Total Knee Arthroplasty
for relieving arthritic knee pain and for improving function. However,
it is a technically demanding procedure and the long-term success is
dependent on the way the prosthesis is implanted. In this chapter
important variables that are associated with achieving optimal results
are presented. These include factors related to patient selection,
preoperative planning, surgical technique and postoperative management.
relief of chronic disabling knee pain owing to arthritis that has
failed to respond to nonsurgical treatment regimens. In the United
States >90% of the patients who undergo total knee arthroplasty
(TKA) have osteoarthritis (OA), with the other main causes including
rheumatoid arthritis and posttraumatic arthritis. Risk factors for the
development of OA include age, body weight, gender, family history of
disease, and prior injuries including meniscectomy and cruciate
ligament tears. The increased risk in each of these groups is likely
multifactorial with both mechanical and chemically mediated components.
The composition of both hyaline cartilage and synovial fluid changes
with age in both men and women, but women have higher rates of knee OA
and therefore, the role of gonadal hormone levels has been debated. A
genetic component has also been implicated, although it is likely that
many genes contribute to this risk. Genetic differences in cartilage
and subchondral bone constituents appear to be involved in this
process, and research is ongoing to identify important markers.
Patients with a high body mass index are also at increased risk for the
development of OA, and this risk may be owing to factors beyond the
simple mechanical trauma produced by the elevated joint forces. Clearly
some or all of these risk factors may be identified in any individual,
and therefore the relative contribution of each is hard to determine.
that approximately 10% to 20% of adult patients older than 35 years of
age experience chronic knee pain. Among this group of patients, the
prevalence of radiographically identifiable OA has been reported to be
between 1% and 70%, depending on the age subgroup, but most studies
have suggested a rate of between 1% and 15%. In the United States
Medicare population, between 30 and 70 people per 10,000, depending on
gender and age subgroup, underwent primary TKA in 2000, with the
highest rate of 67.9 per 10,000 noted in women between the ages of 75
and 79 years. During this time period, >350,000 primary TKAs were
performed annually in the United States.
exacerbated by weight-bearing activity and relieved by rest. Pain may
be isolated to one area of the knee in unicompartmental arthritis or
diffuse when multiple compartments are involved. Anterior knee pain
that is aggravated by stairs or arising from a sitting position is
suggestive of patellofemoral involvement. Secondary symptoms include
varying degrees of swelling, buckling or giving way, catching,
grinding, and stiffness. In some cases, pain may be referred from other
areas of the body to the knee. Other causes should always be
considered, especially in cases where the pain is not clearly activity
related; radiates to the hip, back, or foot; or is inconsistent with
the associated physical exam or radiographic studies. In these
circumstances, arthritis of the hip, lumbar radiculopathy, and
inflammatory diseases without joint destruction should be considered.
It is also important to elicit a history of failed nonoperative and
operative treatments including steroid or hyaluronic acid injections,
oral anti-inflammatory medication, physical therapy, bracing,
arthroscopic debridement, ligament reconstruction, and osteotomy.
for total knee arthroplasty is to improve patient function. Evaluating
the degree of disability experienced by a patient can be difficult but
is crucially important. Patient expectations and goals must be clearly
understood to optimize satisfaction postoperatively. Some patients may
simply be hoping to be able to perform activities of daily living
without pain, whereas others may be expecting to be able to participate
in vigorous sports such as marathon training or basketball. In patients
with high expectations, a frank discussion of the goals of knee
replacement and the types of activities that can be realistically
pursued postoperatively is necessary.
include a history of prior infection in the involved knee or active
infection in any other location, neuromuscular conditions such as
Charcot arthropathy, prior fusion of the involved knee, and a
nonfunctional extensor mechanism. Absolute contraindications include
active infection in the involved knee or periarticular region, severe
peripheral vascular disease, and lack of adequate soft tissue coverage.
conditions that the patient has experienced. Obesity, diabetes,
coronary or pulmonary disease, peripheral vascular disease, and immune
compromise owing to cancer or HIV all increase the risks associated
with joint replacement. Comprehensive consultation with appropriate
specialists is critical to optimize results but rarely precludes joint
replacement as long as the patient understands the potential risks.
prior skin incisions about the knee, the overall clinical alignment of
the leg, joint line and peripatellar tenderness, crepitus, whether the
collateral ligaments are competent, and whether the varus or valgus
deformity is passively correctable to neutral. In cases where the
ligaments may be incompetent, a prosthesis with increased
femoral-tibial constraint should be available for use. In addition, the
passive range of motion, fixed flexion contractures, and extension lags
should be noted. Distal pulses, strength and sensation in the extremity
should also be evaluated. Finally, as previously noted, absence of
significant hip pain with passive motion and adequate hip range of
motion should also be verified.
preoperative counseling in most cases. Standard views include a
weight-bearing anterior-posterior (AP) view in full extension, a
lateral view, and a Merchant view of the patellofemoral joint. In some
cases a posterior-anterior (PA) view in 45 degrees of flexion is
helpful for demonstrating significant joint space narrowing when the AP
standing view shows only minimal changes. The PA flexion view provides
a superior view of the contact between the distal-posterior femoral
condyles and the tibia, which is an area where significant cartilage
wear can occur. In cases where joint space narrowing is unremarkable or
where pain is out of proportion to the radiographic evidence, MRI of
the knee may identify meniscal pathology or other periarticular
pathology such as avascular necrosis, stress fractures, and bone
lesions that require alternative treatment. If lumbar or hip pathology
is suspected after physical exam, then adequate radiographs of these
areas should also be obtained.
view of the lower extremity helps with preoperative planning. However,
this is probably only mandatory in cases where there is a history of
prior fractures or surgery of the ipsilateral extremity, or physical
exam suggests unusual extra-articular deformities.
knee replacement include selecting placement of the skin incision,
gaining adequate exposure to the joint, restoring axial alignment of
the limb by accurately resecting bone from the femur and tibia, and
creation of symmetric flexion and extension gaps with balanced medial
and lateral soft tissue tension by releasing the contracted structures.
Subtle differences exist depending on whether a posterior cruciate
retaining, substituting, or sacrificing prosthesis is implanted, but
the broad principles are the same and these are presented in the
subsequent sections.
that deviates slightly to the medial side of the tibial tubercle
distally is the most utilitarian approach to the knee. Traditionally,
incision length was between 15 and 20 cm depending on the size of the
patient and surgeon preference. However, with increased emphasis in
recent years on reducing incision length and soft tissue dissection in
so-called minimally invasive techniques, the incision length has
declined and various authors have described the ability to perform TKA
through shorter skin incisions.
blood supply to the knee is limited. The vascular supply to the
overlying skin is medially biased, and this should be considered in the
decision about incision placement when prior incisions exist. In
particular, wide scars, lateral incisions, and skin with posttraumatic
or postradiation scarring or thinning should be treated with special
concern. In general, a single pre-existing transverse incision may be
crossed at a right angle with little concern. If a prior anterior
incision is present, it should be used unless it lies too far medial or
lateral. In circumstances where a prior vertical incision is
significantly displaced from the midline, especially with short,
well-matured scars, a second vertical midline incision can be made if
an adequate skin bridge of about 5 cm can be maintained. However, if
multiple vertical or mixed anterior incisions are present, alternative
techniques such as tissue expanders or even prophylactic muscle flaps
may be required to reduce the risk of postoperative wound-healing
problems.
that has been used, although with recent minimally invasive techniques,
placement of the short incision over the area where the arthrotomy will
be performed is optimal. The most utilitarian approach to the knee
joint is via a medial parapatellar arthrotomy that begins 5 to 8 cm
proximal to the superior pole of the patella, about 5 mm lateral to the
medial border of the quadriceps tendon. The arthrotomy extends distally
either around the medial border of the patella or directly over the
medial edge of the patellar and then extends along the medial edge of
the patellar tendon about 5 to 8 cm distal to the joint line. Next, the
anterior horn of the medial meniscus is transected and the medial
capsule and periosteum is elevated from the proximal 3 to 4 cm of the
medial tibia. The infrapatellar fat pad is resected, and the lateral
patellofemoral ligament is divided. If at this stage the patella cannot
be subluxated laterally, or everted from the field of view, a
quadriceps snip can be performed. Beginning at the apex of the
arthrotomy in the quadriceps tendon, the arthrotomy is extended
laterally and superiorly at an angle of 45 degrees into the vastus
lateralis muscle. In the rare case where this maneuver does not relieve
tension on the extensor mechanism and the exposure is still inadequate,
a tubercle osteotomy can then be performed and will provide adequate
exposure.
prompted renewed interest in alternative approaches to the anterior
knee that include subvastus, mini midvastus, and medial and lateral
capsular incisions. Although all of these alternatives are believed to
cause less damage to the extensor mechanism and allow quicker
functional recovery, few controlled studies exist. Furthermore, the
visualization of the knee with any of these exposures is limited, and
therefore, they are not suitable for every patient in all surgeons’
hands. In particular, patients with heavily muscled thighs, obese
patients, and patients with patellar baja or large deformities pose
special challenges and may not be amenable to these limited approaches.
 |
|
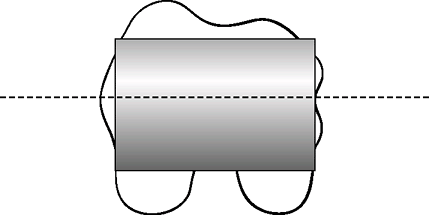
Figure 25-1
The mechanical axis of the knee should pass through the center of the hip, knee, and talus once the prosthesis has been implanted. Both the femoral and tibial components are oriented perpendicular to the mechanical axis. The femoral component is in approximately 5 to 7 degrees of valgus relative to the anatomic axis of the femoral shaft. |
operated leg within a narrow range of ±3 degrees has been demonstrated
to be an important determinant for long-term success following TKA.
Therefore, bone resection must be performed in an accurate and
reproducible way. Orientation of the femoral and tibial components
parallel to the mechanical axis of the leg is the goal of the bone
resection in TKA (Fig. 25-1). Many instruments
have been designed to help the surgeon optimize the bone resection of
the distal and posterior femur and proximal tibia. These include both
intramedullary and extramedually alignment guides and cutting blocks
that are affixed to the bones. Recently computer navigated systems that
use either optical or electromagnetic sensors have been developed to
aid in this task and have demonstrated more reproducible results than
mechanical guides. The specific order of femoral and tibial cuts is
irrelevant as these steps are independent in the classic method of bone
resection that is favored by many surgeons. It must be recognized that
some surgeons favor the use of tensor systems that rely on a tibial cut
made perpendicular to the mechanical axis of the tibia to determine the
femoral cuts. In this technique, the tibial cut must be made first.
should be cut in 5 to 7 degrees of valgus relative to the femoral shaft
or anatomic axis. However, to avoid persistent excessive valgus
alignment in a valgus knee, a distal femoral cut of 4 to 5 degrees of
valgus relative to the anatomic axis is suggested in these cases. A
three-joint view of the limb can facilitate selection of the optimal
distal femoral resection by allowing the angle between the anatomic and
mechanical axes of the femur to be measured for the specific
individual. Other variables such as the placement of the starting hole
and fit of the intramedullary alignment guide in the femoral canal can
affect the accuracy of the cut and probably have more of an influence
on the ultimate resection angle than surgeon choice of 5 or 6 degrees.
 |
|
Figure 25-2
The femoral component is aligned parallel to the transepicondylar axis, which passes through the center of the prominence of the lateral epicondyle and the center of the sulcus of the medial epicondyle. |
This step will determine the anterior femoral and posterior femoral
condylar resections. The epicondylar axis has been shown to be the most
reliable landmark for determining accurate rotation and is easily
identified intraoperatively. If the femoral component is not set
parallel to this axis, it
is
difficult to produce a symmetric flexion space. The AP axis, or
so-called Whiteside line, is a good secondary reference point that
links the center of the intercondylar notch and the center of the
femoral trochlea. This axis is usually perpendicular to the epicondylar
axis. With the femoral cutting block oriented relative to these
landmarks, in most circumstances, more bone will be resected from the
posterior medial condyle than the lateral condyle because the
epicondylar axis is externally rotated relative to the posterior
condylar line. In a varus knee the epicondylar axis is generally
externally rotated by about 3 degrees relative to the posterior
condylar line, whereas in the valgus knee the epicondylar axis tends to
be externally rotated by about 5 degrees.
bone cut perpendicular to the mechanical axis. Approximately 9 to 10 mm
of bone typically will be resected from the unaffected compartment,
i.e., from the lateral side in a varus knee. Once the distal and
posterior femoral cuts and tibial cut have been made, a spacer block
with an extramedullary guide rod is inserted to evaluate whether the
optimal limb alignment has been achieved. If the bone cuts fail to
achieve the desired limb alignment, then soft tissue balancing of the
medial and lateral structures may be difficult to achieve. Furthermore,
as previously noted, detrimental mechanical stresses associated with
chronic malalignment can lead to progressive laxity and instability. If
overall alignment is acceptable, then the next step is creating
balanced and symmetric flexion and extension gaps.
begins with an examination of the extremity under anesthesia to
evaluate the integrity of the collateral soft tissue restraints. If the
deformity can be corrected to neutral, a less aggressive soft tissue
release should be anticipated than in a knee with a fixed deformity.
Once the bone cuts have been performed as noted previously,
re-evaluation of the medial and lateral soft tissue tension is
performed with a spacer block as previously noted. In addition to bone
and cartilage erosion, the development of deformity associated with
degenerative arthritis involves the development of contractures of the
soft tissue structures on the concave side of the deformity, and
eventually, stretching of the structures on the convex side. For
example, in the valgus knee, the lateral structures shorten and the
medial soft tissues may become attenuated. The goal of soft tissue
balancing is to release or lengthen the tight structures to create
symmetric, rectangular flexion and extension spaces (Fig. 25-3).
Although mild degrees of soft tissue imbalance may be clinically
insignificant, it seems prudent to strive for optimal balance. The
techniques described below for soft tissue balancing are based on the
principles described by Insall.
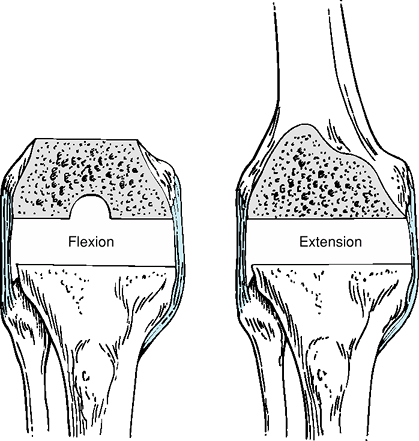 |
|
Figure 25-3 Equal and symmetric flexion and extension gaps are created by bone resection and soft tissue releases.
|
include the pes anserine tendons, superficial medial collateral
ligament (MCL), posteromedial corner including the semimembranosus
insertion, and deep MCL. After the standard arthrotomy and exposure has
been performed and the bony cuts on the femur and tibia have been
completed, the remnants of the cruciate ligaments and menisci should be
excised. This is best performed with the knee in flexion, with a lamina
spreader providing gentle joint distraction. It is important to
remember that the fibers of the deep MCL attach to the peripheral
margin of the midbody of the medial meniscus and must not be damaged
during meniscal resection. This is most safely accomplished by leaving
a thin rim of 1 to 2 mm of peripheral meniscus. At this stage,
posterior condylar osteophytes should be removed with an osteotome.
flexion gap is inserted and stability is assessed. The knee is then
extended and the limb alignment is evaluated. If alignment is
acceptable, then the medial-lateral balance is assessed. If the medial
structures are still tight, as is frequently found in the varus knee,
an incremental release of the medial structures is performed to correct
the asymmetry of the medial and lateral soft tissue tension. A ¾-inch
straight osteotome
is
used to extend the subperiosteal elevation of the distal superficial
MCL insertion and deep fascia along the posteromedial border of the
tibia. This release may be extended to approximately the level of the
middle third of the tibia. In addition, the pes tendons may be
released. In some cases, the popliteus tendon may impinge on the
posterolateral aspect of the prosthesis, and in these cases of varus
deformity it may be released.
release is evaluated. In many cases, once the extension space symmetry
has been restored by the release, the next thicker spacer block is
required. If an imbalance persists, then further subperiosteal
elevation of any palpable tight medial bands should be performed
distally. In addition, the tibia should be subluxated and externally
rotated out from underneath the femur, and in this position a
subperiosteal elevation of the semimembranous and posterior capsule
from the posteromedial tibia should be completed if not already done.
include the iliotibial band (ITB), lateral collateral ligament (LCL),
popliteus tendon, and arcuate ligament/posterolateral capsular complex.
If alignment is acceptable when the knee is brought into extension with
the spacer block, but the lateral side is tight, then the spacer is
removed and laminar spreaders are inserted and gently opened. The
lateral soft tissue structures are then released in a graduated fashion
using an inside-out technique with the popliteus tendon as a landmark.
The arcuate and posterolateral capsular complex are incised
horizontally with a number 15 blade at the level of the tibial bone
cut. Next, multiple “pie crusting” puncture incisions are made through
the ITB and capsule, both at the level of the extension gap and
proximal to the joint. Although no specific attempt is made to divide
the LCL, it is likely at least partially cut. Once the extension gap
appears rectangular, the spacer block is reinserted and the balance
re-evaluated. If at this stage the lateral side is still tight, then
further pie crusting is performed. In certain cases, the ITB may need
to be released entirely from Gerdy’s tubercle.
if possible, to act as a lateral stabilizer in flexion and to help
prevent rotatory instability. However, in severe valgus knees,
typically greater than about 20 degrees, the lateral side may be tight
despite the above-noted releases. In these cases, it may be necessary
to strip the lateral femoral condyle including the insertion of the
popliteus tendon, either sharply or by elevating a wafer of bone from
the lateral epicondyle. In these situations, a constrained prosthesis
may be required to provide medial and lateral stability. In elderly
patients with large valgus deformities, use of a constrained condylar
type of prosthesis has been associated with good long-term results
despite the theoretical concerns regarding loosening.
created in either the varus or valgus knee, the knee is assessed to
ensure that the size of the overall gaps is equal. The spacer block
that allows full extension to be achieved without any tendency to
hyperextension is selected, and finally the flexion space must be
re-evaluated to ensure that it is symmetric with the extension gap. In
cases where the flexion and extension gaps are not equal, further
adjustments to the bone resection may be required.
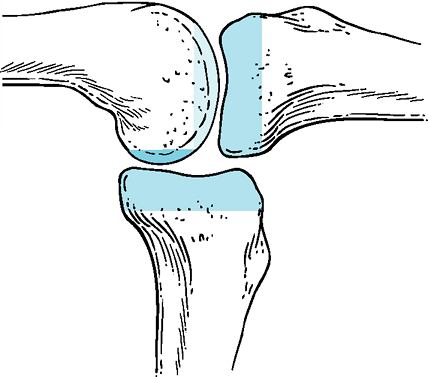
flexion and extension gaps, a comprehensive understanding of the impact
of the three basic bony cuts in total knee arthroplasty is required.
The proximal tibial cut affects both the flexion and extension gap
equally, whereas the distal femoral cut selectively determines the
extension gap and the posterior femoral resection affects only the
flexion gap (Fig. 25-4). These basic principles provide excellent guidance if asymmetric size gaps are encountered.
 |
|
Figure 25-4
The tibial resection influences both the flexion and extension gaps, whereas the distal femoral cut affects only the extension gap and the posterior femoral resection influences only the flexion gap. |
extension, with a persistent flexion contracture, an additional 2 mm of
femur must be removed as femoral resection selectively changes only the
extension gap. In some cases, elevation of the posterior capsule from
the femur can correct a slight tendency to residual flexion
contractures, especially in the setting of significant preoperative
contractures, but bony resection generally provides a more satisfactory
result. If the knee is too tight in both flexion and extension to allow
insertion of the smallest 10-mm spacer, then additional tibia must be
cut as tibial resection changes both the flexion and extension gaps. In
the primary setting, with a posterior cruciate retaining implant, it is
uncommon to find the knee balanced in extension and too loose in
flexion. This may be encountered in a posterior stabilized (PS) knee
where release of the PCL may increase the flexion gap more than the
extension space. In this setting, resection of additional distal femur
and use of a larger polyethylene insert will be the solution. In rare
circumstances with either a cruciate-retaining (CR) or PS knee,
overresection of the posterior femoral condyles owing to the use of an
anterior referencing femoral cutting guide or undersizing of the
femoral component may be responsible. In these cases where a CR
prosthesis has been used, restoring the posterior condylar offset
by
upsizing the femoral component and using posterior augments can be
considered. With a PS knee, additional distal femur can be resected and
a larger polyethylene used. This may move the joint line more
proximally, but 5 to 8 mm of elevation is well tolerated with a PS
knee. In distinction, joint line elevation with a CR knee is less
desirable. Finding that the extension gap is balanced but the flexion
gap is tight is more likely to occur in a CR knee where the PCL is too
tight. In these cases, graduated release of the PCL or increasing the
slope of the tibial cut should be used to solve the gap imbalance.
been obtained, the bone surfaces can be prepared for final component
positioning. On the femoral side, chamfer cuts must be made as well as
a box cut if a PS prosthesis is used. The femoral component should be
lateralized on the distal femur, without creating overhang, to optimize
patellar tracking. Next, tibial rotation is oriented relative to the
junction of the medial and middle thirds of the tibial tubercle.
Internal rotation may result in lateral patellar subluxation. Finally,
the patellar component is positioned slightly medially and superiorly
on the prepared surface, which helps prevent patellar maltracking. The
overall composite thickness of the resurfaced patella should restore,
or when possible, slightly reduce (1 to 2 mm) the thickness of the
native patella. Once these steps have been completed, a reduction using
trial components is performed to ensure that appropriate soft tissue
balance has been achieved without flexion contracture or
hyperextension. If imperfections exist, adjustments are made. Lastly, a
“no thumbs” technique is used to evaluate patellar tracking. If the
femoral and tibial rotations have been set correctly, the thickness of
the patellar has been reproduced, and the other techniques for
optimizing patellar tracking have been used, patellar subluxation is
uncommon in the varus knee. However, if no technical errors can be
identified and maltracking is present, a lateral patellar release
should be performed. Once the result with the trial components is
acceptable, the surfaces are cleaned and dried and the real components
are cemented in place. Once the cement is hard, I routinely release the
tourniquet and cauterize any significant bleeding vessels. The joint is
irrigated and a deep drain is placed prior to arthrotomy closure, which
is performed in extension. After skin closure, a light sterile dressing
is used.
control. Both nonsteroidal anti-inflammatory medications and narcotic
analgesics are given preoperatively in the holding area. Regional
blocks including femoral and sciatic nerve blocks are performed
preoperatively and are continued postoperatively for 24 to 48 hours. In
conjunction with the regional blocks, intravenous narcotics are
administered via a patient-controlled analgesia device for breakthrough
pain during the first 24 hours. Patients are then switched to oral
narcotics for pain control. Passive and active ranges of motion are
begun on postoperative day 1 and are advanced as tolerated; the
importance of active extension is emphasized to the patient. Ambulation
with weight bearing as tolerated is also begun on postoperative day 1,
without limitation. Early goals include independent transfers, walking
as tolerated, and active motion from full extension to 90 degrees of
flexion. Other important perioperative interventions include the use of
prophylactic antibiotics given within an hour of the incision and
continued for 24 hours postoperatively, and deep vein thrombosis
prophylaxis. A multimodal approach to DVT prophylaxis is also used,
including the use of thigh-high compression stockings, mechanical
sequential compression devices, and low-molecular-weight heparin or
adjusted dose Coumadin. The use of continuous passive motion machines
is controversial, and there are studies that both support and refute
its efficacy.
replacement have been proven both consistent and durable. Indeed,
long-term survivorship has been reported from independent centers to be
>90% to 95% at 10 years or greater. In these studies, various
prosthesis designs have demonstrated excellent results in both young
and old adults. Despite these highly reproducible outcomes, failures do
occur. Infection, mechanical failure, periprosthetic fracture, aseptic
loosening, polyethylene wear, and instability are the most common modes
of failure. Although some of these problems may be unavoidable,
long-term success has clearly been noted to be related to patient
characteristics and the accuracy with which the prosthesis is
implanted. Therefore, both careful preoperative evaluation and optimal
surgical technique should be used and remain within the control of the
orthopaedic surgeon.
RA, Rubash HE, Seel MJ, et al. Determining the rotational alignment of
the femoral component in total knee arthroplasty using the epicondylar
axis. Clin Orthop. 1993;286:40–47.
HD, Scuderi GR. Correction of valgus deformity in total knee
arthroplasty with the pie-crust technique of lateral soft-tissue
releases. J Knee Surg. 2004;17(3):157–166.
AL, Rand JA, Bryan RS, et al. Total knee arthroplasty with the
kinematic condylar prosthesis. A ten-year follow-up study. J Bone Joint Surg Am. 1995;77:423–431.
RD, Thornhill TS. Posterior cruciate supplementing total knee
replacement using conforming inserts and cruciate recession. Effect on
range of motion and radiolucent lines. Clin Orthop. 1994;309:146–149
