Anterior Glenohumeral Instability: Treatment of Acute Injury
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 33 – Anterior Glenohumeral Instability:
Treatment of Acute Injury
the most common traumatic dislocations in the human body. The soft
tissues to the glenohumeral joint must be disrupted for the humeral
head to escape the glenoid fossa. The most important factor determining
the location of tissue disruption is the age of the patient. In
patients older than 40 years of age, the posterior mechanism of
dislocation is common. This involves a tear in the rotator cuff with or
without labral tissue involvement. In patients younger than 40 years of
age, the predominant tissue injury is a tear of the anterior inferior
glenoid labrum (Bankart tear). A study delineating the arthroscopic
findings after initial traumatic anterior dislocation in patients
younger than 24 years of age revealed that 61 of 63 patients (97%)
sustained an avulsion of the anterior inferior glenoid labrum. Fourteen
of the 63 patients (22%) had an associated osseous lesion of the
glenoid rim. The most important risk for recurrence after initial
dislocation may be the underlying pathologic tissue disruption. An
arthroscopic study of 45 patients who sustained an initial traumatic
dislocation showed that most had Bankart tears. Moreover, these
patients also were found to have gross instability on examination under
anesthesia. Six of the 45 patients who did not have labral pathology
were found to be stable on examination under anesthesia.
after first-time traumatic anterior dislocation. The risk of recurrence
after initial dislocation has been reported as high as 95% for patients
younger than 20 years of age. For patients younger than 25 years of
age, the recurrence rate has been reported as high as 50% to 75%. After
the age of 25 years, the risk of recurrence has been shown to rapidly
decrease. Despite the varying rates of recurrence that have been
reported, studies have clearly demonstrated that the risk of recurrence
after initial traumatic anterior dislocation is extremely high. This
risk is inversely related to the age of the patient at the time of
initial dislocation. Therefore, treatment should be based on the age of
the patient.
normally a straightforward process. The patient’s history most often
presents a mechanism of an eccentrically applied load to the hand while
the arm is outstretched. At presentation, the patient typically appears
as leaning forward with the humerus in slight abduction, flexion, and
internal rotation. Usually, the humeral head is palpable anteriorly
with a concomitant hollowing and visible deficiency posteriorly under
the acromion. Patients may present after the dislocation has
spontaneously reduced, in which case the diagnosis may not be evident.
The mechanism of injury, history of a “dead arm” event, and reported
information of a pop at the time of injury or pain that was relieved
after a pop often represent key clues toward diagnosis.
examination. The more common neurapraxias can be ruled out with
resistance testing of the posterior and middle deltoids and biceps.
Pulses, warmth, and capillary refill should be compared with the
unaffected extremity. Symmetry, however, does not necessarily exclude
axillary artery injury. In the case of a spontaneously reduced
dislocation, the patient will present with prominent guarding against
combined abduction and external rotation.
of a single oblique view, has often been completed prior to orthopaedic
consultation. This view can adequately rule out fractures about the
humeral head and neck that may prevent closed reduction. If additional
injuries are not present, the surgeon should reduce the shoulder prior
to ordering further radiographs. In the event radiographs cannot be
taken at the time of presentation, such as in the event of an on-field
injury, a gentle attempt at reduction is warranted.
literature. These include the hippocratic technique, the Stimson
technique, and the Milch technique. The hippocratic technique involves
using countertraction either with the surgeon’s foot across the
axillary folds against the chest wall or with a sheet pulling
countertraction from across the patient’s body in a cephalad direction
by an assistant. Simultaneously, axial traction is applied to the
affected shoulder. Internal and external rotation of the humeral head
will help reduce the glenohumeral joint. The Stimson technique involves
placing the patient prone with approximately 5 pounds of axial traction
strapped at the wrist. With the Milch technique, an abduction and
external rotation maneuver with concomitant gentle pressure on the
humeral head with the thumb enables reduction on the supine patient.
Perhaps more important than any particular method of reduction is to
ensure that the patient is adequately relaxed and that adequate
analgesia has been provided. Intravenous sedatives and anxiolytics are
often helpful. Several authors have reported the successful use of
intra-articular lidocaine for anesthetic. The glenohumeral joint can be
easily penetrated posteriorly with an 18-gauge spinal needle.
Aspiration of hemarthrosis verifies joint penetration. Fifteen to 20 mL
of 1% lidocaine will provide adequate analgesia for the patient to
cooperate with reduction efforts. Regardless of the maneuver used,
successful reduction is confirmed with the restoration of normal
humeroscapular relationships and smooth glenohumeral rotation. Patients
generally experience dramatic pain relief after reduction. A thorough
postreduction neurovascular exam must be performed.
postreduction patient can readily tolerate a more thorough radiographic
evaluation. Radiographs generally include a true glenohumeral anterior
posterior (AP) in internal and external rotation and an axillary
lateral. A true shoulder AP view is an x-ray view taken in the plane of
the scapula (at approximately 30 to 40 degrees). Internal and external
rotation views provide information regarding humeral head and
tuberosity injuries. An axillary view confirms reduction of the
glenohumeral joint and aids in the diagnosis of tuberosity fractures
and Hill-Sachs lesions.
include a true axillary view, which involves placing the arm in 70 to
90 degrees of abduction and then directing the x-ray beam superiorly
through the axilla. A safer, less traumatic axillary technique involves
elevating the arm in the plane of the scapula. This modification tends
to prevent the humeral head from being placed into a vulnerable
position. Other axillary images include the West Point view. In this
technique, the patient is placed prone with the shoulders raised
approximately 7 cm off the x-ray table. With the head and neck turned
away, the x-ray beam is directed 25 degrees inferior from the
horizontal and 25 degrees medial. The Velpeau view places the patient
standing and leaning backward over the radiographic cassette. The x-ray
beam is then directed vertically downward.
oblique (Garth) view should be obtained. This radiographic technique
places the scapula flat against the x-ray cassette similar to a true AP
view. The x-ray beam is then directed in a 45-degree caudad direction.
head defects in addition to the internal and external AP views include
the tangential view, the Hill-Sachs view, and the Stryker-Notch view.
The tangential and Hill-Sachs views involve AP x-rays in increasing
degrees of internal rotation. The Stryker-Notch view is taken with the
patient in the supine position with the affected hand placed on the
head. The x-ray beam is then directed 10 degrees in a cephalad
direction.
may be required to assist in patient and extremity positioning.
Obtaining high-quality postreduction radiographs, however, will provide
critical information that will aid the orthopaedic surgeon in
formulating the proper treatment algorithm for the patient.
of an osseous Bankart lesion that involves >25% to 30% of the
glenoid width, further evaluation with CT imaging with
three-dimensional reconstructions is required. A recent study
quantitatively demonstrated that CT imaging was superior to plain
radiographs in assessing the size of a bony defect of the glenoid.
 |
|
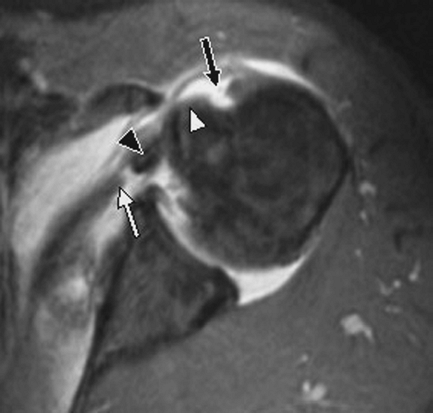
Figure 33-1 MRI of subscapularis tear.
|
specific use in the evaluation of acute anterior glenohumeral
dislocations. An MRI should be obtained when examination in the
subacute postdislocation period yields evidence of a rotator cuff tear,
particularly a subscapularis rupture (Fig. 33-1). A prospective study analyzing the accuracy of subacute MRI scans to identify labral tears in
patients with first-time traumatic dislocations showed only a 70%
correlation with arthroscopically confirmed labral tears. Another
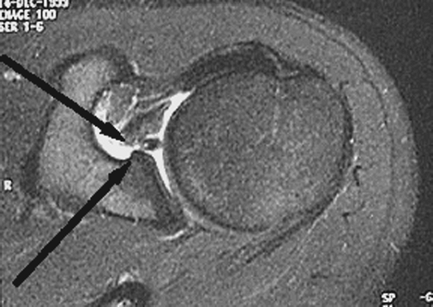
prospective study examining the accuracy of MRI arthrography to
identify labral pathology in patients with traumatic anterior
instability showed a specificity of 98% (Fig. 33-2).
 |
|
Figure 33-2 MRI of an anterior labral tear.
|
weakness without other clinical evidence of rotator cuff tear,
electromyographic studies are indicated.
for postreduction immobilization. A sling with strap padding is often
better tolerated than a shoulder immobilizer. Patients are encouraged
to wear the sling during sleep to protect the shoulder during this
initial period. In addition, patients are encouraged to remove the
sling to exercise the elbow, wrist, and digits frequently. The duration
of immobilization has typically been continued for ≤3 weeks, but
absolutely no longer. Investigators have demonstrated that the length
of immobilization has had no effect on the rates of recurrent
dislocation. Alternatively, recent studies have suggested that the
position of immobilization may affect the healing potential of labral
lesions, thereby potentially affecting the redislocation rates for
first-time dislocators. In a recent study, 19 traumatic anterior
dislocations with Bankart tears were evaluated with MRI scans with the
shoulders placed in both external and internal rotation. Findings
included decreased separation and displacement of the labrum from the
glenoid when the arm was in external rotation compared with when it was
in internal rotation. A follow-up study of 40 patients with acute
traumatic anterior dislocations was recently conducted. The patients
were equally randomized to immobilization in sling and swathe in
internal rotation or in a prefabricated splint in external rotation for
3 weeks. Results showed that none of the 20 patients immobilized in
external rotation had a recurrent anterior dislocation at a mean
15-month follow-up. Whether immobilization in external rotation
prevents long-term recurrence rates still remains to be seen.
after dislocation. Re-evaluation should be during the first week of
index dislocation. A prospective study of 538 first-time traumatic
anterior dislocation patients showed a redislocation rate of 3.2%
within the first week after original dislocation. Factors associated
with increased risk for redislocation included neurologic deficit,
associated large rotator cuff tears, and associated glenoid rim
fractures with or without fractures of the greater tuberosity.
demonstrate appreciable tightening of the shoulder, especially with
external rotation in the unelevated position. External rotation that is
greater than the unaffected side suggests a possible subscapularis
rupture. Rotator cuff function should be assessed, particularly in
patients older than 40 years of age as several studies have
demonstrated the increased incidence of rotator cuff tears in this age
group. Focused attention should be placed on examination of the
subscapularis in all age groups. The lumbar lift-off test as described
by Gerber has been shown to accurately predict subscapularis integrity
and function. This test can usually be performed at the 3-week
postdislocation assessment. An examination that reveals evidence of a
rotator cuff tear mandates further evaluation with an MRI.
stretching program at 3 weeks postdislocation. Exercises consist of
gentle forward elevation and external rotation, with an external
rotation limit of 40 degrees. An over-door pulley may be used for
assistance in regaining forward elevation. Next, a scapular
strengthening and postural program are used. Pendulum exercises are
avoided as they promote poor scapular mechanics and increase
anteroinferior translation of the humeral head. Formal, supervised
therapy is instituted during the sixth week postdislocation. Passive
stretching is used to correct any residual contractures. The mainstays
of treatment at this stage are rotator cuff and scapular strengthening.
Devices that promote normal humeroscapular rhythm are implemented: the
body blade, pulleys, and upper body ergometers. Athletes generally can
return to their sport midseason. Harnesses and prophylactic taping may
provide proprioceptive feedback against extreme abduction and external
rotation. At 12 weeks postdislocation, sport-specific exercises are
started. Plyometrics for athletes and work hardening for heavy laborers
may be necessary.
academies have demonstrated success rates of ≤75% after coordinated
therapy programs for first-time dislocators. It is unclear whether such
results could be reproduced in a more general population over a longer
period of time. One study demonstrated only a 16% decrease in
recurrence rates in patients treated with exercise therapy after
traumatic subluxation.
 |
|
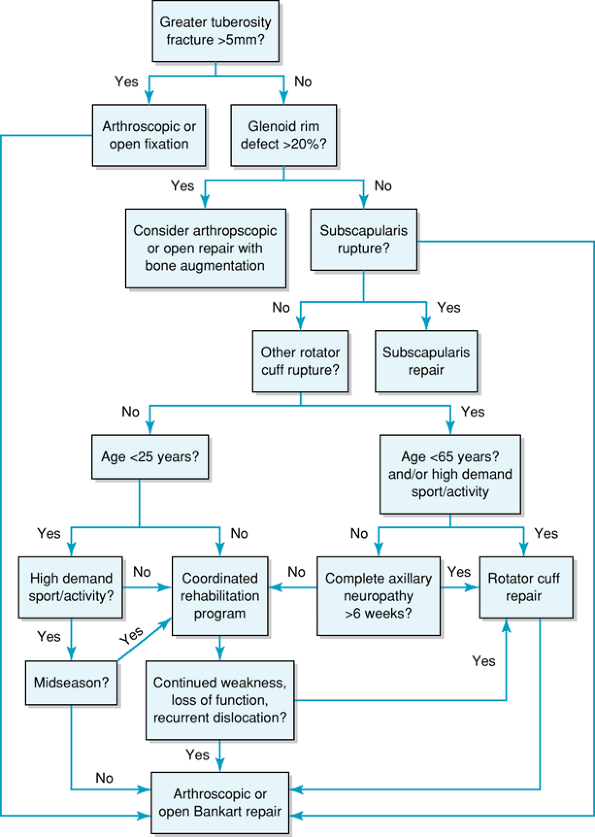
Figure 33-3 Algorithm for the management of first-time traumatic dislocations.
|
with initial dislocation has become more accepted with the advent of
more refined arthroscopic techniques and instrumentation.
Theoretically, these generally young patients have more clearly defined
pathology and healthier tissue, making them good candidates for
arthroscopic repair. In a prospective study comparing nonsurgical
management and arthroscopic repair in West Point military cadets with
initial dislocations, the recurrence rate was 80% in the nonsurgical
group and 14% in the surgical group. In another study comparing
randomized patients younger than 30 years of age with initial
dislocations, those treated with immobilization and rehabilitation had
a recurrence rate of 47% at 33 months compared with 15.9% in the group
treated with arthroscopic Bankart repair. Although repair techniques
vary among studies, most data suggest that arthroscopic Bankart repair
is most advantageous if done after the initial dislocation, before the
development of chronic pathologic changes associated with recurrent
instability.
should be based on current science. The surgeon’s algorithm must take
into account the patient’s age, activity level, and goals (Fig. 33-3).
Several key points must be recognized in formulating a treatment plan.
Tuberosity fractures displaced more than 5 mm require reduction and
fixation. In young patients, concomitant arthroscopic Bankart repair
should be strongly considered. Repair of traumatic subscapularis
rupture should be performed as soon as possible to avoid
musculotendinous retraction and scarring, regardless of age. Glenoid
rim fractures equaling >20% of the intact glenoid width will often
require bone augmentation in addition to a Bankart repair. For patients
who lead an active lifestyle or are involved in a high-demand
occupation and who have sustained a full-thickness rotator cuff tear
from a dislocation, surgical treatment should involve both a rotator
cuff repair and Bankart repair, if present. For the older patient with
a large full-thickness rotator cuff tear and axillary neuropathy,
rotator cuff repair should be considered if deltoid function does not
return in 6 to 12 weeks postdislocation. For competitive athletes
younger than 25 years of age, arthroscopic Bankart repair should be
considered in the off season. For any patient younger than 25 years of
age with a first-time dislocation, the benefits and risks of early
arthroscopic Bankart repair should be discussed and offered as a
reasonable option.
the technique of choice for collision and contact athletes. A recent
study demonstrated excellent long-term results in American football
players treated with open Bankart repair. No patient had recurrent
dislocations postoperatively, and only 2 of 58 had recurrent
subluxation. In another study involving 194 patients with
arthroscopically repaired Bankart lesions, 101 of whom were contact
athletes, a recurrence rate of only 6.5% was present in patients
without associated bone defects. In contrast, a recurrence rate of 87%
was reported for those patients with marked bone loss.
a few absolute indications for open surgical repair in first-time
dislocators. These include substantial humeral and/or glenoid bone
loss, or irreparable rotator cuff deficiency, particularly those of the
subscapularis. Relative contraindications to arthroscopic repair
include humeral avulsions of the glenohumeral ligaments and capsular
ruptures. In general, however, arthroscopic Bankart repair is probably
indicated for first-time dislocations as there has never been any
significant difference demonstrated in the surgical ease or outcome
between early and late open Bankart repair.
RA, Wheeler JH, Ryan JB, et al. Arthroscopic Bankart repair versus
non-operative treatment for acute, initial anterior shoulder
dislocations. Am J Sports Med. 1994;22:589–594.
SS, De Beer JF. Traumatic glenohumeral bone defects and their
relationship to failure of arthroscopic Bankart repairs: significance
of the inverted-pear glenoid and the humeral engaging Hill-Sachs
lesion. Arthroscopy. 2000;16:677–694.
E, Lee S, et al. Quantitative assessment of classic anteroinferior bony
Bankart lesions by radiography and computed tomography. Am J Sports Med. 2003;31(1):112–118.
C, Kelly M, Wakefield AB, et al. Redislocation of the shoulder during
the first six weeks after a primary anterior dislocation: Risk factors
and results of treatment. J Bone Joint Surg Am. 2002; 84:1552–1559.
