Tibia and Fibula
both a grasp of the pertinent anatomy and knowledge of possible
approaches. Whether the operative procedure is done for a congenital
abnormality, an acute fracture or nonunion, or for a complex joint
reconstruction, the surgeon desires the best view with the least trauma
to the tissues.
extremity one must have an absolute knowledge of the relevant anatomy
of the entire lower extremity. The direction of approach will be
dictated by location and pathology. The soft tissue and bony
architecture are reasonably predictable from one patient to the next
with little variability except in pathologic processes. A thorough
understanding of normal anatomy is required to recognize abnormal
anatomy.
as it branches to enter the anterior and posterior aspects of the leg.
The posterior tibial artery enters the deep posterior compartment of
the leg, traveling just posterior to the tibialis posterior muscle. The
deep peroneal artery also runs in the deep compartment, lateral to the
tibial nerve. The anterior tibial artery crosses superior to the
interosseous membrane and travels just anterior to it. In the distal
third of the leg it begins to proceed anteriorly.
the femoral nerve, which innervates the medial aspect of the distal
thigh around the level of Hunter’s canal and continues distally in a
curvilinear pattern to provide sensation along the medial leg and
proximal ankle. One of its larger branches, the infrapatellar branch of
the saphenous nerve, crosses medially to laterally across the anterior
aspect of the leg near the level of the inferior pole of the patella.
This is frequently transected during anterior approaches of the knee.
The saphenous nerve travels primarily down the medial aspect of the leg
on the medial head of the gastrocnemius, along with the greater
saphenous vein.
just lateral to the posterior tibial artery. The sural cutaneous nerve
is a branch of the tibial nerve, which is located in the midline of the
posterior aspect of the leg and is usually lateral to the small
saphenous vein, supplying cutaneous branches through the fascia to the
posterior aspect of the calf.
the common peroneal nerve at the level of the proximal fibula. Along
with innervating the muscles of the lateral compartment of the leg, the
nerve continues to the dorsum of the foot after piercing the anterior
fascial compartment approximately
10
to 12 cm proximal to the tip of the lateral malleolus. Its cutaneous
innervation is to the dorsum of the foot, excluding the first webspace.
The deep peroneal nerve runs in the anterior compartment with the
anterior tibial artery and becomes superficial only after it passes
through the anterior compartment and to the extensor retinaculum where
it supplies cutaneous sensation to the first webspace.
aspect of the leg with the lesser saphenous vein. At approximately the
level of the junction of the proximal two-thirds and distal one-third
of the leg, the nerve begins to take a lateral course with the vein
curving posterior and then distal to the lateral malleolus, supplying
sensation to the lateral ankle as well as the lateral aspect of the
hindfoot. Transection of this nerve during exposure of the ankle or
calcaneus may result in painful neuroma and/or numbness along the
lateral aspect of the foot, which may have irritating consequences.
be compartmentalized to simplify the anatomy, as well as the surgical
approaches. The leg may be divided into four anatomical compartments.
anterior, extensor hallucis longus, and extensor digitorum. Its nerve
supply is a branch of the common peroneal nerve, the deep peroneal, and
its vascular supply is from the anterior tibial artery.
longus and the peroneus brevis, which are supplied by the second branch
of the common peroneal nerve, the superficial peroneal nerve.
superficial and deep compartments with the superficial compartment
being comprised to the two heads of the gastrocnemius muscle, as well
as the soleus and plantaris. The deep posterior compartment is occupied
by the tibialis posterior, the flexor digitorum longus, and the flexor
hallucis longus muscles. The posterior compartment has its vascular
supply from the posterior tibial artery and the nerve supply is from
the tibial nerve. The medial and lateral intermuscular septae are more
defined in the leg than in the hip. The lateral intermuscular septum is
pierced by the superficial peroneal nerve, approximately 12 cm proximal
from the tip of the lateral malleolus as it crosses from the lateral to
the anterior compartment of the distal leg.
incisions for reduction and fixation, one anterolaterally, described
below, and another posteromedially.
-
Incision: the incision is made in line
with the posterior aspect of the tibial shaft. As it is parallel to the
pes tendons, the saphenous nerve is encountered and retracted
anterosuperiorly (Fig. 10-1D). -
The pes tendons are mobilized anteriorly; the medial gastrocnemius fascia is released from the proximal tibia.
-
With posterior retraction of the gastrocnemius, the posteromedial proximal tibia is thus exposed (Fig. 10-1E). Parts of the semimembranosus insertion may have to be elevated as well (Fig. 10-1F,G).
 |
|
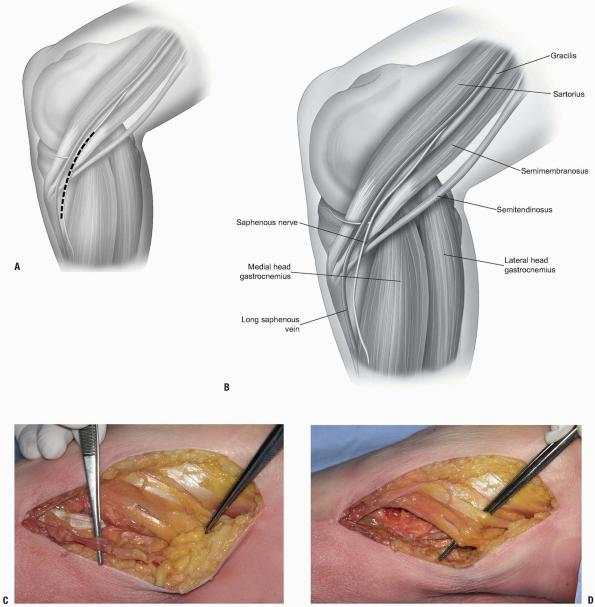
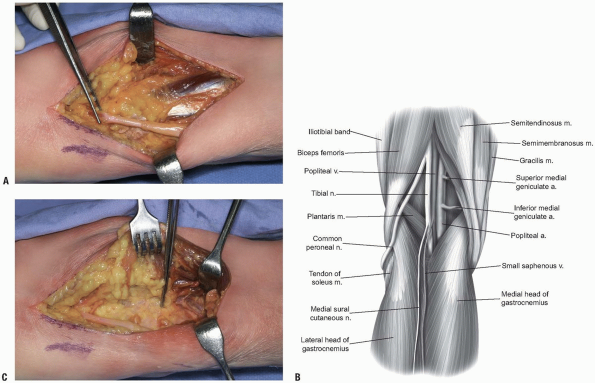
FIGURE 10-1 A-C:
Patient in supine position with the leg flexed and externally rotated. Proximal is to the viewer’s right, posterior to the bottom of the photograph. Forceps to the right is on the pes tendons, forceps to the left is on the saphenous nerve. D: Forceps is elevating the pes tendons. |
 |
|
FIGURE 10-1 (Continued) E: Retractor to the right is holding the pes tendons. Forceps to the left is pointing out the medial gastrocnemius fascia. F,G:
Gastrocnemius retracted posteriorly demonstrating exposure of proximal medial tibia on posterior aspect. The oblique portion of the medial collateral ligament is just distal to the forceps. |
 |
|
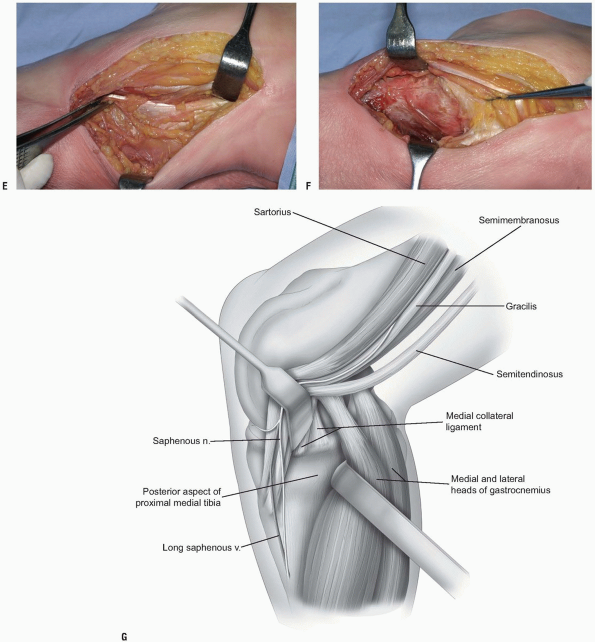
FIGURE 10-2 A:
Patient is prone; proximal is to the viewer’s right, the medial is the the bottom of the photo. The medial head of the gastrocnemius fascia is held by the forceps, the medial collateral ligament is beneath the pes tendons which are being held by the forceps at the bottom of the photograph. B: Medial head of the gastrocnemius retracted to the superior side of the photograph, forceps at the knee joint line. |
exposure have also been described. Placing the patient in the prone
position makes the exposure easier but also requires a second
positioning if one desires to expose the anterolateral tibia as well (Fig. 10-2).
-
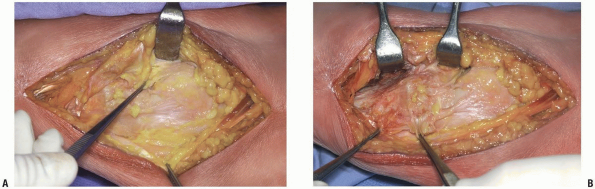
Incision: a straight or lazy S-shaped
incision is usually centered over the lateral epicondyle and extended
distally in line with the iliotibial band toward Gerdy’s tubercle (Fig. 10-3A,B). Extension of the incision distally is dictated by the amount of metadiaphyseal exposure needed. -
Full thickness soft tissue flaps are elevated to expose the iliotibial band. This is then split in line with its fibers (Fig. 10-3C,D). If an arthrotomy is desired, a submeniscal entry is preferred.
-
The coronary ligament is incised and the meniscus is retracted superiorly to visualize the joint surface (Fig. 10-3E).
-
The origins of the anterior compartment
muscles are elevated and retracted posterolaterally as needed to
visualize the proximal tibia (Fig. 10-3F).
 |
|
FIGURE 10-3 A: Incision for anterolateral proximal tibia exposure.
|
 |
|
FIGURE 10-3 (Continued) B: Incision for anterolateral proximal tibia exposure. C,D: Iliotibial band split in line with its fibers. E:
Iliotibial band freed from Gerdy’s tubercle, the extensor muscle attachment seen to the viewer’s right can be elevated as needed for exposure of the proximal tibia. F: A sub-meniscal arthrotomy has been performed as well. The lateral tibial plateau articular surface is visible. This opening can be increased by application of a varus force to the knee. |
-
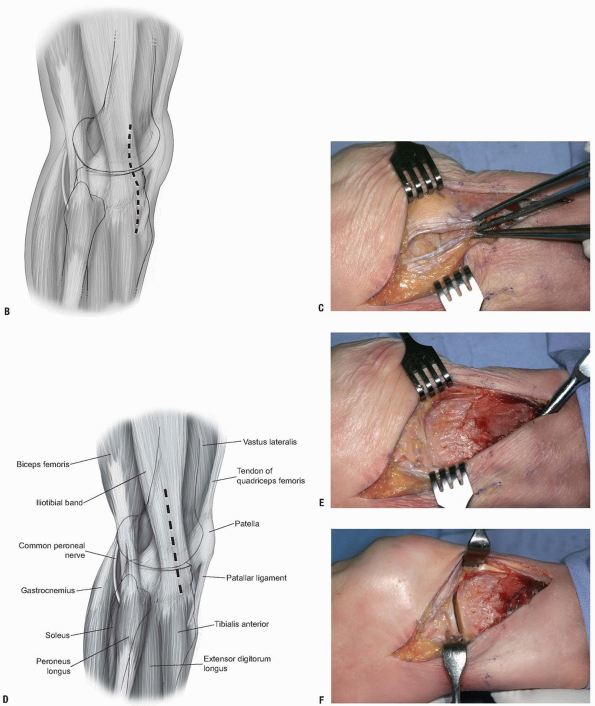
Incision: a curvilinear incision is made
proximally over the biceps tendon, and then curving slightly medially
over the proximal fibula (Fig. 10-4A,B). -
The peroneal nerve is identified (Fig. 10-4A,B).
-
The lateral head of the gastrocnemius is retracted medially (it may have to be released) and the soleus freed from its origin (Fig. 10-4C).
The popliteus tendon can be retracted proximally and medially or
released (to be repaired at the time of closure). The posterior-lateral
tibial articular surface can then be exposed by a submeniscal
arthrotomy, releasing the coronary ligament inferior to the meniscus
and medial to the popliteal tendon hiatus. The breadth of exposure of
the posterolateral tibia is relatively small.
 |
|
FIGURE 10-4 A,B:
Proximal is to the viewer’s left. The common peroneal nerve is held by the forceps. The fascia of the lateral head of the gastrocnemius is visible. C: The lateral head of the gastrocnemius had been retracted to the superior side of the photograph. The forceps is on the knee joint line but the distal (to the viewer’s right) extent of the tibial exposure is limited. One can release the lateral head of the gastrocnemius, but the popliteal artery is medial and anterior tibial artery branches off, proceeding anteriorly and laterally relative to the retractor. |
due to the superficial location of the anterior border of the
triangular-shaped tibia. The anteromedial border can easily be palpated
from the proximal medial aspect of the tibia at the pes anserine
insertion all the way distal to the medial malleolus. The skin incision
is typically made in a longitudinal fashion just medial to the bony
prominence to help facilitate soft tissue closure. The entire anterior
two-thirds may then be easily exposed by performing a subperiosteal
dissection off the medial side of the tibia. Except for the pes
anserine insertion proximally, the anteromedial surface is free of any
soft tissue attachments. The saphenous nerve and vein are the only
neurovascular structures at risk with this exposure. Skin and bone
vascularity are an issue with this approach so although the tibia is
easily exposed via this route, it is less frequently used.
implant, the anterolateral approach allows for placement of the device
between the tibialis anterior muscle and the bone. The incision is made
just lateral to the tibial crest. The anterolateral aspect of the
tibialis anterior is elevated off the surface of the bone. The main
neurovascular structures at risk during this approach are the deep
peroneal nerve and anterior tibial artery, which will remain unharmed
if dissection is carried out subperiosteally in the anterior
compartment.
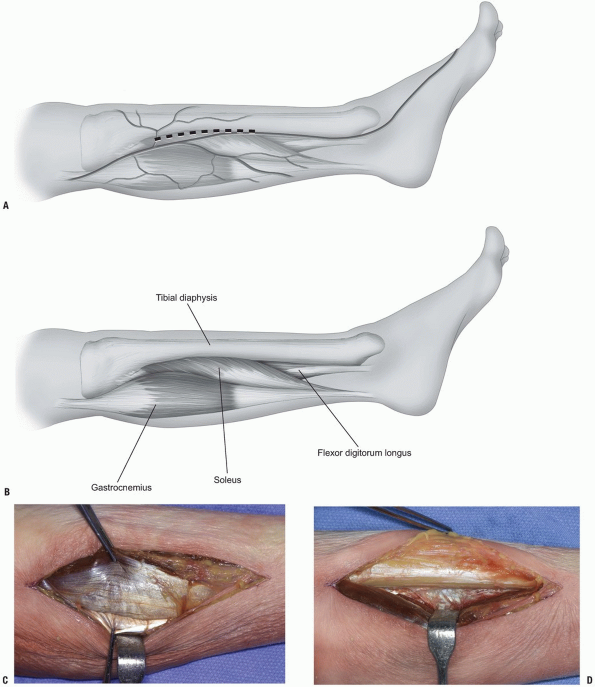
-
Incision: for release of the posterior
compartments of the leg, or for exposure of the posterior part of the
diaphysis of the tibia, one can make an incision just posterior to the
tibia. If one is releasing both compartments, the incision is made
about 2 cm posterior to the posterior tibial border. If one is
approaching the posterior tibia, the incision is at or just posterior
to the tibial border. -
Care should be taken to identify the
greater saphenous vein which courses along the medial aspect of the
tibia. After skin retraction, the posterior aspect of the tibia is
identified and the fascia incised (Fig. 10-5A-C). Both the superficial compartment and the deep compartment can be released through this incision. -
If access to the tibia is desired, the
deep muscles are retracted posteriorly. The neurovascular bundle of the
deep posterior compartment is located lateral and slightly posterior to
the first muscle belly encountered—that of the flexor digitorum longus (Fig. 10-5D).
 |
|
FIGURE 10-5 A-C:
Posteromedial approach to the tibia diaphysis. The soleus muscle is held by the upper forceps, the gastrocnemius fascia by the lower forceps. D: The deep compartment muscles are retracted toward the bottom of the photograph. The posterior and posteromedial aspect of the tibial shaft are visible. |
frequently used in the posttraumatic setting where bone grafting of the
tibia is performed in a patient with compromised anteromedial soft
tissues.
-
Incision: the incision is longitudinal, centered just posterior to the fibula.
-
Dissection is carried down through the
overlying fascia, which is split in line with the skin incision. The
plane between the soleus and the peronei is entered. The soleus is
dissected free from the fibula and the deep posterior compartment is
entered. The flexor hallucis muscle is released from the fibula (Fig. 10-6A). -
The peroneal artery and vein are deep to
this great toe flexor muscle. The remaining deep flexor musculature is
dissected off of the interosseous membrane and the tibia approached (Fig. 10-6B).-
Pearls/Pitfalls:
Often, because of the scarring, it is easier to approach the involved
site from proximally, where the anatomical planes are more distinct.
Although a similar approach can be carried out anterior to the
interosseous membrane, as well through a more anterior lateral
incision, the neurovascular bundle is at much more risk via this route.
-
compartments are released via a longitudinal incision centered midway
between the tibia and fibula. The anterior intermuscular septum is
identified and the fascia released both anterior and posterior to the
septum.
 |
|
FIGURE 10-6 A:
Posterolateral approach to the tibia. The peronei are retracted anteriorly (upper aspect of photograph). The soleus is retracted posteriorly and the fibula is visible in the middle of the wound. B: By staying directly on the fibula as its posteromedial surface angles anteriorly, one will come to the interosseous membrane. The posterior musculature is elevated from the membrane until the tibia is visible. Here the tibial diaphysis is visible in the base of the wound. |
and internal fixation, osteotomy for nonunion of the tibia, or for
vascularized bone grafting is made through a direct lateral approach.
The typical skin incision is made approximately just posterior to the
fibula and may be extended from the tip of the lateral malleolus
proximally to the head of the fibula. There is very little subcutaneous
dissection distally. Care must be taken proximally to avoid injury to
the common peroneal nerve, as it is located in a subcutaneous location
while it crosses the fibular neck. The muscular interval used to gain
access to the fibula is between the soleus posteriorly and the peroneal
muscles anteriorly. The majority of the soft tissue attachments will be
found on the proximal two-thirds of the fibula. The distal one-third
exposure is easily made after incising the deep fascia of the leg. At
this level the peroneal musculature is retracted posteriorly to access
the bone. Again, the amount of soft tissue elevation and dissection
from the fibula should be dictated by the least amount of exposure
needed. In the distal portion of the incision, at a variable length
above the mortise, the superficial peroneal nerve will be encountered.
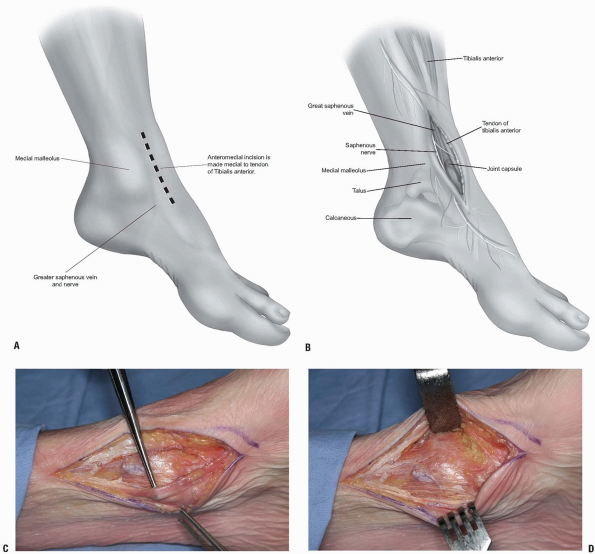
involves entering via the plane between the tibialis anterior medially
and the neurovascular bundle and toe extensors laterally. This works
well for intra-articular ankle procedures but not as well for distal
tibial fracture reduction and fixation. The anteromedial approach works
well for medial plating and fractures of the distal tibia in which the
medial side has failed in compression and requires plating and bone
grafting.
-
Incision: the 8 to 10 cm incision is made medial, rather than lateral, to the tibialis anterior tendon (Fig. 10-7A-C).
-
That tendon is retracted laterally along with the other structures lateral to it (Fig. 10-7D).
-
One must identify and preserve the
saphenous nerve; otherwise, the medial malleolus and medial distal
tibia are well presented via this approach. The tubercle of the Chaput
is not as well visualized via this approach, however.
 |
|
FIGURE 10-7 A-C:
Anteromedial approach to the distal tibia. Proximal is to the viewer’s left. The forceps is elevating the saphenous nerve and vein. D: The knee retractor is holding the anterior tibial tendon and ankle capsule is directly below it in this photograph. |
 |
|
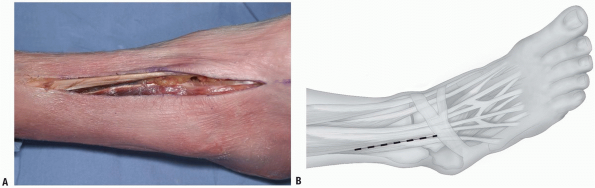
FIGURE 10-8 A,B: Incision for anterolateral approach to the distal tibia.
|
be easily exposed anterolaterally. The window is opened by retracting
the extensors of the ankle and toes medially along the neurovascular
bundle.
to watch out for the superficial peroneal nerve as it crosses the
fibula and proceeds distally and medially. The peroneus tertius is
retracted laterally.
-
Incision: the incision is made in line with the fourth metatarsal distally. It is a straight incision, crossing the ankle joint (Fig. 10-8A,B).
-
It can be extended proximally as
necessary, freeing up the anterior compartment muscles as necessary. It
can be extended distally and allows access to the dorsal lateral aspect
of the talar neck as well, if necessary. -
After incising the skin, the retinaculum
is encountered and incised as well. The tendons and neurovascular
structures are retracted as noted (Fig. 10-8E,F).
 |
|
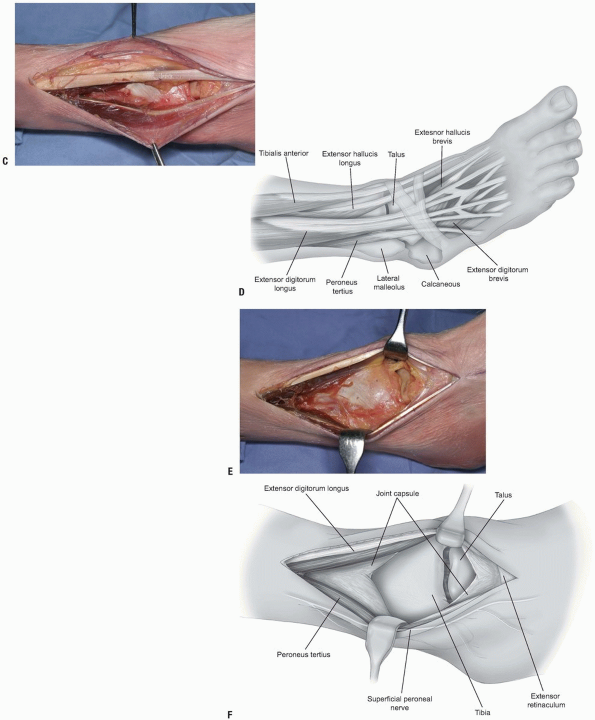
FIGURE 10-8 (Continued) C,D:
Extensor muscles to the top of the photograph, peroneus tertius to the bottom, anterolateral tibia and talus are easily visible. E,F: With retraction, the whole anterior tibia is exposed. The superficial peroneal nerve is behind the lower retractor, with the peroneus tertius tendon. |
the talus via a posterior medial approach. This can be accomplished
with the patient prone or supine.
placed under the opposite hip. The ipsilateral leg is then flexed and
externally rotated.
-
Incision: the incision is made at
approximately the midpoint between the Achilles tendon and the medial
malleolus, with care taken to avoid the saphenous vein (Fig. 10-9A-C). -
The plane past the neurovascular bundle
can either be via the flexor digitorum longus medially and the
neurovascular bundle laterally, between the neurovascular bundle and
the flexor hallucis longus, or by retracting the flexor hallucis
medially and protecting the nerve and artery (Fig. 10-9D).-
Note: One
cannot directly visualize the intracuticular aspect of the distal tibia
directly via this approach but it works well for indirect reduction
techniques and also for posteromedial fractures of the talus.
-
-
It is also possible by making the
incision more anteriorly over the posterior aspect of the medial
malleolus, to access the posterior distal tibia and the medial
malleolus both, by releasing the cephalad attachments of the posterior
tibial sheath, and retracting the tendon distally and posteriorly (Fig. 10-9E).
One can, by retracting the malleolar fragment distally, directly assess
the reduction of the articular surface at the posterior aspect.
 |
|
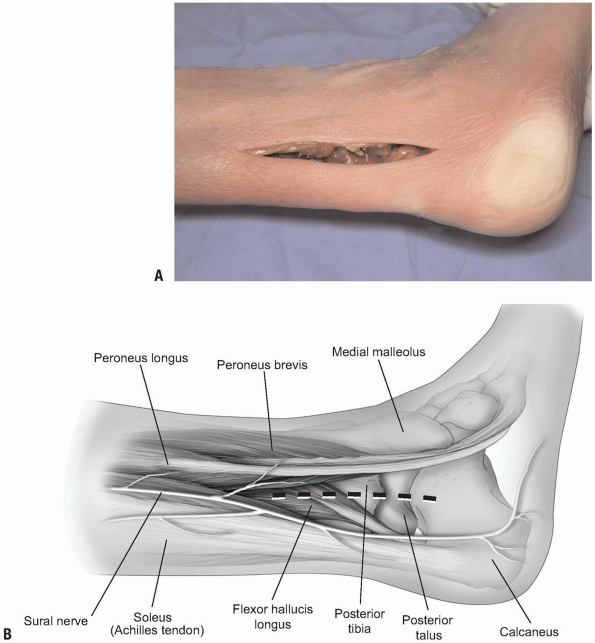
FIGURE 10-9 A-C:
Posteromedial approach to the distal tibia, this exposure allows access to both the posterior tibia and the articular surface if there is a medial malleolar fracture present, or an osteotomy performed. D: Posterior tibial tendon visible along the posterior aspect of the tibia. E: Both the tibial and talar articular surfaces are visible, along with the posterior tibia, through this approach. This approach works well for the supination-adduction type ankle fracture pattern where there is medial plafond depression that has to be elevated. |
supine positioning can be utilized with a bump under the ipsilateral
hip. The patient can also be placed in a sloppy lateral position.
Positioning may depend on the patient’s other injuries.
-
Incision: an incision is made between the fibula and the Achilles tendon (Fig. 10-10A,B).
-
The dissection is carried medial to the peroneal musculature. The sural nerve must be identified and protected (Fig. 10-10C,D).
-
The flexor hallucis longus muscle is elevated as needed and retracted medially (Fig. 10-10E). Both the posterior-lateral tibia and the posterior aspect of the fibula can be approached from this direction.
-
Note: Like
with the posteromedial approach, the articular surface of the distal
tibia won’t be directly seen with this exposure. Both of these
approaches work well if one is applying a buttress plate, however.
Reduction and plating of fibula can be accomplished as well and one can
maintain a very wide skin bridge between anterior and posterior
incisions.
-
 |
|
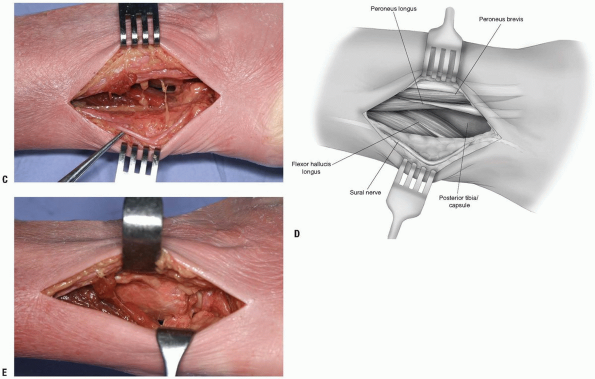
FIGURE 10-10 A,B: Incision for approach to posterolateral distal tibia.
|
 |
|
FIGURE 10-10 (Continued) C,D: Sural nerve shown next to forceps. Peroneal tendons superiorly in the photograph. E:
The peroneal tendons retracted anteriorly, the flexor hallucis muscle belly is elevated and retracted posteromedially. The posterior distal tibia is visible along with the posterior aspect of the talus. |
DM, Nork SE, Mills WJ, et al. Complications associated with internal
fixation of high-energy bicondylar tibial plateau fractures utilizing a
two-incision technique. J Ortho Traumaa 2004;18:649-657.
JK, Ryzewicz M, Hartshorn C, et al, Optimizing the management of Moore
type I postero-medial split fracture dislocations of the tibial head:
Description of the Lobenhoffer approach. J Ortho Trauma 2007;21:330-335.
