SPORTS MEDICINE
come from a variety of sources. The approach to diagnosis, and to
ultimately recommending a course of treatment, lies in four steps:
-
Have an appreciation of normal knee anatomy.
-
Obtain a thorough history, including onset and duration of symptoms, mechanism of injury, and precipitating causes of pain.
-
Perform a complete physical examination
if necessary, taking into account surrounding areas (spine, hip, ankle)
that may be sources of referred knee pain. -
Order supplemental studies, such as
radiographs, magnetic resonance imaging (MRI), bone scans, and special
procedures (arthrocentesis, arthrometer testing, and examination under
anesthesia) if they can aid in identifying the cause of knee pain.
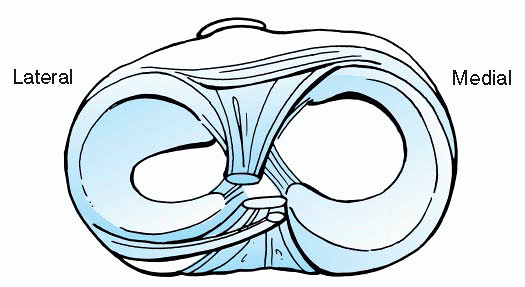
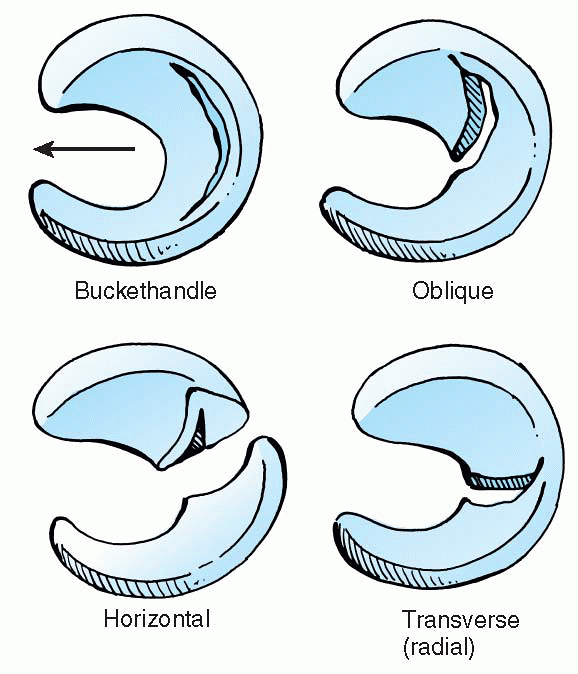
The menisci are found between the medial and lateral femoral tibial
articulations. They provide increased surface area to dispense
weightbearing forces between the femur and tibia, as well as provide
supplemental stability for the knee (Fig. 24.1-4).
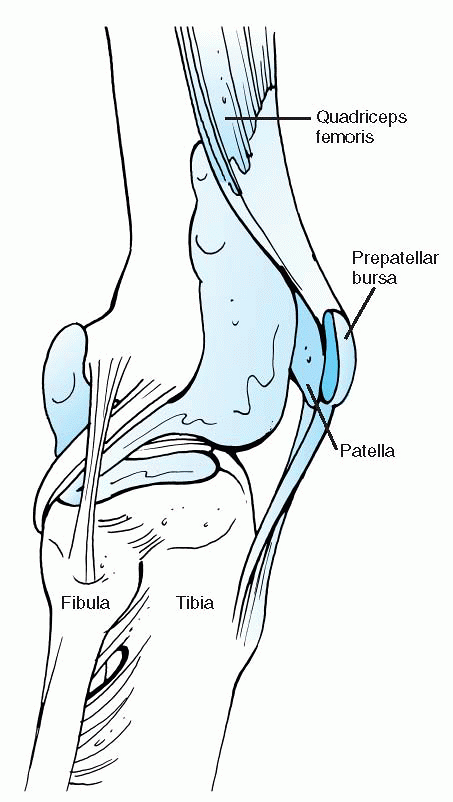
that allow adjacent soft tissue envelopes to glide across one another
about the knee. The most commonly involved in injury are the
prepatellar bursa (Fig. 24.1-5), pes anserine
bursa, and infrapatellar tendon fat pad. When inflamed, they present as
tender, soft, boggy structures overlying the area of injury.
neurovascular structures—the popliteal artery and vein and the tibial,
common peroneal, and saphenous nerves.
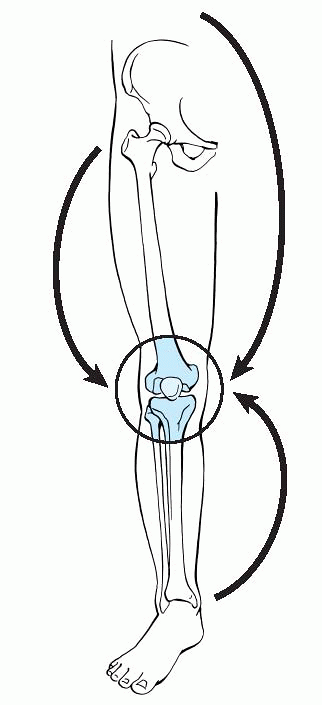
conduct specific examinations of each area previously listed and
identify areas of injury. Localizing the pain to a particular area is
the key to making the correct diagnosis. If the pain cannot be
localized on physical examination, one should consider a referred pain
from another area, such as the hip, spine, or ankle (Fig. 24.1-6).
 |
|
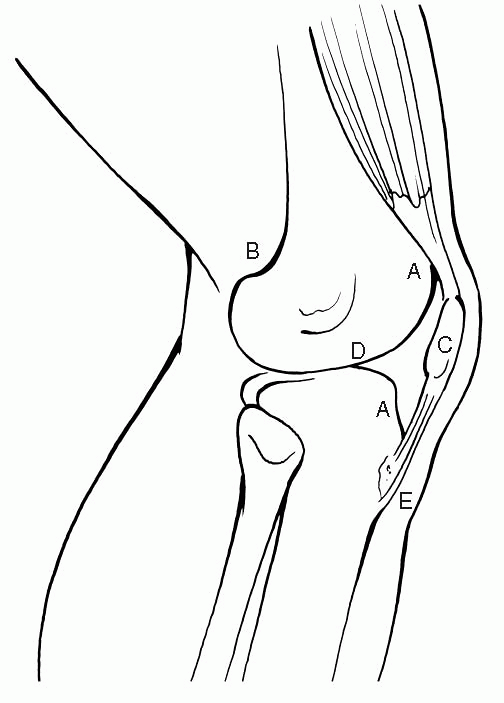
Figure 24.1-1 Surface anatomy of the knee. A; Suprapatellar and infrapatellar depressions. B; Adductor tubercle. C; Patella. D; Joint line. E; Tibial tubercle.
|
 |
|
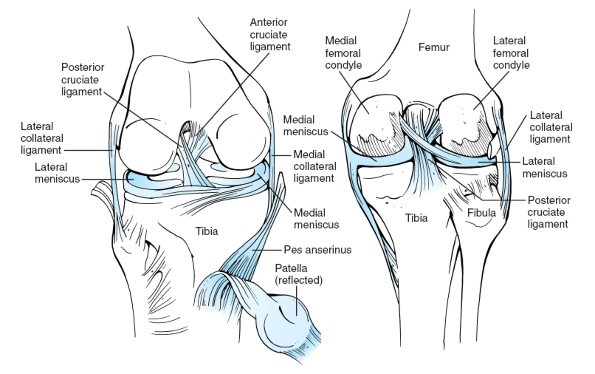
Figure 24.1-2 Normal knee anatomy.
|
 |
|
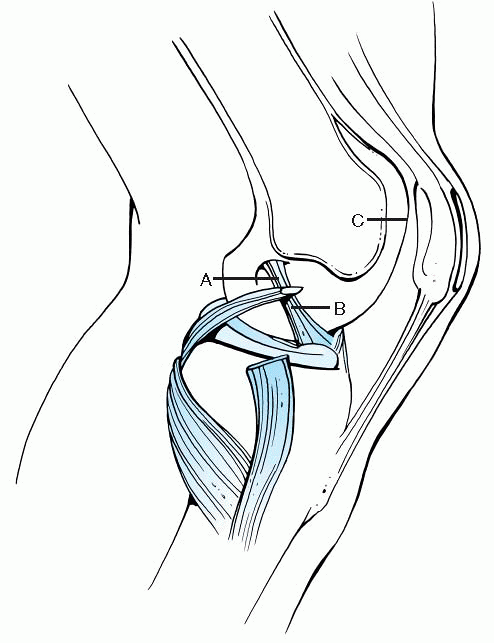
Figure 24.1-3 Ligaments of the knee. A; Posterior cruciate ligament. B; Anterior cruciate ligament. C; Patellofemoral articulation.
|
|
TABLE 24.1-1 KNEE LIGAMENT AND TENDON ANATOMY
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 24.1-4 Axial view of knee menisci.
|
injuries—acute versus repetitive microtrauma accumulated over time.
However, one needs to take a comprehensive approach in identifying the
cause of pain. The anagram VINDICATER is a useful tool as one begins to
formulate a differential diagnosis for knee pain (Box 24.1-1).
identify the cause of knee pain. Obtaining a complete history can be
difficult in a young child. Therefore, in addition to the child, it is
important to interview the caretakers who are familiar with the child
and circumstances related to the child’s symptoms (Tables 24.1-2 and 24.1-3).
 |
|
Figure 24.1-5 Prepatellar bursa.
|
 |
|
Figure 24.1-6 Sources of referred pain.
|
-
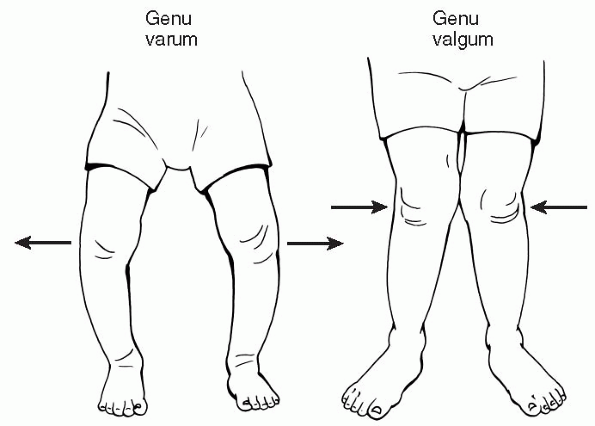
Begin with inspection of the knee alignment (Fig. 24.1-7), observation of the gait pattern, palpating pulses, and a neurologic exam (Table 24.1-4).
-
Follow with evaluation of joint motion, tests for ligament stability, and direct palpation to identify specific areas of injury.
-
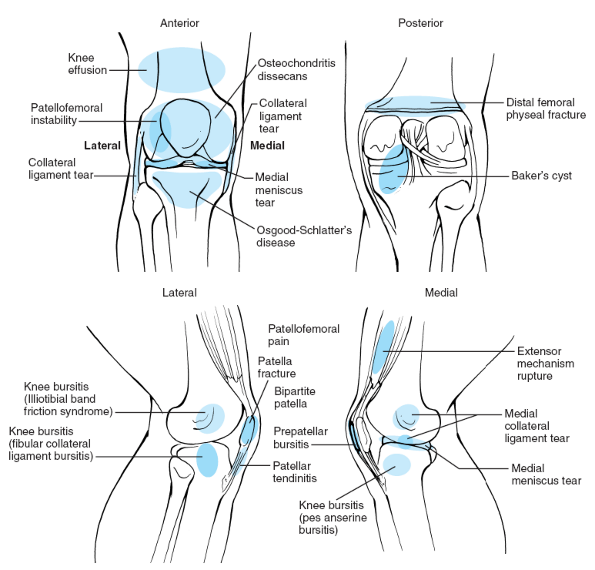
□ Localized tenderness is an important finding to identify the source of pain (Fig. 24.1-8).
-
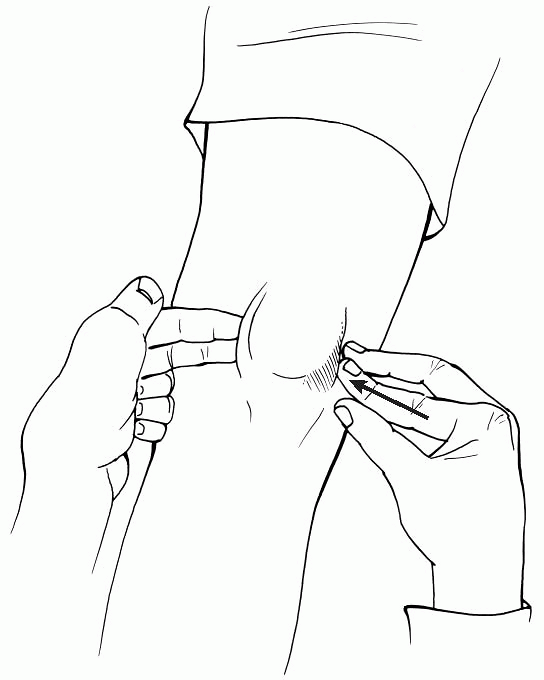
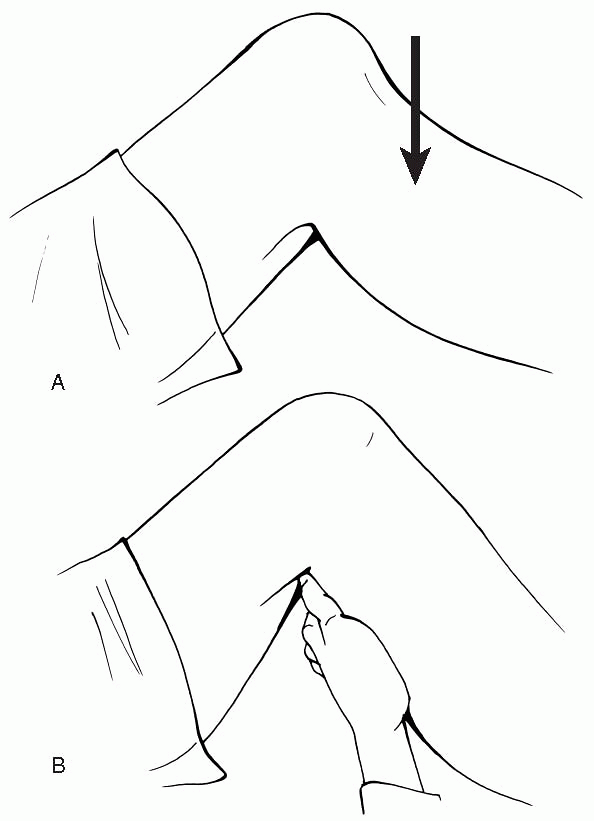
□ Meniscal injuries often present with
joint line tenderness extending from the midportion of the knee in the
coronal plane posteriorly behind the femoral condyle. -
□ Tender crepitance along the joint line
with flexion-rotation (McMurray test) or compressionrotation maneuvers
(Appley test) suggest a meniscal tear. -
□ Severely displaced menisci often found in buckethandle type tears can also limit full knee motion, especially extension.
-
-
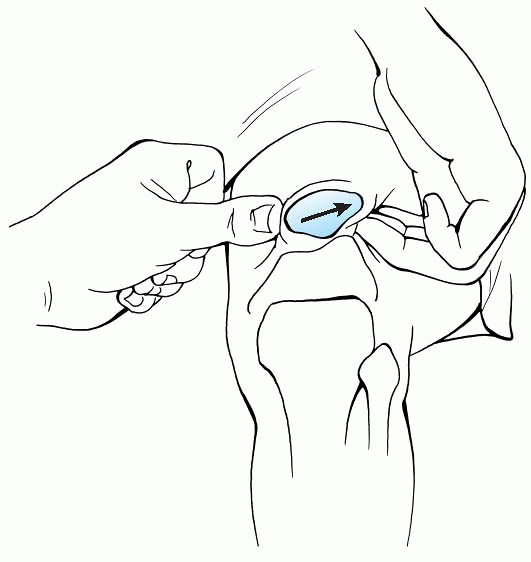
The patellofemoral joint is assessed with the patient lying supine and sitting with the knee bent at 90 degrees (Fig. 24.1-9).
-
□ Attempts at translating the patella
medially and laterally can elicit a sense of apprehension or resistance
from the patient in the case of patellar subluxation or dislocation (Fig. 24.1-10). -
□ Painful crepitance and tenderness along medial or lateral parapatellar retinaculum are also signs of patellofemoral injury.
-
□ Malalignment is determined by measuring
the Q angle, which is formed by the intersection of a line drawn along
the long axis of the thigh and a line drawn from the midpoint of the
patella to the tibial tubercle.-
□ The normal value of the Q angle is 10 degrees in men and 15 degrees in women.
-
□ Increased Q angles are thought to represent lateral tracking or misalignment of the patellofemoral joint.
-
-
□ Direct tenderness of the infrapatellar tendon can represent patellar tendonitis, commonly seen in repetitive jumping sports.
-
□ Sinding-Larsen-Johansson syndrome and
Osgood-Schlatter disease are represented by tenderness over the
inferior pole of the patella and tibial tubercle, respectively. -
□ Tenderness over the lateral femoral
epicondyle is often present with iliotibial band tendonitis, and
tenderness over the pes anserine area can represent an inflamed bursa
adjacent to medial hamstring insertions (Figs. 24.1-8B and 24.1-11, 24.1-12, 24.1-13, and 24.1-14; Table 24.1-5).
-
-
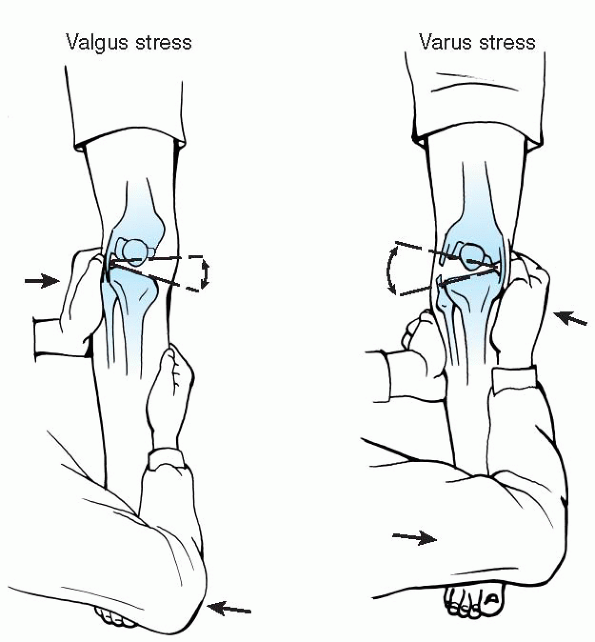
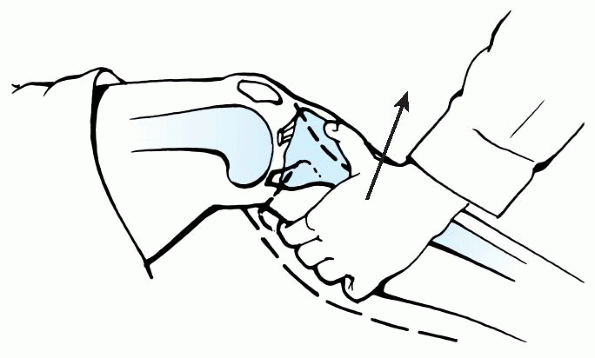
The knee ligament exam is conducted with both the patient sitting and supine.
-
□ Lying supine often helps the patient to
relax, thus avoiding inadvertent hamstring contraction that can
compromise the examination results (Table 24.1-6).
-
-
Vascular
-
Infectious
-
Neoplastic
-
Degenerative
-
Inflammatory
-
Congenital
-
Arthritic
-
Traumatic
-
Endocrine
-
Referred
|
TABLE 24.1-2 HISTORY OF KNEE INJURY
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 24.1-3 OUTCOMES ANALYSIS OF KNEE INJURY MECHANISM
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
|
TABLE 24.1-4 PHYSICAL EXAMINATION FOR KNEE PAIN
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 24.1-7 Knee alignment.
|
 |
|
Figure 24.1-8 Potential causes of knee pain and their respective anatomic locations.
|
 |
|
Figure 24.1-9 Supine evaluation of patellofemoral joint.
|
 |
|
Figure 24.1-10 Lateral translation and palpation of lateral patellar facet.
|
 |
|
Figure 24.1-11 Testing collateral ligaments of the knee.
|
 |
|
Figure 24.1-12 Lachman test for anterior cruciate ligament deficiency.
|
 |
|
Figure 24.1-13 (A) Posterior sag sign, indicating posterior cruciate injury. (B) Absence of posterior sag, indicating normal posterior cruciate ligament.
|
 |
|
Figure 24.1-14 Meniscal injuries.
|
|
TABLE 24.1-5 DIAGNOSIS OF KNEE PAINa
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
|
TABLE 24.1-6 LIGAMENT EXAMINATION
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
-
Routine x-rays of the knee should be part of every “painful knee” evaluation.
-
□ A standard knee x-ray exam should
include a weight-bearing posteroanterior (10 to 15 degrees flexed),
lateral, Merchant or sunrise patella view, and an intercondylar notch
view of the knee. -
□ When the patient is unable to stand, an anteroposterior view of the knee should be obtained.
-
□ After a satisfactory film is obtained, systematic careful evaluation of the x-ray is performed.
-
□ Although seemingly evident, it is wise to confirm the name on the films with the name of the patient being examined.
-
□ Appropriate indicators of the side (right vs. left) being examined should also be noted (Table 24.1-7).
-
-
When knee x-rays are normal, evaluate the spine, hip, and ankle regions to rule out sources of referred pain.
-
Additional imaging studies such as MRI
and bone scans can be useful in determining and localizing the extent
of injury and in making treatment decisions, but they should not be
used as primary screening studies. -
Special procedures for diagnosing knee pain are given in Table 24.1-8.
|
TABLE 24.1-7 RADIOGRAPH EVALUATION GUIDELINES
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 24.1-8 SPECIAL PROCEDURES
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||
|
TABLE 24.1-9 VASCULAR CAUSES OF KNEE PAIN
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||
|
TABLE 24.1-10 INFECTIOUS CAUSES OF KNEE PAIN
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
-
Vascular causes of knee pain are listed in Table 24.1-9.
-
Infectious causes of knee pain are listed Table 24.1-10.
-
As a whole, primary bone tumors around the knee are rare.
-
Degenerative conditions are typically not found in the pediatric age group.
-
Primary inflammatory conditions of the knee are rare.
-
□ Generally, juvenile rheumatoid arthritis presents in the 2- to 6-year-old age group as a swollen knee and a limp.
-
□ Workup to rule out trauma, infection, and tumor are normal.
-
□ Treatment is primarily medical, and patients should be referred to a rheumatologist.
-
□ Outcomes are generally good with appropriate medical management.
-
□ Other considerations for inflammatory causes of knee pain include Lyme disease and lupus erythematosus.
-
□ Extensor mechanism disorders typically fall under the scope of overuse syndromes (Box 24.1-2), which are considered more fully in section 24.2.
-
-
Congenital causes—conditions with
generalized ligamentous laxity, such as Ehlers-Danlos syndrome, Down
syndrome, and nail-patella syndrome—typically make children more prone
to injury, particularly of the patellofemoral joint.P.280-
□ Treatment protocols usually do not differ from those of children without congenital conditions.
-
-
Traumatic causes of knee pain are listed in Table 24.1-12.
-
In cases in which the physical
examination is unremarkable, one needs to consider referred sources of
knee pain, which are given in Box 24.1-3.
|
TABLE 24.1-11 NEOPLASTIC CAUSES OF KNEE PAIN
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
-
Osgood-Schlatter disease
-
Sinding-Larsen-Johansson syndrome
-
Patellar tendonitis
-
Adolescent anterior knee pain
-
Symptomatic plica
-
Iliotibial band syndrome
from minor contusions, muscle strains, or tendonitis related to minor
trauma or overactivity. Most are resolved with conservative measures,
which include rest, application of ice to reduce swelling, compressive wraps, temporary bracing or splinting, and elevation
to prevent edema. This is known as the RICE program, which also
includes activity modification or restriction until symptoms have
resolved. Occasionally, a course of physical therapy is needed to aid
in restoring joint range of motion and muscle strength.
|
TABLE 24.1-12 TRAUMATIC CAUSES OF KNEE PAIN
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||
responding to conservative measures, or if there is suspicion of
infection, vascular injury, obvious deformity, or fracture.
-
Lumbar spine: herniated disc, spondylolisthesis
-
Hip: slipped capital femoral epiphysis
-
Ankle: osteoid osteoma, osteochondritis desiccans
JP, Andrish JT. Knee ligament injuries in the skeletally immature
athlete. In: Orthopaedic knowledge update: sports medicine 2. Rosemont,
IL: American Academy of Orthopaedic Surgeons, 1999:355-364.
MC, Hornicek FJ. Osteosarcoma. In: Orthopaedic knowledge update:
musculoskeletal tumors. Rosemont, IL: American Academy of Orthopaedic
Surgeons, 2002:175-186.
A, Scoles PV. The knee. In: Pediatric orthopaedics in clinical
practice, 2nd ed. Chicago: Yearbook Medical Publishers, 1988: 122-139.
CL. Knee disorders. In: Orthopaedic knowledge update: pediatrics.
Rosemont, IL: American Academy of Orthopaedic Surgeons, 2002:191-201.
in organized sports programs. Sports programs and recreational,
seasonal participation in a variety of sports are being replaced by
year-round competition in a single sport or activity. This trend toward
early specialization in a single activity has increased the number of
sports-related injuries in young athletes. In addition, there has been
a change in the pattern of injuries observed with the microtraumatic or
overuse injury predominating over the acute, or macrotraumatic injury.
repetitive submaximal stresses are applied to otherwise normal tissues.
If there is adequate time for the tissue to repair itself, the tissue
adapts to the demand and is able to undergo further loading without
injury. Without adequate recovery, the normal reparative processes are
overwhelmed; tissue failure (due to microtrauma) develops and
stimulates the body’s inflammatory response, leading to clinical injury.
Growth cartilage is found in three locations in the child: the physes,
the epiphyseal surfaces, and the apophyses, all of which are
susceptible to overuse injuries.
important in diagnosing and treating overuse injuries. One must
remember that the period of abusive training may have occurred weeks to
months before the onset of clinical pain. Predisposing factors leading
up to the onset of pain must be sought.
Intrinsic factors such as limb alignment and resulting biomechanics are
innate to the athlete. Extrinsic factors are determined by the athlete,
and these include training regiments, shoes, and running surfaces.
bone. Much like repetitive bending of a paperclip, repetitive loading
of virtually any element of the musculoskeletal system can lead to
structural fatigue. Ideally, this leads to remodeling and strengthening
that allows more activity as time
goes on. If fatigue occurs faster than remodeling, the tissue fails resulting in clinical injury.
-
Stress fracture
-
Spondylolysis
-
Osteochondritis dissecans—capitellum
-
Little League shoulder
-
Gymnast’s wrist
-
Osgood-Schlatter disease
-
Sinding-Larsen-Johansson syndrome
-
Sever disease
-
Little League elbow
-
Iselin disease
-
Medial tibial stress syndrome
-
Achilles tendonitis
-
Patellar tendonitis
-
Rotator cuff tendonitis
-
Pes planus
-
Hyperpronation
-
Tibial torsion
-
Femoral anteversion
-
Patellofemoral malalignment (Q angle)
-
Leg length discrepancy
-
During growth, lengthening of bone occurs more rapidly than surrounding muscle leaving the muscle-tendon unit tight
-
Susceptibility of growth cartilage
-
Scoliosis
-
Arthritis
-
Nutritional deficiency
-
Excessive ligament laxity
-
Previous injury
-
Sudden increase in intensity, frequency, or duration of an activity
-
Addition of new program or sport
-
Attendance at a specialty camp
-
Pitching style
-
Wornout footwear (should be replaced every 250-400 miles)
-
Grip size, string tension
-
Change in surface (wood, pavement, grass)
-
Hill or bleacher training
stress fracture. Among youths, these most commonly occur with distance
running. The athlete may experience gradual onset of symptoms and
eventually be unable to run because of pain. Acute failure can occur
through the weakened bone resulting in a complete fracture.
-
Virtually any bone can be affected
-
Most common metaphyseal and diaphyseal
stress fractures in young athletes include the fibula, metatarsals,
tibia, femur, and ulna. -
Stress fractures of the metatarsals
(typically the second or third) and the distal fibula rarely have
complications other than pain and disability. -
Fractures of the tibia, humerus, and forearm rarely displace but do represent potential risk for morbidity.
-
Most occur in later adolescence, ages 16 to 19.
-
Boys and girl are equally affected.
-
Initially, only about 10% of radiographs are abnormal.
-
Bone scan and magnetic resonance imaging (MRI) are much more sensitive.
-
Bones scans result in radiation exposure,
but are useful if the exact area of involvement is in question.
Findings must be correlated to the clinical symptoms. As many as 50% of
adolescents with stress fractures will show multiple areas of stress
response on bone scans that do not correlate to areas of symptoms. -
MRI detects subtle marrow edema and early cortical failure.
-
Rest treats most diaphyseal and metaphyseal stress fractures.
-
Crutches are often necessary. Occasionally, immobilization is needed.
-
Healing time can range from 4 to 12 weeks.
-
Alternative training, gradual resumption of sports, and monitoring for recurrent symptoms are necessary.
-
Some stress fractures require surgery.
-
□ Stress fractures of the hip are rare
but have the highest potential for morbidity. Femoral neck fractures
can displace, disrupt the blood supply to the femoral head, and lead to
avascular necrosis. -
□ Stress fractures of the fifth metatarsal tend to be recurrent and are often best managed with an intramedullary screw.
-
-
Fracture through the pars interarticularis of the lumbar vertebrae.
-
Commonly seen in athletes who are under
the age of 20 and involved in a sport that requires repetitive
extension of the lumbar spine, such as gymnastics, cheerleading,
diving, football (linemen), and dance. -
The most common location is L5-S1, followed by L4-L5.
-
Pain with palpation is worse with single or dual leg hyperextension.
-
Flexion usually is painless.
-
Hamstrings frequently are tight.
-
Anteroposterior, lateral, and oblique x-rays of the lumbar spine may be negative.
-
Look for the fracture through the neck of the “Scotty dog” on the obliques.
-
If clinical suspicion is high, and x-rays
negative, consider computed tomography (CT), single-photon emission
computed tomography (SPECT), or MRI.
-
Modify activities to avoid extension for 4 to 8 weeks.
-
Consider rigid lumbar support bracing for 4 to 8 weeks.
-
Physical therapy for truncal stabilization, and functional progression back to sport.
-
Can resume activities without the brace 8 to 12 weeks from diagnosis.
-
A disorder of the proximal tibial
apophysis that commonly affects young athletes, but may bother other
active youngsters who are not involved in formal, organized sports. -
The tubercle of the proximal tibia is the insertion site of the patellar tendon.
-
Because of the strength or the quadriceps, large tensile forces are transmitted through the patellar tendon insertion.
-
The normal transition from the ossified
and unossified tubercle into the tendon undergoes fatigue failure and a
healing response ensues.
-
While activity plays a role, some
individuals appear to be predisposed to this condition; 20% to 30% of
youngsters will have siblings who have had the same problem. -
Typically, the child is between 10 to 15 years of age at the onset.
-
Boys are more commonly affected than girls; however, female gymnasts seem to be particularly prone to this problem.
-
Approximately 15% of teenage boys and 10% of teenage girls are affected.
-
Incidence of bilaterality varies considerably.
-
Typically significant pain and prominence on the presenting side and some degree of findings on the contralateral side.
-
Many patients have a prior history of heel pain compatible with Sever disease (calcaneal apophysitis).
-
Pain is usually well localized to the prominent tibial tubercle.
-
Pain is typically related to activities.
-
There should be no signs or symptoms of intraarticular problems of the knee joint itself.
-
The diagnosis can then be made clinically.
-
A lateral radiograph of the knee can be helpful to confirm the diagnosis by showing irregularity of the tibial tubercle.
-
The radiograph should also rule out any other osseous problems, such as tumor or infection.
-
In most, it simply runs its course with time, with symptoms lasting 1 to 4 years.
-
In approximately 3% of patients a
persistent ossicle forms, which can remain symptomatic and ultimately
require surgical excision. -
Associated tuberosity fractures are so rare that there appears to be no sound evidence that activity restriction is required.
-
Symptomatic measures include ice,
nonsteroidal antiinflammatory drugs (NSAIDs), compressive sleeve or
band, activity modifications as indicated by the symptoms, and
hamstring stretching. -
Casts/rigid braces are rarely used, except for severe acute exacerbation.
-
Pathophysiology is similar to Osgood-Schlatter disease but the pain is located over the inferior pole of the patella.
-
Typically patient is between 8 to 13 years of age at onset.
-
Bilaterality varies considerably.
-
The pain is well localized over the inferior pole of the patella.
-
The pain is related to activities.
-
The diagnosis is clinical.
-
Lateral radiograph may show irregular ossification over the distal patella.
-
Same as Osgood-Schlatter disease.
-
Heel pain is a common complaint of the young adolescent.
-
It is due to the very powerful but tight gastrocsoleus complex as it inserts on the back of the calcaneus.
-
Seen more often in boys age 9 to 13.
-
More common in gymnastics, running, and sports in which cleats are worn (football, soccer).
-
Bilateral in 50% of cases.
-
Pain localized to posterior aspect of calcaneus.
-
Pain with medial and lateral pressure on the heel (squeeze test).
-
Disease is associated with hyperpronation, femoral anteversion, tibial torsion.
-
Those affected usually have tight plantarflexors and weak dorsiflexors.
-
The diagnosis is made clinically. A
lateral radiograph may show fragmentation and irregularity of the
calcaneal apophysis, but this can be seen in asymptomatic heels.
-
The condition is self-limited so
treatment is conservative and aimed at symptomatic relief: ice, NSAIDs,
modification of activities, ¼-inch silicone or Sorbothane heel cups,
orthotics to correct any mechanical problem, physical therapy, and home
exercises to stretch the plantarflexors and strengthen the dorsiflexors. -
Casting for 2 to 3 weeks may be needed in extreme cases.
-
This is an uncommon traction apophysitis at the base of the fifth metatarsal at the insertion of the peroneus brevis.
-
It occurs in skeletally immature athletes.
-
Pain is located on the lateral side of the foot and exacerbated by running, jumping, and cutting.
-
Pain with resisted eversion.
-
Radiographs may show a widened and prominent apophysis at the base of the fifth metatarsal.
-
Ice
-
NSAIDS
-
Activity modification to avoid pain.
-
Physical therapy to stretch the ankle evertors and strengthen the invertors.
-
Throwing produces a valgus moment at the
elbow with compressive loads applied to the lateral side
(radiocapitellar joint) and traction loads across the medial side. -
In the late teen years and above,
repetitive traction injuries involve the medial collateral ligament
itself, and can lead to rupture of the ligament. -
In the immature skeleton, the apophysis
of the medial epicondyle can begin to fragment, which leads to a
reparative process leading to pain and prominence.
-
Point tenderness over the medial epicondyle.
-
Little or no loss of extension.
-
Radiographs usually show some degree of irregularity or fragmentation of the apophysis.
-
Pain usually resolves with time and rest.
-
Avulsion of the medial epicondyle can
occur with forceful throwing, so restriction of rigorous throwing, such
as pitching, is prudent.-
□ Batting is usually not troublesome, and many can play an infield position while this resolves.
-
□ Return to pitching in less than 6 months often results in recurrence.
-
-
During periods of rapid growth, there is
a strength-flexibility imbalance in the muscle tendon unit due to rapid
growth of the bone relative to the muscle tendon. -
Several apophyses in the pelvis are susceptible to traction injuries (Table 24.2-1).
-
These are most commonly seen in runners, sprinters, football players, and soccer players.
|
TABLE 24.2-1 APOPHYSES IN THE PELVIS
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Ice
-
NSAIDs
-
Modification of activities to maintain cardiovascular endurance
-
Stretching of the involved muscle-tendon unit once acute pain subsides
-
Gradual return to activities usually by
the direction of a physical therapist (usually after 2 to 4 weeks; 4 to
6 weeks if avulsion is present)
-
Repetitive stress to the shoulder can lead to widening and resorption around the proximal humeral physis.
-
This “physiolysis” has been termed “Little League shoulder” since it occurs primarily in Little League baseball players.
-
While typically affecting pitchers, other rigorous throwers, such as catchers, can develop this as well.
-
Typically 12- to 15-year-old boys
-
Shoulder pain related to overhead throwing
-
Usually more painful in the deltoid region than the subacromial region
-
Differential diagnosis: rotator cuff tendonitis and impending pathologic fracture from a simple bone cyst to the upper humerus
-
Radiographic widening of the proximal humeral physis on the affected side confirms the diagnosis of Little League shoulder.
-
□ Need comparison with other shoulder.
-
-
Primarily involves rest
-
Complications are uncommon, so if the symptoms are minimal, batting and playing infield positions are usually not painful.
-
Resolution can take up to 6 months.
-
Pitching is gradually resumed.
-
Monitor for resumption of symptoms.
-
Gymnastic training often begins as early
as age 4 or 5 and peaks in the early to mid-teens, during which the
time spent in training may reach as high as 30 to 40 hours per week. -
Because many maneuvers in gymnastics
involve weight-bearing on the dorsiflexed wrist, often with a
rotational component, the wrist is a common site of overuse injury. -
The term gymnast’s wrist is a catchall term often used to describe any of a wide variety of wrist injuries in gymnasts.
-
The most common chronic injury seen is at the level of the distal radial physis.
-
80% to 90% of affected athletes are female.
-
Typically 12 to 14 years of age
-
Symptoms are bilateral in approximately one-third of patients.
-
Usually seen in gymnasts whose weekly training regimen exceeds 20 hours per week.
-
Vault and floor exercise are the events most likely to cause symptoms.
-
Patients have pain with palpation over the distal radial physis.
-
There is pain at extremes of dorsiflexion.
-
This can be differentiated from dorsal impingement by the presence of pain on the volar and radial aspects of the physis.
-
Radiographs may be normal (stage 1), and the diagnosis is made clinically.
-
Radiographs may show widening of the
distal radial physis, irregularity or cystic changes on the metaphyseal
side of the growth plate, or breaking of the radial physis (stage 2). -
With late presentations, the radiographs may show positive ulnar variance due to premature closure of the radial physis.
-
Stage 1 (no radiographic changes)
-
□ Modified rest, which involves avoidance
of axial compressive loads for a period of 2 to 4 weeks. During this
time the athlete may continue to condition, maintain flexibility, and
continue to train on the beam, practice aerial stunts, as well as
footwork on the floor exercise. -
□ After the pain resolves, a gradual return to activity is allowed with close supervision.
P.286 -
-
Stage 2 (radiographic changes with no ulnar variance)
-
□ Avoidance of axial compressive loads for 6 to 12 weeks. Casting may be appropriate for the noncompliant athlete.
-
□ To improve compliance, it is important
to inform the gymnast that absolute rest will provide the best chance
of returning to a competitive level.
-
-
Stage 3 (positive ulnar variance)
-
□ Same as stage 2.
-
□ Consider MRI arthrography for
triangular fibrocartilage complex (TFCC) tears. This should be
suspected in any gymnast with wrist pain on the ulnar side. -
□ Possible need for shortening osteotomy of the ulna.
-
-
Educate athletes and coaches on the importance of wearing variance braces with workouts.
-
Recommend bi-annual routine wrist radiographs in all gymnasts training more than 16 hours per week.
-
Encourage strength and flexibility training of the wrists year-round.
-
Alternate compressive, axial-loading workouts (vault) with traction workouts (uneven bars).
-
Early stage diagnosis: encourage gymnasts at all ages to have wrist pain evaluated.
of the epiphyses occurs at the capitellum—Panner disease and
osteochondritis of the capitellum. In these conditions, a segment of
epiphyseal bone becomes necrotic and can result in separation of the
bone segment and overlying articular cartilage. While technically
classified as an “osteochondrosis,” these have features of repetitive
stressinduced injuries, much like stress fractures.
-
Panner described a lesion of a young boy’s capitellum that he compared with Legg-Calvé-Perthes disease.
-
In patients under 10 years of age who develop irregularity of the capitellum, the course is usually quite benign.
-
An avascular segment of bone develops in the center of the capitellum, revascularizing in time.
-
Loose bodies do not typically form.
-
Sequelae are rare and treatment is simply rest.
-
While the term osteochondritis dissecans implies that there is an inflammatory process present, histologic studies have in fact failed to confirm this.
-
Appears to be a repetitive stress phenomenon
-
Most commonly occurs in baseball pitchers.
-
As the ball is accelerated during the pitching motion, a valgus moment is created at the elbow.
-
□ There is tension on the medial side of the elbow and compressive forces across the radial capitellar articulation.
-
-
The capitellum has an end arterial blood
supply, which may explain its susceptibility to develop avascular
necrosis from chronic repetitive compression loads.
-
Side arm pitches, many curve ball
techniques, and others can increase the compression loads across the
lateral side of the elbow by bringing the ball further away from the
midsagittal plane and accentuating the valgus moment. -
Typically patients complain of an aching pain in the lateral side of the elbow.
-
Often they have flexion contractures.
-
Displaced fragments can result in a loose body sensation, a locked elbow, or significant synovitis and pain.
-
Plain radiographs typically show a sclerotic region or radiolucency. Tangential views may help.
-
Occasionally, CT scan or MRI are indicated.
-
Osteochondritis of the capitellum can result in permanent arthrosis of the elbow joint.
-
Prevention through education is key.
-
□ Junior baseball programs should have
rules limiting how much youngsters can pitch, typically three innings
per game, up to six innings per week.
-
-
Occasionally, intact lesions heal with prolonged rest, but surgery is often necessary to remove unstable or displaced fragments.
-
Compared with simple arthroscopic débridement, there is no proven benefit to grafting, or other procedures.
-
Unlike in adults, tendon degeneration and rupture are rarely seen in youths.
-
The rotator cuff is a convergence of the tendons of the subscapularis, supraspinatus, infraspinatus, and teres minor.
-
□ These extend from the scapula out over the humeral head.
-
□ Together, they stabilize the humeral
head against the glenoid fossa and they prevent the humeral head from
rubbing beneath the arch of the acromion. -
□ The supraspinatus muscle is the most important of these.
-
-
Many factors contribute to rotator cuff tendonitis.
-
□ In young athletes, inherent laxity of the glenohumeral capsule is likely a significant factor.
-
□ Overhead throwing in baseball, swimming, serving motion in tennis, and gymnastics precipitate symptoms.
-
-
Pain produces inhibition of the rotator cuff muscles, which precipitates impingement of the humeral head beneath the acromion.
-
□ With time, a well-established bursitis and tendonitis develop.
-
-
Typical complaints: pain with overhead activities, and sensation of the arm becoming heavy, tired or “dead.”
-
Thoroughly examine the neck and shoulder looking for restriction of motion, muscle atrophy, and focal tenderness.
-
□ There may be tenderness along the course of the biceps tendon, as well.
-
-
The supraspinatus strength should be tested.
-
□ Glenohumeral laxity is common.
-
-
Plain radiographs are useful to rule out other bony abnormalities.
-
MRI can be diagnostic for rotator cuff tendonitis; however the diagnosis can usually be made clinically.
-
□ Partial and full thickness rotator cuff tears are rarely seen before 18 years of age.
-
-
The principles of treatment center on restoring strength and motion of the rotator cuff and scapular stabilizers.
-
NSAIDs.
-
Often overhead activities are curtailed
while physical therapy is initiated. Rehabilitation of the entire
scapular thoracic complex is key. -
As pain diminishes and strength returns,
overhead sporting activities are initiated, with careful monitoring for
evidence of recurrent impingement. -
In recalcitrant cases, a subacromial or intraarticular injection of steroids can hasten resolution of the inflammatory phase.
-
Occasionally, surgical stabilization is necessary, though subacromial decompression is rarely indicated for youths.
the diagnosis of “shin splints” refers to a collection of maladies with
the common feature being activity-induced pain in the midportion of the
leg. Specific diagnoses include:
-
Periostitis
-
Chronic exertional compartment syndrome
-
Stress fracture
-
Muscle herniation
-
Superficial nerve entrapment
-
Deep venous thrombosis
-
Tumor
-
Infection
-
Popliteal artery entrapment
-
This clinical entity is also termed medial tibial stress syndrome and soleus syndrome.
-
The soleus muscle and its investing fascia originate in this area and are also implicated in causing the syndrome.
-
Three-fourths of running athletes with shin pain have posteromedial tenderness, and half of them are bilateral.
-
Boys and girls are equally affected.
-
Predisposing factors include:
-
□ Muscle weakness
-
□ Running shoes with a lack of heel cushion, inadequate arch support
-
□ Hard training surfaces.
-
□ Training errors such as sudden increases in intensity or mileage
-
□ Abnormal lower limb biomechanics
-
-
Activity-related pain
-
No associated numbness
-
Recent increase in the intensity of sports participation, training, and competition schedule
-
Recent change in regimen or shoes, and surface training conditions
-
Pain and tenderness along the distal
third of the posteromedial tibia—extending longitudinally along several
centimeters, and not across to the anterior tibia -
Varus hindfoot alignment, excessive forefoot pronation, genu valgum, excessive femoral anteversion, and external tibial torsion
-
No muscle herniation
-
Negative Tinel test
-
Normal radiographs
-
If confirmation of the clinical diagnosis
is needed, bone scan shows a longitudinal pattern of radionuclide
concentration rather than a transverse pattern more typical of a stress
fracture.
-
NSAIDs
-
Ice
-
Strengthening and stretching
-
Ultrasound
-
Foot orthoses
-
Graduated running program
-
Surgery rarely indicated
-
With repetitive exercise, the interstitial pressure within the osseofascial compartments of the leg can become elevated.
-
When compartment pressures exceed capillary filling pressure, the muscle becomes ischemic and produces pain.
-
This usually has an onset associated with activity and is relieved by rest.
-
Unlike acute compartment syndromes
resulting from trauma or arterial insufficiency, the pressure and blood
flow to the muscles normalizes in chronic compartment syndromes and
rarely result in tissue necrosis or residual disability. -
The anterior compartment is the most commonly involved, although any of the four compartments in the lower leg may be affected.
-
Typical complaints: aching pain, tightness, or a squeezing sensation brought on by and interfering with athletics
-
Usually relieved promptly after exercise
-
Some experience transient foot-drop with paresthesias across the dorsum of the foot if the anterior compartment is involved.
-
Plantar paresthesias with chronic posterior compartment syndrome.
-
Fascial defects with muscle herniation may be present over the anterior and lateral compartments.
-
If clinically indicated or desired, dynamic measurement of compartment pressures during exercise can confirm the diagnosis.
-
□ In chronic compartment syndrome, resting pressures typically are not elevated.
-
□ With exercise, the pressures rise to 70 to 100 mm Hg, while normal compartments rise to less than 30 mm Hg
-
□ MRI done immediately after exercise may have a role as well.
-
-
Initial treatment includes activity modification, foot orthoses, physical therapy, and time.
-
Recalcitrant cases may require a fasciotomy.
-
□ All involved compartments should be released.
-
□ This can be done through limited skin
incisions rather than through the extensive releases suggested for
adequate management of the acute traumatic compartment syndrome. -
□ Care must be taken to protect the saphenous vein, saphenous nerve, and the superficial branch of the peroneal nerve.
-
-
All compartments should be assessed because symptoms may not be adequate to identify all involved compartments.
-
History of bilateral symptoms should be specifically sought.
-
□ After unilateral surgical release,
patients frequently increase their activity levels, only to develop
pain on the side that had been asymptomatic.
-
-
Failures result from failing to
appreciate multiple compartment involvement; from inadequate
decompression, especially of the deep posterior compartments; and from
excessive scar tissue response.
MT. Sports medicine. In: Morrissey RT, Weinstein SL. Lovell &
Winter’s pediatric orthopaedics, 4th ed. Philadelphia: Lippincott
Williams and Wilkins, 2001.
DE, Sharpe K, Sufit RL, et al. Chronic compartment syndrome: diagnosis,
management, and outcomes. Am J Sports Med 1985;13:162-170.
BR, Nativ A. Gymnastics. In: Reider B, ed. Sports medicine, the school
age athlete, 2nd ed. Philadelphia: WB Saunders, 1996:459-462.
