Distal Biceps Tendon Rupture
surgeons now see distal biceps tendon rupture with increasing
frequency. Since the first edition, increased concern about ectopic
bone and a growing interest in suture anchors has emerged. An early
diagnosis is important, since the prognosis with early reattachment is
excellent.
distal biceps tendon should be reattached to the radial tuberosity as
soon as possible (1,2,11,12,13).
The average age of patients is approximately 55, and virtually every
report in the literature has been of a male. In our practice at Mayo we
have treated two females from among 70 with this diagnosis, both with
partial ruptures. Usually the patient is involved with heavy labor or
activity, which further emphasizes the need of early definitive
treatment.
The advantage of the anterior Henry approach is that it is less likely
to create ectopic bone. The disadvantage is that it puts the radial
nerve at jeopardy (6,11,13).
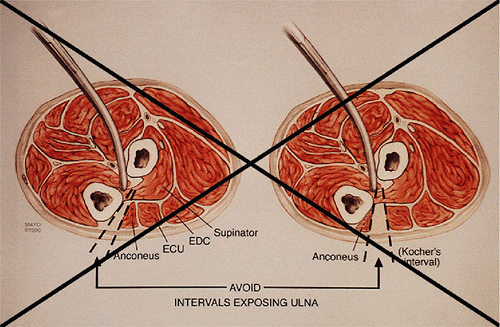
that described by Boyd and Anderson. The advantage of the two-incision
technique is that it lessens and virtually eliminates the likelihood of
injury to the radial nerve (12). The original Boyd-Anderson approach exposes the ulna, and hence can be associated with ectopic bone (7). Through the years we have employed the Mayo modification of the Boyd-Anderson approach, which does not expose the ulna and hence is associated with very little ectopic bone (9).
retracts. If this has occurred, reattachment or embedding the biceps
tendon into the brachialis is easy but rarely acceptable today.
have significant functional impairment. This might be seen in a
sedentary patient, but rarely does such an individual sustain this
injury. An attempt to reattach this tendon if there has been a delay of
more than 3 weeks requires careful thought, as the tendon typically is
retracted into the biceps muscle and is not of adequate length to reach
the radial tuberosity (12). Furthermore, the
tract of the tendon to the tuberosity will have scarred and become
obliterated, making the surgery much more difficult.
 |
|
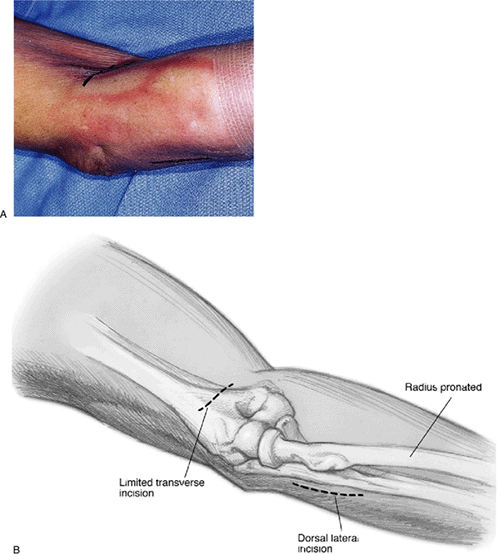
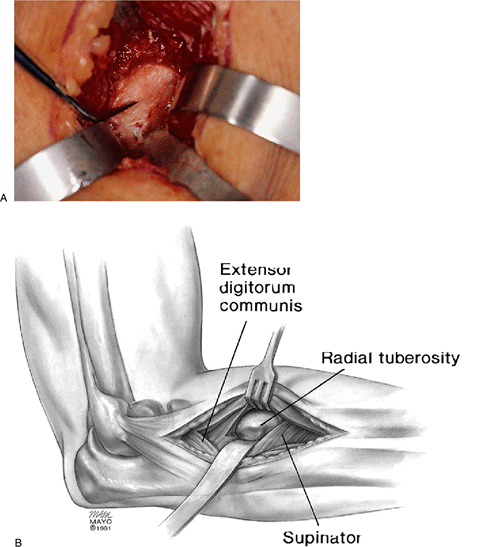
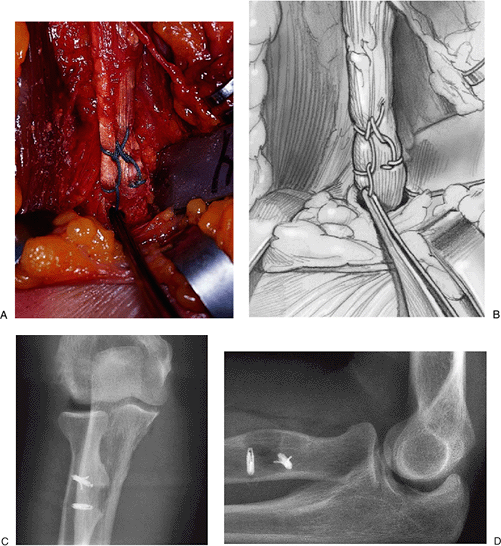
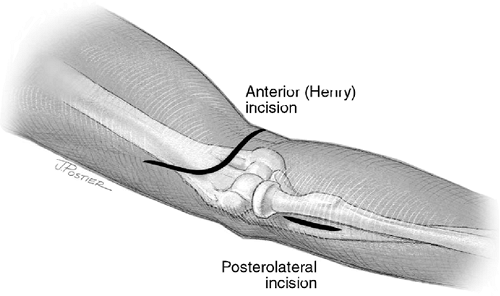
Figure 10-1. A,B:
The two-incision technique employs a simple 4-cm transverse incision in the antecubital space and a 5- to 7-cm incision over the posterior aspect of the proximal forearm. |
and typically is referred to those with experience with this procedure.
The author prefers the achilles allograft for this procedure as
described herein.
occurred, be prepared to perform a more detailed dissection in the
antecubital space. If the tendon has retracted, restoration of length
with an achilles allograft is preferred. The patient must be prepared
for these eventualities.
sandbag may be placed under the shoulder to allow the arm to be brought
across the chest comfortably. Under a general anesthesia, a single 4-cm
transverse incision in the antecubital crease is employed (Fig. 10-1).
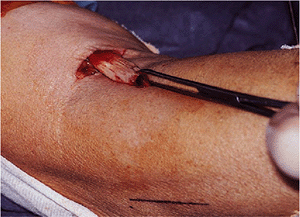
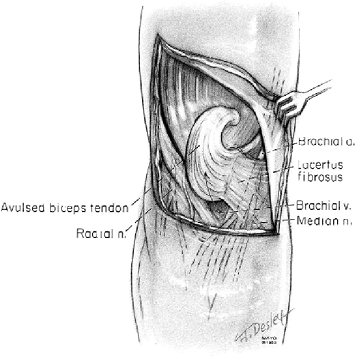
is identified, dissected free of soft tissue, and delivered from the
wound (Fig. 10-2). The end of the tendon tends
to be bulbous and is trimmed to allow it to fit well into the
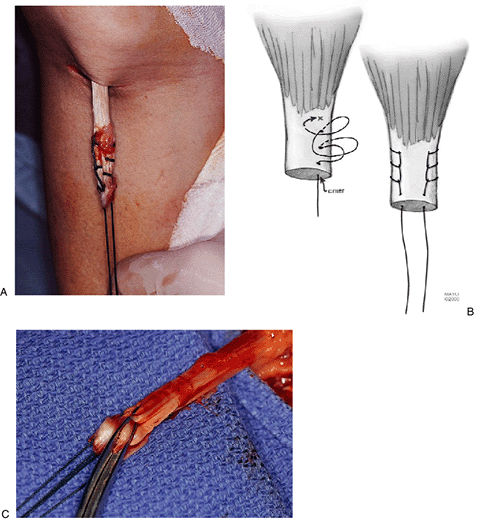
tuberosity. After the tendon has been trimmed, two No. 5 Mersilene
sutures are placed through the torn portion entering the end of the
tendon. A crisscrossed (Bunnell) suture or locking stitch (Krakow) is
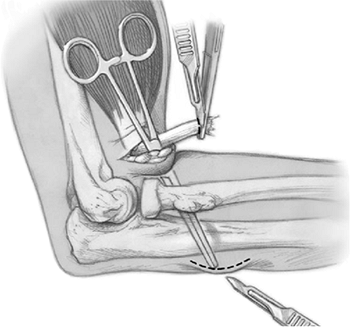
employed (Fig. 10-3). A curved clamp is then introduced into the tunnel previously occupied by the biceps tendon (Fig. 10-4).
It is directed by palpation to and then past the tuberosity between the
radius and ulna. Rotation of the forearm confirms proper position of
the instrument on the ulnar side of the radius. The curved hemostat is
advanced until it punctures the muscle and subcutaneous tissues of the
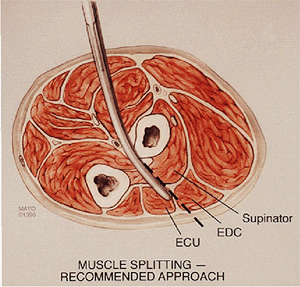
dorsal aspect of the forearm (Fig. 10-4). An incision is then made over the site of prominence splitting the common extensor and supinator muscles (Fig. 10-5). With full forearm pronation the tuberosity is identified and cleaned of soft tissue.
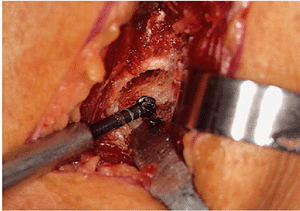
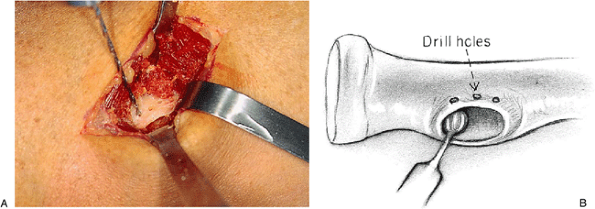
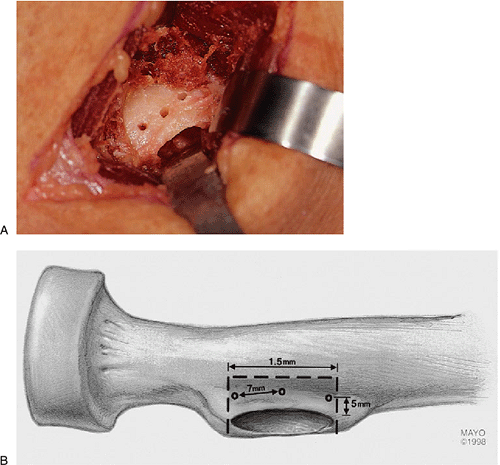
After an adequate orifice 10 to 12 mm з 7 to 8 mm has been made to
receive the tendon, three drill holes are placed on the radial side of
the tuberosity (Fig. 10-7). This is simplified
by allowing the forearm to supinate slightly to bring this margin of
the radial tuberosity into better alignment. The
holes should be placed in such a way as to leave sufficient bone to avoid osseous rupture or pullout of the sutures (Fig. 10-8).
 |
|
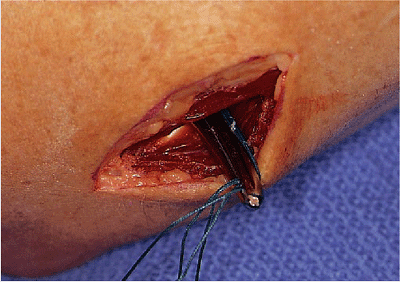
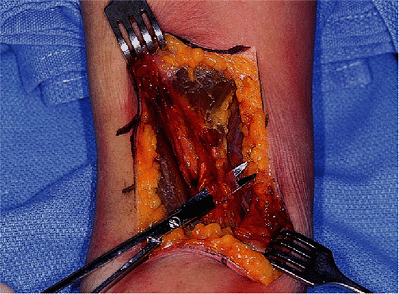
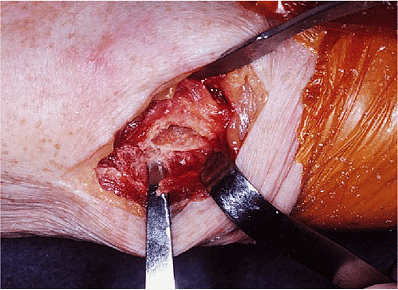
Figure 10-2.
The tendon is identified by digital palpation and delivered through the skin incision, revealing a bulbous degenerative process at the site of disruption. |
 |
|
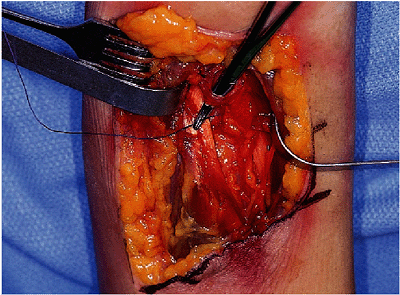
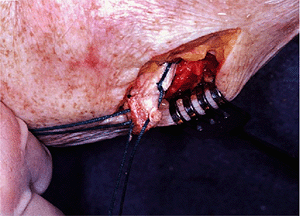
Figure 10-3. A–C: Two No. 5 nonabsorbable sutures are inserted by the crisscross Bunnell or Krachow locking technique.
|
 |
|
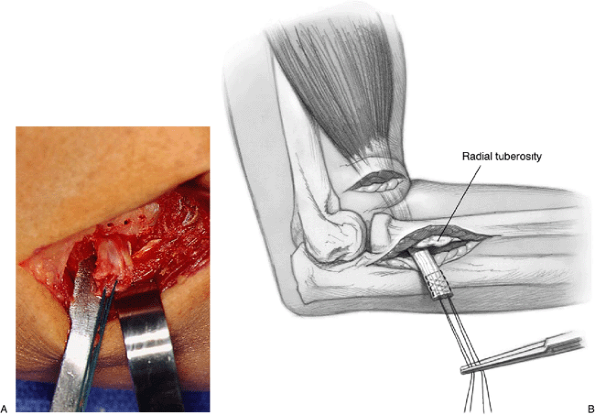
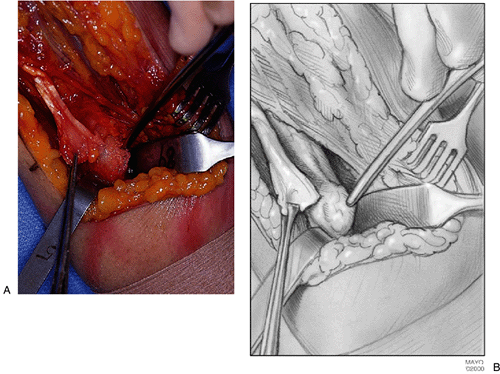
Figure 10-4.
The curved hemostat is passed between the radial tuberosity and the ulna to emerge through the common extensor muscle mass and tent the skin on the proximal posterolateral aspect of the forearm. |
 |
|
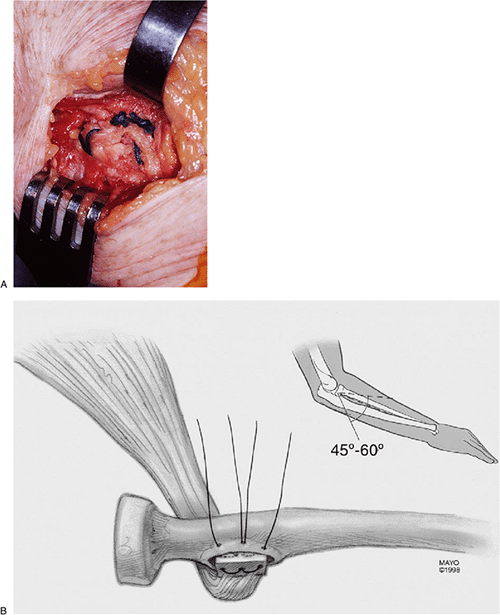
Figure 10-5. A,B: An incision is made over this prominence, the muscle is split, the forearm is fully pronated, and the tuberosity is exposed.
|
 |
|
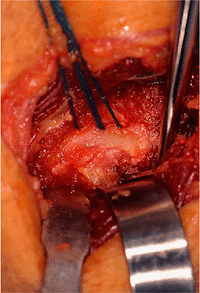
Figure 10-6. The greater tuberosity is excavated with a high-speed bur in such a way as to receive the distal biceps tendon.
|
 |
|
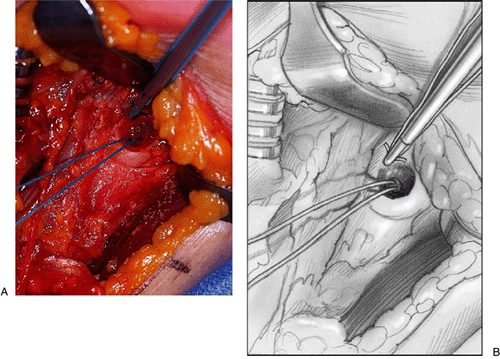
Figure 10-7. A,B: Three holes are drilled in the radial aspect of the tuberosity.
|
incision and the sutures are grasped by the curved hemostat. The
instrument is again directed through the tunnel and out the second
incision (Fig. 10-9). The tendon is then brought through the tunnel from the antecubital space and drawn past the ulnar side of the tuberosity (Fig. 10-10).
The sutures are threaded into each of the holes at the margin of the
tuberosity. One suture is brought into the proximal and one into the
center hole. The second
suture is brought through the common middle hole and its other end through the distal hole (Fig. 10-11).
The biceps tendon is threaded into the tuberosity; once again this is
facilitated by slightly supinating the forearm. With the arm remaining
in less than full pronation, the sutures are tied (Fig. 10-12).
 |
|
Figure 10-8. A,B: Care is taken to provide sufficient space between the holes to provide secure fixation in bone.
|
 |
|
Figure 10-9.
The sutures are grasped again with a curved hemostat and introduced through the tunnel of the biceps tendon to emerge through the forearm incision. |
 |
|
Figure 10-10. A,B: The tendon is then pulled through the forearm wound.
|
 |
|
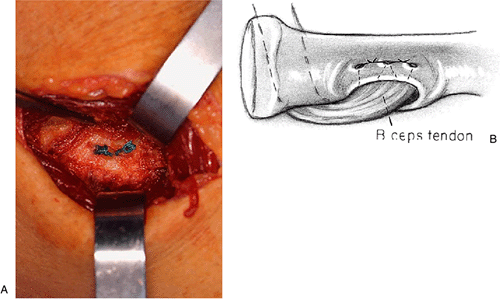
Figure 10-11.
The distal aspect of the biceps tendon is threaded into the excavated portion of the radial tuberosity. The sutures are brought through the three holes, with the center hole used for one arm of each of the sutures. |
 |
|
Figure 10-12. A,B: The sutures are tied while the forearm is allowed to supinate slightly to facilitate this process.
|
that there is no impingement with the ulna. Extension is assessed to
ensure that excessive shortening has not occurred. The incisions are
then closed in a routine fashion. At the proximal forearm the fascia
over the split muscle is closed with a 2-0 absorbable suture, and a
subcutaneous and skin suture of choice is used. In the antecubital
space the tissues are allowed to resume their former position, a drain
is left in the antecubital space, and the remainder of the wound is
closed in layers as desired.
 |
|
Figure 10-13. A Henry anterior exposure identifies the tendon and lacertus fibrosis.
|
 |
|
Figure 10-14.
The radial nerve is identified emerging from the interval between the brachial radialis and lateral aspect of the biceps (above retractor). The recurrent radial artery is identified and ligated. |
 |
|
Figure 10-15. A,B: The tuberosity is exposed.
|
 |
|
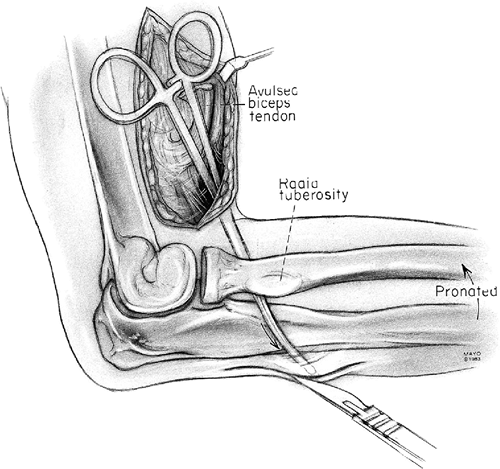
Figure 10-16. A,B: The tuberosity is excavated and two suture anchors are embedded in the tuberosity.
|
threaded proximally while the tendon is being teased distally into the
prepared tuberosity bed (Fig. 10-17). The sutures are tied with the forearm in neutral rotation.
 |
|
Figure 10-17. A crisscross or Krachow stitch is used to secure the tendon, which is then advanced into the tuberosity (A,B) as demonstrated radiographically (C,D).
|
cannot be reattached directly to the tuberosity, augmentation with an
Achilles tendon allograft is our technique of choice.
as described earlier (Fig. 10-21).
The calcaneal portion of the Achilles allograft composite is carefully
trimmed sufficiently small to allow insertion into the tuberosity but
taking care to maintain the tendon insertion to the calcaneus fleck of
bone (Fig. 10-22). A No. 5 nonabsorbable suture
is placed in the allograft tendon through holes in the small piece of
calcaneus using a Krakow stitch. The tendon is then threaded from the
anterior exposure into the forearm incision (Fig. 10-23). This is inserted into the tuberosity and secured through the holes in the tuberosity (Fig. 10-24).
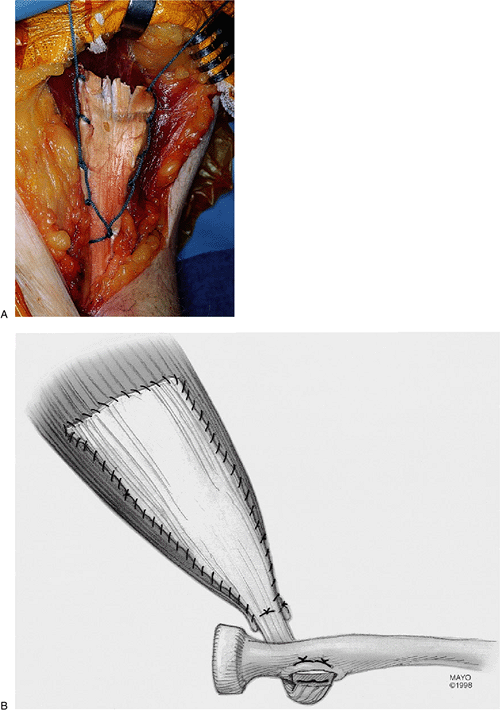
With the elbow at about 45 degrees of flexion the Achilles fascia is
then secured around its margin to the biceps muscle, which has been
retracted distally as much as possible to develop appropriate resting
tension (Fig. 10-25).
 |
|
Figure 10-18.
The two-incision technique is used and employs a Henry-type incision in the antecubital space and a 4-cm incision over the posterolateral aspect of the proximal forearm. The anterior incision is extended as needed to expose the biceps muscle. |
 |
|
Figure 10-19. The tendon usually has recoiled and is of variable length, but the biceps stump is adequate to secure to the tendon allograft.
|
 |
|
Figure 10-20.
The curved hemostat is passed between the radial tuberosity and the ulna to emerge through the common extensor muscle mass and tent the skin on the proximal posterolateral aspect of the forearm. |
 |
|
Figure 10-21. The exposure and preparation of the tuberosity are as described earlier.
|
 |
|
Figure 10-22.
The graft is prepared so the calcaneal attachment is intact and sufficiently small to fit into the prepared cavity in the tuberosity. |
 |
|
Figure 10-23. The stitch passes through a hole in the calcaneus and a Krachow stitch is used to secure the tendon.
|
 |
|
Figure 10-24. A,B:
The fleck of bone is inserted into the tuberosity and secured with sutures placed through the margin of the tuberosity as above. |
 |
|
Figure 10-25. A,B: With the elbow at about 60 degrees of flexion, the biceps is “enveloped” with the Achilles fascia.
|
elbow in 90 degrees of flexion and the forearm in neutral rotation.
This is kept in place for 3 to 7 days.
gentle passive flexion is allowed. Active extension to 30 degrees is
allowed and encouraged from the first week after surgery. Full
extension is allowed as tolerated and generally attained by the third
week. Four weeks after surgery the patient is allowed to flex and
extend against gravity as able. At 6 weeks a gentle
flexion-strengthening program is allowed, starting with 1-kg weights.
Activity as tolerated is permitted at 3 months. Full activity without
restriction is allowed 6 months after surgery.
used. The patient is placed in a CPM and protected for 3 weeks. Passive
assisted motion is begun at 3 weeks and continued to 6 weeks. Full
extension is avoided until the sixth week. Active motion for activities
of daily living is allowed at 6 to 12 weeks. Activity as tolerated
progresses from the third to the sixth month.
reattachment of the tendon are very good. Studies have shown virtually
100% improvement for restoration of flexion and supination strength (1,2,8,11,12).
Loss of motion is not seen, and we have observed only one rerupture
after an acute repair. Although popular, the clinical experience with
suture anchors is limited. To date, 23 cases report no problem from
several combined sources (5,10,14,15,16). Laboratory studies, however, not yet reported in the literature, reveal a statistically significant (p < .01) greater initial strength with the transosseous holes than suture anchor.
 |
|
Figure 10-26.
Ectopic bone bridging the proximal ulna and radius. The exposure of the radial tuberosity was across the periosteal surface of the ulna. |
 |
|
Figure 10-27. The forearm incision should not be through Kocher’s interval or otherwise expose the periosteal surface of the proximal ulna.
|
procedure. Radial nerve injury has been reported and may be seen as
often as 5% of the time after distal biceps tendon reattachment through
anterior modified Henry approach (4,8). Ectopic bone is a recognized complication of the two-incision technique and bridges the proximal radius and ulna (Fig. 10-26). This, however, can be minimized or avoided by not exposing the periosteal surface of the ulna with the forearm incision (Fig. 10-27) and by splitting the muscle fibers as the tuberosity is exposed (Fig. 10-28)(6).
 |
|
Figure 10-28. The forearm incision is a muscle-splitting approach.
|
 |
|
Figure 10-29.
Removal of the ectopic bone restores functional forearm rotation in most patients. In this instance the tendon insertion was involved and required reattachment. |
After at least 6 months or when the radiograph demonstrates maturity,
the osseous bar may be resected. The exposure is generally through the
previously used forearm incision. Care should be taken during the
exposure to avoid excessive retraction on the supinator muscle, which
may injure the posterior interosseous nerve. Occasionally, the
reattached biceps tendon itself is involved in the ectopic bone. In
this instance the tendon may be released during the ectopic bone
removal (Fig. 10-29) and is then reattached at the end of the excision.
reported by Kelly et al. Overall the satisfactory rate was over 90%.
One rerupture occurred in a patient requiring wheelchair transfer. No
synostosis occurred after 74 Mayo modified two-incision approaches. Of
note is that the rate of complication doubles (p < .05) if a delay of more than 21 days occurs before surgery (9).
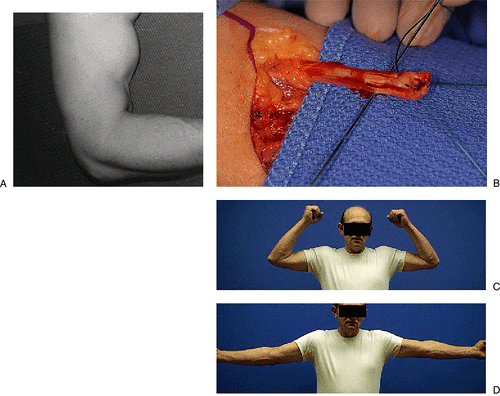
flexed elbow while trying to lift a freezer. He presented with obvious
retraction of the distal aspect of the right dominant biceps muscle as
he attempted to flex the arm (Fig. 10-30A).
After discussion of the risks and benefits, a surgical procedure was
undertaken and the biceps was found to have been avulsed from the
radial tuberosity (Fig. 10-30B). The double
Bunnell suture technique into the tuberosity through two incisions was
carried out. Three weeks after the surgical procedure described
earlier, he was placed in a flexion assist brace. At 6 months the
patient had normal flexion (Fig. 10-30C) and extension (Fig. 10-30D). At 1 year his flexion and supination strength returned to normal.
 |
|
Figure 10-30. A: Proximal retraction of a ruptured distal biceps during resisted elbow flexion. B:
The tendon is identified. The bulbous portion of the distal biceps has been trimmed, and nonabsorbable crisscross sutures have been placed. Six months after the procedure the patient has full range of flexion (C) and extension (D). His strength has returned to normal. |
F, Gelpke H, Hotz T, et al. Distal biceps tendon ruptures—experiences
with soft tissue preserving reinsertion by bone anchors. Swiss Surg 1999;5:186–190.
JM, Amadio PC, Morrey BF, et al. Proximal radioulnar synostosis after
repair of distal biceps brachii rupture by the two-incision technique:
report of four cases. Clin Orthop 1990;Apr(253):133.
BF, Askew LJ, An KN, et al. Rupture of the distal biceps tendon:
biomechanical assessment of different treatment options. J Bone Joint Surg 1985;67A:418.
RJ, Michelson H, Rosenwasser MP. Repair of rupture of the distal tendon
of the biceps brachii. Review of the literature and report of three
cases treated with a single anterior incision and suture anchors. Am J Orthop 1997;26:151–156.
