The Trigeminal Nerve
cranial, nerve (CN V) has a large sensory part that innervates the
face, teeth, oral and nasal cavities, the scalp back to the vertex, and
the intracranial dura; and a much smaller motor part that innervates
the muscles of mastication. The sensory component has 3 divisions: the
first, or ophthalmic division (CN V1), the second or maxillary division (CN V2), and the third or mandibular division (CN V3).
The motor and principal sensory nuclei are located in the midpons. The
spinal tract and nucleus, which subserve pain and temperature, extend
from the pons down into the upper cervical spinal cord. The
mesencephalic root receives proprioceptive fibers.
by examining the muscles of mastication. Bulk and power of the
masseters and pterygoids can be gauged by palpating these muscles as
the patient clenches the jaw. An effective technique is to place the
examining fingers along the anterior, not lateral, border of the
masseters bilaterally. When the jaw is clenched the fingers will move
forward; this movement should be symmetric on the two sides. Unilateral
trigeminal motor weakness causes deviation of the jaw toward the weak
side on opening (Figure 11.1). Subtle deviation
on jaw opening is often the earliest clue to the presence of an
abnormality. It is occasionally difficult to be certain whether the jaw
is deviating or not. Note the relationship of the midline notch between
the upper and lower incisor teeth; it is a more reliable indicator than
lip movement. The tip of the nose and the interincisural notches should
line up. A straightedge against the lips can help detect deviation.
Another useful technique is to draw a vertical line across the midline
upper and lower lips. Failure of the two vertical marks to match when
the jaw is opened indicates deviation. If there is any suggestion of a
problem, have the patient move the jaw from side to side. With
unilateral weakness the patient is unable to move the jaw
contralaterally. With facial weakness there may be apparent deviation
of the jaw, and of the tongue, because of the facial asymmetry. Holding
up the weak side manually will sometimes eliminate the pseudodeviation.
include having the patient protrude and retract the jaw, noting any
tendency toward deviation; and having the patient bite on tongue
depressors with the molar teeth, comparing the impressions on the two
sides and comparing the difficulty of extracting a tongue depressor
held in the molar teeth on each side.
signifies a lesion involving the brainstem, Gasserian ganglion, or the
motor root of CN V at the base of the skull. Severe bilateral weakness
of the muscles of mastication with inability to close the mouth
(dangling jaw) suggests
motor
neuron disease, a neuromuscular transmission disorder, or a myopathy.
With significant atrophy of one masseter, a flattening of the jowl on
the involved side may be apparent (Figure 11.2). With temporalis atrophy there may be a hollowing of the temple. Rarely, fasciculations or other abnormal
involuntary movements occur. There is no reliable or realistic method
for examination of the other muscles supplied by CN V. Because of
bilateral innervation, unilateral upper motor neuron lesions rarely
cause significant impairment of trigeminal motor function. There may be
mild, transitory unilateral weakness. The amount of involvement depends
on the extent of decussation. In bilateral supranuclear lesions there
may be marked paresis.
 |
|
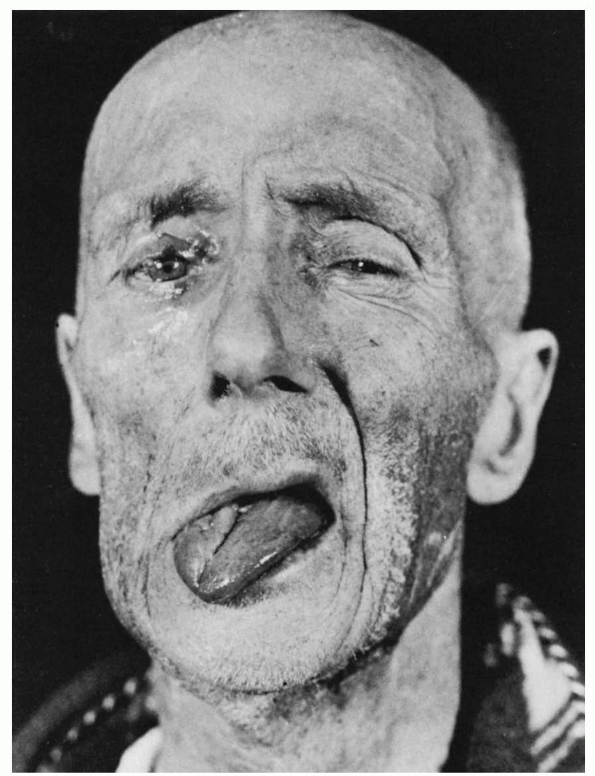
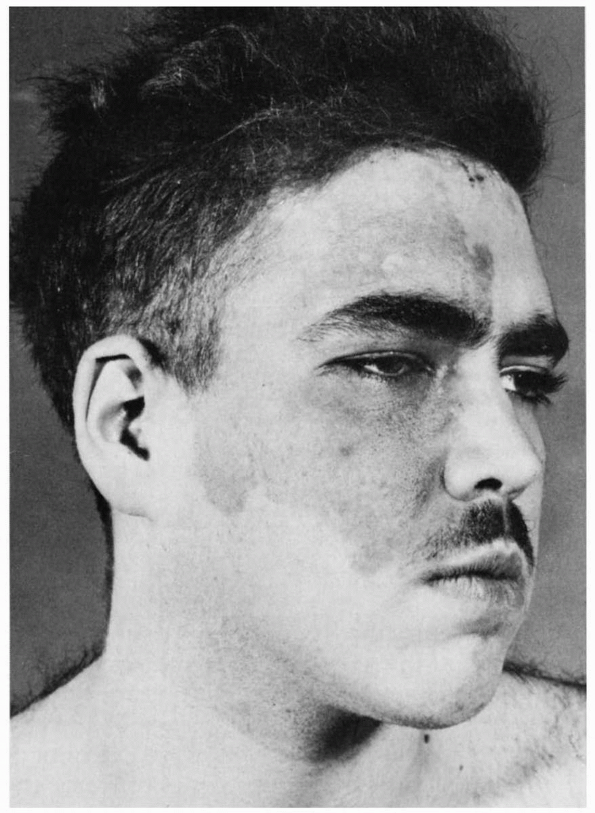
FIGURE 11.1
• Infranuclear paralysis of the right trigeminal, facial, and hypoglossal nerves in a patient with metastatic carcinoma, showing deviation of the tongue and mandible to the right. |
 |
|
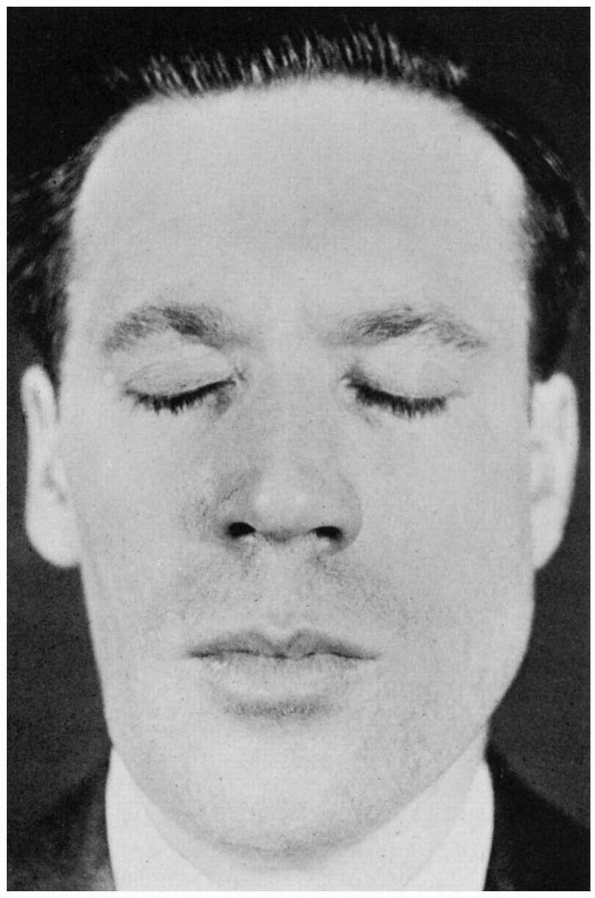
FIGURE 11.2 • Infranuclear paralysis of the right trigeminal nerve with atrophy of the muscles of mastication.
|
occasionally temperature are examined in the same manner as elsewhere
on the body, searching for areas of altered sensation. It is better to
ask the patient if the stimuli feel the same on the two sides, rather
than suggesting they might feel different. Sometimes it is useful to
examine the nostrils, gums, tongue, and insides of the cheeks.
Proprioception cannot be adequately tested, but one can test for
extinction and the ability to identify figures written on the skin.
sensation: (a) determining whether sensory loss is organic or
nonorganic, (b) determining which modalities are involved, and (c)
defining the distribution. Complaints of facial numbness are common,
and not all are organic. However, real facial sensory loss can be a
serious finding, occasionally signifying underlying malignancy. The
various methods and tricks for detecting nonorganic sensory loss are
not entirely reliable, and this diagnosis should be made with caution.
Patients with nonorganic sensory loss may have a demarcation of the
abnormal area at the hairline rather than the scalp vertex. On the
lower face functional sensory loss tends to follow the jaw line and
involve the notch over the masseter muscle, which is not trigeminal
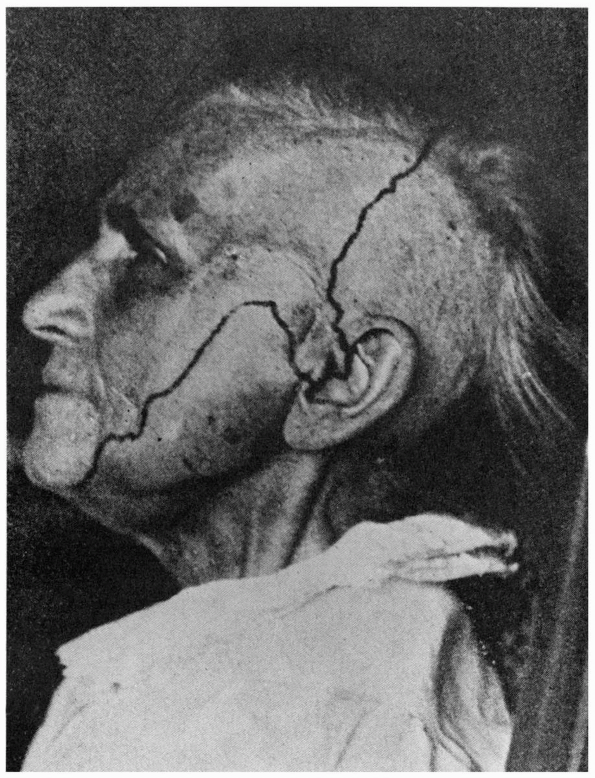
innervated (Figure 11.3). On the trunk, organic
sensory loss typically stops short of midline because of the overlap
from the opposite side, and splitting of the midline suggests
nonorganicity.
This finding is not reliable on the face because there is less midline
overlap on the face, so organic facial sensory loss may extend to the
midline. The corneal and sternutatory reflexes should be normal in
nonorganic sensory loss. Splitting of vibration along the midline is
reputedly a nonorganic sign. Because the frontal bone and mandible are
single bones, there should be no difference in vibratory sensibility on
either side of midline. Patients who report a difference in vibratory
sensibility on testing just to either side of midline may have
nonorganic sensory loss. The reliability of this sign has not been
validated; it can be misleading. Other signs suggestive of
nonorganicity include dissociation between pinprick and temperature,
variability from trial to trial, history of hypochondriasis, secondary
gain, la belle indifference, nonanatomical sensory loss, and changing
boundaries of hypalgesia.
 |
|
FIGURE 11.3
• The distribution of sensory loss following complete section of the trigeminal root. Note the large area at the angle of the jaw that is innervated by C2 through the greater auricular nerve, and the inclusion of the tragus of the ear in the trigeminal distribution. |
reflexes most often assessed in evaluating the trigeminal nerve. Many
other reflexes have been described, but they are of limited value and
are seldom used. The afferent limbs of these reflexes are trigeminal
mediated. In some the efferent limb is also trigeminal (e.g., the jaw
jerk); in others the efferent limb is executed through connections with
CN III, CN VII, or other pathways.
places an index finger or thumb over the middle of the patient’s chin,
holding the mouth open about midway with the jaw relaxed, then taps the
finger with the reflex hammer. The response is an upward jerk of the
mandible. Other methods to elicit the reflex include tapping the chin
directly and placing a tongue blade over the tongue or the lower
incisor teeth and tapping the protruding end. All of these cause a
bilateral response. A unilateral response may sometimes be elicited by
tapping the angle of the jaw or by placing a tongue blade over the
lower molar teeth along one side and tapping the protruding end.
the sensory portion of the trigeminal nerve, possibly through the
mesencephalic root, and the efferent impulses through its motor
portion; the reflex center is in the pons. In normal individuals, the
jaw jerk is minimally active or absent. Its greatest use is in
distinguishing limb hyper-reflexia due to a cervical spine lesion
(where the jaw jerk is normal) from a state of generalized
hyper-reflexia (where the jaw jerk is increased along with all of the
other reflexes). The jaw reflex is exaggerated with lesions affecting
the corticobulbar pathways above the motor nucleus, especially if
bilateral, as in pseudobulbar palsy or amyotrophic lateral sclerosis
(ALS). It is sometimes possible to elicit extra beats or jaw clonus.
The stimulus must be delivered to the cornea, not the sclera. If there
is any evidence of eye infection, different pieces of cotton or tissue
should be used for the two eyes. Crude stimuli, such as a large blunt
object or fingertip should never be used, even in comatose patients.
blinking of the ipsilateral (direct reflex) and contralateral
(consensual reflex) eyes. The afferent limb of the reflex is mediated
by CN V1, the efferent limb by CN VII.
consensual responses may be absent; neither eye blinks. Stimulation of
the opposite eye produces normal direct and consensual responses. With
a unilateral CN VII lesion the direct response may be impaired, but the
consensual reflex should
be
normal. Stimulation of the opposite side produces a normal direct
response but an impaired consensual response. These patterns are
summarized in Table 11.1.
Lesions involving the brainstem polysynaptic trigeminofacial
connections may produce impairment of both direct and consensual
responses. The corneal reflex may be depressed with lesions of the
contralateral hemisphere, especially if there is thalamic involvement.
Because of the descent of the spinal tract and nucleus of CN V into the
upper cervical cord, lesions there sometimes affect the corneal reflex.
Corneal sensation may be impaired in contact lens wearers, even when
the lenses are out.
 |
|
FIGURE 11.4
• Eliciting the corneal reflex. The stimulating object should be brought in outside the patient’s vision. The patient should look upward as the object is brought in from below, or laterally as the object is brought in from the other side. The stimulus must be applied to the cornea, not the sclera. |
spear of tissue, or similar object causes wrinkling of the nose, eye
closure, and often a forceful exhalation resembling a feeble sneeze, as
the
nose tries to rid itself of the foreign object. The ophthalmic, not the
maxillary, division of the trigeminal innervates the nasal septum and
the anterior nasal passages. The afferent limb of the reflex arc is
carried over CN V1,
the efferent limb over CNs V, VII, IX, X, and the motor nerves of the
cervical and thoracic spinal cord. The reflex center is in the
brainstem and upper spinal cord. The primary clinical use of the
sternutatory reflex is as a cross-check on the corneal reflex.
|
TABLE 11.1 Patterns of Direct and Consensual Corneal Reflex Abnormality with Trigeminal and Facial Nerve Lesions
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
involuntary movements, sensory loss or other sensory abnormalities,
facial pain, trophic abnormalities, autonomic dysfunction, or
abnormalities of the reflexes mediated by the trigeminal nerve. The
conditions most commonly seen are facial pain, particularly trigeminal
neuralgia, and facial numbness.
weakness in the trigeminal distribution does not often occur with upper
motor neuron lesions, although slight weakness of the contralateral
muscles with an exaggerated jaw reflex can occur. Bilateral
supranuclear lesions, as in pseudobulbar palsy or ALS, can cause marked
weakness, often with a grossly exaggerated jaw reflex. In supranuclear
lesions no atrophy or fasciculations occur.
distribution is most often the result of a neuromuscular transmission
disorder or ALS. Patients with myasthenia gravis may have chewing
difficulties with masticatory fatigue, especially when eating
difficult-to-chew things such as tough meat. Patients with severe
polymyositis, rarely with other myopathies, may also have difficulty
with jaw power. Patients with giant cell arteritis commonly have jaw
claudication with focal pain in the masseter when chewing, which can be
confused with weakness. Amyotrophic lateral sclerosis commonly causes a
jaw drop, often with dysphagia and difficulty swallowing saliva,
requiring the patients to constantly keep absorbent materials at their
mouth. Lesions anywhere along the course of the lower motor neuron can
cause weakness accompanied by atrophy, sometimes marked;
fasciculations; and a decreased jaw jerk (Figure 11.1).
Oromandibular dystonia produces a variety of abnormal movements: jaw
opening, jaw closing, lateral movements, bruxism, and combinations of
these. Jaw dystonia may occur as part of an extrapyramidal syndrome due
to psychoactive drugs, and abnormal jaw movements are a common
manifestation of tardive dyskinesias. Meige syndrome is oromandibular
dystonia and blepharospasm. Chewing movements and grinding of the teeth
are sometimes present in psychoses, and chewing or tasting movements in
complex partial seizures. Trismus is marked spasm of the muscles of
mastication. The teeth are tightly clenched, the muscles hard and firm,
and the patient is unable to open the jaw. It is a classical
manifestation of tetanus. Some myopathies, especially polymyositis, may
result in fibrosis of the masseters, which causes painless trismus.
or sensory radiations, may raise the sensory threshold of the
contralateral face; a thalamic lesion may cause facial hypesthesia with
hyperpathia or allodynia. Lesions of the principal sensory nucleus in
the pons may cause diminished tactile sensation involving both skin and
mucous membranes on the involved side, and loss of reflexes in which
the afferent arc is mediated by the trigeminal nerve. Lesions of the
spinal tract or nucleus cause a disturbance of the pain and temperature
modalities, and, possibly to a lesser extent, of tactile sense.
involvement of light touch as compared to pain and temperature suggests
a lesion in the substance of the brainstem (intramedullary), where the
different sensory pathways are running in widely separate locations.
Extramedullary lesions
are
characterized by loss or diminution of all types of exteroceptive
sensation, dysesthesias or paresthesias, or spontaneous pain. A lesion
central to or at the Gasserian ganglion will affect all three
divisions; a lesion peripheral to the ganglion will involve only
isolated divisions or branches. There may also be reflex changes, such
as absence of the corneal or sternutatory.
function is trigeminal neuralgia (TN), or tic douloureux. Trigeminal
neuralgia causes paroxysms of fleeting but excruciating unilateral
facial pain. It usually involves the second or third division, rarely
the first. The lancinating pain lasts only seconds, but it may occur
many times per day. Stimulation of some specific area, a trigger zone,
in the involved nerve distribution will often provoke a paroxysm of
pain. Pain may be brought on by activities such as talking, chewing,
brushing teeth, exposure to cold, or by wind on the face. Male patients
may present with the trigger zone unshaven. The patient may be
reluctant to allow neurologic examination of the involved area for fear
of triggering a paroxysm of pain. Patients with idiopathic TN have no
clinical motor or sensory deficit in the distribution of the involved
nerve.
sensory root by an ectatic arterial loop of the basilar artery, most
commonly the anterior inferior cerebellar or superior cerebellar.
Rarely, structural lesions may cause facial pain resembling TN. These
may cause sensory loss in the involved distribution, motor dysfunction,
or involve neighboring structures. Examples include multiple sclerosis
(MS), tumors involving the Gasserian ganglion or its branches, and
other tumors in the cerebellopontine angle. MRI in idiopathic
trigeminal neuralgia is rarely abnormal except for vascular loops. The
presence of a complaint of numbness, impaired sensation on examination,
other neurologic abnormalities, history of symptom progression, and
duration of symptoms of less than 1 year greatly increase the
likelihood of an abnormal imaging study.
commonly than in the general population; it is usually caused by a
demyelinating lesion involving the trigeminal root entry zone in the
pons.
Bilateral
tic douloureux is especially suggestive of MS. Most TN patients are in
the fifth decade or beyond; the onset in a young person should prompt
consideration of demyelinating disease. The term atypical facial pain
is used to refer to a syndrome of facial pain that does not have the
characteristics of TN. The pain in atypical facial pain is typically
chronic, not restricted to a single trigeminal division,
not
lancinating, and not associated with any trigger zone. No identifiable
etiology is usually apparent, and the pain is often attributed to
depression or other emotional factors.
 |
|
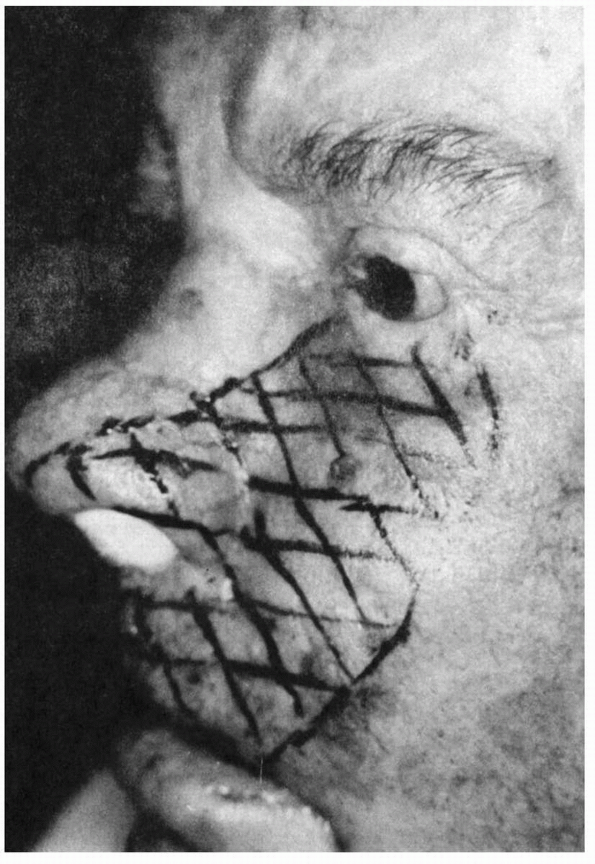
FIGURE 11.5
• Patient with infraorbital neuropathy from carcinomatous infiltration. Note that the maxillary division innervates only the side of the nose distally. This patient had numbness of only the anterior teeth and gums, which proved the lesion was at the infraorbital foramen and not intracranially. (From Campbell WW. The numb cheek syndrome: a sign of infraorbital neuropathy. Neurology 1986;36:421-3.) |
|
TABLE 11.2 Some Causes of Trigeminal Sensory Neuropathy
|
||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||
 |
|
FIGURE 11.6 • A patient with encephalotrigeminal angiomatosis (Sturge-Weber syndrome).
|
extremely painful. It is usually seen in elderly or immunocompromised
patients. HZ most often affects CN V1, causing pain and
vesicles over the forehead, eyelid, and cornea (herpes ophthalmicus),
but may affect any of the trigeminal divisions, and there may be motor
involvement. Ophthalmic involvement may lead to keratitis, corneal
ulcerations, residual corneal scarring, and sometimes results in
blindness.
elderly, the pain of the acute phase evolves into a dreadful,
persistent neuralgic pain syndrome called postherpetic neuralgia. Pain
persisting for more than one month after the acute eruption is
appropriately labeled as postherpetic neuralgia. The pain is probably
related to deafferentation and mediated centrally. It is typically
dysesthetic with a burning component, constant but with superimposed
paroxysms of lancinating pain that may be provoked by touching certain
spots within the affected area. There may be hypesthesia or
hyperesthesia in the affected area.
of processes, some ominous, may be responsible. The numb chin syndrome
refers to hypesthesia and sometimes paresthesias involving the lower
lip and chin, approximately in the distribution of the mental nerve.
The numb chin syndrome is often due to a neoplastic process, with
metastasis either to the mental foramen of the mandible or to the
intracranial meninges or skull base, often from carcinoma of the breast
or lung. The numb cheek syndrome is similar but usually due to a lesion
involving the infraorbital nerve (Figure 11.5).
The numb chin or cheek syndrome can be the presenting manifestation of
cancer. Unusual causes of trigeminal sensory dysfunction include
pontine hemorrhage, Wegener granulomatosis, localized hypertrophic
mononeuropathy, and a midbrain lesion affecting the crossed
trigeminothalamic fibers.
isolated facial numbness, usually gradual in onset, which may involve a
single division or the entire face; it is occasionally bilateral. Some
cases are idiopathic, but many underlying diseases, particularly
connective tissue disorders, can cause trigeminal sensory neuropathy (Table 11.2).
connections may result in misdirection of nerve fibers, producing
unusual and interesting effects. Congenital ocular aberrant innervation
syndromes are a complex group of disorders involving abnormal miswiring
of the extraocular muscles. The Marcus Gunn phenomenon, or jaw-winking,
occurs in patients with congenital ptosis; opening the mouth, chewing,
or lateral jaw movements cause an exaggerated reflex elevation of the
ptotic lid. The phenomenon may be the result of proprioceptive impulses
from the pterygoid muscles being misdirected to the oculomotor nucleus.
Involuntary closure of one eye on mouth opening (reversed Gunn
phenomenon, inverse jaw winking, or Marin Amat sign) is a synkinesia
due to aberrant regeneration of the facial nerve; it occurs most often
following Bell palsy. The auriculotemporal (Frey) syndrome produces
flushing, warmness, and excessive perspiration over the cheek and pinna
on one side following ingestion of spicy food. This syndrome is due to
misdirection of the secretory fibers to the parotid gland to the sweat
glands and vasodilator endings in the auriculotemporal nerve
distribution; it usually follows trauma or infection of the parotid
gland or local nerve injury. In encephalotrigeminal angiomatosis
(Sturge-Weber syndrome, or Weber-Dimitri disease), there are congenital
nevi or angiomas over one side of the face in the trigeminal
distribution with associated ipsilateral leptomeningeal angiomas and
intracortical calcifications with attendant neurologic complications (Figure 11.6).
