Humerus
Editors: Morrey, Bernard F.; Morrey, Matthew C.
Title: Master Techniques in Orthopaedic Surgery: Relevant Surgical Exposures, 1st Edition
Copyright ©2008 Lippincott Williams & Wilkins
> Table of Contents > Section I – Upper Extremity > 4 – Humerus
4
Humerus
Bernard F. Morrey
In this chapter the theme is extensile type of exposure
to the anterior and posterior aspects of the humerus. Limited portions
of these exposures, of course, may be employed depending on the
pathology being addressed. The flexibility, expressed in this chapter,
is quite effective in addressing the majority of pathology encountered
in the brachium.
to the anterior and posterior aspects of the humerus. Limited portions
of these exposures, of course, may be employed depending on the
pathology being addressed. The flexibility, expressed in this chapter,
is quite effective in addressing the majority of pathology encountered
in the brachium.
EXTENSILE ANTERIOR LATERAL APPROACH TO THE HUMERUS
The most common and useful approach to the anterior
aspect of the humerus is through the anterolateral interval. The value
of this exposure is that it can be extended through the deltopectoral
interval to expose the proximal humerus and extension distally allows
adequate access even to the anterior aspect of the elbow joint.
aspect of the humerus is through the anterolateral interval. The value
of this exposure is that it can be extended through the deltopectoral
interval to expose the proximal humerus and extension distally allows
adequate access even to the anterior aspect of the elbow joint.
Indications
Fracture of the proximal mid and midshafts of the
humerus, malignancy, osteomyelitis, access to shift for periprosthetic
fracture, and revision.
humerus, malignancy, osteomyelitis, access to shift for periprosthetic
fracture, and revision.
Position
The patient is placed in the semi-sitting, barber chair
position or supine on the table with the arm resting to the side and
the forearm across the abdomen.
position or supine on the table with the arm resting to the side and
the forearm across the abdomen.
-
Note: By tilting the table 10 degrees to the contralateral direction easier access is provided.
Preparation
For the proximal exposures, the shoulder and arm is
draped free sufficiently proximally to allow extension to the clavicle
and to expose the shoulder joint if necessary.
draped free sufficiently proximally to allow extension to the clavicle
and to expose the shoulder joint if necessary.
Landmarks
The deltopectoral groove proximally, the lateral margin of the biceps, and the mobile wad distally.
Technique
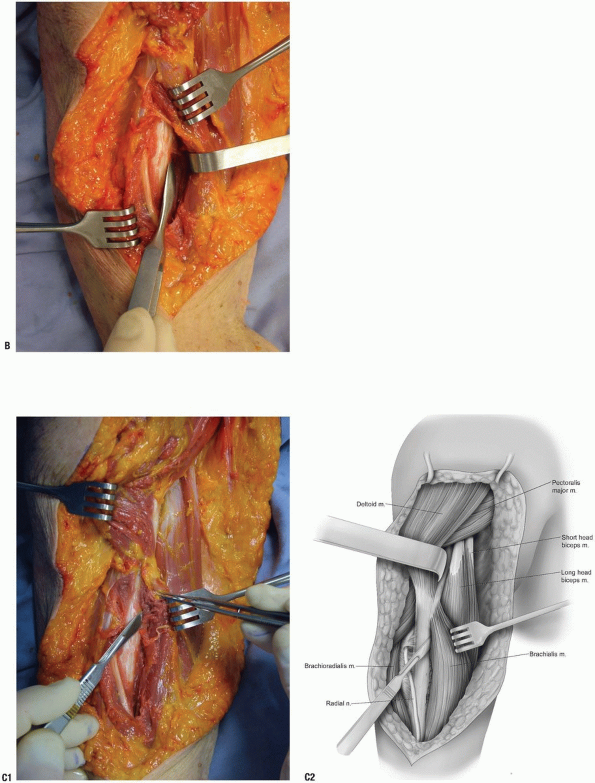
Proximal Portion
-
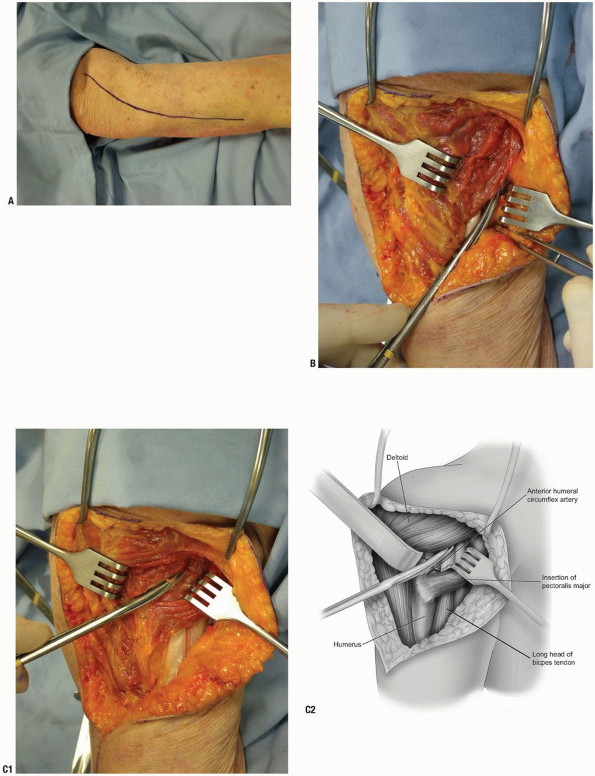
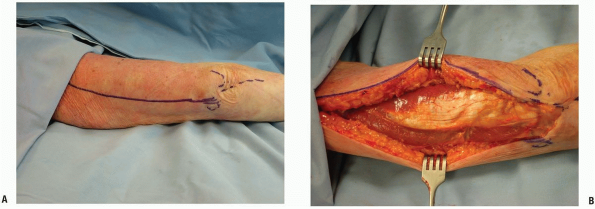
Skin incision: beginning at, or just
distal to, the coracoid proceed distal and lateral in the deltopectoral
groove curving distally at the insertion of the deltoid following the
lateral margin of the biceps (Fig. 4-1A). -
The deltopectoral groove is identified
and is entered. Proximally the medial margin of the deltoid is defined
along with the cephalic vein. This is done by blunt and sharp
dissection (Fig. 4-1B). The insertion of the pectoralis major muscle is identified. -
The proximal humerus is exposed medially
by incising the humeral insertion of the pectoralis insertion and
laterally by mobilizing and elevating the medial margin of the deltoid.
This allows exposure of the humerus proximal to the deltoid insertion.
The long head of the biceps tendon is identified in the medial aspect
of the exposure (Fig. 4-1C). The anterior circumflex humeral artery is present at the proximal aspect of the pectoralis insertion on the humerus. -
Retracting the deltoid laterally and the
pectoralis major medially allows ready access to the proximal humeral
shaft distal to the subscapularis muscle and lateral to the long head
of the biceps tendon (Fig. 4-1D).-
Pearls/Pitfalls:
If a greater medial/lateral exposure is required, the pectoralis
tendinous attachment may be released from the humerus and the deltoid
insertion may be elevated from the lateral aspect of the humerus. Care
must be taken to avoid injury to the axillary nerve with reflection and
retraction of the deltoid.
-
P.92
 |
|
FIGURE 4-1
|
P.93
 |
|
FIGURE 4-1 (Continued)
|
Distal Extension—Anterior/Lateral Humeral Shaft
-
For a distal expansion the skin incision
is carried distally over the lateral margin of the biceps muscle to the
extent needed (see Fig. 4-1A). -
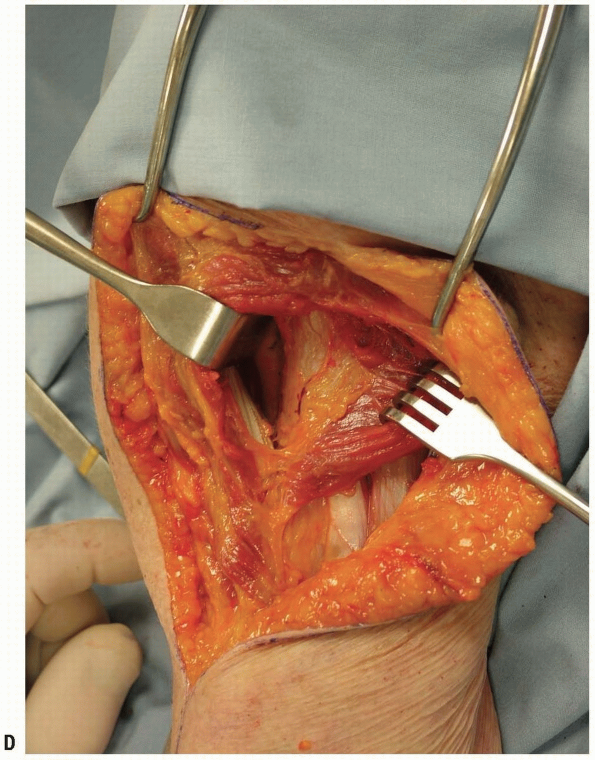
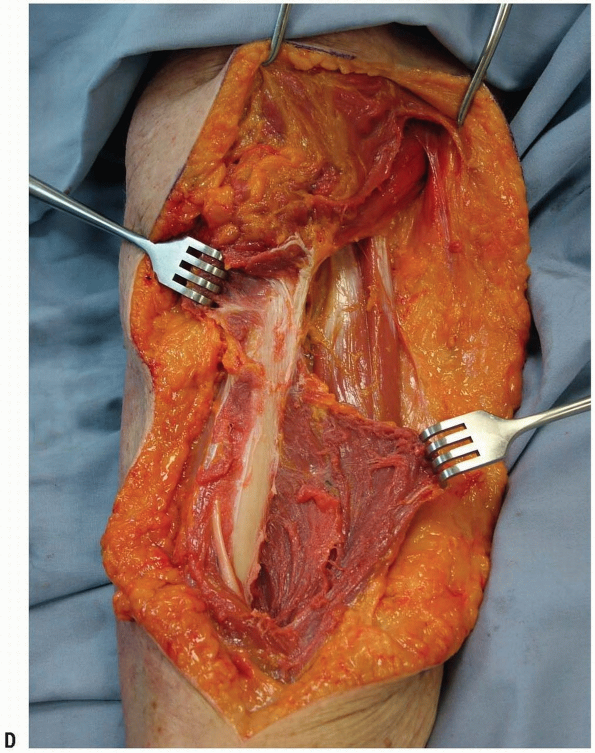
The brachial fascia is split distally
exposing the lateral margin of the biceps. The lateral brachial
cutaneous nerve is identified and protected as it crosses
anterolaterally to the biceps muscle near the tendinous junction (Fig. 4-2A). -
The interval between the biceps and the
brachialis muscles is identified and developed by blunt and sharp
dissection. The biceps is retracted medially and, in so doing, the
musculocutaneous nerve is identified between the two muscles and is
retracted medially with the biceps muscle (Fig. 4-2B). -
Exposure of the humeral shaft is
accomplished by either splitting the brachialis muscles longitudinally
or elevating its lateral attachment from the intermuscular septum of
the humerus. The dissection continues with subperiosteal elevation of
muscle medially and laterally thus exposing the proximal half of the
humerus (Fig. 4-2C).-
Pearls/Pitfalls:
The site of the radial nerve perforation of the intermuscular septum
should be noted and excessive traction at this locus should be avoided
by palpation (Fig. 4-2D). The safest exposure of the shaft is brachialis muscle splitting as this protects the radial nerve from injury.
-
P.94
 |
|
FIGURE 4-2
|
P.95
 |
|
FIGURE 4-2 (Continued)
|
P.96
More Distal Extension
-
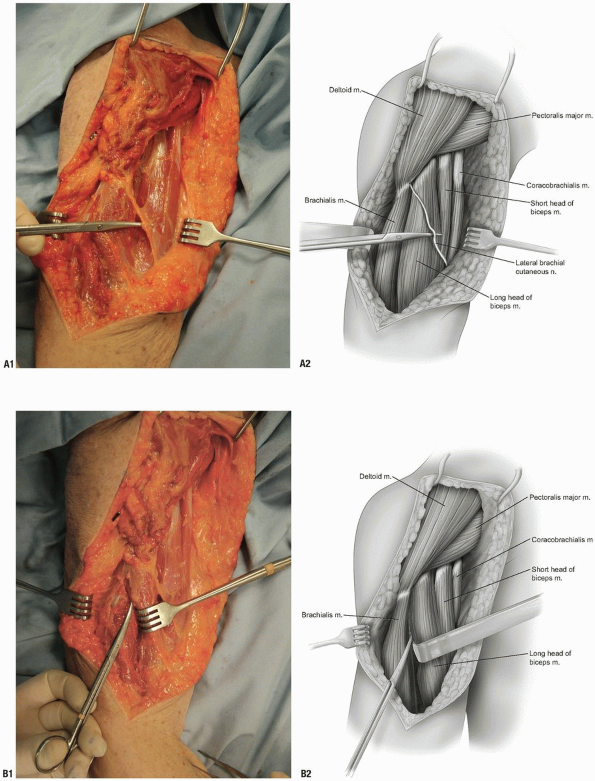
If a more distal or extensive exposure is
required, the interval between the brachialis and the brachioradialis
is further developed at the site of the radial nerve as it emerges from
the intermuscular septum. -
The radial nerve is palpated or observed on the undersurface of the brachioradialis and is exposed by sharp dissection (Fig. 4-3A).
-
The brachialis muscle is retracted
medially protecting the cutaneous branch of the musculocutaneous nerve
and the humeral shaft is exposed with a periosteal elevator. The radial
nerve is protected and retracted laterally (Fig. 4-3B). -
The humeral shaft may be further exposed
by sharp dissection proximally to the lateral origin of the brachialis
muscle on the humerus which is confluent with the deltoid attachment
distally (Fig. 4-3C). Both attachments may be released to afford complete access to the entire proximal two-thirds of the humeral shaft (Fig. 4-3D).
 |
|
FIGURE 4-3
|
P.97
 |
|
FIGURE 4-3 (Continued)
|
P.98
 |
|
FIGURE 4-3 (Continued)
|
POSTERIOR EXPOSURES
The Extensile Posterior Medial Exposure of the Humerus (Mayo Exposure)
We have found this approach extremely valuable for
exposing the posterior aspect of the humerus since it allows extension
distally by employing the triceps reflexion exposure from the
olecranon. The unique (Mayo) feature is to the manner of exposing and
protecting the radial nerve.
exposing the posterior aspect of the humerus since it allows extension
distally by employing the triceps reflexion exposure from the
olecranon. The unique (Mayo) feature is to the manner of exposing and
protecting the radial nerve.
Indications
Fractures of the posterior aspect of the humerus,
extensile exposure for revision of total elbow, and humeral and ulnar
components.
extensile exposure for revision of total elbow, and humeral and ulnar
components.
Position
The patient is supine and the arm is brought across the
chest. The surgical table is tilted 10 degrees to the contralateral
side.
chest. The surgical table is tilted 10 degrees to the contralateral
side.
Landmarks
Olecranon, medial epicondyle distally.
Technique
-
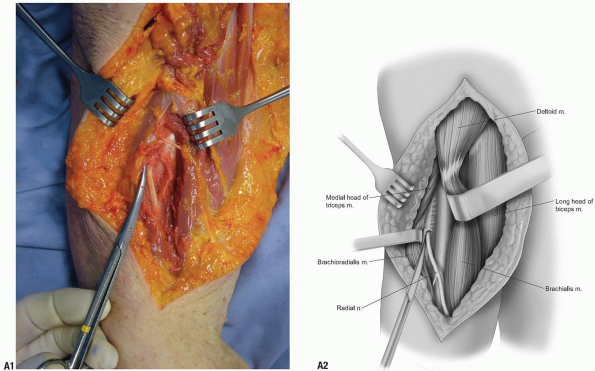
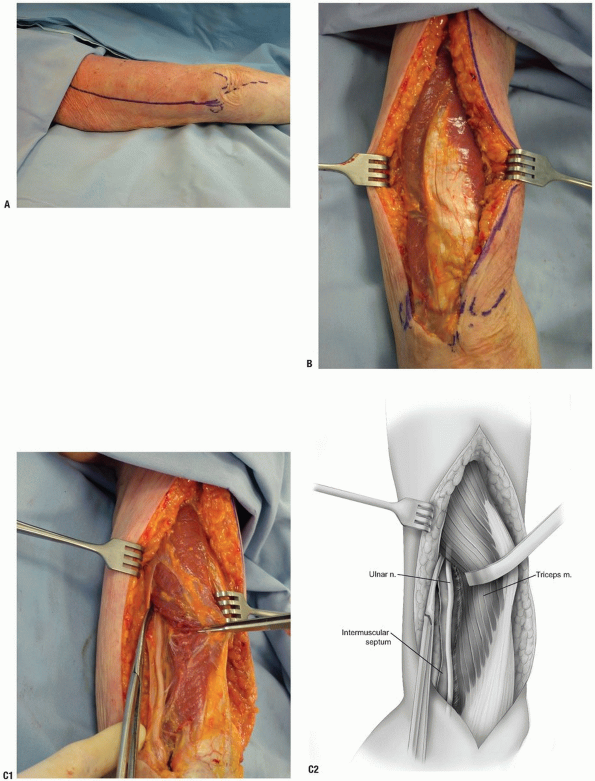
Skin incision: proximally from the
posterior medial aspect of the triceps in line with the long head,
distally between the medial epicondyle and tip of the olecranon (Fig. 4-4A).-
Note: The
skin excision can be extended distally over the subcutaneous border of
the ulna if required. This provides an extensile exposure that can
include the elbow joint and entire humeral shaft.
-
-
The skin and subcutaneous tissue is
entered. The ulnar nerve is identified distally at the cubital tunnel
and skin flaps are raised medially and distally (Fig. 4-4B). -
The ulnar nerve is released as it lies on
the anterior surface of the intermuscular septum. The nerve is
mobilized including release of the ligament of Struthers proximally.
The nerve is identified distally to the level of the cubital tunnel but
the cubital tunnel retinaculum is not released unless an extensile
exposure is performed distally (Fig. 4-4C). -
With sharp dissection, the medial head of the triceps is freed from the distal aspect of the humerus (Fig. 4-4D). The triceps muscle is elevated and retracted laterally.
-
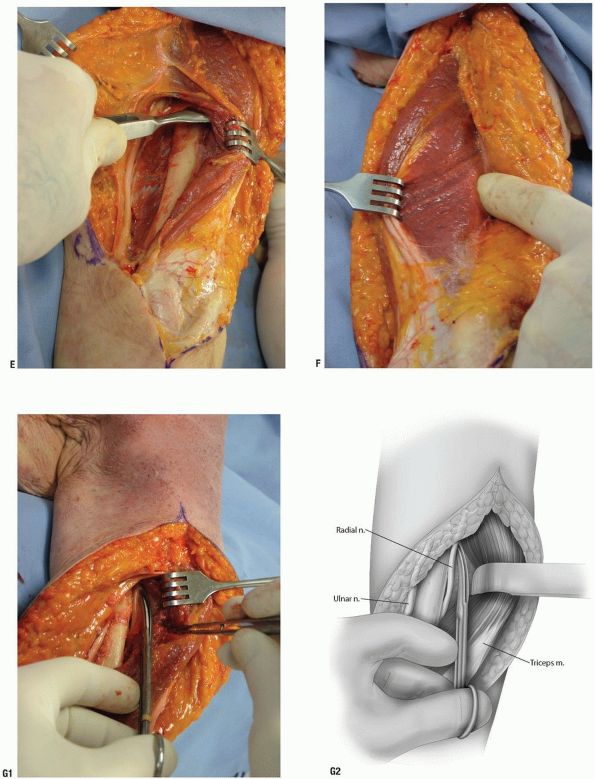
The muscle is then easily elevated from the entire posterior medial aspect of the humerus with a periosteal elevator (Fig. 4-4E).
-
Note: The
critical departure of this exposure is that laterally elevating the
radial nerve subperiosteally provides more proximal exposure of the
humerus.
-
-
At this point the triceps position is
restored and is retracted medially. A subcutaneous flap is elevated
laterally. The location of the radial nerve is identified by palpation
as it penetrates the intermuscular septum (Fig. 4-4F). -
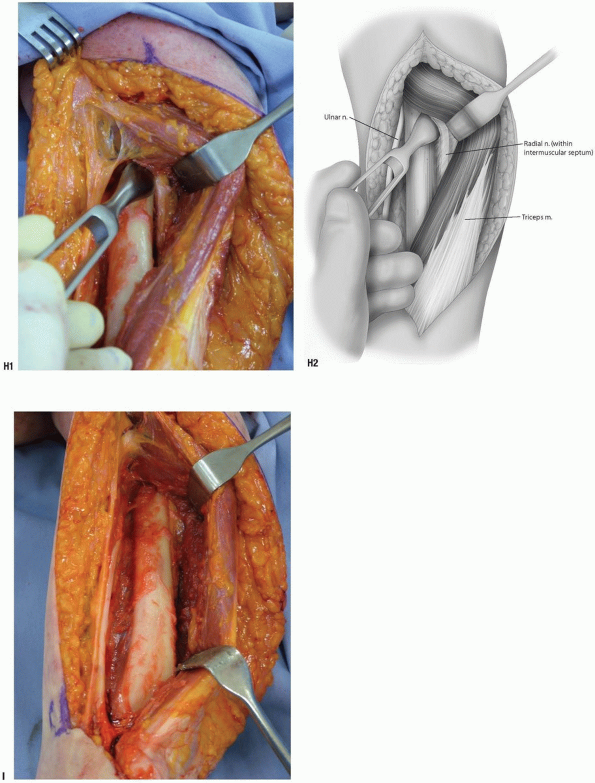
The triceps muscle is then again elevated
and further reflected from medial to lateral. The radial nerve is
identified at the site of penetration of the intermuscular septum
laterally which is then elevated from the lateral aspect of the humerus
(Fig. 4-4G). This affords greater access to the proximal aspect of the humerus (Fig. 4-4H). -
The radial nerve is protected and retracted laterally for greater exposure of the posterior proximal aspect of the humerus (Fig. 4-4I).
-
Pearls/Pitfalls:
If concern regarding impingement or pressure on the radial nerve exists
the nerve is exposed and decompressed by incising the intermuscular
septum. Further, since the radial nerve has been freed from the
intermuscular septum, it is safely protected and is retracted medially
with the brachioradialis muscle distally.
-
-
Closure: The muscle is allowed to return
to its anatomic position. If the triceps has been reflected, the
recommended reattachment is described in the elbow exposure chapter
(see Fig. 3-11). Otherwise, only a subcutaneous and skin closure is required.
P.99
 |
|
FIGURE 4-4
|
P.100
 |
|
FIGURE 4-4 (Continued)
|
P.101
 |
|
FIGURE 4-4 (Continued)
|
P.102
 |
|
FIGURE 4-4 (Continued)
|
P.103
Distal Extension
If more distal exposure is necessary, the triceps may be
reflected from the tip of the olecranon using the Bryan-Morrey
technique. This allows complete exposure of the entire posterior
humerus, elbow joint, and proximal ulna.
reflected from the tip of the olecranon using the Bryan-Morrey
technique. This allows complete exposure of the entire posterior
humerus, elbow joint, and proximal ulna.
Posterior Triceps Splitting Approach
This along with exposure of the ulna is the easiest and safest exposure of the upper extremity.
Indications
Mid and distal shaft fractures, when extended distally,
can be used for exposure for total elbow arthroplasty and fracture of
the midshaft of the humerus.
can be used for exposure for total elbow arthroplasty and fracture of
the midshaft of the humerus.
Position
The patient is supine and the arm brought across the chest. The table is tilted 10 degrees away from the involved extremity.
Landmarks
Tip of olecranon, ulnar nerve, and medial and lateral epicondyle.
Technique
-
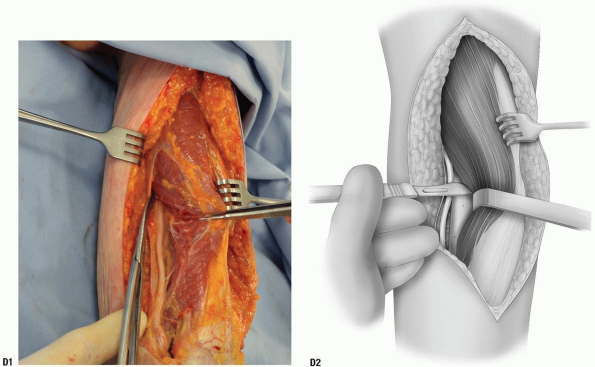
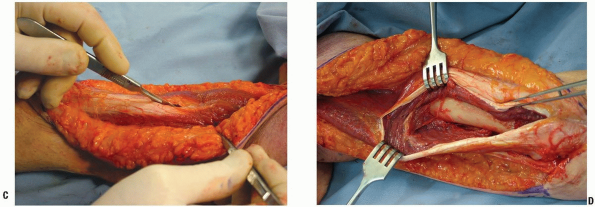
Skin incision: a longitudinal skin
incision is made from the tip of the olecranon distally to the
posterior aspect of the deltoid proximally. The length is dictated by
the pathology (Fig. 4-5A). -
Flaps are elevated medially and laterally
and the tendon of the triceps distally and the muscle fibers proximally
are identified (Fig. 4-5B). -
A longitudinal incision is made in the tendinous portion of the triceps exposing the posterior aspect of the humerus (Fig. 4-5C).
-
The triceps muscle is split proximally
and distally. The tendon is incised to the level of its attachment on
the olecranon. Subperiosteal dissection medially and laterally exposes
the posterior aspect of the humerus (Fig. 4-5D).
P.104
 |
|
FIGURE 4-5
|
 |
|
FIGURE 4-5 (Continued)
|
RECOMMENDED READING
Banks S, Laufman H. An Atlas of Surgical Exposures of the Extremities. Philadelphia: W.B. Saunders Co., 1953.
Campbell WC. Incision for exposure of the elbow joint. Am J Surg 1932;15:65-67.
Grant JCB. An Atlas of Anatomy, 6th ed. Baltimore: Williams & Wilkins Co., 1972.
Gray H. The Anatomy of the Human Body, 29th ed. Philadelphia: Lea & Febiger, 1975.
Henry AK. Extensile Exposure, 2nd ed. New York: Churchill-Livingstone, Inc., 1963.
Hollinshead WH. Anatomy for Surgeons: The Back and Limbs, 3rd ed. Philadelphia: Harper & Row, 1982.
Hoppenfeld S, deBoer P. Surgical Exposures in Orthopaedics: The Anatomical Approach, 1st ed. Philadelphia: JB Lippincott Co., 1984.
Reckling FW, Reckling JB, Mohr MC. Orthopedic Anatomy and Surgical Approaches. St. Louis: Mosby Year-book, 1990.
Tubiana R, McCullough CJ, Masquelet AC. An Atlas of Surgical Exposures of the Upper Extremity. London: Martin Dunitz Publisher, 1990.
