Compartment Syndrome
defined as an enclosed space formed by fascia, or a combination of
fascia and bone, that contains one or more muscles. An exception to
this definition is the carpal tunnel, which contains nine flexor
tendons but no muscle—except for those individuals with low-lying
muscle fibers from the flexor digitorum superficialis (FDS) that
sometimes extend into the carpal canal. The contents of an anatomic
compartment are muscles, arteries, veins, and nerves.
defined as a symptom complex resulting from increased tissue pressure
within a limited space that compromises the circulation and function of
the contents of that space. This occurs when intramuscular pressure is
elevated to a level, and for a period of time, sufficient to reduce
capillary perfusion.
undergoes necrosis, fibrosis, and contracture; associated nerve injury
causes further muscle dysfunction, sensibility deficits, or chronic
pain. The end result is a dysfunctional muscle compartment with local
and distant manifestations that depend upon the compartment involved
and the degree of muscle contracture and nerve dysfunction.
pressure (IMP) exceeds capillary blood pressure for a prolonged period
of time. In this circumstance, immediate decompression is required to
prevent muscle necrosis.
to cause ischemia, pain, and in some instances, diminished sensibility
or neurological dysfunction.
by tighter-than-normal fascia, small increases of volume associated
with exercise may significantly increase IMP.
neurologic deficit for a sufficient period of time, an acute
compartment syndrome may result. This condition is seen most often in
the lower extremity, but it also may occur in the upper extremity.
of irreversible hypoxic damage to muscles, nerves, and vascular
endothelium of an anatomic compartment. It may be categorized as mild,
moderate, or severe. In its mild form,
portions of normal muscle are replaced by contractile scar tissue that
shortens or contracts the affected muscle. The adjacent nerves are not
affected and the resultant deformity may be minimal.
muscle or muscles are more severely involved, and the adjacent nerves
may be affected to some degree. The end result is a more significant
deformity involving the FDS and flexor pollicis longus (FPL)—and in
some instances, portions of the FDS muscles and the median nerve.
the digital flexors are involved, along with the extrinsic wrist
flexors. In some cases, the muscles in the extensor and mobile wad
compartment are also involved. The median nerve is severely
compromised, and often degenerates into a fibrous tissue thread at its
midaspect. Although less likely to be involved, the ulnar nerve may
also be compromised. The end result is a severe flexion contracture of
the wrist and digits, with significant sensory deficit. Figure 15-1 depicts the clinical and intraoperative appearance of Volkmann’s ischemic contracture.
the shoulder to the hand. They are the deltoid, anterior arm, posterior
arm, mobile wad of the forearm, flexor forearm, extensor forearm, and
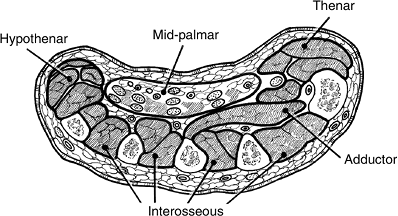
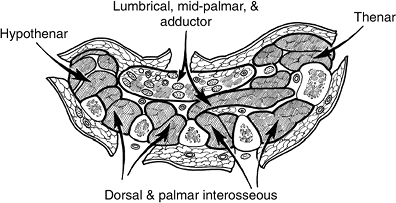
pronator quadratus. In the hand they
include
the central palmar, adductor, thenar, hypothenar, interosseous, and
finger compartments. The central palmar compartment contains the
lumbrical muscles, and thus meets the definition of a compartment. The
finger or digits, although not a definite compartment, may require
release if they are significantly compromised by both internal and
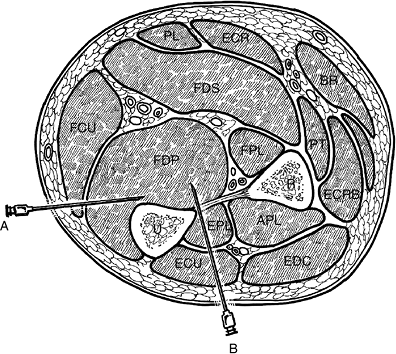
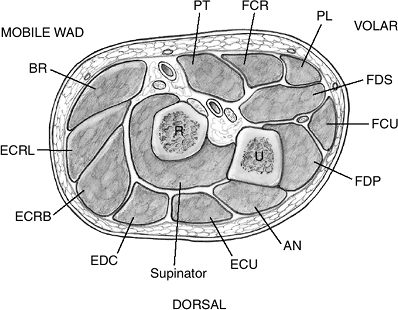
external pressure. The flexor forearm (Figure 15-2) and the interosseous (Figure 15-3) compartments have the greatest clinical significance, since development of a compartment
syndrome in these two locations probably results in the most significant functional loss and deformity.
 |
|
Figure 15-1 Clinical and intraoperative appearance of Volkmann’s ischemic contracture in an elderly alcoholic. A. Note the fixed and flexed wrist, the adduction contracture of the thumb, and the claw deformity of the fingers. B. Note the necrotic muscle at the tip of the forceps. C. The median nerve was surrounded by necrotic muscle (Penrose drain).
|
 |
|
Figure 15-2
The three forearm compartments: the flexor containing the finger, thumb, and wrist flexors; the extensor containing the finger, thumb, and ulnar wrist extensor (ECU); and the mobile wad of three, which is represented by the brachioradialis and the ECRL and ECRB (radial wrist extensors). R, radius; U, ulna. |
 |
|
Figure 15-3 Cross section of the midpalm, depicting the thenar, adductor, interosseous, midpalmar, and hypothenar spaces.
|
 |
|
Figure 15-4 Matsen’s unified concept of compartment syndrome (see text for details).
|
-
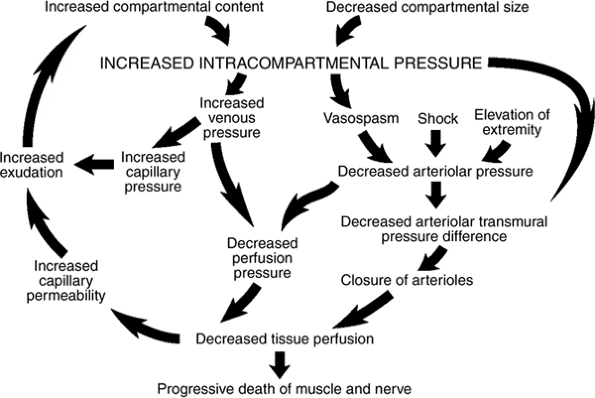
Compartment syndrome is caused by elevated pressure inside a closed compartment.
-
Matsen’s unified concept of compartment syndrome is presented in Figure 15-4.
-
Increased pressure within a compartment
may be caused by either an increased volume within the compartment
(such as fracture, hemorrhage, soft-tissue injury, and snake bite) or a
decrease in the size of the compartment (such as a tight cast or
dressing, burn eschar, or prolonged external limb pressure during
anesthesia or during an unconscious state resulting from drugs or
alcohol). -
In children, supracondylar fractures of
the humerus are a frequent cause because of a cast that fits tightly,
or an injury or occlusion of the brachial artery. -
Because of the relatively noncompliant
nature of the fascia around the specific anatomic compartments, either
of these two situations will result in an increase in pressure. -
Increased pressure within a compartment decreases the blood supply to the soft tissues, resulting in tissue hypoxia and damage.
-
The blood flow is determined by several
factors, including arterial pressure, venous pressure, resistance
within the vessel, and local tissue pressure. -
The difference between the arterial and venous pressures is the arteriovenous gradient.
-
This gradient, and therefore blood flow,
will be decreased if venous pressure is increased or if the incoming
arterial blood pressure is decreased (such as in shock, hemorrhage, or
limb elevation). -
All blood vessels, but particularly the microcirculation
and veins, are collapsible. Blood flow, therefore, also can be
decreased if the surrounding tissue pressure exceeds both the strength
of the vessel wall and the pressure within the vessel.
-
-
Tissue pressure affects both the flow
through a vessel, and the fluid equilibrium and exchange across the
walls of the microcirculation. -
Both the fluid pressure within the
capillary and the surrounding tissues, and the respective osmotic
pressures within the tissue and plasma, determine fluid exchange.
are given in Box 15-1. Compartment syndrome must be distinguished from
arterial injury and nerve injury. Table 15-1,
based on five of the six Ps, helps to differentiate compartment
syndrome from the ischemia associated with arterial injury or from the
findings in nerve injury that might mimic some of the components of
compartment syndrome.
-
The diagnosis of forearm compartment
syndrome is made by clinical findings, and may be confirmed by
measurement of intracompartmental pressure.
-
Pressure (elevated)
-
Pain (especially with passive stretch of the involved muscle[s])
-
Paresthesia
-
Paresis or Paralysis
-
Pink skin color
-
Pulse (usually intact)
-
Clinical findings include the following:
-
A swollen, tense, tender compartment with overlying skin that is often pink or red (Figure 15-5).
-
Pain that may seem out of proportion to the injury.
-
Sensory deficits or paresthesias.
-
Paresis or paralysis.
-
Distal pulses are usually intact.
-
-
Pain is usually increased by passive
stretch of the muscles in the affected compartment. For pain in the
flexor forearm compartment, stretching regimens would include passive
extension of the wrist and finger flexors.-
This finding may not be specific or reliable if there is an associated fracture or blunt trauma.
-
-
Sensory changes usually occur before motor deficits.
-
Radial and ulnar pulses are usually
intact, since systolic arterial pressure (+/- 120 mm Hg) exceeds the
pressure within the involved compartment.
-
-
If the extremity is swollen, Doppler examination may be useful to determine the status of the pulse.
-
Pink or red discoloration of the skin may
be absent, and temperature, capillary refill, and compartment turgor
may not be reliable signs in many instances. -
In children, anxiety associated with an increasing analgesic requirement is a very reliable indicator of compartment syndrome.
|
Table 15-1 Differential Diagnosis of Compartment Syndrome, Arterial Injury, and Nerve Injury Based On Five P’s
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
-
Although the diagnosis of compartment
syndrome may be made clinically, the measurement of the
intracompart-mental pressure is an additional diagnostic tool that may
aid in confirmation of the diagnosis. -
Compartment pressures can be measured by
the needle manometer technique, continuous infusion technique, the wick
or slit catheter technique, or with transducers that measure pressures
digitally. -
Self-contained devices with instructions
for use, such as the Stryker and Whitesides pressure monitor, are
commercially available. -
It is important to become familiar with
at least one of these techniques or devices so that the necessary tools
may be readily located in your emergency department, clinic, or
hospital, and utilized in a timely fashion. -
The threshold pressures considered
consistent with a compartment syndrome range from 45 mm Hg to 20 mm Hg
below diastolic pressure. -
Animal studies of compartment syndrome
have indicated that clinical signs along with compartment pressures of
30 mm Hg or greater are consistent with compartment syndrome.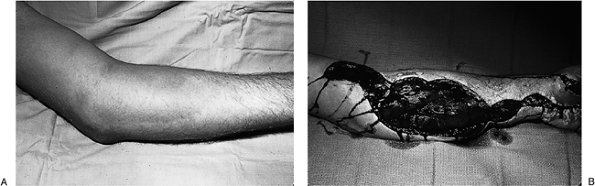 Figure 15-5 Acute compartment syndrome of the forearm. A.
Figure 15-5 Acute compartment syndrome of the forearm. A.
This patient was obtunded from drugs. He lay on his left arm/forearm
for an unknown length of time; note the swelling in the forearm and
arm. He complained of severe pain. B. He
was immediately taken to the operating room, where a comprehensive
fasciotomy was performed, which revealed swollen and edematous forearm
muscles. -
Figure 15-6 demonstrates ulnar and dorsal approaches for needle placement in the flexor aspect of the forearm.
-
The carpal tunnel, although not a true
compartment, may act as a closed space, and the median nerve may be
subject to the adverse effects of increased pressure. -
The hand compartments that may be
involved in compartment syndrome are the interosseous (both dorsal and
palmar), the thenar and hypothenar, the adductor, and the fingers. -
The clinical findings in compartment
syndrome in the hand are similar to the previously described findings
in the forearm, and include pain in the region, pain with passive
stretch of the involved muscles, localized swelling, paresthesia in the
involved nerve distribution, and muscle paresis. -
In the hand, all the intrinsic muscles
may be evaluated by passively abducting and adducting the digits with
the metacarpophalangeal (MCP) joints in extension and the proximal
interphalangeal (PIP) joints in flexion. -
The adductor compartment in the thumb is
tested by positioning the thumb in palmar abduction to produce
stretching of the adductor. -
The thenar muscles are stretched by
abduction and extension of the thumb, and the hypothenar muscles are
stretched by abduction and extension of the little finger.![]() Figure 15-6
Figure 15-6
Ulnar and dorsal approaches for needle/catheter placement in the flexor
forearm to obtain intracompartmental pressure. The starting point for
both approaches is at the junction of the proximal and middle third of
the supinated forearm. A. The ulnar approach inserts the needle/catheter into the deep or profundus compartment using the ulna as a guide. B.
The dorsal approach permits measurement of the dorsal compartment
pressures, as well as the deep compartment depending on the depth of
insertion. R, radius; U, ulna.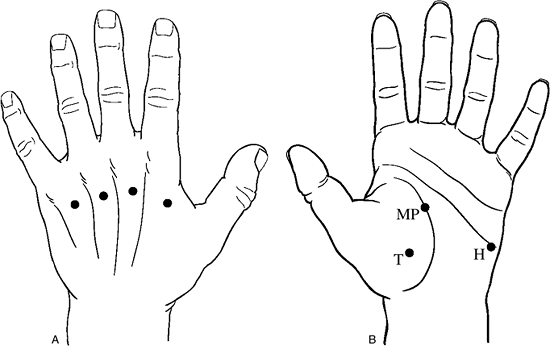 Figure 15-7 Portals for compartment pressure measurements in the hand. A. Interosseous compartment pressures may be measured through these four portals on the dorsum of the hand. B. The thenar (T), midpalmar (MP), and hypothenar (H) compartments may be measured through these portals.
Figure 15-7 Portals for compartment pressure measurements in the hand. A. Interosseous compartment pressures may be measured through these four portals on the dorsum of the hand. B. The thenar (T), midpalmar (MP), and hypothenar (H) compartments may be measured through these portals. -
Swelling and increased tissue turgor may be noted over the individual involved compartments.
-
In the fingers, the amount of swelling
and the nature of the injury—as well as the presence of a nonyielding
burn eschar—may indicate increased pressure and the need for a
fasciotomy. -
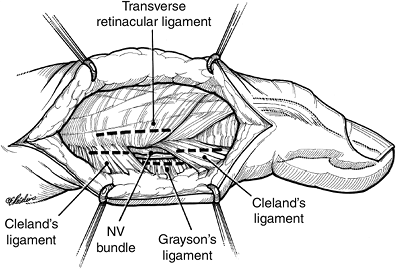
Potential compartments are present in the
finger due to the presence of fascial bands around the neurovascular
bundles, including Grayson’s and Cleland’s ligaments.
-
Figure 15-7 depicts the sites of needle placement for measurement of compartment pressures in the hand.
-
The goals of treatment are to restore microcirculation to the compartment through decompression.
-
This includes splitting or removing a
tight cast, including the removal of cast padding and tight dressings
or bandages of any type down to the level of the skin. -
If these maneuvers fail to resolve the problem, then immediate operative decompression is performed.
-
Decompression is typically achieved by fasciotomy.
 |
|
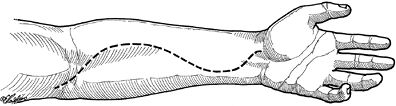
Figure 15-8
Comprehensive incision for release of the volar forearm compartment syndrome. Note that the incision includes the distal arm and should include the carpal tunnel. |
-
The forearm compartments (involving the
forearm flexor compartment and the mobile wad compartment) are
decompressed by a comprehensive incision from the distal arm to the
midpalm, as noted in Figure 15-8 and 15-5B. -
The deep fascia is incised from the region of the distal arm to, and including, the carpal canal.
-
The underlying flexor muscles will often bulge dramatically into the wound.
-
-
The median nerve is at risk at four
locations: the lacertus fibrosus, the pronator teres, the deep fascial
arcade of the flexor digitorum superficialis, and the carpal tunnel. -
If preoperative findings indicate that
the ulnar nerve is involved, it is also decompressed as indicated at
the cubital tunnel, forearm, and Guyon’s canal at the wrist and hand. -
If signs of radial nerve dysfunction are present, decompression of the radial tunnel may also be indicated (see Chapter 7, Entrapment Neuropathies, for details of radial nerve decompression).
-
Coexisting forearm fractures are usually stabilized operatively at the time of fasciotomy.
-
Skin incisions are left open to accommodate swelling, but are loosely reapproximated to cover the nerves.
-
If fractures are open and contaminated, fasciotomy is performed, wounds debrided, and fractures stabilized.
-
In contaminated wounds, external fixation or limited internal fixation may be preferable to standard internal fixation methods.
-
Skin grafting and limited secondary closure is performed when wounds demonstrate clean granulation tissue.
-
Compartment syndromes involving the forearm extensor compartment are released through a dorsal incision.
-
When both the flexor and extensor
compartments are involved, it is preferable to release the flexor
compartment first; the relaxation afforded by the skin and fascia often
decompresses the dorsal compartments. -
Dorsal compartment pressures are used to determine whether or not to release the extensor compartment.
-
If required, it is released through a
longitudinal incision 2 cm lateral and distal to the lateral
epicondyle. The incision is continued distally to the myotendinous
junction of the extensor muscles in the midforearm.
-
-
Fasciotomy is also indicated at the time of limb revascularization if the duration of ischemia has been as much as 4 to 6 hours.
-
Post revascularization edema may precipitate compartment syndrome, and prophylactic fasciotomy is indicated.
-
The principles of treatment of hand compartment syndromes are similar to those of the forearm.
-
The appropriate incisions for decompression of the various hand compartments are depicted in Figure 15-9.
-
The essentials of the deeper dissection for decompression of the hand compartments are given in Figure 15-10.
-
Release of swollen fingers may be required based on the amount of swelling and the nature of the skin envelope.
-
If a significant burn eschar or swelling
is present, digital fasciotomies are performed through midlateral
incisions on the nondominant or noncontact side of the digits. The
incisions are dorsal to the neurovascular bundles; Cleland’s and
Grayson’s ligaments are incised. -
The dissection usually ends at the flexor sheath.
-
The incision is centered over the PIP joint and may extend 2 cm proximal and 2 cm distal to the PIP joint, as described in Figure 15-11.
-
The prognosis depends on the intensity and duration of the elevated compartment pressure.
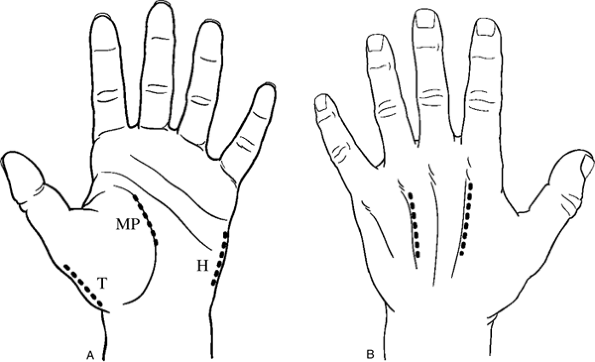 Figure 15-9 Appropriate incisions for release of the hand compartments. A. The thenar (T), midpalmar (MP), and hypothenar (H) incisions. B. Suitable incisions for release of the interosseous compartments.
Figure 15-9 Appropriate incisions for release of the hand compartments. A. The thenar (T), midpalmar (MP), and hypothenar (H) incisions. B. Suitable incisions for release of the interosseous compartments. -
Therefore, time is of the essence in the management of compartment syndrome.
-
If clinical findings and/or pressure
readings are suggestive, but not conclusive, remember that the scar
from a fasciotomy incision is of relatively minimal consequence
compared to an untreated compartment syndrome that results in a
Volkmann’s ischemic contracture.
 |
|
Figure 15-010
Depiction of the details of the deeper dissection for release of the interosseous muscle compartments, the thenar compartment, the midpalmar and adductor compartments (both of which may be released through a midpalmar incision), and the hypothenar compartment. |
-
Treatment goals are to increase function,
decrease associated pain factors if present, and, if possible, restore
limb sensibility.
 |
|
Figure 15-11 Midaxial incision for release of compromised digits in compartment syndrome.
|
-
Treatment of mild contractures depends upon the severity of the deformity and the time interval between injury and initiation of treatment.
-
Contractures of the deep forearm flexors,
with normal hand sensibility and preservation of remaining extrinsic
muscle strength, are treated by a comprehensive hand rehabilitation
program that includes active and passive mobilization, strengthening,
and static and dynamic extension splinting. This regimen works to
improve thumb web space width, strengthen weak thumb intrinsic muscles,
and correct or improve digital flexion contractures.
-
Treatment of moderate to severe
contractures is based on elimination of contractures, release of
secondary nerve compression, and tendon transfers to recover some of
the lost function. -
The surgical procedures employed include
excision of the muscle infarct, tendon lengthening, muscles slides,
neurolysis (or nerve graft in very severe cases), and various tendon
transfers to restore balance and function. -
Microvascular free tissue transfers of nerve and muscle have been promising in severe cases of Volkmann’s contracture.
AR, Mubarak SJ. Current concepts in the pathophysiology, evaluation and
diagnosis of compartment syndrome. Hand Clinics 1998;14:371–383.
CG, Johnson GHF. A new technique of catheter placement for measurement
of forearm compartment pressure. J Trauma 1991;31:1404–1408.
SJ, Hargens AR, Owen CA, et al. The wick-catheter technique for
measurement of intramuscular pressure. A new clinical and research
tool. J Bone Joint Surg 1976;58A:1016–1020.
K. Management of established Volkmann’s Contracture. In: Green DP,
Hotchkiss RN, Pederson WC, eds. Green’s operative hand surgery. 4th Ed.
New York: Churchill Livingstone, 1999:593–603.
Schroeder HP, Botte MJ. Definitions and terminology of compartment
syndrome and Volkmann’s ischemic contracture of the upper extremity.
Hand Clin 1998;14:331–341.
TE Jr, Heckman MM. Acute compartment syndrome: update on diagnosis and
treatment. J Am Acad Orthop Surg 1996;4:209–218.