CHAPTER 3 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
Section – Surgical Techniques for Shoulder Instability
CHAPTER 3 – Suture Anchor Fixation for Shoulder Instability
Brett D. Owens, MajorMD
Recurrent anterior glenohumeral instability is a common sequela of traumatic glenohumeral dislocation or subluxation. The major pathoanatomic features of a traumatic dislocation are the capsulolabral avulsion of the inferior glenohumeral ligament (Bankart-Perthes lesion) and capsular redundancy, which typically worsens with repeated injuries. [1] [5] [6] [17] [19] Once recurrent instability affects activities of daily living or precludes return to sporting activities, operative stabilization is typically recommended. However, there is still considerable debate about when to proceed with surgery after the first traumatic dislocation. The orthopedic literature supports early acute arthroscopic stabilization after a traumatic dislocation in a select group of young athletes who are at high risk for repeated shoulder injuries, ostensibly to decrease the risk of recurrence compared with traditional nonoperative management. [2] [3] [4] [7] [8] [14] However, patient issues such as player position, time remaining in a season, and time available for rehabilitation may affect the decision of when to undergo surgery.
Before the introduction of arthroscopic techniques in the mid-1980s, shoulder stabilization surgery necessitated a formal deltopectoral approach, through which the subscapularis was either released from its humeral insertion or split longitudinally for access to the glenohumeral joint. The initial technique to reattach the avulsed labrum to bone was through bone tunnels; however, following their introduction in the 1980s, suture anchors quickly became the most commonly used soft tissue repair devices. With the introduction of arthroscopic shoulder techniques, the number as well as the different varieties of fixation devices has exploded.
Arthroscopic shoulder stabilization offers a number of advantages over traditional open repairs. These include smaller incisions, less muscle dissection, less postoperative pain, and better visualization of the entire glenohumeral joint.[10] The first arthroscopic Bankart repairs were performed by transglenoid suture fixation. Sutures were passed across the glenoid and tied over the posterior fascia. As bioabsorbable polymers were developed for use in the shoulder, soft tissue fixation with tacks became popular. The tacks can be inserted arthroscopically over a guide wire to ensure correct placement. Although they are still in use, the tacks have been shown to have limited pullout strength and have for the most part been abandoned for shoulder stabilization. The success of metallic suture anchors in open shoulder surgery led to the development of arthroscopic deployment techniques. Development of longer-lasting polymers and much stronger suture made bioabsorbable anchors the most popular choice for soft tissue repair. The goal of any suture anchor is to repair soft tissue to bone and be able to withstand the forces required for rehabilitation until the normal bone-to-tissue interface is restored. The focus of this chapter is on the technique of arthroscopic anterior shoulder stabilization with use of suture anchors.
It is essential to establish an accurate diagnosis. Important information to elicit includes mechanism of initial injury, frequency and mechanism of dislocation or subluxation episodes, presence of instability during activities of daily living, and prior surgeries.
Recurrent anterior instability typically presents with a limitation of shoulder function due to a subjective feeling that the shoulder is “slipping out of the joint.” For anterior instability, shoulder abduction with external rotation most commonly reproduces these symptoms.
Many shoulder dislocations are reduced by athletic trainers, coaches, or emergency department personnel. The on-field reduction is typically easier and less traumatic than a delayed reduction because of the absence of muscle spasm. Crepitation or pain at the upper arm may be indicative of a proximal humerus fracture. If any question exists, reduction should be delayed until sufficient radiographs are obtained. Plain radiographs will confirm a shoulder dislocation and can assist in identifying any concomitant fractures before a reduction maneuver. Once reduction is obtained, a physical evaluation is repeated to document any neurologic injury or weakness. A radiographic examination is required to confirm reduction and to evaluate the joint for other associated injuries. It is important to determine the presence of an axillary nerve injury, which can be associated with anterior dislocations. It is also imperative to assess the integrity of the rotator cuff, especially in older patients.
Recurrent instability presents with apprehension in the abducted, externally rotated position. Relief of the apprehension with posteriorly directed pressure on the proximal humerus, the relocation sign, is often present. Glenohumeral patholaxity can be assessed and graded in comparison to the contralateral side. This examination should be repeated under anesthesia, when a better comparison to the normal side can be obtained. The examination under anesthesia includes the supine load-shift test with the arm abducted at 70 to 90 degrees to document and to quantify the degree of anterior instability of the glenohumeral joint compared with the contralateral side.
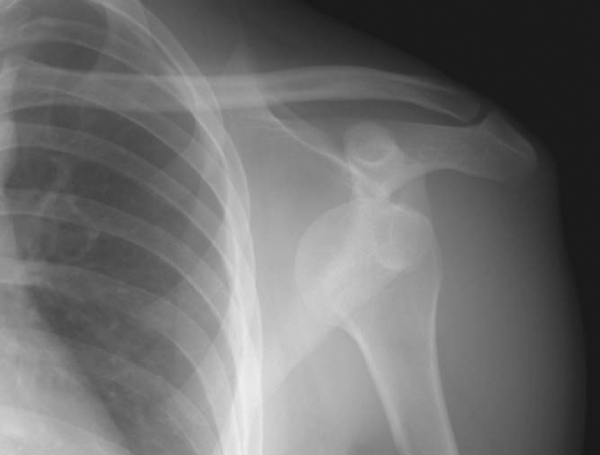
| • | A standard anteroposterior view with the arm in slight internal rotation is used to identify fractures of the greater tuberosity and Hill-Sachs lesions ( Fig. 3-1 ). |
|
| • | The transscapular Y view can assist with the direction of dislocation before reduction and confirm successful reduction. | |
| • | The West Point axillary view can be used to assess glenoid rim fractures (bony Bankart lesion; Fig. 3-2 ). |
|
|
|
|
Figure 3-2 |
| • | Computed tomographic scans are occasionally used to assess the extent of bone injuries of the humerus or glenoid. In addition, they can be used to evaluate the glenoid version. | |
| • | Magnetic resonance imaging is the “gold standard” to evaluate intraarticular pathoanatomy. For evaluation of recurrent instability, we prefer magnetic resonance arthrography because the addition of gadolinium improves the visualization of the shoulder pathoanatomy ( Fig. 3-3 ). After an acute dislocation or subluxation, the hemarthrosis serves to distend the joint and obviates the need for contrast agent. |
|
|
|
|
Figure 3-3 |
Indications and Contraindications
The primary reason to offer a surgical stabilization procedure is shoulder instability that interferes with activities of daily living or recreational sports. Recurrent dislocation or subluxation episodes can result in additional chondral or osteochondral damage. Contraindications include habitual or voluntary dislocation, a large bony Bankart lesion, and a large engaging Hill-Sachs lesion.
Anterior stabilization is typically performed under general anesthesia. An adjunctive regional (interscalene) block may be performed to provide postoperative analgesia. Positioning of the patient is based on the surgeon’s preference. Many surgeons believe that the lateral decubitus position allows better visualization and ease of instrumentation with a shoulder distraction system (STaR Sleeve and 3-Point Shoulder Distraction System; Arthrex, Inc., Naples, Fla;
Fig. 3-4
). However, the beach chair position may allow greater control of the entire arm, especially internal and external rotation. This position also facilitates easier conversion to a traditional open approach.
|
|
|
|
Figure 3-4 |
Surgical Landmarks, Incisions, and Portals
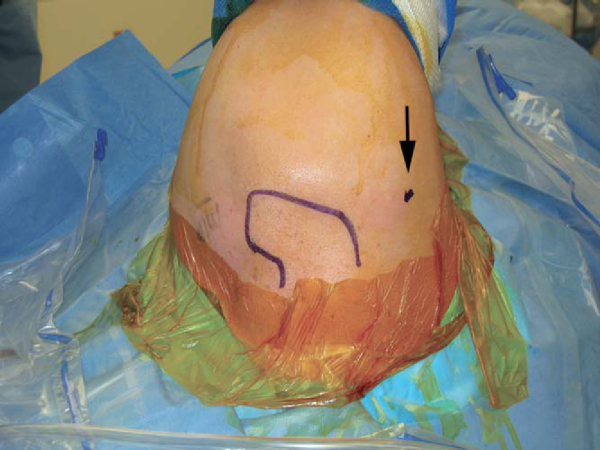
The bone landmarks may be identified with a skin marker to assist in portal position (
Fig 3-5
). The standard posterior viewing portal is established approximately 2 cm medial and 2 cm inferior to the posterolateral edge of the acromion.
|
|
|
|
Figure 3-5 |
The anterosuperior portal is established by an outside-in technique. An 18-gauge spinal needle is inserted 1 cm anterior to the acromion and 2 cm lateral to the coracoid close to the anterolateral edge of the acromion. The needle should enter the joint high and just medial to the biceps tendon near the root attachment as visualized arthroscopically. A clear 6.5-mm cannula (Stryker Endoscopy, San Jose, Calif) is used for instrumentation.
An anteroinferior portal is established just above the superior edge of the subscapularis and as lateral as possible to obtain the best angle toward the glenoid when suture anchors are inserted. Because of the required instrument passage, a larger 8.25-mm twist-in cannula (Arthrex, Inc., Naples, Fla) is used to establish and to maintain this portal.
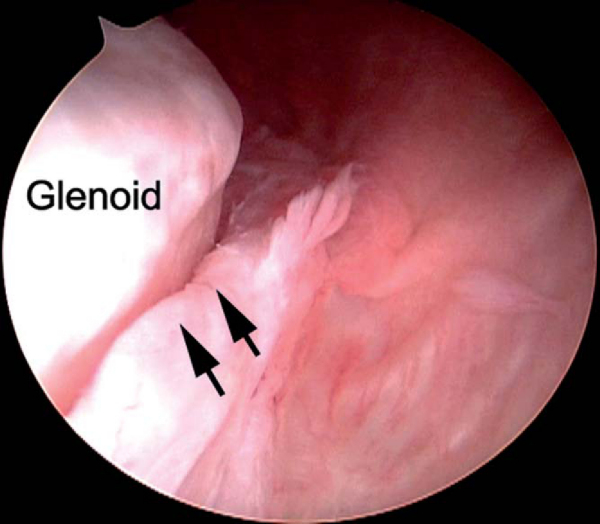
A systematic diagnostic arthroscopy is performed. The superior and posterior labral attachments are inspected. If they are torn, arthroscopic repair is performed as described in
Chapters 8
and
22
before anterior pathologic processes are addressed. With anterior instability, the anteroinferior labral attachment is often disrupted (Bankart lesion). Chronic instability often results in a medialized capsulolabral complex (anterior labral periosteal sleeve avulsion [ALPSA lesion];
Fig. 3-6
). When it is present, this labral attachment must be sharply reflected from the glenoid and then reattached to the articular margin. The anteroinferior glenoid is evaluated for bone and cartilage loss and the posterosuperior humeral head for a bony or cartilaginous Hill-Sachs defect (
Fig. 3-7
).
|
|
|
|
Figure 3-6 |
|
|
|
|
Figure 3-7 |
Specific Steps (
Box 3-1
)
For arthroscopic stabilizations to be successfully performed, a reproducible sequence of steps allows the surgeon to properly address the pathoanatomy and avoid the myriad pitfalls that can complicate the procedure.
| Surgical Steps | |||||||||||||||
|
1. Positioning and Portal Placement
The correct patient positioning and portal placement are critical to allow access to the entire shoulder. For lateral decubitus positioning, the patient is maintained with a deflatable beanbag. It is important to ensure that the patient is well secured to prevent the patient from leaning during the surgery and precluding adequate visualization. The 3-point shoulder system (STaR Sleeve and 3-Point Shoulder Distraction System) incorporates a strap that wraps under the proximal humerus and allows lateral distraction to improve joint visualization (see
Fig. 3-4
).
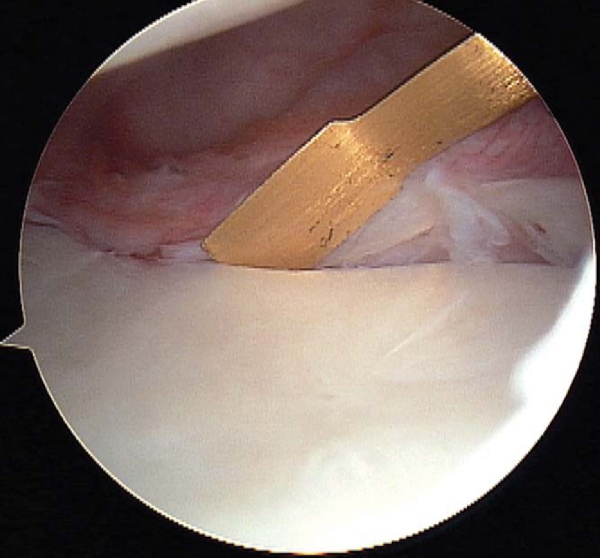
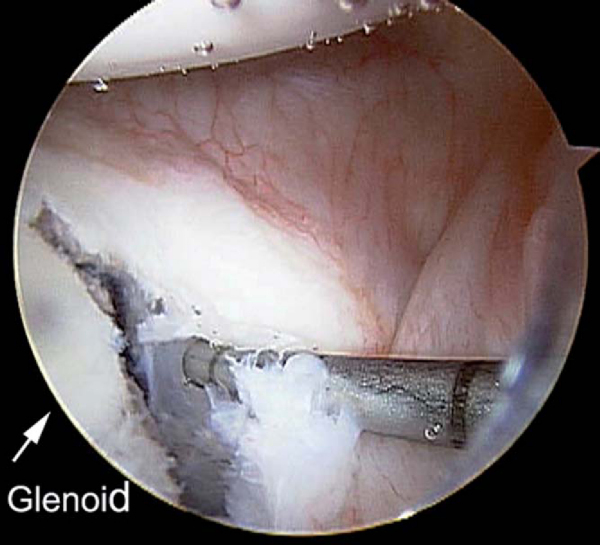
This step is crucial to prepare the capsulolabral tissue for repair. A sharp arthroscopic elevator (Liberator; ConMed Linvatec, Inc., Largo, Fla) is used to mobilize the capsulolabral tissue from the glenoid attachment (
Fig. 3-8
). Elevation should be performed until muscle fibers of the subscapularis are visible along the anterior glenoid neck. After mobilization, the capsulolabral tissue will be completely free, thus allowing superior translation for subsequent repair to the articular margin of the glenoid. A mechanical shaver or bur is used to abrade the anterior glenoid and to stimulate a bleeding bed to which the capsulolabral tissue will be reattached (
Fig. 3-9
). To better visualize the anterior glenoid during preparation, a 70-degree arthroscope may be used from the posterior portal to “look over the edge,” or the standard 30-degree arthroscope can be inserted down the anterosuperior portal while instrumenting through the anteroinferior portal.
|
|
|
|
Figure 3-8 |
|
|
|
|
Figure 3-9 |
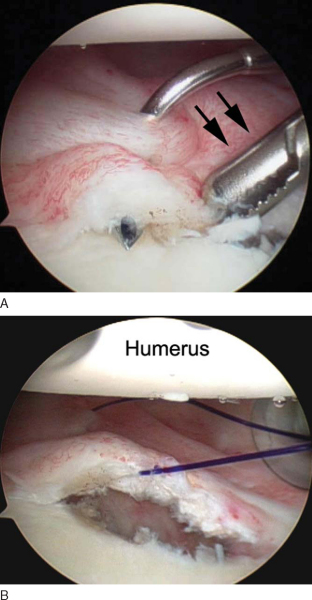
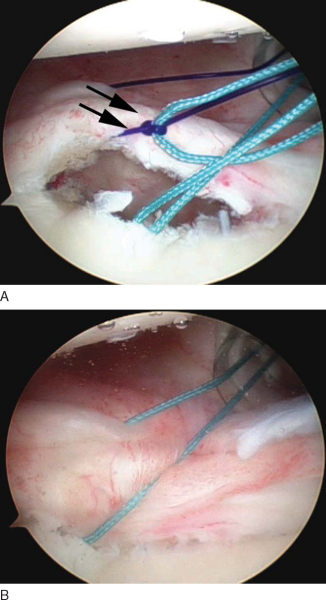
The next step is to pass a temporary suture that will be used subsequently to shuttle one limb of the permanent suture from the anchor through the tissue and labrum, which will secure the capsulolabral tissue back to the glenoid. Several arthroscopic instruments are commercially available to facilitate this step. We prefer to use a 45-degree curved suture shuttle (Spectrum Soft Tissue Repair System; ConMed Linvatec, Inc., Largo, Fla) through which a No. 1 PDS suture (Ethicon, Inc., Somerville, NJ) is passed (
Fig. 3-10
). It is important to place this shuttle stitch as inferior as possible to allow superior translation and retensioning of the capsulolabral complex onto the articular margin once it is tied. The suture delivery instrument is passed first through the capsule approximately 1 to 2 cm from the labrum. The hook is then passed through the labrum (
Fig. 3-10A
). The first passage will produce a capsular plication as it forms a pleat in the capsule. The second pass facilitates repair of the labrum back to the glenoid. The primary purpose of the shuttle suture is to serve as a temporary stitch that will then be used to pass one limb of the suture from the suture anchor to be passed through the tissue. Many instruments are available to allow the surgeon to skip this step by passing the instrument through the tissue to retrieve the suture from the previously placed anchor. However, use of a shuttle suture as described allows more precise placement of the sutures through the tissue.
|
|
|
|
Figure 3-10 |
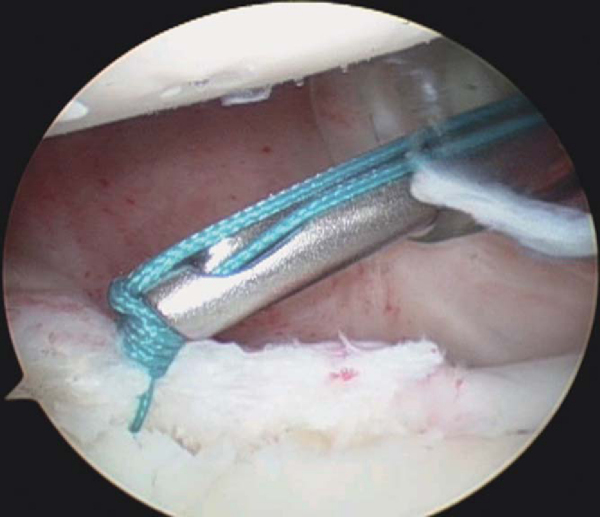
4. Suture Anchor Insertion and Suture Passage
Through the anterosuperior portal, a grasper is used to retrieve the shuttle stitch and pull it out the anterosuperior portal (
Fig. 3-10B
). At this time, upward retraction of this temporary stitch will allow a determination of how much superior shifting of the capsulolabral tissue is possible and, therefore, where the suture anchor should be correctly placed. Excessive tension on this first stitch will increase the likelihood of a knot’s loosening. We prefer the Bio-FASTak suture anchor preloaded with No. 2 FiberWire (Arthrex, Inc., Naples, Fla). The primary advantage of this suture anchor is that the implant can be placed without the use of a drill. The hole is initiated with a sharp trocar and then tapped by hand. The suture anchor is passed through the anteroinferior portal and placed 1 to 2 mm onto the articular margin (
Fig. 3-11
). After anchor insertion, the suture tails must be separated and cleared of any twists. A knot pusher may be placed on one strand of the suture and passed down the cannula. While the knot pusher is inserted, the more inferior or anterior limb is identified. This limb is then retrieved through the anterosuperior portal with a ringed grasper (
Fig. 3-12
). It is imperative to clamp or to hold the opposite limb that is exiting the anteroinferior portal to prevent “unloading” of the suture from the anchor.
|
|
|
|
Figure 3-11 |
|
|
|
|
Figure 3-12 |
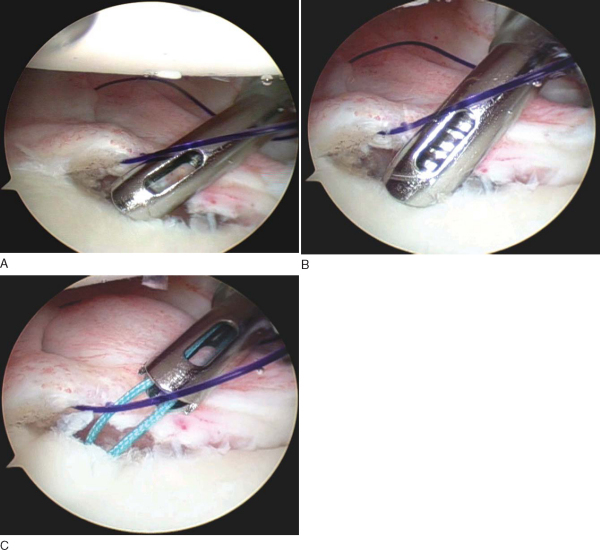
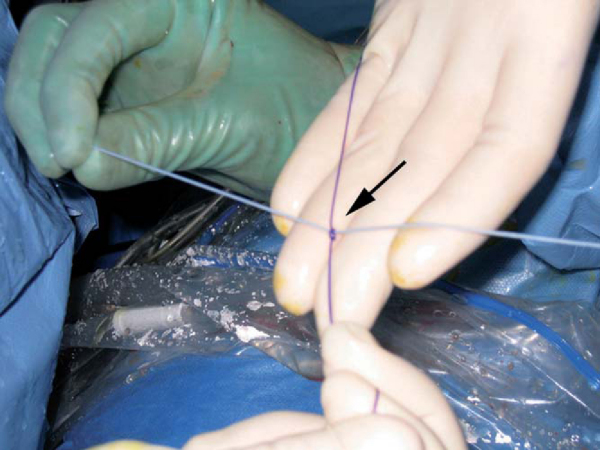
At this point, one limb of the PDS shuttle suture and one limb of the permanent suture are exiting each of the anterior cannulas. Outside the anterosuperior portal cannula, the PDS suture is tied to the permanent suture several centimeters from the end (
Fig. 3-13
). A dilating knot can be made with a simple half-hitch to facilitate passage of the shuttle suture. Once secured, the PDS shuttle suture, along with the attached permanent suture, is pulled through the anteroinferior portal (
Fig. 3-14
). Arthroscopic visualization of this maneuver is important to ensure that the sutures do not become entangled during passage through the tissue. The PDS suture is now discarded, and both limbs of the permanent suture are exiting the anteroinferior portal, with one limb now through the soft tissue.
|
|
|
|
Figure 3-13 |
|
|
|
|
Figure 3-14 |
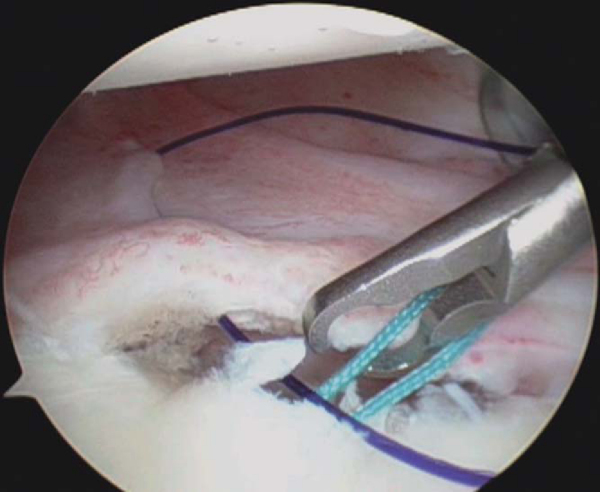
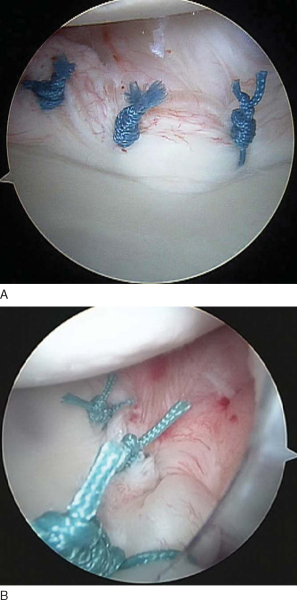
The knot pusher is again passed down one limb to ensure that the tails are not twisted around one another. An arthroscopic knot is now tied to secure the capsulolabral tissue back to the glenoid (
Fig. 3-15
). Many arthroscopic knots have been described; however, the surgeon should become proficient with one sliding-locking knot so it can be tied quickly and reproducibly with little effort. We prefer to use a modified Roeder knot that allows a strong suture buttress. This is backed up with three half-hitches to secure the knot. To reduce the tension on the tissue during tying, an atraumatic tissue grasper can be passed through the anterosuperior portal to translate the tissue while this first knot is tied. The tails of the completed knot are cut with the arthroscopic scissors passed through either the anterosuperior portal or the anteroinferior portal, depending on the optimal angle. This entire process is repeated two or three times to restore the tissue back to the glenoid. The knots should be secure and induce a dimpling effect on the capsulolabral tissue (
Fig. 3-16
).
|
|
|
|
Figure 3-15 |
Instability surgery is typically performed on an outpatient basis. A standard sling can be applied postoperatively. We prefer the Cryo/Cuff cooling device (Don Joy, Vista, CA) for additional pain relief. The patients are then seen several days after the procedure for their first dressing change.
The arthroscopic repair, like its open counterpart, requires that the capsulolabral tissue heal back to the glenoid. We have adopted a three-phase rehabilitation program. Each phase lasts approximately 4 weeks but is modified to the patient’s individual progress. The first phase consists of immobilization in a standard arm sling with gentle range-of-motion (Codman pendulum) exercises, wrist and elbow motion, and low-resistance isometrics during supervised physical therapy. The sling is worn at all times during this phase except during physical therapy sessions. The second phase consists of progressive resistive exercises and neuromuscular training. We recommend continued sling use during this period. Abduction with external rotation of the shoulder is avoided, but forward elevation with extension is encouraged. The final phase consists of progressive range-of-motion exercises as tolerated, increased resistance, neuromuscular training, and aerobic conditioning. Rubber-band resistance exercises and high-repetition sets are used to regain muscle conditioning. Return to full active duty, contact sports, and activities requiring overhead or heavy lifting is restricted until 4 months postoperatively.
The complications associated with arthroscopic stabilization include not only problems associated with the actual performance of the steps required to restore the normal anatomy but also problems associated with the equipment required to maintain adequate visualization during the procedure. The camera, arthroscope, and monitor equipment may malfunction, and specialized knowledge by the operating room staff is necessary to troubleshoot problems that inevitably occur. Replacement parts should be readily available to permit continuation of the procedure in the event that some of the equipment becomes damaged.
Complications associated with this procedure include inadequate tissue preparation leading to an inability to properly mobilize the capsulolabral complex. Medialized repairs often result in recurrent instability. Inadequate tensioning of the tissue can lead to suture breakage or recurrent laxity in the tissue, resulting in recurrent instability or failure. Metallic anchors used to secure soft tissue, if left protruding above the articular cartilage, can result in disastrous consequences for the humeral articular surface. Even slight prominence can result in a destruction of the humeral cartilage as the shoulder abrades on the metallic edge. In addition, improperly placed metallic or bioabsorbable anchors can dislodge and become loose bodies that result in destruction of articular cartilage. Some bioabsorbable fixation devices have been associated with a reactive synovitis as they are hydrolyzed. This may be manifested clinically as an increase in shoulder pain at 4 to 6 weeks after surgery and a loss of glenohumeral motion.
Traditionally, compared with open techniques for recurrent instability, results of arthroscopic Bankart repairs have been less favorable. The use of transglenoid fixation, tacks, and nonanatomic repairs resulted in unreasonably high recurrence rates. However, with improved arthroscopic techniques and implants, the results of arthroscopic instability repair have approached and even surpassed those of open techniques (
Table 3-1
). With comparable rates for recurrent dislocation, arthroscopic stabilization is rapidly becoming the technique of choice, even in the contact and collision athlete. A careful and diligent approach to arthroscopic stabilization can lead to success rates of more than 90%.
| Author | Mean Followup | Outcome |
|---|---|---|
| Warme et al[18] (1999) | 25 months | 38 shoulders mean Rowe score: 94 3 (8%) recurrence |
| Kandziora et al[11] (2000) | 38 months | 55 shoulders mean Rowe score: 85 9 (16%) recurrence |
| Tauro[16] (2000) | 39 months | 29 shoulders mean Rowe score: 92 2 (7%) recurrence |
| Kim et al[13] (2002) | 39 months | 59 shoulders mean Rowe score: 93 2 (3%) recurrence |
| Kim et al[12] (2003) | 44 months | 167 shoulders mean Rowe score: 92 7 (4%) recurrence |
| Fabbriciani et al[9] (2004) | 24 months | 30 shoulders mean Rowe score: 91 No recurrence |
| Mazzocca et al[15] (2005) | 37 months | 18 shoulders mean ASES score: 90 2 (11%) recurrence |
| Bottoni et al[7] (2005) | 32 months | 32 shoulders mean Rowe score: 89 1 (3%) recurrence |
1.
Arciero RA, St Pierre P: Acute shoulder dislocation. Indications and techniques for operative management.
Clin Sports Med 1995; 14:937-953.
2.
Arciero RA, Taylor DC: Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study.
J Bone Joint Surg Am 1998; 80:299-300.
3.
Arciero RA, Taylor DC, Snyder RJ, et al: Arthroscopic bioabsorbable tack stabilization of initial anterior shoulder dislocations: a preliminary report.
Arthroscopy 1995; 11:410-417.
4.
Arciero RA, Wheeler JH, Ryan JB, et al: Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations.
Am J Sports Med 1994; 22:589-594.
5.
Baker CL, Uribe JW, Whitman C: Arthroscopic evaluation of acute initial anterior shoulder dislocations.
Am J Sports Med 1990; 18:25-28.
6.
Bottoni CR, Arciero RA: Arthroscopic repair of primary anterior dislocations of the shoulder.
Tech Shoulder Elbow Surg 2001; 2:2-16.
7.
Bottoni CR, Smith EL, Berkowitz MJ, et al. Arthroscopic versus open anterior shoulder stabilization: a prospective, randomized clinical trial with preoperative and postoperative magnetic resonance arthrograms. Paper presented at the 31st annual meeting of the American Orthopaedic Society for Sports Medicine; Keystone, Colorado; 2005.
8.
DeBerardino TM, Arciero RA, Taylor DC, et al: Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes: Two- to five-year followup.
Am J Sports Med 2001; 29:586-592.
9.
Fabbriciani C, Milano G, Demontis A, et al: Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study.
Arthroscopy 2004; 20:456-462.
10.
Green MR, Christensen KP: Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications.
Arthroscopy 1993; 9:371-374.
11.
Kandziora F, Jager A, Bischof F, et al: Arthroscopic labrum refixation for posttraumatic anterior shoulder instability: suture anchor versus transglenoid fixation technique.
Arthroscopy 2000; 16:359-366.
12.
Kim SH, Ha KI, Cho YB, et al: Arthroscopic anterior stabilization of the shoulder: two to six-year followup.
J Bone Joint Surg Am 2003; 85:1511-1518.
13.
Kim SH, Ha KI, Kim SH: Bankart repair in traumatic anterior shoulder instability: open versus arthroscopic technique.
Arthroscopy 2002; 18:755-763.
14.
Kirkley A, Werstine R, Ratjek A, et al: Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation.
Arthroscopy 2005; 21:55-63.
15.
Mazzocca AD, Brown Jr FM, Carreira DS, et al: Arthroscopic anterior shoulder stabilization of collision and contact athletes.
Am J Sports Med 2005; 33:52-60.
16.
Tauro JC: Arthroscopic inferior capsular split and advancement for anterior and inferior shoulder instability: technique and results at 2- to 5-year followup.
Arthroscopy 2000; 16:451-456.
17.
Taylor DC, Arciero RA: Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations.
Am J Sports Med 1997; 25:306-311.
18.
Warme WJ, Arciero RA, Savoie 3rd FH, et al: Nonabsorbable versus absorbable suture anchors for open Bankart repair. A prospective, randomized comparison.
Am J Sports Med 1999; 27:742-746.
19.
Wheeler JH, Ryan JB, Arciero RA, et al: Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes.
Arthroscopy 1989; 5:213-217.