Bite to the Hand
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Bite to the Hand
Bite to the Hand
Dawn M. LaPorte MD
Chris Hutchins MD
Description
-
Hand bites (direct or indirect) are
serious injuries that, if not managed correctly, may result in
substantial morbidity to the hand. -
A direct bite to the hand, such as a dog bite or intentional human bite, can occur in any location.
-
The more common “clenched-fist” (or
indirect) injury occurs over the MCP joint (the knuckle) when a fist
strikes an opponent’s mouth.-
This seemingly benign injury is, in fact, treacherous and, unfortunately, common.
-
A tooth may lacerate the extensor tendon, the joint capsule, or the joint itself.
-
As the digit is straightened, the underlying wound is obscured by normal soft tissue.
-
-
Classification:
-
Minor: Small puncture wound
-
Major: Large lacerations and soft-tissue damage (2–5 cm, exposed bone or cartilage, tendon rupture)
-
-
Synonyms: Clenched fist injury; Fight bite; Dog or cat bite
General Prevention
-
Little can be done in terms of prevention
for direct or indirect bites except to counsel patients about avoiding
unknown animals and fighting, respectively. -
Complications may be minimized by
recognizing the human bite wound as a serious injury and treating with
early irrigation, débridement, and appropriate antibiotics (1).
Epidemiology
Incidence
-
Common
-
>1 million dog bites reported annually
Risk Factors
-
Alcohol abuse
-
Fighting
Etiology
-
Fist fights
-
Dog or cat exposure
Associated Conditions
Fractures
Signs and Symptoms
-
Signs:
-
Puncture or laceration to the hand is present.
-
Associated swelling and erythema may be present.
-
Cellulitis and lymphangitis are present if an infection occurs.
-
If a tendon has been lacerated, the patient may experience difficulty with finger extension.
-
-
Symptoms:
-
Decreased hand function, such as difficulty with grasping or moving an individual digit
-
Pain
-
History
Many combatants are embarrassed or hesitant to admit
injury to this region or the mechanism of injury and consequently
present late for evaluation and treatment.
injury to this region or the mechanism of injury and consequently
present late for evaluation and treatment.
Physical Exam
-
Examine the hand closely for any sign of
skin puncture, particularly over the 3rd and 4th MCP joints in
instances of clenched-fist injuries. -
Assess the motor, sensory, and vascular status of the hand and digits.
-
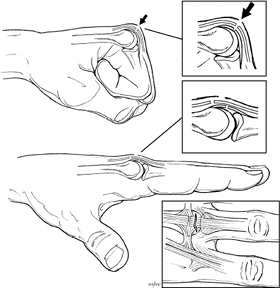
If the injury is of a clenched-fist type,
have the patient make a fist, if possible; this procedure may reveal
the underlying soft-tissue damage and may facilitate deep wound
inspection. -
In clenched-fist injuries, the damage to
underlying structures is proximal to the skin wound when the fingers
are in the extended, anatomic position (Fig. 1).
 |
|
Fig.
1. With a bite to the hand, the extensor injury usually is proximal to the skin laceration because the MCP joint is flexed at the time of injury. |
Tests
Lab
Cultures in the acute period before surgical débridement are unlikely to be helpful.
Imaging
-
Obtain radiographs of the hand to assess for fracture and tooth fragments.
-
In subacute presentations, look for osteomyelitis.
Differential Diagnosis
Any puncture wound over the MCP joints must be regarded with great suspicion and treated as a clenched-fist–type bite injury.
General Measures
-
If the patient has not been immunized within the past 10 years, tetanus toxoid should be administered.
-
The most important therapeutic
interventions are aggressive irrigation and débridement, to remove all
devitalized tissue and to irrigate the wound copiously with normal
saline solution, povidone-iodine (Betadine), or both. -
The wound may need to be extended surgically to facilitate exposure of the injured tissue.
-
In clenched-fist injuries, the skin wound is distal to the zone of deeper injury.
-
After irrigation and débridement, the wound should be packed, and the hand should be immobilized and elevated.
-
Do not suture bite wounds.
-
Antibiotics should be commenced
(amoxicillin [Augmentin] is a reasonable 1st line agent) and should be
continued for 5–7 days in the absence of overt infection. -
At 24 hours, the packing should be removed, the patient should be reexamined, and warm soaks should be started.
-
If infection is present, the wound should
undergo repeat irrigation and débridement, and the patient should be
admitted for parenteral antibiotic therapy. -
For patients presenting late to
evaluation and treatment, and for those in whom infection is manifest,
urgent irrigation and débridement followed by parenteral antibiotics
are essential. -
Immediate referral to a hand specialist
should be considered for any patient presenting >24 hours after the
initial injury, for those who have infected wounds, and for those who
have sustained injury to the tendon, capsule, joint, or bone.
P.39
Special Therapy
Physical Therapy
-
Physical therapy is not necessary in the acute period.
-
At 1 week after treatment, ROM exercises should be started to prevent stiffness (especially of the MCP joints).
Medication (Drugs)
First Line
-
More than 40 bacterial species have been isolated from infected bite wounds.
-
The most common organisms are Eikenella corrodens and group A Streptococcus species in human bite wounds and Pasteurella multocida, S. aureus, and Bacteroides in animal bite wounds (2–4).
-
Augmentin provides satisfactory coverage for all organisms.
-
Treat infection empirically with intravenous antibiotics for 48 hours, then adjust based on cultures.
Surgery
-
Irrigation and débridement consist of cleaning infected tissues and removing devitalized tissues.
-
Cultures should be obtained.
-
Wounds should be left open and managed with dressing changes.
-
Extensor tendon injury should not be repaired until infection resolves.
Prognosis
Prognosis usually is good if infection is avoided or treated early.
Complications
-
Infection: Both soft tissue and bone
-
Stiffness
-
Pain
-
Extensor tendon injury
Patient Monitoring
-
At 24 hours, the packing should be changed.
-
The patient should be followed closely until the wound shows satisfactory healing with no evidence of infection.
-
When doubt exists about the stability of the wound, the patient should be followed at 24–48-hour intervals.
References
1. Mennen U, Howells CJ. Human fight-bite injuries of the hand. A study of 100 cases within 18 months. J Hand Surg 1991;16B:431–435.
2. Dire DJ. Emergency management of dog and cat bite wounds. Emerg Med Clin North Am 1992;10:719–736.
3. Garcia VF. Animal bites and Pasturella infections. Pediatr Rev 1997;18:127–130.
4. Talan DA, Citron DM, Abrahamian FM, et al. Bacteriologic analysis of infected dog and cat bites. N Engl J Med 1999;340:85–92.
Additional Reading
Abrams RA, Botte MJ. Hand infections: treatment recommendations for specific types. J Am Acad Orthop Surg 1996;4:219–230.
Baratz ME, Schmidt CC, Hughes TB. Extensor tendon injuries. In: Green DP, Hotchkiss RN, Pederson WC, et al., eds. Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier Churchill Livingstone, 2005:187–217.
Siverhus DJ, Stern PJ. Avoiding complications of human bite injuries. J Musculoskelet Med 1996;13:32–36, 43.
Stevanovic MV, Sharpe F. Acute infections in the hand. In: Green DP, Hotchkiss RN, Pederson WC, et al., eds. Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier Churchill Livingstone, 2005:55–93.
Codes
ICD9-CM
882.1 Wound hand complicated
Patient Teaching
-
Patients are instructed in cases of open wounds to watch for signs of infection.
-
Open packing
-
Soaking
-
ROM
-
Redness
-
Pain
-
Fever
-
Drainage
-
Inability to move finger
-
FAQ
Q: What are the most important treatment interventions in a bite to the hand?
A:
The 1st priority is prevention of infection, which consists of prompt
surgical exploration with irrigation and débridement of the joint and
treatment with intravenous antibiotics.
The 1st priority is prevention of infection, which consists of prompt
surgical exploration with irrigation and débridement of the joint and
treatment with intravenous antibiotics.
Q: When should an extensor tendon laceration secondary to a bite wound be repaired?
A: In this setting, repair of the extensor tendon can be delayed 7–10 days until the infection is resolved.
