STENOSING TENOSYNOVITIS AND EPICONDYLITIS
III – THE HAND > Conditions of Tendons > CHAPTER 50 – STENOSING
TENOSYNOVITIS AND EPICONDYLITIS
almost frictionless gliding of flexor and extensor tendons.
Inflammation of the tenosynovium, especially at points where a tendon
changes direction, can lead to stenosis of the tendon sheath, which
interferes with the action of the enclosed tendon. Symptoms include
pain and limitation or irregularity of joint motion. Stenosing
tenosynovitis may affect any of the flexor or extensor tendons, alone
or in combination.
repetitive trauma related to occupation or sports, tumor, infection,
gout, rheumatoid arthritis, and metabolic disorders. The principles of
treatment include cessation or modification of the activities
contributing to pain, hand therapy, use of antiinflammatory agents, and
surgical correction of the impediments to tendon motion.
the first annular pulley of the flexor tendon sheath, which causes pain
and difficulty in extending or flexing the proximal interphalangeal
joint (44,66,94). In the case of trigger thumb, the patient has difficulty extending or flexing the interphalangeal joint (45,98). It appears that fibrocartilaginous metaplasia of the A1 pulley is the cause of the crepitus (82). Repetitive flexion and direct trauma may also cause stenosing tenosynovitis of the flexor tendon of the finger (9,10,25,48,64,88).
The patient feels pain when the digit is forcibly straightened or
flexed. Extending the distal interphalangeal joint before straightening
the proximal interphalangeal joint often avoids the characteristic
painful snap. On palpation, there is usually tenderness just proximal
to the metacarpophalangeal joint on the palmar side.
the flexor digitorum profundus or flexor pollicis longus tendon, which
is proximal or distal to the A1 pulley. A ganglion within
the substance of the first or second annular pulleys may be found in
cases of stenosing tenosynovitis of the flexor tendons of the digits.
tenosynovitis. Interphalangeal joint locking may be caused by
interference with the normal gliding mechanism of the lateral bands or
by irregularities within the interphalangeal joints. Osteophytes and
malunited fractures of the proximal interphalangeal joints can block
extensor hood function and the normal motion of the collateral
ligaments, and joint “mice” can restrict proximal interphalangeal joint
mobility.
It is associated with de Quervain’s disease, with carpal tunnel
syndrome, and with triggering of any of the other nine digits of the
hand (1,6,8,38,54,58,80,81). It occurs more commonly in de Quervain’s disease than in carpal tunnel syndrome.
Surgical correction can be deferred until 1 year of age without
permanent loss of motion. Thirty percent of congenital cases correct
themselves spontaneously before 1 year of age. Splint immobilization
and steroid injection in the flexor tendon sheath may be curative (69).
conservative management. Percutaneous release is less reliable than
other surgical techniques and offers little advantage in the middle and
ring fingers (3,79). For nonrheumatoid patients, percutaneous release is an available but less reliable form of treatment than others (3,79).
It is indicated in the middle and ring fingers where the risk of nerve
damage is less than in other digits. It may be indicated in the elderly
patient with Dupuytren’s disease. The best cure rates are obtained when
the patient is actively locking. The technique involves the use of a
19-gauge needle to cut the A1 pulley distal to proximal over
the hyperextended metacarpophalangeal joint. Partial laceration of the
superficialis tendon is common but generally does not result in
clinical sequelae.
-
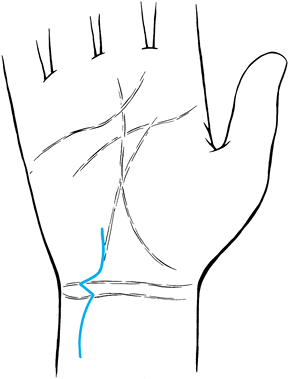
Infiltrate the area of the proposed skin
incision with local anesthetic. In the case of stenosing tenosynovitis
of the index finger, incise the proximal flexor crease of the palm. In
treating triggering of the middle, ring, or little fingers, make a 15
mm incision in the distal flexion crease. In the thumb, incise the
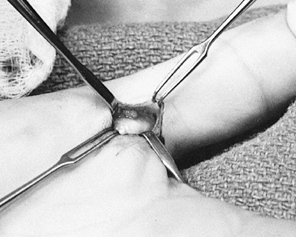
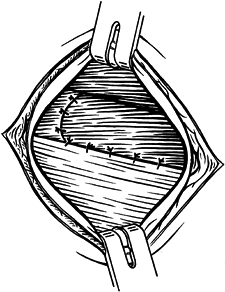
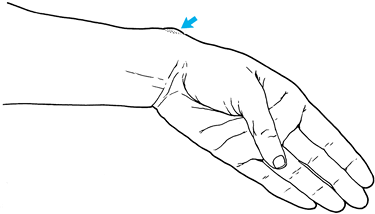
proximal flexion crease in the area between the two sesamoids (Fig. 50.1). Figure 50.1. Skin incision for correction of trigger thumb.
Figure 50.1. Skin incision for correction of trigger thumb. -
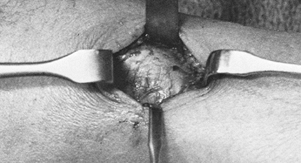
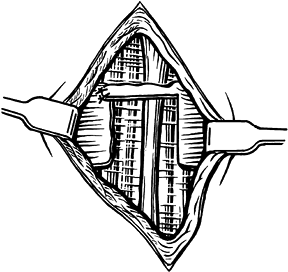
With pneumatic tourniquet control, clear
fat from the palmar surface of the flexor tendon sheath by blunt
dissection. Use medial and lateral Ragnel retractors to protect the
neurovascular bundles (Fig. 50.2).![]() Figure 50.2. Exposure of the thickened proximal pulley in a trigger thumb.
Figure 50.2. Exposure of the thickened proximal pulley in a trigger thumb. -
Identify the proximal edge of the first
annular band by its thickened transverse collagen bundles, which
contrast with the longitudinal striations of the paratenon proximally. -
Incise the radial half of the proximal pulley and resect the redundant tenosynovium from the flexor tendons (Fig. 50.3). Withdraw both flexor tendons from the wound to examine them for thickening.
 Figure 50.3. Division of the proximal pulley of the thumb.
Figure 50.3. Division of the proximal pulley of the thumb. -
If there are tendon nodules and
triggering persists, perform a mid-lateral partial wedge resection of
the tendon substance and primary closure. -
Evaluate the reconstruction by having the
patient move the affected finger. If triggering still persists,
partially section no more than 5 mm of the second annular band by
gentle pressure with open blunt dissecting scissors. -
Fingers caught in extension may have nodular thickening of the flexor digitorum profundus tendon distal to the A2 pulley or constriction of the sheath. Consider performing a partial sectioning of the distal edge of the A2
pulley through an oblique incision near the proximal flexion crease of
the finger, or perform an elliptical resection of tendon substance,
followed by primary tendon closure. -
In patients with rheumatoid arthritis,
strip the flexor tendons at their nodules and tenosynovium through a
zigzag incision from the distal flexor crease at the palm to the volar
distal interphalangeal joint crease. Preserve annular pulleys when the
flexor sheath is opened. Repair them afterwards if their release is
necessary. Resistance to ulnar drift is thereby improved. -
Occasionally, resection of the ulnar slip
of the sublimis tendon is necessary to achieve adequate active and
passive range of motion during the procedure. -
Achieve hemostasis after the tourniquet
is released. Close the skin using nonabsorbable, interrupted sutures.
Apply soft compression dressing to maximize finger mobility.
Occupational therapy may be necessary to reduce residual soft-tissue
contractures in chronic cases.
increased propensity for Dupuytren’s disease (i.e., those of Irish,
English, and northern German extraction) may develop localized
thickening of the palmar fascia as a complication of surgery for
transverse bands of the trigger digit. Excise the palmar fascia that is
visible around the edges of the skin incision to prevent this
complication. In patients with demonstrable Dupuytren’s disease,
surgical correction of trigger digit may stimulate progression of
fascial thickening, and the value of surgery should be weighed
carefully against this risk. If neurovascular injury occurs during
surgery, immediate microsurgical repair is indicated. Avoid resecting
more than 25% of the second annular band to prevent PIP joint
contraction and reduction of total active range of motion of the digit.
Palpating the sesamoids overlying the first metacarpophalangeal joint
prevents excessive radial placement of the skin incision and potential
digital nerve damage.
of the abductor pollicis longus and extensor pollicis brevis within the
first dorsal compartment of the wrist (21,27,42). Pain that often radiates up the forearm or
down to the thumb and swelling over the radial styloid characterize the disorder (Fig. 50.4).
Wringing motions of the hand and wrist, and repetitive flexion and
extension of the thumb, especially the basal joint, magnify the
symptoms (47,74).
Finkelstein’s maneuver (hyperflexion of the entire first ray with ulnar
deviation of the wrist) reproduces the pain during physical examination
(27). Tenderness on palpation of the radial styloid process and crepitus on motion of the first ray may be evident (13,42).
The inflammatory process may involve either or both the long abductor
and short extensor tendons of the thumb. The abductor pollicis longus
is made up of two or more tendons in 80% of patients (27,61,90). Ganglionic degeneration of the roof of the first extensor compartment is sometimes found.
 |
|
Figure 50.4. Nodular thickening of the first dorsal compartment in de Quervain’s disease.
|
An increased incidence of de Quervain’s disease has been found in
patients with Dupuytren’s disease, rheumatoid arthritis, gout, or
diabetes mellitus. Many patients with de Quervain’s disease develop
trigger finger or carpal tunnel syndrome, or both, although the reverse
is not true (1,25,38,54,63,80,81). Bilateral involvement eventually occurs in 30% of patients with de Quervain’s disease (80,81).
of the radiocarpal and carpometacarpal joints must be identified before
treatment. Try brief periods of splint immobilization of the wrist,
including the first metacarpal, and glucocorticoid injections of the
first dorsal compartment; these are, however, less successful in
treating de Quervain’s disease than other forms of stenosing
tenosynovitis. Avoid prolonged splinting. Instead, initiate active and
passive stretching exercises early to promote tendon gliding. Surgery
is indicated if the symptoms persist despite conservative treatment.
-
Infiltrate the area of the proposed skin incision with local anesthetic before inflating the pneumatic tourniquet (Fig. 50.5).
Make the dorsal half of the incision along a transverse extensor crease
of the wrist about 10 mm proximal to the tip of the radial styloid (Fig. 50.6).
Follow Langer’s lines in a palmar direction, making a 30 mm incision
centered over the radial styloid. Radial sensory nerve branches are
encountered just deep to the dermis; protect them by gentle retraction (Fig. 50.7).![]() Figure 50.5. Infiltration of the skin in surgery for de Quervain’s disease.
Figure 50.5. Infiltration of the skin in surgery for de Quervain’s disease. Figure 50.6. Skin incision for surgical treatment of de Quervain’s disease.
Figure 50.6. Skin incision for surgical treatment of de Quervain’s disease.![]() Figure 50.7. Exposure of the thickened roof of the first dorsal compartment.
Figure 50.7. Exposure of the thickened roof of the first dorsal compartment. -
With a scalpel, incise the thickened sheath of the first dorsal compartment distally and proximally (Fig. 50.8).
There may be more than one septum separating the numerous slips of the
abductor pollicis longus or the extensor pollicis brevis; carefully
identify each tendon.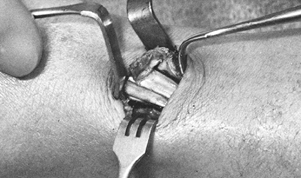 Figure 50.8. Elevation of the roof of the first dorsal compartment.
Figure 50.8. Elevation of the roof of the first dorsal compartment. -
Excise thickened tenosynovium and
retinacular ganglia. Examine the floor of the first dorsal compartment
for bony, neoplastic, and calcific irregularities or anomalous
P.1519
tunnels
containing aberrant tendons. These must be unroofed. Ask the patient to
flex and extend the thumb to demonstrate unimpeded motion. -
After the tourniquet is released, achieve hemostasis. Close the skin with a nonabsorbable intracuticular suture (Fig. 50.9). To prevent palmar subluxation of the tendons, apply a palmar spica splint for 2 weeks until the skin suture is removed.
![]() Figure 50.9. Running intracuticular 5-0 monofilament steel suture is tied over a 4×4 cm gauze dressing.
Figure 50.9. Running intracuticular 5-0 monofilament steel suture is tied over a 4×4 cm gauze dressing.
from thick adhesions to the abductor pollicis longus or failure to
identify and to incise its separate sheath may cause symptoms to
persist. The abductor pollicis longus may have multiple slips inserting
into the first metacarpal and into the trapezium, carpometacarpal joint
capsule, fascia of the opponens or abductor pollicis brevis, or flexor
retinaculum. Failure to identify and separate all of the tendons may
result in incomplete resolution of symptoms.
immediate microsurgical repair to reduce the likelihood of painful
neuroma formation. Compression of the terminal branches of the radial
nerve may also produce pain in the area of the first dorsal
compartment. Symptoms include numbness and tingling over the dorsal
surface of the thumb and index finger. Paresthesias are accentuated by
percussion in this area. In making a diagnosis, be careful to
differentiate this nerve compression syndrome (Wartenberg’s disease)
from de Quervain’s disease.
Usually, there are small tears of the tendon of origin of the extensor
carpi radialis brevis, although the extensor digitorum communis may be
involved as well (70,72). The pathology ranges from angiofibroblastic proliferation to complete tendon rupture (24,71).
Pain over the lateral epicondyle and extensor muscle mass when lifting
objects palm down and when playing racket sports is characteristic.
Throwing and wringing motions may also be painful. Grip strength is
decreased as a result of pain on attempts to stabilize the wrist in
extension. Tenderness to palpation occurs over the lateral epicondyle
of the elbow and radial collateral ligament. Wrist extension against
resistance causes pain at the lateral epicondyle. Radiographic
evaluation of the elbow may demonstrate a lateral exostosis, bone
fragments, or calcific deposits over the lateral epicondyle.
tunnel syndrome, in which the posterior interosseous nerve is
compressed under the fibrous arch of the supinator muscle (60).
Radial tunnel syndrome is characterized by tenderness over the
supinator, just distal to the radial head. Pain is reproduced by the
patient resisting forearm pronation, or by resisting middle finger
extension with the wrist supported. A lidocaine injection at the arcade
may help to distinguish them. The two entities may coexist.
A 90° long-arm splint with the wrist slightly extended and supinated
may be used in recalcitrant cases, although it rarely affects the
outcome. Local injections of glucocorticoids are helpful in severe
cases; repeated injections, however, may cause delayed tendon rupture
resulting from their catabolic effects. Advise patients to change to
“palm-up” lifting and analyze their sport technique and form to prevent
relapse.
prevent relapses. Because the condition is attributable to overuse,
gentle and then progressive wrist curls to strengthen forearm
extensors, and proper stretching exercises are indicated after the
initial recovery is well under way (32).
Surgery is indicated in the few cases that do not respond to
conservative therapy. Endoscopic and arthroscopic releases do not have
the outcome studies yet to justify their use (2,37).
-
After administration of regional or general anesthesia, make a 5 cm longitudinal incision centered over the radial head (Fig. 50.10).
 Figure 50.10. Skin incision used in the surgical treatment of lateral epicondylitis.
Figure 50.10. Skin incision used in the surgical treatment of lateral epicondylitis. -
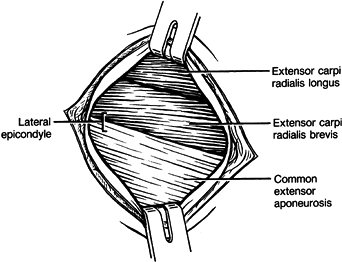
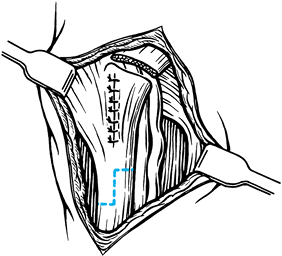
Retract and incise the antebrachial fascia over the extensor carpi radialis brevis, and identify the common extensor origin (Fig. 50.11).
Gross disruption may be visible. Chronic inflammatory changes may be
seen in the proximal margin of the extensor tendon, but
angiofibroblastic changes become apparent after exposing the deep
surface of the tendon of origin.![]() Figure 50.11. Exposure of the common extensor muscle group with their tendons of origin after retraction of the antebrachial fascia.
Figure 50.11. Exposure of the common extensor muscle group with their tendons of origin after retraction of the antebrachial fascia. -
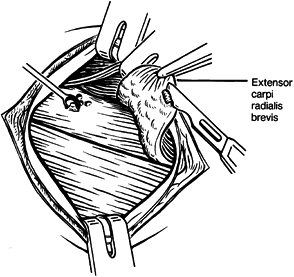
Incise the extensor aponeurosis
longitudinally, where the damage is most accessible. You may need to
elevate the extensor carpi radialis brevis completely as a flap (Fig. 50.12). Do not damage the radial or lateral ulnar collateral ligaments.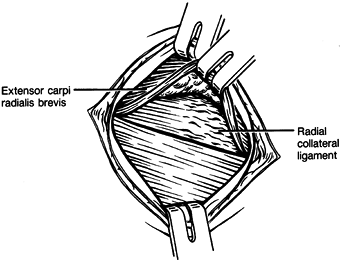 Figure 50.12.
Figure 50.12.
Partial elevation of the tendon of origin of the extensor carpi
radialis brevis, demonstrating tendinous degeneration on its
undersurface where it is attached to the lateral epicondyle and radial
collateral ligament of the elbow. -
Remove proliferative synovium from the
anterolateral joint if crepitus was felt preoperatively. Excise
granulation tissue from beneath the extensor carpi radialis tendon (Fig. 50.13)
and the extensor digitorum communis, if necessary. Debride degenerated
tendon to healthy tissue. The deep surface of the tendon should be free
of all granulation tissue (Fig. 50.14).![]() Figure 50.13.
Figure 50.13.
Excision of granulations from the deep surface of the extensor carpi
radialis brevis tendon and decortication of the lateral epicondyle.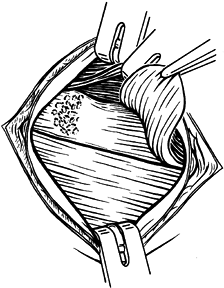 Figure 50.14.
Figure 50.14.
Well-debrided tendon of origin of the extensor carpi radialis brevis
and lateral epicondyle, which are decorticated and prepared for tendon
reattachment. -
Decorticate the lateral epicondyle to punctate bleeding corticocancellous bone. Remove exostoses and calcifications.
-
Suture the extensor carpi radialis brevis tendon to the surrounding periosteum and to the extensor digitorum communis tendon (Fig. 50.15).
If adequate tendon length remains, suture it through connecting drill
holes in the epicondylar ridge. When inadequate tissue remains for a
repair, I use a tendon graft figure-of-eight. Place a bone tunnel or
two suture anchors across the ridge. Capture the fascia and septa of
the affected muscles distally (Fig. 50.16).![]() Figure 50.15.
Figure 50.15.
Reattachment of the extensor carpi radialis brevis tendon of origin to
the extensor aponeurosis and periosteum of the lateral epicondyle.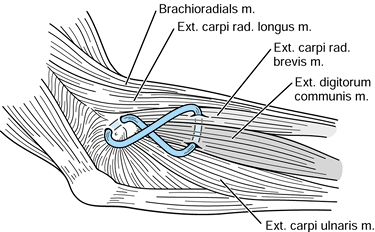 Figure 50.16. Figure-of-eight tendon graft. See text for details.
Figure 50.16. Figure-of-eight tendon graft. See text for details. -
Suture the common extensor aponeurosis
closed, and then close the skin. Immobilize the forearm in a long-arm
splint in neutral rotation with the elbow flexed 90° and the wrist
extended 20°. Remove the splint in 2 to 3 weeks, depending on the
degree of extensor tendon repair. Encourage patients to begin gentle
range-of-motion exercises, but they should avoid stress for 5 weeks.
P.1522
After
that time, gradually initiate progressive, resistive exercises. Advise
patients with complete tears to forego vigorous sports for 6 months.
causes of lateral elbow pain. Rheumatoid arthritis, gout, radial tunnel
nerve syndrome, osteochondritis dissecans, and loose bodies may cause
lateral elbow pain alone or in concert with lateral epicondylitis.
tendons of origin of the flexor pronator muscle group, most commonly
the pronator teres and the flexor carpi radialis (30,32).
Overuse in golf and throwing are common causes of microtearing in this
near mirror-image of its lateral counterpart. During physical
examination, pain on resisted pronation or wrist flexion helps to make
the diagnosis.
well as forceful gripping and twisting. Counterforce bracing over the
proximal muscles of the pronator and flexor radialis may be useful; be
careful to avoid ulnar nerve compression. Injection of a corticosteroid
usually provides fast relief but no long-term benefit (87).
Begin flexor and pronator strengthening exercises when symptoms
persist. Encourage sports technique training since medial epicondylitis
is usually an overuse syndrome. Reserve surgery for at least 6 months
in cases unresponsive to conservative care.
-
Make a skin incision 4 cm long, parallel
and 1 cm proximal to the course of the ulnar nerve, beginning at the
medial epicondyle. Take care to avoid branches of the medial
antebrachial cutaneous nerve. Reflect the affected tendons—the pronator
teres and flexor carpi radialis—off the medial epicondylar ridge.
Reflect them as far posteriorly as the septum between the flexor carpi
radialis and the palmaris longus (when present) or the humeral head of
the flexor carpi ulnaris. While undermining distally, carefully
consider the depth of dissection to avoid the anterior band of the
medial collateral ligament. -
Roughen the epicondyle before reattaching
the tendons to surrounding tendon and fascia. Use a suture if necessary
through connecting drill holes, or one attached to an anchor, to affix
the common tendon of origin more securely to the medial ridge. -
Place the arm into a long-arm splint for
3 weeks with the elbow flexed 90°, the forearm in neutral rotation, and
the wrist at 0°. Begin strengthening exercises at 4 to 6 weeks and
sports at 4 to 6 months.
valgus instability, and medial antebrachial cutaneous or ulnar
neuropathy. Plain and stress radiographic views may demonstrate
nonunion of the medial epicondyle and laxity of the medial collateral
ligament of the elbow. Tenderness to palpation and Tinel’s sign may
demonstrate more distal ligamentous laxity, superficial medial
antebrachial cutaneous neuropathy, or posterior ulnar neuritis. Cubital
tunnel syndrome and its subtle variations must be completely treated
because they may coexist with medial epicondylitis (31,52).
In such cases, even the additional release of the transverse humeral
ligament will fail. Submuscular, ulnar nerve transposition must be
added to the reconstruction to achieve a high level of success.
Repetitive motions of the digits and wrist and direct trauma may cause
or exacerbate flexor tendonitis. Many conditions may precipitate
symptomatic digital flexor tenosynovitis at the wrist. These include
rheumatoid arthritis; gout; collagen vascular disease; anomalous
muscles, tendons, and arteries; tumors; congenital dysplasias; fungus;
tubercle bacillus; and atypical bacteria (1,4,10,39,41,50,58,62,63,67,78,83,97).
Occasionally, local steroid injections or flexor tenosynovectomy are
necessary in recalcitrant cases. Cases involving infection require
surgical decompression and intravenous antibiotics. The treatment of
dysplastic, neoplastic, toxic, and metabolic sources of flexor
tendinitis usually requires surgical decompression and tenosynovectomy
of the flexors or the carpal tunnel and pharmacologic therapy to
protect the contents of the carpal tunnel from irreparable damage and
to eradicate the underlying disease process.
of oral antiinflammatory agents are usually successful in treating noninfectious causes of this condition.
through a limited incision distal to the transverse flexor crease of
the wrist, or through a more extensive exposure involving a 4 cm zigzag
proximal extension of the original thenar crease incision to include
the distal forearm (see Chapter 52); the
latter is more commonly used in patients with rheumatoid arthritis.
Bone spurs need to be excised and large areas of raw bone covered with
ligamentous rotation flaps or patch grafts of transverse retinacular
origin.
-
In performing tenosynovectomy of the
flexors of the carpal tunnel, be careful to avoid lacerating the large,
aberrant sensory branches of the ulnar and median nerves in the
subcutaneous fat, or those penetrating the transverse carpal ligament,
or damaging the median nerve. -
Splint the dorsiflexed wrist for 2 weeks
after surgery to allow a new, loose retinacular “ligament” to form,
preventing painful recurrent subluxation of the finger flexors from the
carpal tunnel when the hand is used to grip in the flexed wrist
position. If subluxing flexor tendinitis occurs at the carpal tunnel,
do a reconstruction of the transverse retinacular ligament using
ligamentous remnants or the adjacent fascia. -
Fashion the new ligament at the distal margin of the carpal canal to prevent compression of the median nerve (Fig. 50.17, Fig. 50.18).
Because Dupuytren’s disease or its diathesis is exacerbated by this
procedure, weigh the pros and cons of surgical management of flexor
tendinitis carefully for patients with coexistent Dupuytren’s disease.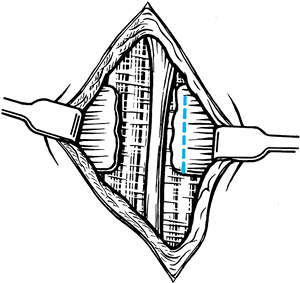 Figure 50.17. Formation of a distally based “ligament” that is 5 mm in diameter.
Figure 50.17. Formation of a distally based “ligament” that is 5 mm in diameter.![]() Figure 50.18. A new transverse carpal ligament is sutured to the old ligamentous stump on the opposite side of the carpal tunnel.
Figure 50.18. A new transverse carpal ligament is sutured to the old ligamentous stump on the opposite side of the carpal tunnel.
and that of the flexor carpi ulnaris occur independently and are
usually related to repetitive flexion, direct trauma, wrist fracture,
cysts, or excessive wrist extension (28). Calcifications may exist within the tenosynovium (Fig. 50.19).
Rheumatic, metabolic, infectious, and neoplastic diseases may also
involve these tendons. Inflammation of the flexor carpi radialis tendon
occurs in its fibroosseous tunnel within the transverse carpal ligament
(28). The flexor carpi ulnaris tendon may become inflamed just proximal to the pisiform (77).
The latter may also be involved in an arthritic process at its
articulation with the triquetrum. Ulnar neuritis at Guyon’s canal may
be secondary to flexor carpi ulnaris tendinitis (77).
 |
|
Figure 50.19. Calcification of a portion of the tenosynovium of the flexor carpi ulnaris tendon.
|
splinting in neutral flexion, administration of oral antiinflammatory
drugs, and local application of ice.
-
Decompress the flexor carpi radialis
tendon using a 4 cm zigzag incision that begins at the tuberosity of
the scaphoid and extends proximally. -
Repair or Z-lengthen a contracted flexor carpi radialis tendon.
-
Close the skin with interrupted sutures and apply a dorsal splint in 20° flexion, which the patient must wear for 2 weeks.
-
Advise the patient to begin active exercises after the sutures are removed.
-
For surgical treatment of chronic flexor carpi ulnaris tendinitis, use a palmar-ulnar zigzag incision (Fig. 50.20).
![]() Figure 50.20. The incision used to expose Guyon’s canal and the distal portion of the flexor carpi ulnaris tendon.
Figure 50.20. The incision used to expose Guyon’s canal and the distal portion of the flexor carpi ulnaris tendon. -
When signs of ulnar nerve compression are
present, section the palmar fascia and the origin of the abductor
digiti minimi muscle; also divide the pisohamate ligament,
decompressing Guyon’s canal (Fig. 50.21).
Protect the ulnar nerve and artery proximally and distally, and
preserve the pisiform metacarpal ligaments. When pisotriquetral
arthritis is present, enucleate the pisiform subperiosteally from its
capsule through a palmar longitudinal incision (Fig. 50.22, Fig. 50.23) (77).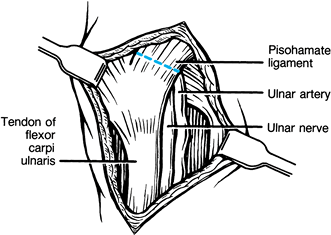 Figure 50.21. Incision of the pisohamate ligament.
Figure 50.21. Incision of the pisohamate ligament.![]() Figure 50.22. Incision of the capsule of the pisiform.
Figure 50.22. Incision of the capsule of the pisiform.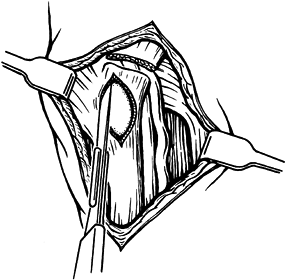 Figure 50.23. Removal of the pisiform.
Figure 50.23. Removal of the pisiform. -
Just proximal to the pisiform, perform a Z-plasty of the flexor carpi ulnaris tendon to allow 5 mm of tendon lengthening (Fig. 50.24, Fig. 50.25) (77). Suture the capsule of the pisiform closed.
![]() Figure 50.24. Incision used to Z-lengthen the flexor carpi ulnaris tendon, with subsequent closure of the capsule of the pisiform.
Figure 50.24. Incision used to Z-lengthen the flexor carpi ulnaris tendon, with subsequent closure of the capsule of the pisiform.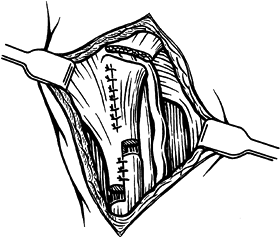 Figure 50.25. Lengthening of the flexor carpi ulnaris tendon by 5 mm using a Z-plasty.
Figure 50.25. Lengthening of the flexor carpi ulnaris tendon by 5 mm using a Z-plasty. -
After the tourniquet is released and
hemostasis is achieved, close the skin. Immobilize the wrist for 2
weeks in a dorsal splint in 20° of palmar flexion until the sutures are
removed.
carefully protected in the radial wrist exposure. The ulnar nerve and
artery are in proximity to the flexor carpi ulnaris and can be injured
by laceration or too-vigorous traction. The pisiform metacarpal
ligament should be kept intact to avoid weakening wrist flexion in a
palmar-ulnar direction.
occur over the dorsum of the wrist, distal to and including the
extensor retinaculum. Extension of the fingers causes heaping of the
tenosynovium at the distal margin of the extensor retinaculum (Fig. 50.26). It is usually attributable to repetitive extension of the fingers and wrist or to direct trauma (9,10,64).
 |
|
Figure 50.26. Heaping up of the extensor tenosynovium distal to the extensor retinaculum during finger extension.
|
tumors, fungus, congenital dysplasias, and typical or atypical
bacterial infections may also cause symptomatic extensor tenosynovitis
of the wrist (4,5,10,39,41,50,57,58,62,63,67,78,83,97).
Palmar splinting of the wrist in 20° extension, local application of
ice, and dorsal administration of antiinflammatory drugs are usually
successful
in
treating the condition. Local injections of steroids around the
inflamed tenosynovium or extensor tenosynovectomy may be necessary in
severe cases.
is caused by repetitive flexion and extension of the thumb with ulnar
and radial deviation of the wrist. Treatment includes splinting,
application of ice, and oral administration of nonsteroidal
antiinflammatory drugs. Local instillation of steroid preparations or
surgery is occasionally warranted.
-
After administering regional or general
anesthesia, make an oblique incision from the base of the second
metacarpal to the metaphysis of the distal ulna (Fig. 50.27).
Identify and protect the sensory branches of the radial and ulnar
nerves. If possible, retract rather than transect large veins while
exposing the tendons in the distal part of the wound (Fig. 50.28).![]() Figure 50.27. The incision used to expose the extensor retinaculum.
Figure 50.27. The incision used to expose the extensor retinaculum. Figure 50.28. Tenosynovitis of the extensors at the wrist
Figure 50.28. Tenosynovitis of the extensors at the wrist -
Incise the extensor retinaculum at the
septum between the first and second dorsal compartments. Preserve the
proximal 20% of the extensor retinaculum to prevent bow-stringing of
the extensor tendons, and raise the extensor retinaculum as an
ulnar-based flap until the sixth compartment is decompressed (Fig. 50.29). Remove Lister’s tubercule using a rongeur.![]() Figure 50.29. The extensor retinaculum is raised as an ulnar-based flap.
Figure 50.29. The extensor retinaculum is raised as an ulnar-based flap. -
Excise the tenosynovium from all of the finger and wrist extensors (Fig. 50.30).
Pass the flap of extensor retinaculum deep to the finger and wrist
extensor, and sew it back to adjacent soft tissues in the area of the
first dorsal compartment of the wrist (Fig. 50.31).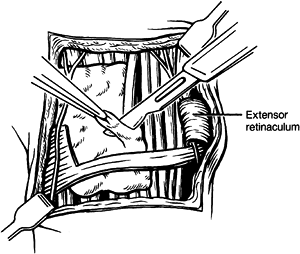 Figure 50.30. Extensor tenosynovectomy.
Figure 50.30. Extensor tenosynovectomy.![]() Figure 50.31.
Figure 50.31.
The extensor retinacular flap is laid deep to the extensor tendons and
sewn to the roof of the first dorsal compartment and to the adjacent
wrist capsule. -
After the tourniquet is released and
hemostasis is achieved, close the wound. Drainage may be continued for
2 days, if necessary. Have the patient wear a 20° dorsiflexed palmar
splint until the skin sutures are removed; then begin gentle active
range-of-motion exercise. -
Treat isolated tenosynovitis of the
extensor pollicis longus by incising the third dorsal compartment and
by removing Lister’s tubercle. Do this through a 2 cm transverse
incision extending in an ulnar direction from Lister’s tubercle. -
Protect the sensory branches of the radial nerve.
-
Transpose the extensor pollicis longus
tendon radially, away from Lister’s tubercle, which has been removed.
Suture the tendon sheath closed, and then close the skin. Have the
patient wear a palmar splint for 2 weeks until the skin sutures are
removed.
dorsal cutaneous branch of the ulnar nerve can be lacerated during
surgery; take care to avoid them, and repair them if injured. The
extensor pollicis longus tendon can also be lacerated as it crosses the
radial wrist extensors obliquely. Immediate tenorrhaphy is necessary.
differentiated from de Quervain’s disease, as different points of
maximal tenderness are evident with palpation.
is caused by inflammation of the tenosynovium of the extensor carpi
radialis longus and brevis within the second dorsal extensor
compartment of the wrist (40). Pain and
swelling are elicited on palpation where the two wrist extensors cross
the abductor pollicis longus and extensor pollicis brevis (6,40,43,92).
The condition may be attributable to repetitive extension and flexion
of the wrist or to direct trauma. It is known as “bugaboo forearm” in
helicopter skiers (76).
20° extension, application of ice, administration of oral nonsteroidal
antiinflammatory agents, and local injections of steroid preparations.
Changing sports techniques and equipment is helpful. Surgery is
reserved for recalcitrant cases that are unresponsive to prolonged
conservative therapy, including steroid injections around the tendons
just proximal to the extensor retinaculum.
-
Using regional or general anesthesia,
make an ulnar-based chevron incision over the second dorsal
compartment, crossing the wrist creases diagonally. Protect the
branches of the radial nerve. -
Incise the second dorsal extensor
compartment and remove exuberant tenosynovium from the two radial wrist
extensors back to their junction with the tendons of the abductor
pollicis longus and extensor pollicis brevis (40).
Attempt to leave intact a portion of the distal extensor retinaculum.
Examine the tendons, and remove their tenosynovium. Achieve hemostasis
after the tourniquet is released. -
Close the skin and apply a palmar splint in 20° dorsiflexion. Remove skin sutures 2 weeks later, and discard the splint.
recurrent subluxation of the extensor carpi ulnaris tendon) may result
in painful tenosynovitis. This condition is usually attributable to a
single forceful or repetitive hypersupination motion of the wrist with
ulnar deviation (14). The infratendinous
retinaculum of the wrist is stretched or ruptured, allowing palmar
subluxation of the extensor carpi ulnaris tendon (14,35).
Conservative management consists of splint immobilization in a
dorsiflexed position, pronation, and radial deviation of the wrist.
Administration of oral antiinflammatory agents and local injection of
steroids may alleviate symptoms. Surgical reconstruction is indicated
in selected individuals in whom conservative therapy fails to resolve
symptoms (20).
-
After administration of general or
regional anesthesia, pronate the wrist and make a hockey-stick incision
from the base of the fifth metacarpal; extend it 2 cm radially and 4 cm
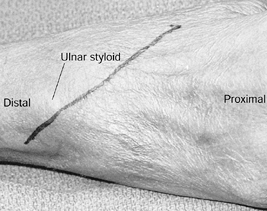
proximally (Fig. 50.32). Protect the sensory
branches of the ulnar nerve as they cross the distal portion of the
wound. Expose the supratendinous portion of the retinaculum, and
identify the sixth dorsal extensor compartment.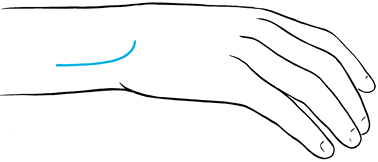 Figure 50.32. Incision to reconstruct the sixth dorsal compartment of the wrist.
Figure 50.32. Incision to reconstruct the sixth dorsal compartment of the wrist. -
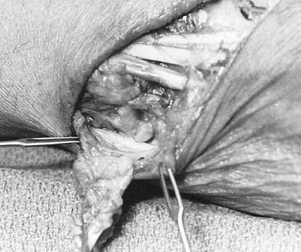
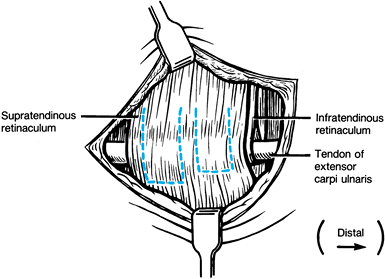
Make a radially based flap about 1 cm
wide and about 5 mm proximal to the distal margin of the retinaculum
through the supratendinous extensor retinaculum. Make the window palmar
enough to view the extensor carpi ulnaris tendon, which is subluxed
into the depths of the wound (Fig. 50.33) (11).![]() Figure 50.33. Preparation of the flaps in the supratendinous portion of the extensor retinaculum.
Figure 50.33. Preparation of the flaps in the supratendinous portion of the extensor retinaculum. -
Locate the stretched or torn
infratendinous retinaculum, which normally creates a medial wall
against palmar subluxation of the extensor carpi ulnaris tendon. -
After assessing the proper dorsal
replacement position for the extensor carpi ulnaris tendon, create a
second radially based flap, about 1 cm wide, from the proximal portion
of the extensor retinaculum. Make it long enough in a palmar-ulnar
direction to allow creation of a sling around the tendon of the
extensor carpi ulnaris (35).
P.1529
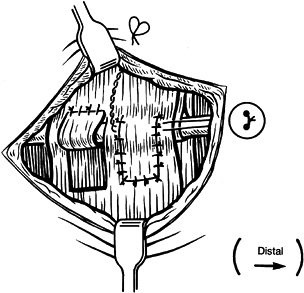
After the proximal flap has been wrapped around the extensor carpi
ulnaris tendon and sutured to itself with two horizontal mattress
sutures, repair the infratendinous retinacular leash around the same
tendon, using a pull-out wire suture (Fig. 50.34) (14).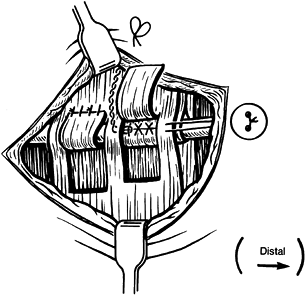 Figure 50.34. Creation of an extensor carpi ulnaris sling and repair of the infratendinous retinaculum using a pull-out wire technique.
Figure 50.34. Creation of an extensor carpi ulnaris sling and repair of the infratendinous retinaculum using a pull-out wire technique. -
If the septal tissues are irreparable,
use the distal flap portion of the extensor retinaculum as a free
fascial graft. A portion of the extensor carpi ulnaris tendon proximal
to the extensor retinaculum may also be used as a free graft (14). Close the retinaculum (Fig. 50.35).![]() Figure 50.35. Closure of the retinacular window and placement of the pull-out wire.
Figure 50.35. Closure of the retinacular window and placement of the pull-out wire. -
After the tourniquet is released, achieve
hemostasis and close the skin. Place the extremity in a long-arm splint
for 6 weeks with the wrist dorsiflexed at 25° with the forearm in
neutral rotation. Remove the splint and encourage the patient to engage
in active motion of increasing intensity over the next 6 weeks.
lacerated; if it is, repair it microscopically. Use a free graft to
repair a deficient infratendinous retinaculum, because swinging a
fascial flap toward the deficient medial wall may tether wrist rotation.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
M, Riordan D. Trigger Finger, Carpal Tunnel Syndrome and de Quervain’s
Disease: Tardive Manifestation of Deficient Connective Tissue (1993,
unpublished data).
M, Riordan D. The Association of Trigger Finger, Carpal Tunnel Syndrome
and de Quervain’s Disease with Dupuytren’s Disease (1993, unpublished
data).