Radiology and Imaging
Editors: Tornetta, Paul; Einhorn, Thomas A.; Cramer, Kathryn E.; Scherl, Susan A.
Title: Pediatrics, 1st Edition
Copyright ©2004 Lippincott Williams & Wilkins
> Table of Contents > Section III: – Specialty Clinics > 32 – Radiology and Imaging
32
Radiology and Imaging
Evan Geller
Barbara J. Wolfson
Children are not small adults, and nowhere is this
statement more apparent than in the bones. A child’s skeletal system is
constantly growing and remodeling. The choice of imaging modality to
evaluate the pediatric skeleton is influenced by a child’s age, site of
clinical concern, and the type of information needed. The femoral head
of an infant, for example, is entirely cartilaginous and therefore
cannot be visualized on plain radiography. It is best examined by
ultrasound, a modality that is capable of imaging cartilage while
providing the additional benefit of a dynamic evaluation of hip
stability. After the head ossifies (between 4 and 6 months of age),
plain radiography is preferred.
statement more apparent than in the bones. A child’s skeletal system is
constantly growing and remodeling. The choice of imaging modality to
evaluate the pediatric skeleton is influenced by a child’s age, site of
clinical concern, and the type of information needed. The femoral head
of an infant, for example, is entirely cartilaginous and therefore
cannot be visualized on plain radiography. It is best examined by
ultrasound, a modality that is capable of imaging cartilage while
providing the additional benefit of a dynamic evaluation of hip
stability. After the head ossifies (between 4 and 6 months of age),
plain radiography is preferred.
Imaging plays a major role in the diagnosis and
management of orthopaedic diseases. The mainstay remains plain
radiography but in recent years other imaging modalities such as
computed tomography (CT), magnetic resonance imaging (MRI), nuclear
medicine, and ultrasound have made significant contributions to
orthopaedic care. This chapter is intended to provide an introduction
and overview of the various available imaging modalities and to give
the orthopaedic resident some useful guidelines in choosing the most
appropriate modality. It is not intended as an exhaustive review of
imaging technology. It is good practice to remember that the
radiologist is the imaging expert and should be consulted when imaging
questions arise. It is difficult enough for a radiologist to stay
current with all the new modalities and applications and a busy
orthopaedist caring for patients cannot possibly know as much about
imaging as the radiologist.
management of orthopaedic diseases. The mainstay remains plain
radiography but in recent years other imaging modalities such as
computed tomography (CT), magnetic resonance imaging (MRI), nuclear
medicine, and ultrasound have made significant contributions to
orthopaedic care. This chapter is intended to provide an introduction
and overview of the various available imaging modalities and to give
the orthopaedic resident some useful guidelines in choosing the most
appropriate modality. It is not intended as an exhaustive review of
imaging technology. It is good practice to remember that the
radiologist is the imaging expert and should be consulted when imaging
questions arise. It is difficult enough for a radiologist to stay
current with all the new modalities and applications and a busy
orthopaedist caring for patients cannot possibly know as much about
imaging as the radiologist.
IMAGING METHODS
Plain Radiography
Since its discovery in 1895, radiography has been known
to be an excellent modality for the visualization of bones. For decades
it was the only imaging modality available and many important
observations about trauma, tumor, dysplasia, and metabolic bone disease
were made by radiology pioneers.
to be an excellent modality for the visualization of bones. For decades
it was the only imaging modality available and many important
observations about trauma, tumor, dysplasia, and metabolic bone disease
were made by radiology pioneers.
-
Plain radiographs, or conventional
x-rays, provide information about the bony skeleton and, to a more
limited extent, the joint spaces and soft tissues. -
X-rays are generated by bombarding a tungsten target with an electron beam.
-
□ As x-rays pass through a body part, they are absorbed to varying degrees prior to striking a fluorescent film-screen system.
-
□ It is this differential absorption of
x-ray photons that accounts for the differences in the appearance of
bone and soft tissue structure. -
□ Film technique differences (e.g., KvP and mAs) can be changed to highlight either bone or soft tissue.
-
-
There are five basic radiographic densities seen on plain film.
-
□ From most lucent to most dense these are air, fat, soft tissue (water), bone (calcium), and metal (Fig. 32-1).
-
□ Evaluating the density of a structure can help in formulating a differential diagnosis.
-
 |
|
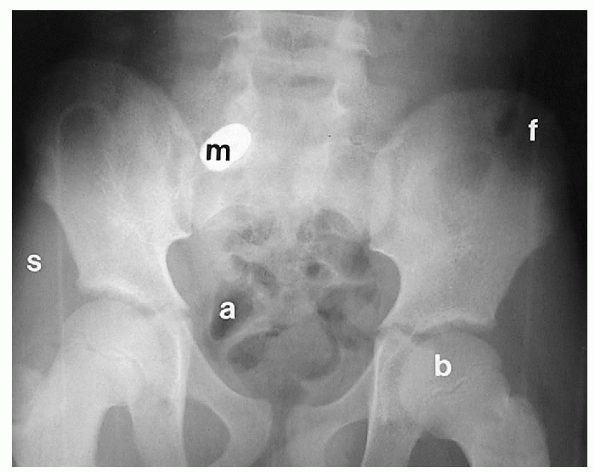
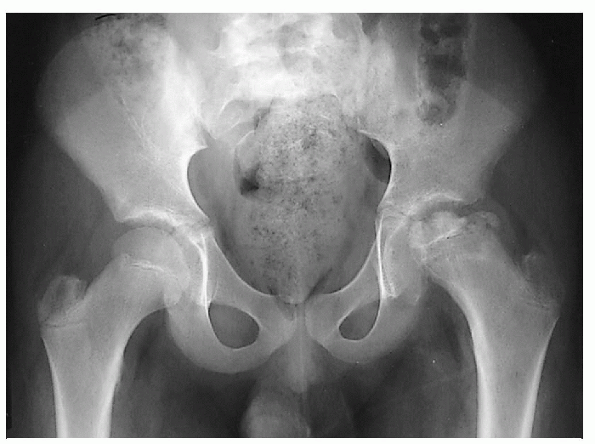
Figure 32-1 Plain radiograph of the pelvis demonstrates the five basic radiographic densities: a, air (in bowel); f, fat (properitoneal fat stripe); s, soft tissue (muscle); b, bone (femur); m, metal (bullet).
|
P.345
Computed Tomography
-
CT is a modality that uses x-rays to look at the body in slices.
-
□ A series of thin x-ray beams pass through the body as the x-ray tube moves around the body.
-
□ Detectors placed on the opposite side of the patient receive the x-ray beam.
-
□ The computer then processes the information obtained and assigns a density to each pixel (or picture element).
-
-
Water has been arbitrarily assigned a value of zero.
-
□ Any substance that is of greater
density than water will exhibit a positive value and any substance of
lesser density (such as fat or air) will have a negative value. -
□ These densities are expressed in Hounsfield units, named for Sir Godfrey Hounsfield who was one of the pioneers of CT imaging.
-
-
CT has the capability of distinguishing differences of density that cannot be distinguished by plain radiography.
-
Images are acquired in the axial plane,
but modern helical and multidetector scanners can reconstruct the image
in multiple planes, which can be useful when evaluating skeletal
abnormalities in children (Fig. 32-2). -
Advantages of CT include excellent resolution of bony structures and a fast acquisition time, minimizing the need for sedation.
-
Disadvantages of CT imaging include a high radiation dose, high cost, and limited soft tissue delineation.
 |
|
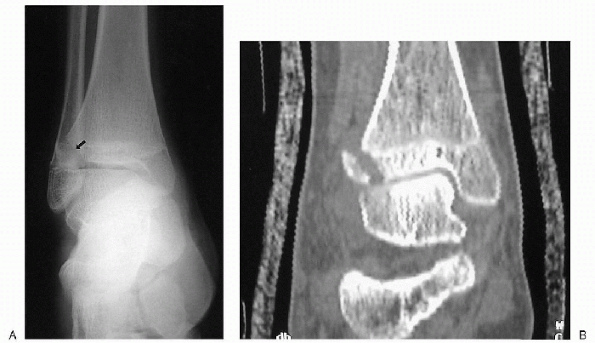
Figure 32-2 Tibial fracture seen better on computed tomography (CT) with three-dimensional reconstruction than on plain film. (A) Plain film showing the fracture fragment hidden behind the fibula. (B)
CT with reconstruction in the coronal plane showing the fracture clearly. Note that there is an overlying cast but the cast does not interfere with CT imaging. |
Magnetic Resonance Imaging
-
MRI uses magnets and radio waves to generate an image.
-
The routine MRI technique depends upon the mobile hydrogen concentration of tissues.
-
□ Cortical bone has a low mobile hydrogen content and is therefore virtually devoid of MRI signal.
-
□ MRI excels in the evaluation of bone marrow, cartilage, and soft tissues.
-
□ It has become the modality of choice in diseases involving these structures (Fig. 32-3).
-
-
Advantages of MRI over CT include a lack of ionizing radiation, and multiplanar capability.
-
Disadvantages include the need for
sedation in young children (because of the lengthy nature of the
study), high cost, and an inability to evaluate cortical bone.-
□ Because strong magnets are used,
patients with metal rods or plates, or patients with pacemakers may not
be suitable candidates for MRI.
-
Nuclear Medicine
-
Bone scintigraphy is performed by
administering a radioisotope intravenously followed by imaging of the
musculoskeletal compartment with a gamma camera.-
□ The most commonly used agents for bone
scintigraphy are the technetium-labeled phosphate analogs that become
incorporated into the bone.
-
-
Causes of abnormally increased isotope activity include increased blood flow and bone turnover.
-
Causes of abnormally diminished or absent
uptake include bone infarction, aggressive infection, or high
intracapsular pressures due to large joint effusions. -
A SPECT scan
(single photon emission computed tomography) differs from routine
two-dimensional planar images in that it allows improved image contrast
by removing overlying structures that may interfere with image
interpretation.-
□ As with conventional cross-sectional
imaging modalities such as CT and MRI, images are presented as “slices”
in axial, coronal and sagittal planes, or as a three-dimensional (3D)
rotating image. -
□ SPECT studies are especially useful in the evaluation of suspected vertebral or rib abnormalities.
-
 |
|
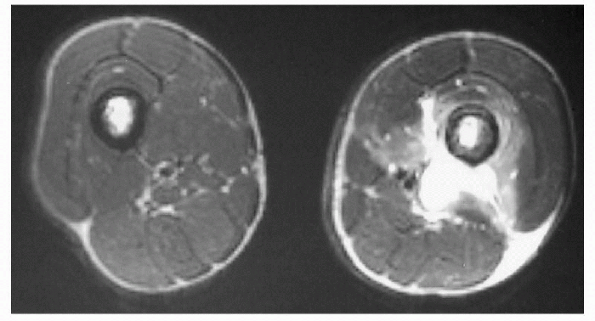
Figure 32-3
Pyomyositis of the left thigh. Magnetic resonance T2-weighted imaging of both thighs in the axial plane demonstrating location and extent of involvement in this 16-year-old boy with sickle cell disease. Note the high-signal intensity consistent with edema of the soft tissues. |
Ultrasound
-
Ultrasound technology was developed from “sonar” used by the U.S. Navy to detect submarines during World War II.
-
An ultrasound transducer is both a
transmitter and receiver of sound waves. It sends sound waves out, the
sound waves bounce off interfaces, and then return to the transducer.-
□ Ultrasound waves cannot go through air or bone.
-
□ Their natural medium is water and
therefore they are most useful when looking at fluid-filled structures
or structures with a high water content, such as cartilage.
-
-
Ultrasound is useful in assessing certain
cartilaginous structures such as the newborn hip and in identifying
joint effusions, fluid collections, and radiolucent foreign bodies in
soft tissue (Fig. 32-5).
Bone Densitometry
-
A DEXA scan (dual energy x-ray absorptiometry) is useful in the evaluation of bone mineral density and fracture risk assessment.
-
It uses low-dose x-rays to evaluate the whole body or selected regions including the lumbar spine or femoral neck.
-
It takes approximately 10 minutes to perform so sedation is rarely required.
-
In the pediatric age group, results are compared to agematched controls and are expressed as a “Z score.”
-
□ Greater than 2 standard deviations indicates increased risk for osteoporotic fractures.
-
P.347
 |
|
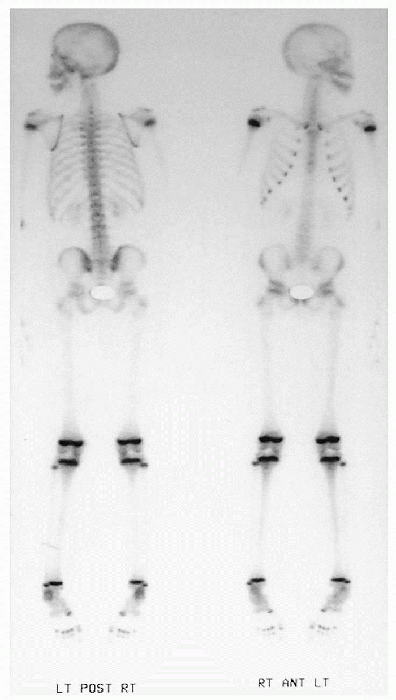
Figure 32-4
Normal radionuclide bone scan of the whole body. Note the increased uptake of isotope at the growth plates that can mask subtle abnormalities. |
 |
|
Figure 32-5 Ultrasound of the plantar surface of the foot demonstrating a wooden splinter (cursors).
This splinter could not be seen on plain film. Ultrasound guidance was used in the operating room to assist in removal of the foreign body. |
CHOICE OF IMAGING METHOD
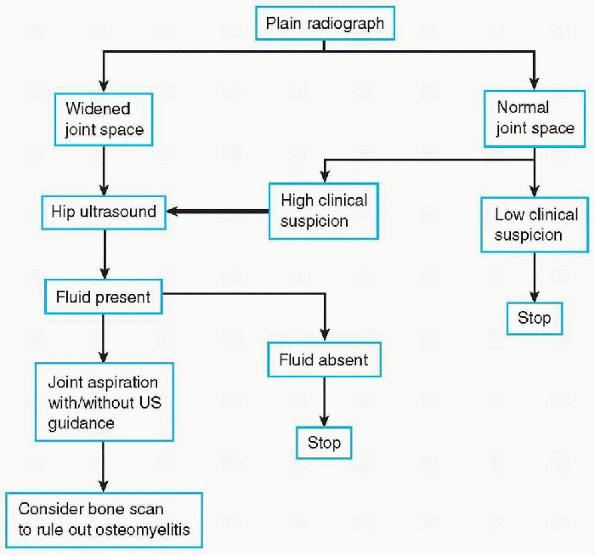
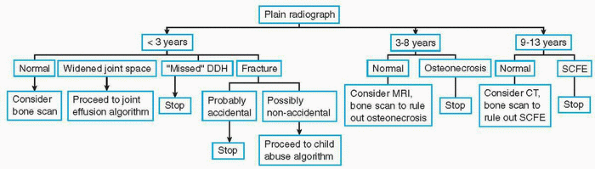
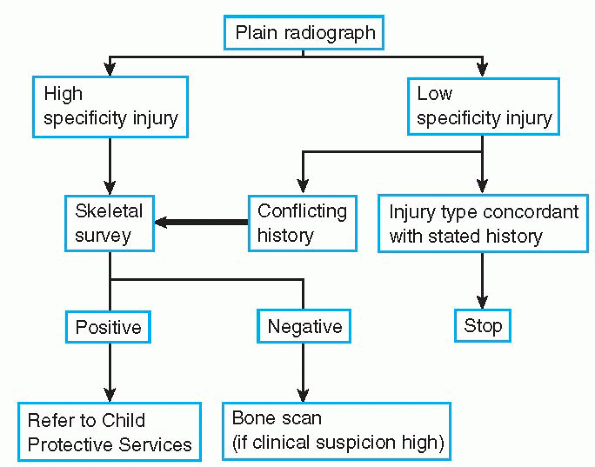
Diagnostic imaging algorithms have evolved with the development and refinement of imaging technology (Algorithms 32-1, 32-2 and 32-3).
MRI, multidetector CT, and SPECT imaging have revolutionized our
approach to certain musculoskeletal disorders and have added
considerably to diagnostic accuracy.
MRI, multidetector CT, and SPECT imaging have revolutionized our
approach to certain musculoskeletal disorders and have added
considerably to diagnostic accuracy.
 |
|
Algorithm 32-1 Workup of joint effusion.
|
Infection
-
The imaging workup of musculoskeletal infection begins with the plain radiograph.
-
□ Osteomyelitis will produce localized and deep soft tissue swelling within 48 to 72 hours.
-
□ This is followed by osteopenia, bone destruction (osteolysis), and periosteal reaction at 7 to 14 days (Fig. 32-6B).
-
□ Most cases of long-bone osteomyelitis
are metaphyseal in origin, but may spread to the epiphysis in young
infants and may involve the adjacent joint if the metaphysis is
intracapsular. -
□ Osteomyelitis limited to the epiphyses or epiphyseal equivalents (patella, greater trochanter) is less common but does occur.
-
-
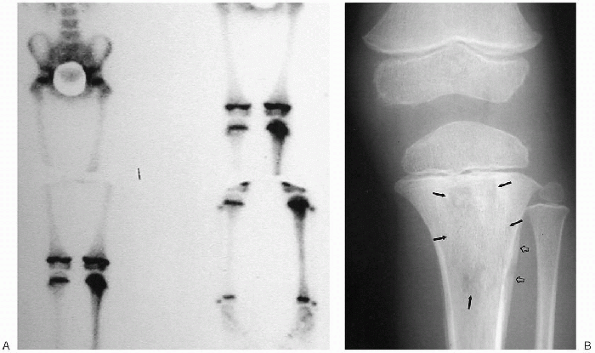
MRI and bone scintigraphy provide a much
more sensitive means of osteomyelitis detection, especially during the
first few days, when the radiograph may still be normal (see Fig. 32-6A).-
□ These studies often turn positive
within the first 24 hours of infection. MRI demonstrates altered signal
intensity consistent with marrow edema.
-
-
A “triple-phase” bone scan is the standard for scintigraphic imaging in infection.
-
□ The first phase is the “perfusion” or
“angiographic” phase that highlights the vascularity of a lesion and is
performed by rapid sequence imaging immediately following intravenously
administered isotope. -
□ The final or “delayed” phase of a
triple-phase bone scan is performed 2 to 3 hours after isotope
administration and reveals the patterns of isotope localization to the
cortical bone. -
□ The single, largest advantage of a triple-phase scan is its ability to differentiate cellulitis from osteomyelitis.
-
□ In cellulitis, there is increased activity on the two initial phases only (perfusion and blood pool).
-
□ In osteomyelitis, there is increased
activity on all three phases with localization of isotope to the
infected bone on the delayed phase. -
□ The differential diagnosis of increased uptake on all three phases includes acute trauma and vascular tumor.
-
□ Absence of uptake may indicate a very aggressive pattern of bone destruction with vascular compromise.
-
-
-
Scintigraphy is unreliable in the diagnosis of osteomyelitis in the neonatal period.
-
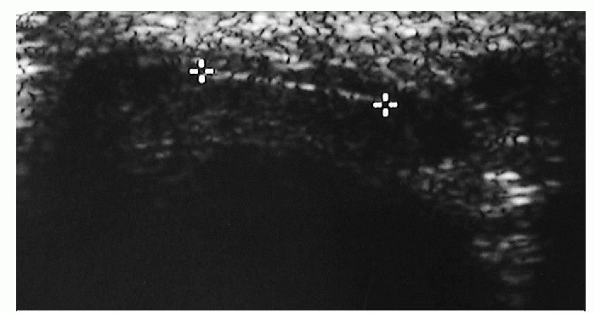
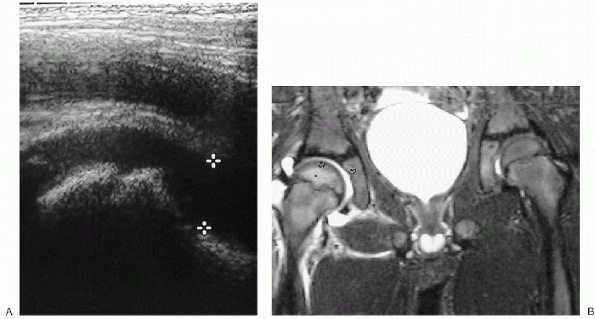
The most sensitive imaging modalities in the diagnosis of joint fluid is ultrasound or MRI (Fig. 32-7).
-
□ Ultrasound is the imaging modality of
choice in excluding a septic joint in that it offers the advantage of
speed and portability, as well as the ability for realtime-guided
needle aspiration of joint fluid. -
□ MRI may reveal an associated
osteomyelitis, if present, although similar information may be obtained
with bone scintigraphy following an initial ultrasound.
-
 |
|
Algorithm 32-2 Workup of hip pain or limp.
|
 |
|
Algorithm 32-3 Workup of suspected child abuse injuries.
|
Trauma
-
Plain radiography is the initial imaging
modality for all forms of musculoskeletal trauma, since it shows most
fractures and their manner of displacement or angulation.-
□ It will also demonstrate the
relationship of the fracture line to the growth plate (Salter-Harris
classification), a finding that may have prognostic significance.
-
-
CT with 3D reconstruction is useful in
defining the exact relationship of fracture fragments in complex
injuries and provides a roadmap for surgical reduction (Fig. 32-2). -
MRI may be useful in evaluating osteocartilaginous injury.Nonaccidental injury deserves special mention.
-
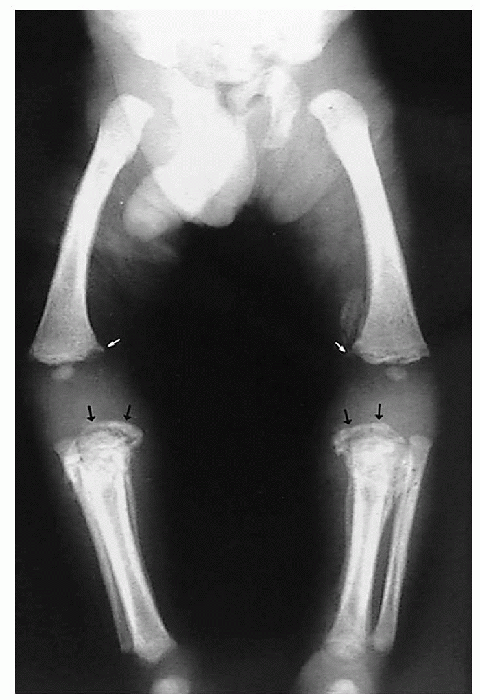
The evaluation of a physically abused child includes diagnostic imaging.
-
A skeletal survey is the modality of
choice in the imaging workup of nonaccidental injury and must be
performed correctly to maximize detection of injuries. -
A “babygram,” a single image of the entire skeleton, is not acceptable.
-
In our institution, a skeletal survey for
child abuse includes frontal and lateral views of the axial skeleton
and frontal views of the extremities. -
Lesions of high specificity include:
-
□ Fractures in different stages of healing
-
□ Metaphyseal “corner” or “bucket-handle” fractures (Fig. 32-8)
-
□ Posterior rib fractures
-
□ Fractures of bones that are difficult to fracture including the spinous processes, sternum, and scapulae (“three S’s”)
-
-
Bone scintigraphy has been used in the initial evaluation of nonaccidental injury.
-
□ Its strength lies in the discovery of old, near completely healed rib fractures.
-
□ The major limitation of bone
scintigraphy is its inability to recognize subtle metaphyseal injuries
in the presence of normal “hot” growth plates.
-
-
The use of both modalities is
complementary and should be considered in situations in which the
skeletal survey is normal despite a very high clinical suspicion or
when there is a paucity of radiographic findings in general. -
A follow-up skeletal survey is an alternative to performing a bone scan.
P.349
 |
|
Figure 32-6 Osteomyelitis of the proximal left tibia. (A) Bone scan showing increased isotope uptake within the metaphysis. Plain film at this time was normal. (B) Plain film obtained 2 weeks later reveals bone destruction (solid arrows) and periosteal new bone formation (open arrows).
|
 |
|
Figure 32-7 Hip effusion. (A)
Ultrasound. The capsule of the hip joint normally hugs the neck of the femur but when a joint effusion is present, the joint capsule is elevated away from the bone by the sonoluccent fluid (cursors). (B) Magnetic resonance T2-weighted imaging in another patient reveals a high signal-intensity fluid collection surrounding the right hip (arrows). Increased marrow signal (asterisk) is noted as well, consistent with edema. |
P.350
 |
|
Figure 32-8
Child abuse. Frontal views of both legs show fractures in different stages of healing. Bucket-handle fractures of the proximal tibiae (black arrows) and corner fractures of the distal femurs (white arrows). Periosteal new bone is noted along the tibial shafts. |
Developmental Dysplasia of the Hip
-
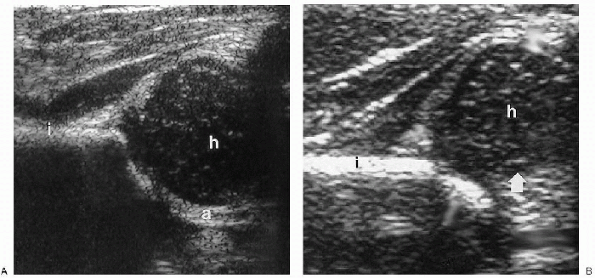
Ultrasound is recommended as the initial imaging modality in the diagnosis of developmental dysplasia of the hip (DDH).
-
□ Hip ultrasound may be used in the perinatal period and in early infancy until approximately 4 to 6 months of age.
-
□ Radiographic examination is recommended
thereafter as the appearance of ossific nuclei within the femoral
epiphyses limits further sonographic evaluation. -
□ The hips should not be evaluated by
ultrasound before 72 hours because of a high rate of false-positive
examinations owing to ligamentous laxity. -
□ Many radiologists prefer to wait until the child is between 2 to 4 weeks of age to perform the initial hip ultrasound.
-
□ Hip ultrasound, by the method of
Harcke, is a dynamic evaluation of the cartilaginous femoral epiphysis
and its relationship to the bony acetabulum.-
□ Provocative maneuvers (Ortolani, Barlow) are employed during the study to assess hip stability (Fig. 32-9).
-
□ A static hip ultrasound method, described by Graf, is more commonly used in Europe.
-
-
□ Ultrasound is also useful on follow-up examinations to assess proper placement of the hip in a Pavlik harness.
-
-
CT may be helpful in evaluating the position of the femoral heads after a spica cast has been applied.
Legg-Calvé-Perthes Disease
-
Idiopathic ischemic necrosis of the hips occurs between the ages of 4 and 8 years.
-
Radiographic evaluation is pursued initially with the hips examined in the neutral and frog-leg lateral projections.
-
□ Findings include increased density of
the femoral head, subchondral fissure, and with progression,
irregularity and flattening of the head with metaphyseal broadening,
trochanteric overgrowth, and metaphyseal cysts (Fig. 32-10). -
□ Lateral extrusion of the femoral head may occur as a complication.
-
□ These radiographic findings represent
subacute or late changes of osteonecrosis and, as in other causes of
osteonecrosis, MRI and bone scintigraphy are more sensitive in the
earliest period of symptoms.
-
-
MRI shows alteration in signal intensity within the femoral head.
-
Bone scintigraphy demonstrates photopenia within either a portion or the entire femoral head.
Slipped Capital Femoral Epiphysis
-
The diagnostic imaging workup of slipped
capital femoral epiphysis (SCFE) consists of radiographic evaluation of
the pelvis in the frontal neutral and frog-leg lateral projections.-
□ The frog-leg lateral radiograph is more sensitive than the neutral radiograph in the detection of an SCFE (Fig. 32-11).
-
-
Radiographs are used to follow these patients after surgical pinning.
-
□ Alterations in pin position,
chondrolysis, or osteonecrosis are complications to be excluded on
follow-up radiographic evaluation.
-
-
CT can also be used to evaluate a SCFE, although generally plain films suffice.
Skeletal Dysplasias
-
Plain radiography is the modality of choice in the evaluation of skeletal dysplasias.
-
The workup begins with a skeletal survey,
but frequently the findings evolve and repeat examinations may be
necessary as the child grows. -
Some common dysplasias such as
achondroplasia are easily recognized clinically and radiographically,
but skeletal dysplasias are frequently peculiar to a single family and
cannot be classified.
P.351
 |
|
Figure 32-9 Ultrasound of developmental dysplasia of the hip. (A) The coronal image of the normal hip shows that the femoral head is seated deeply within the acetabulum. (B) The coronal image of the dysplastic hip shows that the acetabulum is shallow and the femoral head is laterally displaced (arrow). h, cartilaginous femoral head; i, ileum; a, acetabulum.
|
 |
|
Figure 32-10
Legg-Calvé-Perthes disease. Plain radiograph reveals sclerosis and widening and irregularity of the left femoral head with shortening and broadening of the femoral neck. A widened joint space is also visible. |
 |
|
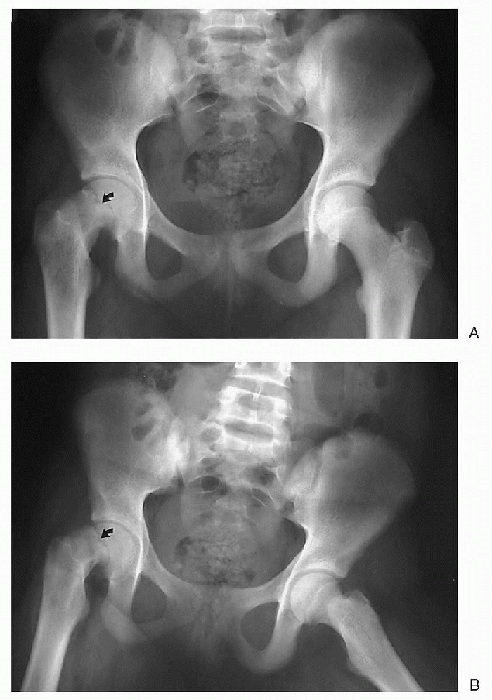
Figure 32-11 Slipped capital femoral epiphysis. (A) Frontal view. (B)
Frog-leg lateral view. The right femoral head has slipped medially on the frontal view and posteriorly on the frog-leg lateral view (arrows). A frog-leg lateral is a frontal view of the pelvis but a lateral view of the femur. |
P.352
 |
|
Figure 32-12
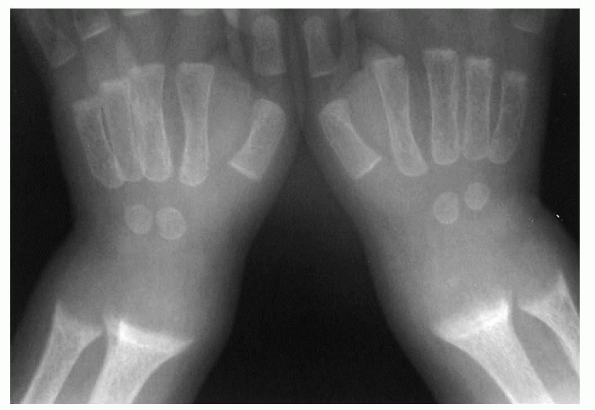
Rickets. The hallmark of rickets is loss of the zone of provisional calcification. Note also the cupping and the “paintbrush” appearance of the radial and ulnar metaphyses. |
Metabolic Bone Disease
-
Plain radiography is suitable for imaging of rachitic changes.
-
□ It is best to image the wrists or
knees, since these are the fastest growing and most metabolically
active regions of the appendicular skeleton. -
□ Findings include the following (Fig. 32-12):
-
□ Loss of the zone of provisional
calcification (ZPC) of the cartilaginous growth plate (white line
bordering the metaphysis; earliest finding) -
□ Metaphyseal fraying, cupping
-
□ Growth-plate widening (deposition of nonmineralized osteoid)
-
□ Bowing deformities
-
□ Rachitic rosary (bulbous overgrowth of costochondral junction)
-
-
SUGGESTED READING
Kleinman PK. Diagnostic imaging of child abuse, 2nd ed. St. Louis: Mosby, 1998.
Novelline RA. Squire’s fundamentals of radiology, 5th ed. Cambridge, MA: Harvard University Press, 1997.
Ogden JA. Skeletal injury in the child. Philadelphia: Lea & Febiger, 1982.
Resnick D. Diagnosis of bone and joint disorders, 3rd ed. Philadelphia: WB Saunders, 1995.
Silverman FN, Kuhn JP. Caffey’s pediatric x-ray diagnosis: an integrated imaging approach, 9th ed. St. Louis: Mosby, 1993.
Taybi H, Lachman RS. Radiology of syndromes, metabolic disorders, and skeletal dysplasias, 4th ed. St. Louis: Mosby, 1996.
