OSTEOTOMIES OF THE KNEE FOR OSTEOARTHRITIS
– JOINT RECONSTRUCTION, ARTHRITIS, AND ARTHROPLASTY > Lower
Extremity > CHAPTER 107 – OSTEOTOMIES OF THE KNEE FOR OSTEOARTHRITIS
Professor of Surgery, Cornell University Medical College, Chief: Knee
Service, Associate Attending Surgeon, Hospital for Special Surgery, New
York, NY, 10021.
address osteoarthritis of the knee. Surgery was performed to shift load
bearing from one arthritic tibiofemoral compartment to the other, less
affected compartment. Success rates of 65% at 10 years (9) and 63% at 9 years (24)
are reported after high tibial osteotomy (HTO) for medial compartment
arthritis. Current prosthetic knee arthroplasty techniques have
provided successful results in over 93% of patients at 10 years (12). The role of osteotomy has decreased in the face of these outstanding results from joint replacement (50).
Prosthetic arthroplasty requires activity modification to protect the
implant. The implant also has a finite life span and may require
repeated surgery to replace failed devices. Realignment osteotomy is
viewed as a way to allow unrestricted patient activity and to delay the
time to joint replacement surgery (23,40,42).
was the first to report his experience with femoral and tibial
osteotomies to treat osteoarthritis with associated valgus and varus
knee alignment. Jackson and Waugh (26)
published a more detailed follow-up report. Their greatest success was
with tibial osteotomy to correct varus knees. Subsequent reports by
Wardle (47), Garièpy (15), and Coventry (5)
more clearly defined the indications and techniques of the operation,
specifically an osteotomy performed between the tibial tuburcle and the
joint line.
that excessive force carried across the joint from the abnormal
alignment of the limb leads to degeneration within the affected joint
compartment (5,26). A
cadaveric model has demonstrated that increased contact pressures in
the knee accompany increasing varus or valgus alignment of the tibia (33).
With time, the excessive pressure leads to breakdown of the cartilage
matrix, with loss of the cartilage structural integrity (3). The altered stress may also cause architectural changes in the subchondral bone, further altering the joint geometry (4).
In the medial compartment of the knee, for example, once arthritis is
established, serial examination reveals clinical and radiographic
progression in nearly all cases (39). The goal
of realignment osteotomy has been traditionally to alter the vector of
forces across the knee, to unload the affected compartment, and thereby
to gain relief of pain.
osteoarthritis is a lateral closing wedge, valgus-producing proximal
osteotomy. Valgus malalignment is usually due to lateral femoral
condyle undergrowth and is best addressed through distal femoral
osteotomy (16).
Also, patients with anterior cruciate ligament insufficiency with
medial joint space narrowing will benefit from osteotomy. Osteotomy
alone or in conjunction with anterior cruciate ligament reconstruction
will help remove the varus forces that are present. The patient will
generally report morning stiffness and medial knee pain with weight
bearing that is relieved with rest and anti-inflammatory medication.
The patient’s arthritis should be from a structural cause due to
osteoarthritis or posttraumatic arthritis. Knee range of motion should
approach 90° of flexion with full extension. Any laxity should be
addressed before osteotomy, although a lateral closing wedge osteotomy
performed above the tibial tubercle can tighten the medial collateral
ligament (16) by creating a valgus force
sufficient to cause an opening of the medial joint. Also, performing an
open-wedge osteotomy on the medial side will tighten the medial
collateral ligament.
Osteotomy is traditionally reserved for patients younger than 65 years
of age; however, older patients with high activity levels may be
candidates for HTO, whereas younger patients with lower activity levels
may be candidates for knee replacement. The decision to operate must be
individualized to each patient’s circumstance.
valgus-producing osteotomy is symptomatic or radiographic arthritis in
one or both of the other joint compartments. Other generally accepted
contraindications are varus deformity greater than 15°, flexion
contracture greater than 15°, or underlying inflammatory arthritis (1,6,37,42). The procedure, by design, results in valgus alignment of the lower extremity, which may be unacceptable to some patients.
arthritis. Inspect the affected leg for alignment, fixed knee
deformities, range of motion, stability, and the integrity of the skin
on the knee. Radiographs of the knees during weight bearing demonstrate
the extent of arthritis and loss of joint space. Single standing,
full-length radiographs offer the best method to determine limb
alignment and to plan the osteotomy (19).
 |
|
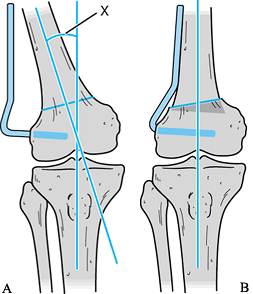
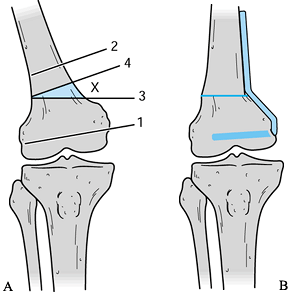
Figure 107.1. Determine the desired angle of correction from standing long-leg films by the method of Miniaci et al. (34). See text for details.
|
-
First, draw the predicted mechanical axis
of the affected limb on the full-length radiograph by connecting a
point from the center of the hip to a point on the lateral tibial
plateau that is one third of the way from the center of the knee to the
lateral margin of the lateral plateau (line A). Extend this line to the
level of the ankle. -
Make a second line (line B) from the
point on the proximal medial tibia that will be the pivot point of the
osteotomy to a point in the center of the ankle. -
Draw a third line (line C) from the
medial pivot point to a point on the predicted mechanical axis (line A)
that is at the level of the ankle. The angle (X) between the second and
third lines (lines A and B) is the angle of the wedge to be resected.
have pointed out that the center of rotation of the deformity, while
close to the knee joint, can vary in position from patient to patient.
The apex of the osteotomy should fall very close to the point of
maximal deformity to avoid the creation of a secondary deformity. The
patient may also have an associated rotational or sagittal plane
deformity. Procurvatum deformity was the most commonly encountered
deformity associated with tibia vara. All of these variations must be
recognized during preoperative planning so that they may be corrected
at surgery.
diagnostic arthroscopy be performed in order to examine the lateral and
patellofemoral joint spaces before osteotomy. However, Keene and Dyreby
(27) demonstrated that lateral compartment involvement noted on arthroscopy does not predict failure of valgus osteotomy. Korn (28)
made the same observation in a more recent study. The combination of a
valgus-producing osteotomy and the Maquet tibial tubercle elevation
procedure for patellofemoral and medial compartment arthritis gives
only 50% good or excellent results in short-term follow-up (2,21,44,). The role of prophylactic osteotomy in patients with excessive varus alignment has not been established.
method of fixation. We prefer internal fixation of the osteotomy with
an L plate and screws, as described by Hofmann et al. (20).
When combined with preservation of the medial tibial cortex, this
construct provides rigid fixation of the osteotomy, which allows early
range of motion of the knee and shorter rehabilitation time (18).
There are two osteotomy systems available in North America that use
this type of plate. Both also use angular cutting jigs to allow more
precise bone cuts.
-
Perform surgery under a spinal or
epidural block. Position the patient supine and use a tourniquet. Give
prophylactic antibiotics before inflation of the tourniquet. A straight
anterior midline incision may be used but will need to be extended
proximally and distally for adequate exposure of the lateral tibia. -
We prefer an L-shaped
incision. Begin it laterally at the joint line and extend it parallel
to the joint to the midline and then extend it distally along the
anterior tibia as necessary. The vertical midline of this incision can
be incorporated into an anterior midline approach for total knee
arthroplasty. -
Dissect the cephalad anterior compartment
muscles at a subperiosteally level off the tibial cortex. Carry the
dissection distally only as far as needed to accommodate the plate. -
Once the lateral tibia is exposed, carry
the dissection posteriorly to the proximal tibiofibular joint. The
tibiofibular joint can be handled in three different ways. The fibular
head may be resected and the lateral collateral ligament sutured to the
iliotibial band (8). Alternatively, a segment of proximal fibula may be resected (34). Finally, the joint may be disrupted, allowing the fibular head to slide proximally when the osteotomy is closed (20).
We prefer the fibular slide because we believe proximal resection
compromises lateral stability of the knee and resection of a shaft
segment puts the superficial peroneal nerve at risk of injury. To
complete the exposure, incise the anterior joint capsule, and place a
periosteal elevator into the joint. Use the elevator to disrupt the
remaining joint capsule. -
After exposing the tibia, line up the
transverse osteotomy jig provided with each system with the articular
surface of tibial plateau under fluoroscopic guidance. Once this jig is
satisfactorily positioned, place two Steinmann pins across the tibial
metaphysis by using the holes in the proximal guide. The Steinmann pins
parallel the articular surface and serve as a reference from which all
cuts are made. Place a variable-angle drill guide over the proximal
pins. The guide directs two distal pins in at the desired angle of the
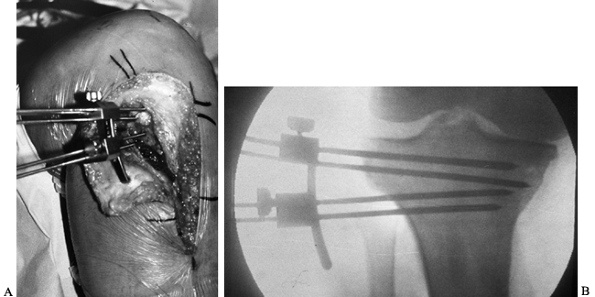
resection (Fig. 107.2). Exchange the variable-angle guide for proximal and distal cutting blocks (Fig. 107.3A), and perform cuts with an oscillating saw (Fig. 107.3B). The two arms of the osteotomy meet at a point just lateral to the medial cortex.![]() Figure 107.2. Tibial osteotomy angle cutting jig in place. B: Fluoroscopic view of angle cutting jig in place.
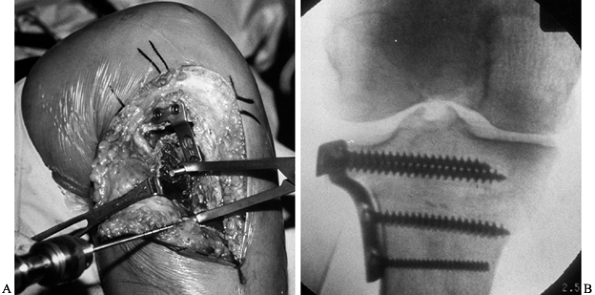
Figure 107.2. Tibial osteotomy angle cutting jig in place. B: Fluoroscopic view of angle cutting jig in place.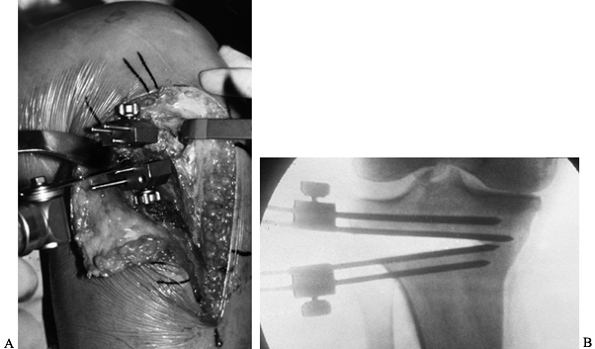 Figure 107.3. A: Osteotomy cutting blocks in place. B: Fluoroscopic view of completed wedge resection.
Figure 107.3. A: Osteotomy cutting blocks in place. B: Fluoroscopic view of completed wedge resection. -
Remove the wedge of bone from the tibia (Fig. 107.4A).
Removing the resection wedge can be difficult if the posterior bone
cuts are incomplete. Poor visualization and concern over the safety of
posterior soft-tissue structures can result in undercutting this
portion of the osteotomy. A hand osteotome can be used to complete the
cut, but the osteotome must not plunge beyond the cortex. A curved
curet is also useful in removing the bone.![]() Figure 107.4. A: Pins have been removed, and the L plate and the proximal cancellous screws have been placed. A ratcheted clamp is in place to close the osteotomy. B: Fluoroscopic view of completed osteotomy with fixation plate.
Figure 107.4. A: Pins have been removed, and the L plate and the proximal cancellous screws have been placed. A ratcheted clamp is in place to close the osteotomy. B: Fluoroscopic view of completed osteotomy with fixation plate. -
Once the wedge is removed, close the osteotomy. Apply the L plate and hold it with two cancellous screws through the proximal, transverse arm of the plate. Each
P.2862P.2863
osteotomy system provides a special ratcheted clamp that attaches to
the distal arm of the plate through an empty screw hole, and to the
tibial cortex by an additional drill hole or separate pin (Fig. 107.4A).
Slowly compress the clamp and close the osteotomy. The medial cortex
should deform rather than fracture. Integrity of the medial cortex is
imperative to maintain stability of the osteotomy. Once the osteotomy
is closed, lock the clamp to hold the osteotomy closed and place two or
three bicortical screws through the distal arm of the plate (Fig. 107.4B). -
Before closing the wound, perform a
subcutaneous fascial release of the anterior compartment muscles off
the tibial crest. Then reapproximate the muscles to the tibial
periosteum by interrupted, absorbable tacking sutures. This covers the
plate and osteotomy site. Close the wound in layers over a drain. Apply
a soft knee wrap in the operating room.
0° to 60°, and advance as tolerated to 90°. Administer antibiotics over
24 hours, and remove the drain on the first or second postoperative
day. Place the patient in a hinged knee brace and encourage knee range
of motion. The brace is worn for 8 to 12 weeks. Allow partial weight
bearing and crutch ambulation. Full activity can be resumed once there
is radiographic evidence of healing. Early motion helps avoid patella
infera (48). We recommend removal of the implant 1 year after surgery.
complications include tibial plateau fractures, superficial wound
infections, deep venous thrombosis and pulmonary emboli, peroneal nerve
palsy, and anterior compartment syndrome (6,19,20,22). Hernigou et al. (19)
reported 10 inadvertent plateau fractures followed for 10 years or
more. All fractures were treated conservatively, healed uneventfully,
and did not seem to affect the results of the surgery. If peroneal
nerve palsy develops, rule out compartment syndrome. Catastrophic
complications reported in the literature are very rare. Coventry (6)
reported one arterial thrombosis leading to limb amputation. The one
study that compared results of staple fixation of the osteotomy with
those of plate fixation noted a much higher rate of wound infection
with the plate fixation (18). Late complications include nonunion, loss of correction, and disease progression in the remaining knee compartments (6,19,22). The method of fixation does not seem to affect the rate of late complications (18).
Failures increase with time owing to progression of arthritis into the
remaining joint compartments or recurrence of varus deformity. We
advise patients to anticipate 8 to 10 years of pain relief following
tibial osteotomy. Failed HTO is best addressed with total knee
arthroplasty. Unfortunately, proximal tibia osteotomy can compromise
the result of total knee arthroplasty (35,38,49). Nizard et al. (38)
compared patients who underwent knee replacement after HTO with a
matched group of patients undergoing primary knee replacement. More
pain was reported in those who had a previous HTO. Functional scores
were similar. Patella baja, lateral soft-tissue scarring, and abnormal
proximal tibia anatomy have all been problems in arthroplasty patients
who have had an HTO (35,38,49). These results must be considered when advising patients who are considering tibial osteotomy.
stabilizing the osteotomy have been proposed. The dome osteotomy,
attempts to allow correction with minimal bone loss, and maintenance of
tibial length (29,31,).
Forming the hemispherical osteotomy can be technically difficult. More
extensive exposure of the tibia is needed, and the resulting bone
segments can be less stable because all cortices are involved in the
osteotomy.
apex of the wedge proximal and medial, and the lateral segment more
distal (23,34). This
technique leaves more bone in the proximal segment. The proximal
tibiofibular joint is not exposed, and a fibular osteotomy is required
to allow compression of the tibial osteotomy.
the opening wedge medial osteotomy with the addition of a specialized
fixation plate. The defect created is filled with illiac crest bone
graft. The osteotomy is then held with a specially designed bone plate.
Early results are encouraging. This technique is bone conserving but
may place greater loads on the proximal fragment because the bone graft
acts like a wedge under the proximal plateau segment.
-
Apply the fixator pins medially with two
cancellous threaded pins in a transverse array proximally and two
bicortical pins distally. -
Then perform a medial corticotomy 4 to 5
cm below the tibial plateau without violating the lateral cortex. Apply
the fixator and hold the corticotomy closed for 10 days until early
callus has formed. -
At 10 days, start distraction at 1 mm a
day until the desired correction is obtained. Then lock the frame for 3
to 4 weeks until consolidation occurs. When the lengthening site is
stable, unlock the frame to allow compression across the osteotomy site
and advance weight bearing. Remove the frame 12 to 14 weeks after
application.
extensor mechanism seen with traditional methods of osteotomy fixation.
Also, all implants are removed at the completion of treatment. This
method may compromise future arthroplasty by introducing bacteria to
the bone adjacent to the pins (37). Initial reports of knee replacement after use of the Orthofix fixator have not included any joint infections (10,30).
This technique requires close attention to detail and a cooperative
patient. Complications include pin track infection, loss of position,
delayed consolidation, and nonunions. These can be difficult to treat.
also had limited success with this method. Patients did well
clinically; however, technical considerations made the surgery less
than satisfactory. An excessively large wedge of bone was required for
correction beyond 12°. Also, the joint line remained in valgus,
potentially complicating future procedures. Supracondylar femoral
osteotomy was recommended for correction of larger deformities.
affecting the lateral compartment predominately. The defect is not in
the tibial plateau but is caused by hypoplasia of the lateral femoral
condyle. Preoperative planning for the supracondylar osteotomy is
similar to the tibial osteotomy. Use standing long-leg films of the
lower extremities to calculate the degree of valgus deformity. Plan
correction to obtain neutral anatomic alignment, although the ideal
degree of correction is not well established (32). Both Coventry (8)and Morrey and Edgerton (36)
recommend fabrication of a triangular metal plate, with the two long
sides reproducing the desired angle of correction as calculated from
preoperative films (Fig. 107.5A). Sterilize the
triangular plate and use it as a template at the time of surgery. Use a
95° blade plate to hold the osteotomy. Staples are not adequate (8,36). The angle of the template must be increased by 5° if a 95° blade plate is to be used.
 |
|
Figure 107.5. A:
Distal femoral osteotomy by the medial approach. The degree of valgus alignment (X) is calculated from standing long-leg films. Place Steinmann pins in the sequence outlined in the text. The wedge osteotomy is represented by the shaded segment. Undercutting the angle allows impaction of the proximal segment into the distal segment. B: Apply the blade plate medially. |
The femoral vessels must be protected if the medial approach is
selected. An anterior skin incision can be used; however, most authors
prefer to approach the operated side directly. The medial approach with
slight variation, has been described by Morrey and Edgerton (36) and by Healy et al. (17) (see also Chapter 3).
-
Make a medial longitudinal skin incision
10 cm in length or longer, if needed. Reflect the vastus medialis
muscle anteriorly. Expose the femoral cortex from the insertion of the
joint capsule to a point sufficiently proximal to accommodate the side
plate. -
Under fluoroscopic guidance, drill a guide pin for the blade plate chisel across the femur 2.5 cm proximal to the condyles (107.5A,1).
Direct the pin at a gentle angle from anterior to posterior to keep it
centered within the condyles. Place a second, proximal Steinmann pin
perpendicular to the femoral shaft proximal to the osteotomy site (107.5A,2). Use a third pin to reproduce the desired angle of correction in relation to the perpendicular, proximal pin (Fig. 107.5A,4).
Place this pin between the first two pins. The prefabricated angle
template can help with proper placement of this pin. It is important to
prepare for easy blade plate placement by seating the chisel fully into
the condyles before the actual osteotomies are performed. -
Perform the osteotomy with an oscillating
saw. Keep the distal side of the osteotomy proximal to the adductor
tubercle. Guide the transverse, proximal cut by visually referencing
the pin placed perpendicular to the femoral shaft. A fourth pin may be
placed coincident with the proximal osteotomy line to act as a guide
for the saw (107.5A,3). The angle of the wedge
should be kept slightly less than the desired angle of correction. The
proximal segment can be impacted into the distal segment to obtain the
desired correction. Converge the two osteotomies to a point several
millimeters medial to the lateral cortex. -
Before completing the osteotomy,
P.2866
seat the blade plate in the distal fragment. Take care to align the
blade plate along the posterior femoral cortex. Use a varus force to
close the osteotomy site. The side plate can be used as a lever to
assist in closing the osteotomy. An osteotome may be used to perforate
the lateral cortex, if needed. Undercutting the angle of the osteotomy
allows impaction of the proximal segment into the metaphyseal bone
until the desired angle is achieved. After the osteotomy is closed, the
blade plate can be further impacted into the distal femoral condyles (107.5B). -
Use three to four bicortical screws to
fix the plate to the proximal segment; place one cancellous screw
through the plate into the distal segment. -
The lateral approach follows a similar
sequence. Make an anterior or direct lateral incision. Use the
prefabricated angle template to direct the tip of the blade into the
distal femur (Fig. 107.6A). Make the osteotomy
perpendicular to the shaft, above the adductor tubercle. Seat the
blade. As the plate contacts the cortex of the lateral shaft, the
proximal segment is impacted onto the distal segment and the correction
is obtained (Fig. 107.6B).![]() Figure 107.6. A:
Figure 107.6. A:
Distal femoral osteotomy by the lateral approach. Insert the tip of the
blade into the distal segment, with the plate parallel to the desired
final alignment line. Place the prefabricated angle template between
the plate and femoral shaft to ensure that the blade is directed at the
proper angle. Perform the osteotomy above the adductor tubercle. B:
Impact the proximal segment into the distal segment because the blade
is seated. The plate comes to rest against the cortex shaft.
 |
|
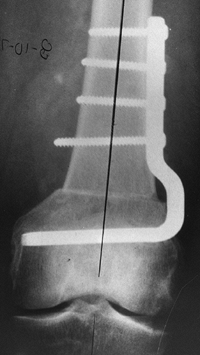
Figure 107.7. Radiograph of healed supracondylar osteotomy.
|
Avoid nonunion by ensuring that the osteotomy is rigidly fixed with
good impaction of the bone fragments. If residual motion is evident
after fixation, consider additional fixation such as an anteroposterior
interfragmentary screw or a smaller supplementary plate. Avoid
stiffness of the knee by early motion, supervised, if necessary, by a
therapist to be certain that the patient regains motion.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
Y, Masuhara K, Shiomi S. The Effect of High Tibial Osteotomy on
Osteoarthritis of the Knee. An Arthroscopic Study of 54 Knee Joints. Orthop Clin North Am 1979;210:585.
AA, Wyatt RWB, Beck SW. High Tibial Osteotomy: Use of an Osteotomy Jig,
Rigid Fixation, and Early Motion Versus Conventional Surgical Technique
and Cast Immobilization. Clin Orthop 1989;271:212.
DL, James SL, James RL, Slocum DB. Proximal Tibial Osteotomy in
Patients Who are Fifty Years Old or Less: A Long-term Follow-up Study. J Bone Joint Surg [Am] 1988;70:977.
HA, Sigholm G, Redfern FC, et al. The Effect of Simulated
Fracture-angulation of the Tibia on Cartilage Pressures in the Knee
Joint. J Bone Joint Surg [Am] 1991;73:1382.
MA, Alexander N, Krackow KA, Hungerford DS. Total Knee Arthroplasty
After Failed Proximal Tibial Osteotomy for Osteoarthritis. Orthop Clin North Am 1994;25:515.
RS, Cardinne L, Bizot P, Witovet J. Total Knee Replacement after Failed
Tibial Osteotomy: Results of a Matched-pair Study. J Arthroplasty 1998;13:857.
D, Tetsworth K. Mechanical Axis Deviation of the Lower Limbs.
Preoperative Planning of Uniapical Angular Deformities of the Tibia or
Femur. Clin Orthop 1992;280:48.
Paper presented at the annual meeting of the American Academy of
Orthopaedic Surgery, Specialty Day—The American Orthopaedic Society for
Sports Medicine, Anaheim, February 1999.