Total Elbow Arthroplasty for Rheumatoid Arthritis
IV – Elbow Reconstruction > Part C – Operative Treatment Methods
> 59 – Total Elbow Arthroplasty for Rheumatoid Arthritis
inflammatory disorder in which the body’s immune system mistakes
articular cartilage for foreign (nonself) material. The exact cause for
RA is unknown. Genetic susceptibility is recognized, including
monozygotic HLA DR4, which has a 12% to 15% concordance rate. Women,
especially postpartum and those breastfeeding, have an increased risk
along with smokers.
are affected with rheumatoid arthritis, or approximately 1 per 300,000.
It is generally believed that the ratio of women to men is between 2 to
1 and 3 to 1. It is rare in men younger than the age of 45 years; in
this age group, the condition is predominately among women (6 to 1).
The peak incidence is between the ages of 20 and 50 years, but it can
affect both the young and the elderly. Its prevalence is lowered among
black African and Chinese and among certain Indian tribes. It most
commonly affects adults as a polyarticular disease where
extra-articular features are uncommon.
-
Synovitis—The
synovial lining of the joint is congested and at times villous.
Subsynovial infiltrates of lymphocytes and plasma cells are present.
The effusion is cellular, and the capsule is thickened. -
Joint destruction—Within
the first 2 years, proteolytic enzymes and direct invasion of the
pannus of granulation tissue destroys the articular surface. The joint
margins are eroded by the same process. Tendon sheaves develop
tenosynovitis, and this process causes invasion of the collagen bundles. -
Deformity—Over
time, joint destruction capitula thickening and distension along with
tendon rupture leads to progressive instability and deformity.
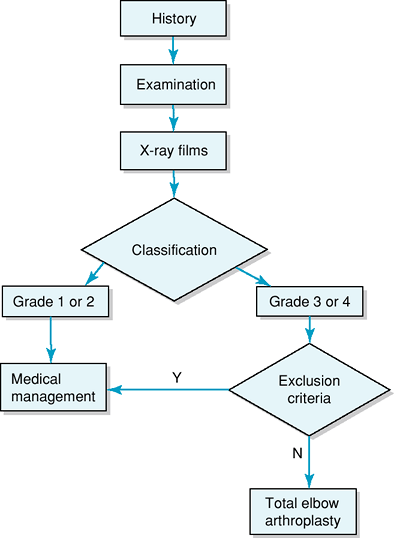
This classification system is based on both the pathologic changes and
the changing x-ray film appearances. This classification system can be
used to guide the orthopaedist with regard to treatment options.
seven revised American Rheumatism Association (ARA) criteria in the
last 6 months.
history to focus on pain, associated stiffness, and/or instability. One
should inquire about neurologic symptoms, especially that of the ulnar
nerve, remembering that approximately 40% of rheumatoid arthritic
patients with elbow pathology have either clinical or subclinical
peripheral neuropathy or nerve compressions. Previous surgery to the
elbow (radial head excision or replacement and/or interposition) has
prognostic implications. A more general view of the patient including
the joints above and below the elbow and cervical spine in mode and
abilities and ambulation is important. The overall functional capacity,
e.g., the ARA classification, may also be useful.
|
TABLE 59-1 Classification of Rheumatoid Arthritis of the Elbow
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
-
The integument—the
skin, especially posteriorly where the incision will be made. The
muscles, the flexors of the elbow: What are their strengths, and what
is their condition? Neurovascular considerations, particularly to the
course of the ulnar nerve and its behavior in flexion. -
The joint—the
range of motion and both flexion and extension along with
pronation/supination; its stability in reference to whether the joint
is enlocated or whether it remains subluxed or flail. -
The patient—particular
reference to the joints above and below (wrist and shoulder), the
cervical spine, and the patient’s general ambulatory ability and if the
affected elbow is used in ambulation in any way (cane, crutch, or
wheelchair).
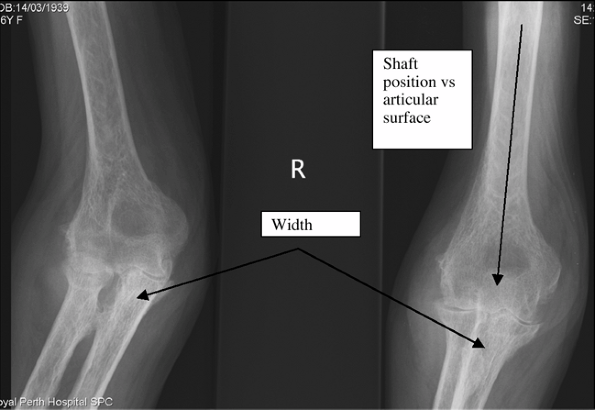
specifically, one should examine the plain x-ray films to determine
surgical requirements. Canal capacity length and alignment relative to
the articulate surfaces are important. Any bone thinning, particularly
cortical bone thinning, especially at points of entry of the prosthesis
or at the tips of potential prosthetic replacement, needs to be noted (Fig. 59-1).
|
TABLE 59-2 Severity of Rheumatoid Arthritis Of the Elbow
|
||
|---|---|---|
|
 |
|
Figure 59-1 Diagnostic workup algorithm.
|
surgical goal is the relief of pain. Total elbow arthroplasty for
rheumatoid arthritis should be considered in patients with grade 3 or 4
disease. The contraindications are bone or joint infection or an open
wound about the elbow. Relative contraindications include the medical
state of the patient specifically with regard to Parkinsonian or other
neurologic disorders, particularly if the patient has a history of
recurrent falls. The possibility that anaesthesia will place the
patient at unnecessary risk must also be considered. The other relative
risk is bone ankyloses. The technical demands of joint replacement at
the elbow are such that the general orthopaedist should refer to those
surgeons with high-volume experience in total elbow arthroplasty.
unconstrained and semiconstrained joint replacements are currently
available. Traditionally, unconstrained joint replacement (with which
there is no direct linkage between the humeral and ulnar components)
has been considered for those patients with grade 3 disease where there
is still primary ligamentous stability. Semiconstrained implants have a
loose linkage between the humeral and ulnar components, allowing
approximately 7 to 10 degrees of toggle at the articulation but at the
same time maintaining the articulation’s
stability. This type of prosthesis is the most commonly used and may be considered for both grade 3 and grade 4 patients.
 |
|
Figure 59-2 Anteroposterior radiograph of an elbow with rheumatoid arthritis.
|
history and examination, the orthopaedist having satisfied himself or
herself that the patient is a surgical candidate and has no
contraindications. The examination can specifically review those
aspects important for the joint replacement itself—soft tissue coverage
and the quality of the integument: There must be at least one flexor of
antigravity power and preferably an extensor of similar power both for
extension and to cover the prosthesis. Bone deficiency is covered both
clinically and on the radiographs; the minimum requirement for a
semiconstrained prosthesis is two tubes of bone (the humeral canal, the
ulnar canal, and a grade 4 flexor). These are the minimum requirements
for undertaking elbow replacement arthroplasty.
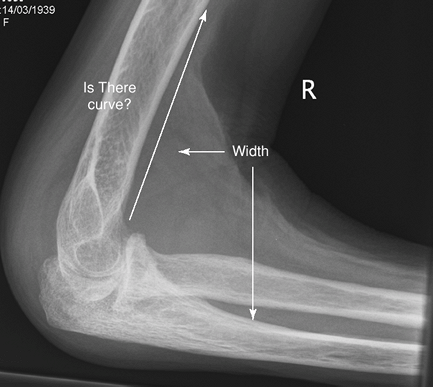
clinic appointment, focuses the orthopaedist on any technical
difficulties of implantation of the preferred implant. The size, the
position of the humeral and ulnar cuts, and the relationship of the
intramedullary canals to the articular surface are brought to the
orthopedist’s attention. Also of note is the curvature of the humerus
on lateral view and therefore its relationship to the prosthesis being
used and the narrowing on lateral view of the ulna beyond to the
olecranon with specific reference to the stem of the prosthesis to be
used (Figs. 59-2 and 59-3).
replacement arthroplasty is covered in other chapters. Important steps
to be focused on include the following:
-
Exposure
-
Ulnar nerve identification and transposition
-
Dislocation
-
Release of anterior humerus
-
Accurate identification of the canals
-
Bone cuts as per manufacturer requirements
-
Trial components; Ensure soft tissue releases for balance of prosthesis
-
Cement prosthesis (sequentially is recommended)
-
Rearticulation
minor and permit easy recovery. Intraoperative bone fracture, either
that of the condyles or perforation of the canals, can occur without
careful preoperative planning. If there is canal perforation, more
distant neurovascular structures such as the radial or median nerve are
at risk. Early complications include wound-healing difficulties,
bleeding, and joint stiffness. Temporary paresthesia, particularly of
the ulnar nerve, is also recognized. Late complications that have been
recognized and should be considered are loosening of the implant’s
bushing in those implants using bushings, triceps failure, and
component fracture. Infection of total elbow arthroplasty in rheumatoid
patients is said to be approximately 2%, which is slightly higher than
that of standard lower extremity (hip and knee) joint replacement.
 |
|
Figure 59-3 Lateral radiograph of an elbow with rheumatoid arthritis.
|
patients with rheumatoid arthritis is a 100-degree arc motion generally
from approximately 30 degrees of fixed flexion to 130 degrees of
flexion. The patient should expect excellent relief of pain, which
provides a high degree of satisfaction. When scored by a common elbow
evaluation rating at 10 years, 85% of patients will have a good or
excellent result. The survivor rate is approximately 92% at 10 years
for this group of patients.
commercial or plaster of Paris splint until the following day. This
achieves a decrease in elbow joint volume and therefore reduces
swelling. Thermal regulation that caused the joint may also be used to
reduce the initial swelling. Typically, once the dressings are removed,
simple dressings are applied to the wound, a compressive long arm
stocking is applied, and unrestricted elbow motion can be commenced.
Discharge of the patient from the hospital is dependent on overall
recovery as semiconstrained implants are stable from the beginning and
no specific postoperative splinting is required. If an unconstrained
implant is chosen, the manufacturer’s specific recommendations must be
followed regarding postoperative splinting and protection.
arthritis requires specific restrictions in use of the limb and can be
summarized as follows: no more than 5 kg repeated lifting and no more
than 10 kg in a single event.
DRJ, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients
who have rheumatoid arthritis. A ten to fifteen-year follow-up study. J Bone Joint Surg Am. 1998;80:1327.
D, Claydon P, Stanley D. Total elbow replacement using the Kudo
prosthesis. Clinical and radiological review with five- to seven-year
follow-up. J Bone Joint Surg Br. 2003;85:354.
J, O’Driscoll S, Morrey BF. Periprosthetic humeral fractures after
total elbow arthroplasty: treatment with implant revision and strut
allograft augmentation. J Bone Joint Surg Am. 2002;84:1642.
