11).
With extension of the elbow, the view of the trochlea of the humerus is
improved. Take care not to pull the arthroscope out of the joint when
attempting visualization of the radial head. Once a portal is
established, leave a cannula in the portal to prevent extravasation of
fluid. -
Then establish the anteromedial portal
under direct arthroscopic visualization. This method is preferred to
the use of an inside-out switching stick, as it allows for better
control in placing the portal. Insert an 18-gauge
P.2239
spinal
needle at a point 2 cm distal and 2 cm anterior to the medial
epicondyle. When it is inside the joint, bring the needle over the
humerus just above the articulation between the coronoid process and
the humerus. Use the needle to test the optimal angle for the shaver.
The portal needs to be made anterior enough to allow the shaver to be
brought down onto the humerus if any debridement or anterior capsular
release is anticipated. Make this portal in the same fashion as the
anterolateral portal, with an incision in only the skin layer, and
blunt dissection to the level of the joint capsule. Insert the cannula
into the joint under direct visualization. With the arthroscope in the
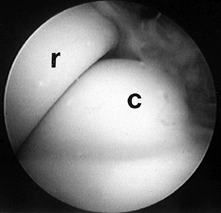
anteromedial portal, it is easy to visualize the radial head and
capitellum (Fig. 82.12).
Pronation and supination of the forearm provides additional
visualization of the radial head. The coronoid process can also be seen
if the scope is carefully withdrawn from the joint. The ulnar-radial
articulation can be inspected through this portal. Small loose bodies
are often found in this location. The anteromedial portal is critical
for viewing the radial head, as visualization of the radial head from
the anterolateral portal is very poor.![]() Figure 82.12. Arthroscopic view of the radial head (r) and the capitellum (c) from the anteromedial portal.
Figure 82.12. Arthroscopic view of the radial head (r) and the capitellum (c) from the anteromedial portal. -
Next establish a direct lateral, or “soft
spot” portal. Use a #11 blade to incise the capsule. Make the initial
portal just off the center of the soft spot to help establish a second
working portal in the lateral compartment. Use a straight hemostat in
the portal to spread the capsule. Place a blunt trocar into the portal
and direct it toward bone. Once bone is contacted, change the direction
of the cannula to parallel the lateral capsule, which points the
cannula toward the ceiling. This technique allows the edge of the
cannula to enter the joint, so that when the trochar is withdrawn, the
cannula will remain inside the capsule. The lateral compartment is
tight, and the small 2.7-mm arthroscope may be helpful. Through the
straight lateral portal, the radial head, capitellum, articulations of
both the trochlea and olecranon, and the ulna are visualized. The
landmark of the lateral compartment is the articulation of the “three
bones” (Fig. 82.13).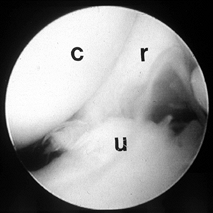 Figure 82.13. Arthroscopic view of the lateral compartment including the capitellum (c), radial head (r), and ulna (u), as seen from the straight lateral, or soft spot, portal.
Figure 82.13. Arthroscopic view of the lateral compartment including the capitellum (c), radial head (r), and ulna (u), as seen from the straight lateral, or soft spot, portal. -
Then establish a working portal in the
lateral compartment. Introduce a spinal needle. Arthrofibrosis in a
joint can be difficult to visualize. It is possible at times to place
the shaver in the portal and then look for the movement in the
synovium. Take care to avoid scuffing the cartilage. Once the shaver is
visualized, place it slightly ahead of the arthroscope. The arthroscope
can then follow the shaver down the olecranon curve to enter the
posterior compartment. If the shaver is not used to clear the synovium
in this area, it can be difficult to follow the curve of the ulna into
the posterior compartment. -
Once the arthroscope is at the tip of the
olecranon viewing in the posterior direction from the direct lateral
portal, introduce an 18-gauge spinal needle through the posterolateral
portal. With supine arthroscopy, the needle is directed almost toward
the ceiling. After it is correctly positioned, use a #11 blade to make
the portal, entering the capsule while visualizing the blade with the
arthroscope. Use a hemostat to spread the capsule, and introduce the
cannula into the portal site. The olecranon tip, the posterior
olecranon fossa, and the posterior trochlea are visualized from this
portal. Loose bodies are frequently encountered posteriorly in the
olecranon fossa. The posteromedial olecranon osteophyte is seen, as
well as chondral defects posteriorly. -
If a second operative portal is required
posteriorly, make a straight posterior portal under direct
visualization. Place an 18-gauge spinal needle at the level of the
P.2240
tip
of the olecranon and pass it straight through the triceps, in the
middle portion of the tendon. The needle can be used to confirm that
the areas the shaver needs to reach will be accessible through this
portal. Insert a #11 blade in line with the fibers of the triceps
tendon. The posterior capsule can be difficult to enter, especially if
there is a thickened olecranon bursa. Use a hemostat to expand the
portal site. Once the portal is established, loose bodies can be
removed, and debridement of posterior olecranon osteophytes can be
performed as well as synovectomy of the posterior compartment. The
ulnar nerve rests against the posteromedial capsule; exercise great
care when shaving in the posteromedial area. Keep the back side of the
shaver against this capsule, never allowing the mouth of the shaver to
work against the capsule.
most common arthroscopic procedures. Osteocartilaginous bodies are
usually the result of osteochondritic lesions of the capitellum,
osteochondral fractures of the radial head, and synovial diseases, such
as synovial chondromatosis. The patient usually complains of catching
and locking in the elbow, and a joint effusion may develop after a
painful episode. Radiographs, CT-arthrograms, and MRI all may be
negative preoperatively. The procedure is usually undertaken more on
the basis of clinical findings than the results of imaging studies. It
is important to obtain consent for a possible arthrotomy, as it may not
be possible to remove the fragment arthroscopically.
when searching for loose bodies, as defects from the anterior and
lateral compartments can frequently lodge in the posterior compartment.
The loose body may be drawn into view by using the shaver with full
suction. If one loose body is encountered, make a careful search for
others. In the anterior compartment, loose bodies are more easily
removed through the lateral portal. If a large piece is too big to pull
through the portal, it can be removed in piecemeal fashion. The
Schlessinger grasper is useful for breaking a loose body into pieces,
or a shaver can be used to break up the large fragment.
patient that other loose bodies may have been left behind in the joint
and, in addition, that new loose bodies may form (28).
This is often the case in the throwing athlete, who continues to
subject the joint to repetitive microtrauma. Once the portals are
healed, start the patient on range-of-motion exercises and a
strengthening program. Most athletes are ready to start throwing at 6
to 8 weeks after surgery. Several studies have shown the benefits of
removal of loose bodies from the elbow, especially in the joint free of
degenerative changes (5,8,17,18).
forearm about the elbow results in compression of the lateral joint. In
the skeletally immature, osteochondritis dissecans can result, which is
usually seen in throwing athletes or gymnasts (4,10,21).
The patient usually has a flexion contracture, locking episodes caused
by loose bodies, and pain, with decreased ability to participate in
sports.
anteromedial portal initially. The best visualization of the typical
osteochondritis lesion, however, is from the soft spot, or straight
lateral portal. Once the synovial tissue is debrided, locate the
chondral defect. It is usually soft, and there may be a large flap of
cartilage. A small (3.5 mm) shaver is useful both to probe and to
debride the lesion. Use forceps or a small knife to debride the crater,
and once the cartilage flaps are removed, use awls to microfracture the
subchondral bone in an attempt to heal the area with fibrocartilage.
Braungaraten et al. advise against attempting to reattach the fragment (4).
After debridement, younger athletes are usually able to return to full
activity, but older patients have less successful results (4,19,21).
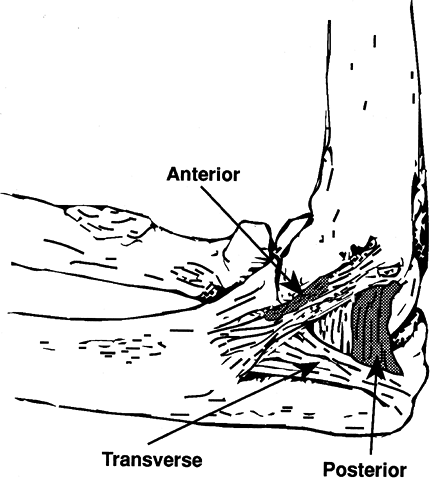
of elbow pain is the formation of a posteromedial osteophyte on the
olecranon, resulting in impingement and chondromalcia on the trochlea (1).
The forces of throwing place a valgus force across the medial elbow,
and with ball release a forced extension occurs. The combination of
this valgus and extension force is referred to as “valgus extension
overload syndrome” (22,30).
In 72 professional baseball players requiring arthroscopy, 65% had
posterior olecranon osteophytes requiring debridement, which was the
most commonly performed procedure (3).
during the throwing motion, especially after ball release. Physical
examination typically reveals slight loss of full extension, and valgus
and extension loading cause pain. Ulnar nerve symptoms may also be
present. Assess the stability of the ulnar collateral ligament. Medial
instability increases the valgus force across the elbow, and
osteophytes may form in response to medial laxity. Routine radiographs
are often normal. The osteophyte may be seen on an axial view (1) or on MRI. The diagnosis is usually based on the clinical history and the findings on physical examination.
posterior trochlea can be very difficult to see without the arthroscope.
-
Position the patient supine and place the
arthroscope in the posterolateral portal with the elbow in
approximately 30° of flexion. Use a cannula in this portal because
fluid extravasation can make it difficult to find the portal again.
Make a second working portal and bring a shaver in through this portal. -
Initially debride the synovitis
posteriorly in order to improve visualization. Then use a burr or
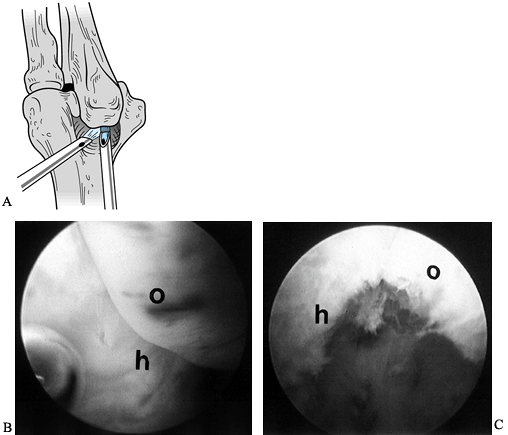
shaver to debride the posterior olecranon osteophyte (Fig. 82.14).
It is important to completely remove the posteromedial corner of the
osteophyte, but the ulnar nerve is very close to this location; take
care to keep the open side of the shaver away from the nerve.![]() Figure 82.14. A:
Figure 82.14. A:
A diagram of debridement of a posteromedial olecranon osteophyte. The
camera is in the posterolateral portal, with the burr in the straight
posterior portal. B: Arthroscopic view of the posterior compartment with olecranon osteophyte (o) and humerus (h). C: Arthroscopic view after debridement of the olecranon osteophyte. -
The question is how much of the osteophyte should be removed. When this operation was initially developed (1),
a relatively generous excision of the osteophyte was recommended. In
more recent years, however, less aggressive excision has been adopted
because excessive debridement increases the stress on the ulnar
collateral ligament. Typically 4 to 5 mm is removed, or enough to
debride the loose fragments and prevent further impingement. If there
is a chondral defect on the trochlea, use a burr to debride the lesion
to stimulate bleeding and fibrocartilage formation. -
Once the portals are healed, start
range-of-motion exercises, followed by a strengthening program.
Athletes are usually able to return to an early throwing program by 6
to 8 weeks after surgery, but it may take 4 to 6 months for complete
recovery.
there is a high rate of reoperation because of recurrence of the
posteromedial osteophyte. In addition, 25% of the athletes who
initially had debridement of the posterior osteophyte required an ulnar
collateral ligament reconstruction. It is important to carefully assess
the integrity of the ulnar collateral ligament in the presence of a
posterior osteophyte. In athletes who continue to throw, this procedure
is palliative and does not solve the underlying problem of overstress.
subject to large forces. The anterior bundle of the ulnar collateral
ligament is the primary stabilizer against valgus stress (9,13,23). Injuries to this ligament are usually the result of repetitive microtrauma (27); less commonly, sudden severe trauma can result in an acute tear. Maximum valgus instability occurs at 70° of elbow flexion (23) after
sectioning of the anterior bundle of the ulnar collateral ligament
(UCL). This instability can be difficult to detect clinically. It may
be that the high forces of throwing are required to cause the painful
symptoms.
Only the anterior 20% to 30% of the anterior bundle and the posterior
30% to 50% of the posterior bundle are visualized, using both anterior
and posterior portals (Fig. 82.15). A complete
tear of the anterior bundle of the UCL can be missed during
arthroscopy. With a ligament injury, however, laxity will result that
can then be visualized arthrosocpically (27).
 |
|
Figure 82.15.
The portion of the ulnar collateral ligament that is visible arthroscopically. (From Timmerman LA, Andrews JR. The histologic and arthroscopic anatomy of the ulnar collateral ligament of the elbow. Am J Sports Med 1994;22(5):667.) |
visualized are the coronoid process and the trochlea. With the humerus
stabilized, apply a valgus force to the forearm and assess the
resulting opening between the humerus and olecranon (Fig. 82.16; see also COLOR FIG. 82.16).
Normally there is no, or minimal (less than 1 mm), opening in the
ulnohumeral joint. With injury to the UCL an increase in opening is
seen, and with a complete large tear the arthroscope itself may be
placed between the ulna and humerus. Reconstruction of the UCL may be
indicated when the typical history and physical findings are present, a
course of conservative treatment fails, and increased valgus opening of
the joint is seen on arthroscopy.
 |
|
Figure 82.16. (See COLOR FIG. 82.16) A: An arthroscopic view from the anterolateral portal in a right elbow of the humerus (h) and the ulna (u). B: With valgus stress applied, the increase in space between the ulna and the humerus is seen.
|
the forearm bones subluxate as a unit on the humerus in a pivot-shift
fashion. A stress examination at the time of arthroscopy is useful to
see this abnormal intraarticular movement (Fig. 82.17; see also COLOR FIG. 82.17).
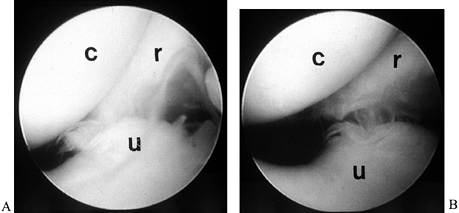 |
|
Figure 82.17. (See COLOR FIG. 82.17) Arthroscopic view of the lateral compartment, demonstrating posterolateral subluxation of the forearm bones on the humerus. A: No stress. B: With stress. c, capitellum; r, radius; u, ulna.
|
elbow joint that can be very difficult to treat. It is seen most
commonly after an intraarticular fracture or dislocation. A
nondisplaced radial-head fracture can result in significant elbow-joint
contracture (6). Immobilization of the elbow,
usually in 90° of flexion, is associated with the formation of fibrous
bands in the anterior elbow. Although it is often stated that an arc of
motion between
30° and 100° of flexion is required for functional activities of the elbow (14);
for some activities, particularly in athletes, a flexion contracture of
10° to 20° may be symptomatic. Arthroscopic debridement of
arthrofibrosis of the elbow can be successful (6,11,15,25).
-
The elbow must have at least 50° to 60°
of motion for arthroscopic debridement to be considered. It may be
difficult to inject fluid into the joint. Maintain pressure on the
syringe as you make the anterolateral portal. Direct the trocar toward
the humerus and take care not to pull the cannula back as the trochar
is removed. Instead, advance the cannula slightly so that it stays
inside the capsule. Then introduce the scope, looking for articular
cartilage to confirm entry. If articular cartilage is not visualized,
redirect the trochar. Once articular cartilage is seen, establish a
second working portal medially. Use a switching stick to do so if the
spinal needle is not visible. -
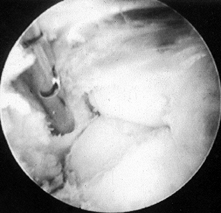
Bring in a shaver through the medial
portal. Keep the open side of the debrider pointing toward the humerus.
Release the anterior capsule and debride adhesions from the humerus. If
the capsule is thickened, direct the shaver anteriorly with caution and
debride this tissue (Fig. 82.18; see also COLOR FIG. 82.18).![]() Figure 82.18. (See COLOR FIG. 82.18) Arthroscopic view of arthrofibrosis in the anterior compartment.
Figure 82.18. (See COLOR FIG. 82.18) Arthroscopic view of arthrofibrosis in the anterior compartment. -
Once the humerus is visualized, use
either the shaver or a small burr to re-form the anterior radial and
olecranon fossae. The arthroscope and shaver can be interchanged, but
take care not to withdraw the cannulas from the joint. It is easy to
lose a portal and often difficult to reestablish it. -
Once the anterior tissues have been
released, debride the lateral compartment. Then visualize through the
posterolateral portal and debride the posterior compartment through the
straight lateral portal. Even though most of the scarring may seem to
be in the anterior compartments, significant scarring can be found
posteriorly, with the olecranon fossa completely filled in. This
condition prevents full extension. In a difficult case, soft-tissue
swelling or lack of tourniquet time may preclude complete posterior
debridement, which can be done at a second procedure. Once the
arthroscopy is completed, manipulate the elbow to gain range of motion,
which is documented with a sterile goniometer. -
Postoperatively, start gentle motion
immediately; once the portals are healed (usually 4–5 days), pursue an
active mobilization program. Usually a 50% improvement in motion can be
expected. It may take 3 to 4 months before the patient is able to
achieve the motion that is achieved on the operating table.
it is usually the result of previous trauma or longstanding overuse.
Typical complaints are of pain, loss of motion, and catching and
locking. Radiographs usually demonstrate degenerative changes,
including loss of joint spaces and formation of osteophytes. Large
coronoid osteophytes can impinge anteriorly, preventing flexion, and
posterior olecranon osteophytes can impinge and prevent extension.
Loose bodies can cause locking or can block motion.
elbow joint is similar to that described for arthrofibrosis. More bony
work is usually required with degenerative arthritis, with emphasis on
removing the osteophytes that impinge. A small ¼-in. osteotome is often
useful; it can be introduced through the portal to remove large pieces
of bone. A burr that fits through the cannula may be preferred to
prevent loss of the portal site. The associated synovitis and capsular
contractures can also be debrided. Caution the patient preoperatively
that the procedure is palliative and that symptoms may recur.
Treat rheumatoid arthritis involving the elbow arthroscopically; it may
be easier to enter the joint in these cases, as the capsule tends to be
lax and enlarged. Perform the synovectomy using the usual portals.
Occasionally a synovial band will thicken in the elbow, creating
symptoms of popping and catching (7), which are
usually seen laterally and are referred to as a lateral band or plica.
This thickening can result in impingement on the radial–capitellar
joint, resulting in persistent lateral elbow pain. Its symptoms can be
confused with those of lateral epicondylitis. The lesion can be
visualized and debrided arthroscopically. Take care not to excessively
debride the lateral capsule, including the annular and lateral
collateral ligaments, to prevent destabilizing the joint.
 |
|
Figure 82.19. (See COLOR FIG. 82.19) Arthroscopic examination of the anterior lateral compartment with extensive inflammatory synovitis.
|
suture, using a nylon in the skin or a subcutaneous absorbable suture.
It can be difficult to apply Steri-Strips, as extensive soft-tissue
swelling is often present. Injection of the joint with morphine helps
postoperative pain. It is preferable not to inject a local anesthetic
until after a neurologic examination can be completed in the recovery
room; the agent can extravasate from the joint and produce a nerve
palsy.
compression ice dressings designed for the knee work well on the elbow,
with the olecranon placed in the same area as the patella. If the
patient is excessively uncomfortable in the recovery room, use an
axillary block before discharge. A short course of antibiotics may be
desirable if significant posterior debridement was performed, as the
posterior triceps portal can sometimes drain excessively.
immediately and to work on gentle range of motion with the soft
dressing in place. Increase motion as tolerated, with emphasis on
maintaining extension and flexion. Once inflammation and swelling have
subsided, initiate strengthening exercises. Initially use 1-lb weights,
increasing gradually to a 5-lb weight; subsequently increase
repetitions rather than increasing the weight.
but familiarity with the procedure and careful patient selection
improve the surgeon’s ability.
common to all surgical procedures. They do not appear to occur at an
increased rate in elbow arthroscopy. Occasionally persistent draining
from a portal occurs, usually the posterior portal. Considerable
soft-tissue swelling occurs posteriorly when both posterior portals are
used, and the fluid can collect in the olecranon bursa. Treat this
condition with immobilization and oral antibiotics.
completed, insert a blunt trocar into the portal to prevent fluid from
leaking out. Placement of the trocar also allows return to these portal
sites later if needed.
familiar with use of this position. I find it easier to work in the
anterior compartment with the patient supine, and it is not different
to do posterior debridement and inspection of the radiocapitellar
articular in the supine position. If I plan an open procedure, I use
the supine position to avoid having to reposition the patient.
elbow is the most difficult joint to arthroscope, but skills improve
considerably with experience. Among the most satisfied patients I have
treated are those with arthrofibrosis of the elbow. They report
improvement of both pain and function (25). A
close second in patient satisfaction—although the procedure is less
common—is the group of adolescents treated by debridement of
osteochondritis dissecans. These patients typically regain range of
motion quickly and are throwing at approximately 3 months. Removal of a
loose body is the easiest operative procedure to perform, although an
isolated loose body is not often present without another associated
disorder, such as a posteromedial osteophyte or arthrofibrosis. The
most difficult procedures to perform are debridement of extensive
arthrofibrosis and debridement of a posteromedial olecranon osteophyte.
probably the treatment of choice for several disorders discussed above.
The major advantages of improved visualization and more rapid
rehabilitation are tempered by the difficulty of the procedure and the
remote risk of significant neurologic damage. Meticulous technique as
outlined above gives the best assurance of a satisfactory outcome.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
TE, Andrews JR, Satterwhite YE. The arthroscopic classification and
treatment of osteochondritis dissecans of the capitellum. Am J Sports Med 1998;26:520.
KD, Shall LM. Arthroscopic Release of a Posttraumatic Flexion
Contracture in the Elbow: A Case Report and Review of the Literature. Arthroscopy 1992;8:544.
JD, Neff RS, Shall LM. Compression Neuropathy of the Radial Nerve as a
Complication of Elbow Arthroscopy: A Case Report and Review of the
Literature. Arthroscopy 1988;4:284.
LA, Schwartz ML, Andrews JR. Preoperative Evaluation of the Ulnar
Collateral Ligament by Magnetic Resonance Imaging and Computed
Tomography Arthrography. Evaluation in 25 Baseball Players with
Surgical Confirmation. Am J Sports Med 1994;22:26.