Glenohumeral Arthritis: Rheumatoid
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 43 – Glenohumeral Arthritis: Rheumatoid
inflammatory disorder with an estimated worldwide prevalence of about
1%. Its prevalence increases starting in the third decade of life; 5%
of the population older than 70 years develops RA. Musculoskeletal
involvement in RA is characterized by the formation of an erosive
synovitis that results in continued bone, cartilage, and soft tissue
degradation.
some authors have estimated shoulder involvement in about 60% of
rheumatoid patients. The condition may affect all the synovial joints
of the shoulder region—glenohumeral, acromioclavicular, and
sternoclavicular—and the scapulothoracic articulation may become
secondarily affected by periscapular fibrosis (Table 43-1).
Associated soft tissue involvement is common, and many patients
(between 25% and 50% depending on the series) with rheumatoid
involvement of the shoulder eventually develop rotator cuff compromise.
When the cervical spine is affected, patients may complain of referred
pain to the shoulder region.
of rheumatoid arthritis has continued to improve, and the presentation
of patients with RA has changed somewhat owing to the effect of these
medications. Some of them are powerful modulators of the immune system
that may substantially increase the risk of infection if they are not
discontinued prior to surgery. The possibility of rheumatoid
involvement and infection coexistence should be taken into
consideration. Some patients may also develop shoulder symptoms related
to steroid-induced humeral head osteonecrosis.
and surgical treatment of glenohumeral rheumatoid arthritis. Physical
therapy and steroid injections also play a role in the treatment of
shoulder RA. However, multiple steroid injections should be avoided, as
they may have a deleterious effect on connective tissue structures.
Most physicians suggest limiting injections to three and repeating
injections only when significant improvement resulted from the previous
injection.
by pain associated with various degrees of stiffness, weakness, and
deformity. Most patients are referred to the orthopedic surgeon for
evaluation and treatment of glenohumeral joint involvement. However,
the acromioclavicular, sternoclavicular, and scapulothoracic
articulations should be evaluated systematically, as failure to address
them may lead to incomplete improvement. It is important to assess
active and passive range of motion as well as rotator cuff atrophy and
strength.
context of other joints involved in the upper and lower extremity. Hip,
knee, foot, or ankle problems may need to be addressed first if they
are symptomatic enough, as well as to decrease the load of crutches or
a walker on the upper extremity, especially if rotator cuff repair will
be required. Hand and elbow involvement should also be taken into
consideration not only to address the most symptomatic joint first and
delineate an overall surgical plan for the upper extremity but also to
leave room for shoulder and elbow stems should shoulder and elbow
arthroplasty both be needed. Finally, all patients undergoing surgical
intervention should be evaluated for atlantoaxial instability and
temporomandibular involvement (Fig. 43-2).
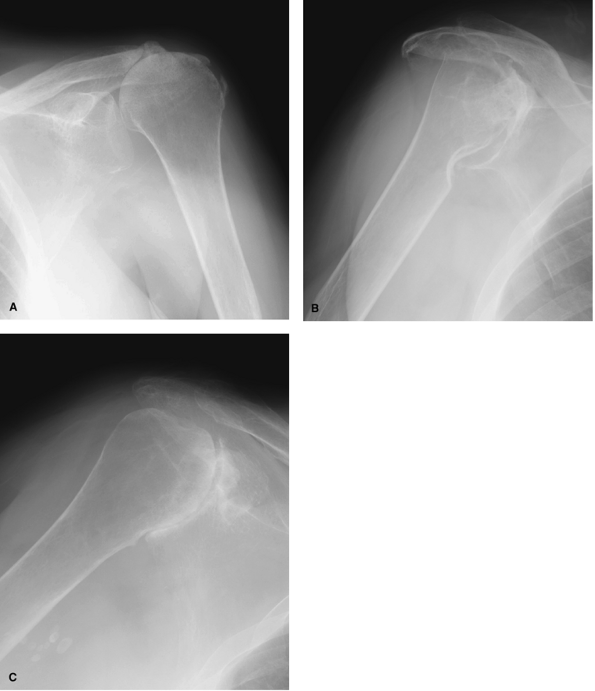
depending on the stage and severity of rheumatoid involvement. Patients
with early synovitis may have minimal radiographic changes, but most
patients do present joint line narrowing, osteopenia, and various
amounts of erosion and bone loss at the humeral head, glenoid, and
coracoacromial arch (Fig. 43-1). Proximal humeral migration may indicate cuff attenuation or tearing.
CT scan may be helpful for preoperative planning. Shoulder MR should be
considered in patients with clinical evidence of rotator cuff
involvement but is not needed in every case.
 |
|
Figure 43-1 Radiographic examples of rheumatoid arthritis of the shoulder.
|
with synovitis when the glenohumeral arthritis is not severe enough to
warrant shoulder arthroplasty. The indications for synovectomy have
decreased as the effectiveness of medical treatment has increased. The
severity of synovitis may be evaluated with either MR or arthrography.
Arthroscopic surgery provides global access to the entire joint with
minimal morbidity, allows a relatively quick recovery, and is
associated with a low complication rate. In addition, it provides
access not only to the glenohumeral joint but also to the subacromial
space and acromioclavicular joint if needed. Associated rotator
pathology may be addressed at the time of arthroscopy. Finally, it does
not burn any bridges for a later arthroplasty unless it is complicated
by a permanent nerve injury or deep infection.
|
TABLE 43-1 Spectrum of Shoulder Pathology in Rheumatoid Arthritis
|
|
|---|---|
|
of at least three portals, as the axillary recess is difficult to reach
from the standard posterior and anterosuperior portals. Patients with
associated capsule contracture and floating cartilage flaps may benefit
from contracture release and cartilage debridement, respectively.
Subacromial bursectomy may be required as an isolated or associated
procedure; acromioplasty and resection of the coracoacromial ligament
are not recommended to avoid weakening of the coracoacromial arch,
which may become problematic should cuff attenuation or tearing occur.
 |
|
Figure 43-2 Atlantoaxial instability is present commonly in patients with RA and may complicate anesthesia.
|
 |
|
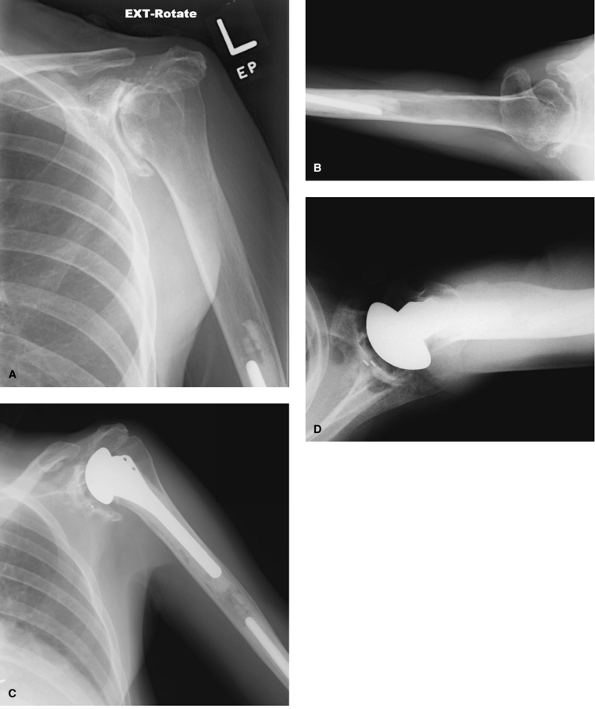
Figure 43-3 Progressive glenoid bone loss may compromise the ability to implant a glenoid component.
|
reliable in terms of pain relief than restoration of motion.
Interestingly, published reports on the effectiveness of arthroscopic
shoulder synovectomy for RA are sparse. Although synovectomy has been
proposed to delay progressive joint deterioration, this prophylactic
effect has been difficult to prove in clinical practice. The Mayo
Clinic experience on arthroscopic shoulder synovectomy was recently
reviewed. Sixteen shoulders were followed for a mean of 5.5 years after
synovectomy; improvement in pain was noted in 13 patients, with less
predictable improvement in motion. Most patients with radiographic
follow-up showed disease progression, and worse results were obtained
in those patients with more severe radiographic changes at presentation.
improve function in patients with symptomatic glenohumeral arthritis
that will not respond to other treatment options. Although orthopedic
surgeons generally advise delaying joint arthroplasty in other
locations or conditions as much as possible, it may be advisable to
recommend shoulder arthroplasty sooner rather than later in rheumatoid
patients before glenoid bone loss, contractures, and rotator cuff
tearing compromise the ability to use a glenoid component or to improve
motion and strength.
provide the best results in terms of pain relief and functional
restoration. However, glenoid component implantation is contraindicated
if glenoid bone stock is insufficient or there is an associated large
and irreparable rotator cuff tear. Good results have been reported with
both resurfacing and standard humeral components. Uncemented
tissue-ingrowth
humeral
components can be used if the metaphyseal bone is intact and if it is
possible to achieve adequate diaphyseal contact and fit. However,
cemented fixation is advisable in many instances, realizing the
potential complications of cement removal from the humeral shaft in
rheumatoid patients should revision surgery be needed. When cement is
used, it is wise to use antibiotic-loaded polymethylmethacrylate. The
use of a reverse shoulder arthroplasty in rheumatoid patients with
extensive cuff tearing is controversial; it may provide surprisingly
good functional results initially, but the glenoid is oftentimes too
osteopenic to allow secure and long-lasting fixation of the glenoid
implant.
The skin is usually extremely fragile. Local osteopenia may facilitate
the occurrence of intraoperative fractures; humeral rotation for
exposure should be done carefully, and extension of the deltopectoral
approach by deltoid detachment from the acromion and spine of the
scapula (the so-called anteromedial approach) is recommended to reduce
the risk of fracture in the presence of severe osteopenia and
contractures. The rotator cuff should be systematically evaluated and
prepared for repair when tears are found. The coracoacromial arch
should be preserved intact as a stabilizing mechanism against
anterosuperior subluxation in the event of rotator cuff failure.
useful information to determine the feasibility of glenoid
implantation, the final decision is made at the time of surgery. A hole
may be drilled at the glenoid center to estimate the thickness of
remaining bone stock; usually, a component can be safely placed if
there is at least 2 cm of depth. Central bone loss is more common than
peripheral bone loss; however, when segmental bone loss is present,
consideration may be given to structural bone graft. A pegged glenoid
component is used if possible, as it seems to allow better
implant/cement/bone interface (Fig. 43-4);
however, keeled glenoid components may allow implantation in situations
where loss of bone stock will not allow secure placement of a pegged
glenoid component. When glenoid bone stock is insufficient, shoulder
hemiarthroplasty is the preferred option.
|
TABLE 43-2 Shoulder Arthroplasty in RA: Technical Considerations
|
|||
|---|---|---|---|
|
humeral size as well as stability and motion. When the joint is
contracted, it may be necessary to select a smaller humeral head to
maintain functional motion. On the other hand, patients with attenuated
soft tissues may require a larger humeral head to fill the joint space
in the presence of a stretched capsule and rotator cuff tendons.
cuff involvement is not associated with severe glenoid bone loss may
benefit from a reverse shoulder arthroplasty. The same precautions in
terms of exposure and avoidance of undue stresses to decrease the risk
of fracture should be taken into consideration. Glenoid reaming should
be done carefully, because the glenoid can be easily fractured by a
sudden torque if the reamer is trapped against irregular bone.
guidelines of shoulder arthroplasty, with sequential passive,
active-assisted, and strengthening exercises. Patients who require an
associated rotator cuff repair should not start active use of the
shoulder for at least 6 weeks. Patients with severely compromised soft
tissues and cuff benefit from a limited-goals type of program., Some
authors recommend letting the patient immediately return to activities
of daily living after a reverse arthroplasty; in patients with
rheumatoid arthritis, it is probably best to delay immediate activity
for the first 4 weeks with the use of a sling.
most rheumatoid patients; functional improvements have not been
consistently reported in the literature. When a glenoid component can
be safely implanted, total shoulder arthroplasty is associated with a
better outcome than with humeral head replacement. Likewise, when an
associated cuff tear is found, concomitant cuff repair significantly
improves postoperative clinical shoulder scores compared with those of
patients in whom tears are not repaired.
recently published. Thirty-six hemiarthroplasties and 25 total shoulder
arthroplasties were followed for a mean of 3 years. The underlying
diagnosis was rheumatoid arthritis in 53 shoulders and other
inflammatory conditions in the remaining shoulders. Shoulder
arthroplasty was associated with a significant improvement in pain and
quality
of
life. Motion was also improved, to a mean of 90 degrees with
hemiarthroplasty and 115 degrees with total shoulder arthroplasty.
Complications included four periprosthetic fractures (two
intraoperative), glenoid loosening in two shoulders, and progressive
glenoid erosion in four hemiarthroplasties. Other authors have reported
a high incidence of rotator cuff tears occurring after shoulder
arthroplasty in RA, as well as higher rates of glenoid loosening with
longer follow-up.
 |
|
Figure 43-4 Preoperative (A, B) and postoperative (C, D)
radiographs of a patient with severe rheumatoid involvement that required total shoulder arthroplasty. Glenoid bone loss was not severe enough to prevent implantation of a glenoid component. The tip of an elbow humeral component can be appreciated below the cemented shoulder humeral stem. |
which facilitates the use of stemmed elbow replacement as well as
shoulder revision surgery should this become needed. However, humeral
head erosion commonly seen in rheumatoid arthritis may compromise
fixation of resurfacing components. In addition, glenoid exposure is
compromised by the retained humeral head. The published experience of a
single institution with this type of component has been satisfactory.
These authors studied 33 hemiarthroplasties and 42 total shoulder
arthroplasties and reported significant improvements in pain relief, an
average flexion gain of about 50 degrees, a high rate of satisfactory
results, and only three reoperations for component loosening or
progressive glenoid erosion after hemiarthroplasty.
patients with glenohumeral arthritis, an associated irreparable cuff
tear, and pseudoparalysis. General concerns about glenoid component
failure are especially concerning in RA owing to glenoid erosion and
osteopenia. Many authors consider RA a relative contraindication for
reverse arthroplasty. In a small series of eight rheumatoid shoulders
treated with a reverse arthroplasty, the average Constant score
improved from 17 to 63 points; there were two cases of glenoid
loosening, and three failed acromion osteosynthesis. These findings
emphasize the functional improvement that can be expected after reverse
arthroplasty as well as the high rate of mechanical failure and other
complications.
arthritis is not very commonly required. Most patients with a cuff tear
have associated glenohumeral arthritis and undergo shoulder
arthroplasty and cuff repair in the same surgical intervention.
However, rheumatoid patients will occasionally present with symptomatic
rotator cuff tear and minimal articular changes, and when nonoperative
treatment fails, they may be candidates for rotator cuff repair.
may be challenging. Some patients have associated stiffness. In
addition, the friable nature of the cuff and humeral head osteopenia
may compromise the security of open and arthroscopic techniques.
Acromioclavicular erosion may debilitate the coracoacromial arch; if
acromioplasty is needed, it should be performed carefully, and every
effort should be made to preserve the coracoacromial arch.
of cuff repair in RA. The Mayo Clinic experience was recently reviewed.
Twenty-three repairs were followed for a mean of 10 years or until
revision. Tears were partial thickness in nine cases; full-thickness
tears were categorized as medium in nine cases, large in four, and
massive in one. Surgery provided significant improvements in pain, but
motion and strength remained mostly unchanged. No improvement was
reported in five cases, three of which underwent reoperation.
Full-thickness tears tended to be associated with worse function after
surgery. Although pain relief and patient satisfaction may be achieved
after surgical repair of rotator cuff tears, functional gains should
not be expected when the tear is full thickness.
respond to nonoperative treatment, consideration should be given to ACJ
synovectomy and resection of the distal end of the clavicle, which may
be performed open or arthroscopically. Involvement of the
sternoclavicular joint may require synovectomy and rarely resection of
the medial end of the clavicle.
WP, Thornhill TS, Thomas WH, et al. Nonconstrained total shoulder
arthroplasty in patients with polyarticular rheumatoid arthritis. J Arthroplasty. 1989; 4:91-96.
HE III, Inglis AE, Goldberg VM, et al. An analysis of factors affecting
the long-term results of total shoulder arthroplasty in inflammatory
arthritis. J Arthroplasty. 1988; 3(2):123-130.
RJ, Thornhill TS, Thomas WH, et al. Non-constrained total shoulder
replacement in patients who have rheumatoid arthritis and class-IV
function. J Bone Joint Surg. 1989; 71A:494-498.
RC, Merkies ND, de Waal Malefijt MC, et al. Shoulder hemiarthroplasty
in rheumatoid arthritis. 19 cases reexamined after 1-17 years. Acta Orthop Scand. 1997; 68(3):243-245.
JT, Kaarela K, Belt EA, et al. Incidence of glenohumeral joint
involvement in seropositive rheumatoid arthritis. A 15 year endpoint
study. J Rheumatol. 2000; 27(2):347-350.
M, Kerschbaumer F. Grammont reverse total shoulder arthroplasty in
patients with rheumatoid arthritis and nonreconstructable rotator cuff
lesions. J Shoulder Elbow Surg. 2001; 10:17-22.
O, Fruensgaard S, Johannsen HV, et al. Total shoulder replacement in
rheumatoid arthritis: proximal migration and loosening. J Shoulder Elbow Surg. 1996; 5(1):47-52.
