Acute Spinal Injury
-
Initial evaluation and management.
Optimal outcome following acute spinal injury depends upon early
recognition of the injury and appropriate management to prevent further
injury. Adherence to the principles of advanced trauma life support
(ATLS) is mandatory. All patients with a mechanism of injury compatible
with spinal injury should be assumed to have a spinal injury until
proven otherwise. -
Clearance of spine in trauma patients.
While protection of the spine is mandatory at all stages of managing
the traumatized patient, “clearance” of the spine should take place
only after potentially life-threatening injuries have been stabilized.-
In the cognitively intact patient
(including the absence of drugs or alcohol) and cooperative patient,
clinical clearance of the spine may be possible. While case reports
have documented bony and ligamentous spinal injuries in such patients,
unstable spinal injuries or neurologic deterioration in these patients
have not been reported. Accordingly, routine radiographic evaluation in
such cases is not indicated. However, the physical examination findings
of neck or back pain, neurologic abnormalities, bruising, spinal
deformity, pain with active range of motion, or significant
“distracting” nonspinal injury should prompt further investigation. -
Obtunded or uncooperative patients, as
well as alert patients with physical examination findings consistent
with spinal injury, should be maintained on spinal precautions until
thorough clinical and radiographic evaluation of the spine has been
completed.
-
-
Studies
-
Roentgenograms.
The standard radiographic evaluation of the cervical spine includes the
lateral, open-mouth (odontoid), and anteroposterior plain films. The
lateral view will detect up to 85% of significant cervical spine
injuries provided that the occiput-C1 and C7–T1 junctions are
visualized. Despite normal x-rays of the upper cervical spine and the
absence of clinical findings suggestive of a lower-cervical injury, one
study has detected a 3.1% incidence of occult fractures at the C7–T1
level on computed tomographic (CT) scanning (1).
CT scanning of the upper cervical spine has become the method of
initial evaluation in many trauma centers. While the addition of
orthogonal oblique views does not increase the sensitivity of plain
film evaluation, these views provide excellent visualization of the
cervical posterior elements and foramina. Anteroposterior and lateral
images of the thoracic and lumbar segments are indicated in the
presence of pain or abnormal physical examination findings in these
regions and in cognitively impaired patients who cannot cooperate with
the physical examination. Additionally, because up to 6% of spinal
injuries have a noncontiguous injury elsewhere in the spine, the
presence of an injury anywhere in the spine should prompt radiographic
evaluation of the entire spine. -
Important points to consider in interpreting plain radiographs include (Fig. 11-1):
-
Any alteration in the alignment
of the bodies. Straightening of the cervical spine can result from
muscle spasms or from positioning the patient’s head in slight flexion.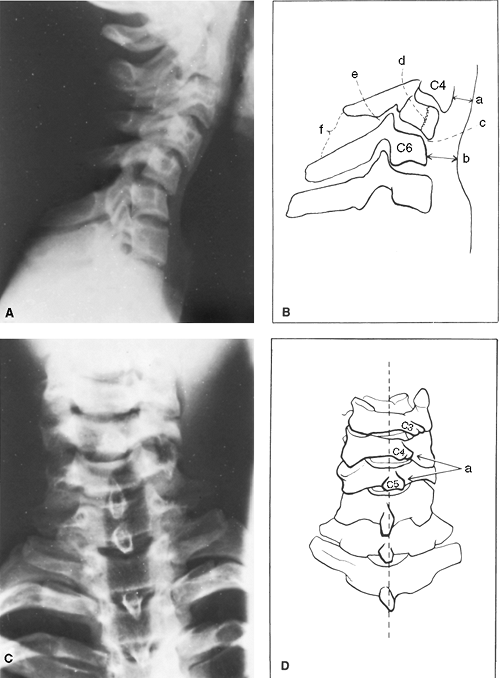 Figure 11-1. Important roentgenographic signs of a cervical spine injury. A and B:
Figure 11-1. Important roentgenographic signs of a cervical spine injury. A and B:
(a) Normal width of the retropharyngeal space at C4 is 4 to 6 mm. (b)
Normal width of the retropharyngeal space at C6 is 8 to 10 mm. (c) An
alteration in the alignment of the bodies. (d) Look for fracture lines
in the bodies or in the posterior elements. (e) A step-off in the line
of the posterior intervertebral facet joint. (f) An increased distance
between two spinous processes. C and D: The C4 spinous process is displaced laterally in relation to C5, demonstrating facet disruption. -
Any step-off in the line of the posterior intervertebral facet joints.
-
Any increase in the width of the retropharyngeal space in front of the vertebral bodies (normal is 4–6 mm at C3 and 15–20 mm at C6). This rule does not apply in a crying child.
-
Any fracture lines in the bodies or in the posterior elements.
-
Any increase of distance between two spinous processes.
-
Any displacement of the spinous process on the cephalad side, which is toward the side of any unilateral dislocation on the anteroposterior film.
-
Any indication that
the body of one vertebra has moved forward in relation to another on
the lateral roentgenogram because such movement usually indicates a
dislocation or fracture-dislocation of one or both joint facets at that
level. If the amount of displacement is more than half the width
of the vertebral body, the dislocation is bilateral and the spine is
extremely unstable.
P.184P.185 -
-
CT scanning
can provide rapid and detailed assessment of the spine. This should
include high-resolution imaging (2- to 3-mm collimation and 1.5-mm
pitch) from the occiput to T1 with sagittal and coronal
reconstructions. Several studies have demonstrated high levels of
sensitivity (90%) and specificity (100%) of screening CT scanning in
polytrauma patients (2,3,4). While CT appears to be a cost-effective primary screening tool in patients at high or moderate risk for cervical injuries (5), CT scanning represents the standard of care in all patients when:-
poorly visualized areas are encountered on plain films
-
visualization of T1 is not improved with gentle downward traction on the arms, swimmer’s views, or oblique views
-
fractures or dislocations are identified elsewhere in the spine
-
in patients who are intubated, as plain
films will miss up to 17% of injuries to the upper cervical spine in
the presence of an endotrachial tube
-
-
Magnetic resonance imaging (MRI) is less
sensitive, less specific, and less cost effective than the plain film
series or screening CT for the identification and evaluation of
cervical fractures (6). However, MRI is
extremely sensitive and specific for evaluation of the paravertebral
soft tissues, including the spinal cord, intervertebral discs, and
ligamentous structures. Patients with abnormal neurologic findings,
particularly incomplete injuries, should undergo MRI scanning of the
relevant spinal segment(s) to visualize the spinal cord and nerve roots. -
Dynamic fluoroscopy.
Passive flexion and extension stressing of the cervical spine,
performed by an experienced physician under fluoroscopy, has a reported
sensitivity of 92.3% and specificity of 98.8% for detecting significant
ligamentous injuries and instability of the cervical spine (7).
While some centers support the use of this technique in clearing the
spine of unconscious patients, the risk of neurologic deterioration may
outweigh its benefits, especially given the widespread availability of
CT and MRI imaging (7).
-
-
The ASIA (American Spinal Injury Association) classification
is a modification of the Frankel scale and is the most commonly used
classification of spinal cord injuries. The ASIA classification grades
spinal cord injuries from A through E, where ASIA A represents complete loss of motor and sensory function below the level of the lesion and ASIA E represents normal sensory and motor function. Incomplete spinal cord injuries are classified as ASIA B (preserved sensation but no motor function below the level of the injury), ASIA C (motor function less than or equal to grade 3 distal to the level of the injury), or ASIA D (motor function greater than grade 3 but less than normal distal to the level of the injury). -
Partial cord syndromes.
Incomplete spinal cord injury may involve discrete anatomical zones of
the spinal cord, resulting in characteristic patterns of neurologic
deficits.-
The anterior cord syndrome
involves loss of neural function in the anterior two thirds of the
spinal cord. Patients with these injuries experience complete loss of
motor function and of pain and temperature sensation but retain
sensations of vibration, proprioception, and light touch. These
preserved functions result in an improved prognosis. -
The posterior cord syndrome
is characterized by loss of proprioception and vibrational sensation.
Motor function and gross touch sensation typically are spared due to
the ventral location of the descending motor tracts and spinothalamic
tracts, respectively. The prognosis in posterior cord syndrome is fair. -
The central cord syndrome
is typically associated with a cervical hyperextension injury, often in
older patients. This syndrome consists of a disproportionately greater
weakness in the upper extremities compared with lower extremities,
various sensory changes at or below the site of the lesion, and urinary
bladder dysfunction. Proposed causes include hematomyelia, contusion,
cord swelling, and ischemia of the cervical spinal cord. The anterior
horn cells at the level of injury may also be involved. The prognosis
depends on the amount of initial neurologic involvement and the
rapidity of subsequent recovery. The signs of neurologic damage tend to
disappear in reverse order of their appearance. -
A penetrating injury or unilateral facet dislocation can result in unilateral injury to the spinal cord: the Brown-Séquard syndrome. Patients experience loss of ipsilateral motor and dorsal column function and contralateral pain and temperature sensation.
-
-
Pharmacologic management of spinal cord injuries.
Pharmacologic agents thought to mitigate the secondary effects of
spinal cord injury have been extensively studied and widely debated in
recent years. These agents include opiate antagonists, calcium channel
blockers, free radical scavengers, neurotropic compounds, and, most
notably, steroids (8) and gangliosides (9).-
Methylprednisolone.
The National Acute Spinal Cord Injury Studies (NASCIS I, II, and III)
have studied the use of parenteral methylprednisolone following spinal
injury. NASCIS I detected no benefit in the treatment group, but the
steroid dose used was found to be below the therapeutic threshold in
subsequent animal experimentation (10). In
NASCIS II, patients were randomly assigned to receive a higher loading
dose of methylprednisolone, naloxone (an opioid antagonist), or placebo
within 12 hours of acute spinal cord injury (11).
While investigators found no overall benefit in the methylprednisolone
group, post hoc analysis of the data suggested small gains in total
sensory and motor scores in a subgroup of patients who had received
drugs within 8 hours of the injury. Naxolone was less effective than
methylprednisolone. Despite the weakness of the data, high-dose
methylprednisolone infusion over 24 hours became the standard of care
in patients treated within 8 hours of acute spinal cord injury. NASCIS
III compared 48-hour infusion with 24-hour infusion and found no
benefit to extending the treatment beyond 24 hours (12).
Again, in post hoc analysis of the data, there appeared to be a benefit
from extending the infusion to 48 hours when treatment began between 3
and 8 hours after the injury. While no other study has verified the
results of the NASCIS conclusions, most centers have adopted the
following protocol:-
An initial loading dose of 30 mg/kg of methylprednisolone intravenous (IV), given over one hour, followed by:
-
a 23-hour infusion of 5.4 mg/kg of the same drug if administered within 3 hours of injury or
-
a 47-hour infusion of 5.4 mg/kg of the same drug if administered within 3 to 8 hours after injury
-
-
Newer pharmacologic regimens are being studied to clarify their role in improving outcomes (9,12).
-
-
-
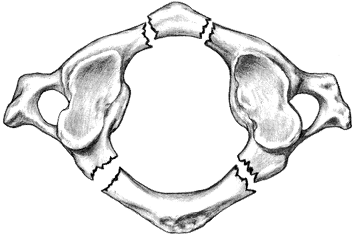
Fracture of the C1 vertebra (Jefferson fracture)
-
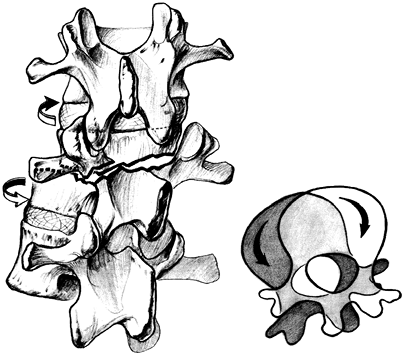
Mechanism of injury.
The superior articular processes of the atlas face upward, inward, and
slightly backward. A vertical compression force can thrust the
articular facets of the occipital condyles of the skull downward, push
the lateral masses outward, and disrupt the ring of the atlas producing
a C1 ring fracture, as shown in Fig. 11-2 (13).
Less commonly, this same mechanism can produce an occipital condylar
fracture, which can be isolated or associated with a basilar skull
fracture (14). -
Anatomic considerations.
The anteroposterior diameter of the ring of the atlas is approximately
3 cm. The spinal cord and the odontoid process each are approximately 1
cm in diameter, approximately one third the diameter of the ring.
According to Steel rule of thirds, the
remaining centimeter of free space allows for some degree of pathologic
displacement. Therefore, anterior displacement of the atlas exceeding 1
cm (the thickness of the odontoid process) threatens the adjacent
segment of cord. This usually occurs with disruption of the transverse
ligament of C1. This ligament maintains the proper relationship of the
dens to C1 and is often ruptured as a pure ligamentous disruption from
a flexion injury. Because the cardiac and respiratory centers lie at
this level, displacement of the atlas threatens the life of the
patient. If the ring of the atlas is capacious (greater than 3 cm in
diameter either as an anatomic feature or as a result of a C1 ring
fracture), there is less danger, whereas if it is narrow and
unfractured, there is more (13). -
History. If
consciousness is not lost as a result of a concurrent head injury, the
history should suggest a mechanism for a vertical compression injury.
The injury often results from a diving accident or any mechanism that
applies axial force to the head. -
Examination.
Clinical symptoms and signs vary from minimal complaints to severe pain
and gross limitation of movement. Extension usually produces some pain,
but rotation may be relatively pain free. Because the suboccipital
nerve crosses the ring posterior to each lateral mass and the greater
occipital nerve emerges just below the posterior ring of the atlas to
supply the skin over the occiput, testing of sensation can show
involvement of the suboccipital or, more commonly, the greater
occipital nerve. Damage to the spinal cord is uncommon because a
significant cord injury at this level causes immediate death. -
Roentgenograms.
Anteroposterior films, including an open-mouth view and a lateral view,
are routine and CT scanning may be indicated. The common fracture sites
are the anterior arch, either midline or just lateral to the midline,
and the posterior arch at its narrowest portion just posterior to each
lateral mass. Displacement of the fracture can be minimal. In an
open-mouth roentgenogram of the odontoid process, when a comminuted
fracture of C1
P.188
shows
bilateral overhang of the lateral masses totaling 7 mm or more, a
rupture of the transverse ligament may have occurred, rendering the
spine unstable (Fig. 11-3).![]() Figure 11-2. Jefferson fracture.
Figure 11-2. Jefferson fracture.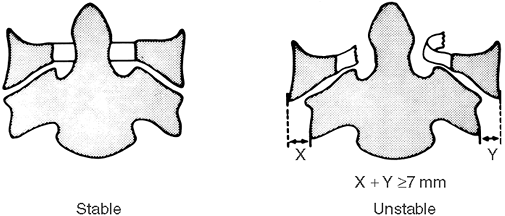 Figure 11-3.
Figure 11-3.
Jefferson fractures. When a comminuted fracture of C1 shows bilateral
overhang of the lateral masses that total 7 mm or more, rupture of the
transverse ligament has probably occurred, rendering the spine
unstable. (From White AA III, Panjabi MM. Clinical biomechanics of the spine. Philadelphia, PA: JB Lippincott, 1978:203, with permission.) -
Treatment.
Treat by immobilization in a cervicothoracic orthosis or halo vest
until healing occurs, usually in 2 to 3 months. Initially, use 5 to 8
lb of tong traction in bed while the extent of the injury is assessed.
Reduction of the fracture is best accomplished by adjusting the
relative position of the head to the thorax. Head extension is required
when the transverse ligament is ruptured (14,15).
-
-
Fracture of the odontoid process (15,16)
-
Mechanism of injury.
The C1 vertebra and the odontoid process of C2 are a single functional
unit. The apical/alar and transverse ligaments on the posterior aspect
of the odontoid process can remain intact following an injury,
producing a fracture of the base of the process. The skull, the C1
vertebra, and the odontoid process of the C2 vertebra then move
relatively independently of the body of the C2 vertebra. -
History.
Symptoms can be minimal, but severe pain behind the ears and stiffness
following a flexion or extension injury are frequent. The patients
often report a feeling of instability at the base of the skull and
present themselves by holding their head with both hands. There is
seldom any suggestion of weakness or numbness of the limbs following an
acute injury. -
Examination. Tenderness in the suboccipital region may be present. The neurologic examination is generally normal.
-
Roentgenograms.
A lateral roentgenogram demonstrates that the C1 vertebra has moved in
relation to C2, and it is also usually seen that the anterior arch of
the C1 vertebra and the odontoid process are in their normal
relationship; that is, the odontoid process has been carried with the
arch of the C1 vertebra (16). Translation of C1
or C2 of 3.0 to 4.5 mm, with neurologic symptoms or signs, can indicate
clinical instability. Normally, the position of the posterior part of
the C1 ring is equidistant between the base of the skull and the
spinous process of C2. An open-mouth anteroposterior roentgenogram
usually shows a fracture line at the base of the odontoid process, and
this fracture line may run inferiorly, possibly involving the upper
part of the vertebral body. The fracture must be differentiated from
congenital etiologies such as a secondary ossification center with an
open apophyseal plate, which may be seen in younger patients, or from a
failure of segments of the odontoid process to fuse to the body of C2,
which may be seen in older patients. With a congenital etiology, the
radiolucency usually is situated more cephalad and is less irregular
than that seen with an acute fracture. In addition, an increased
incidence of
P.189
anomalies
of the anterior arch of C1 and of the atlanto-occipital articulation is
seen with congenital abnormalities of the odontoid process (15,16,17). CT scans are usually helpful. -
Treatment (15,16)
-
Type I is a
fracture through the upper portion of the odontoid process. Treatment
with a cervical orthosis is satisfactory. Nonunion usually presents few
problems because the fracture is too far above the level of the
transverse ligament to cause instability. These fractures are rare. -
Type II is a
fracture at the junction of the dens with the vertebral body of C2.
Reduction of an anteriorly displaced C1 with a fractured odontoid
process can often be achieved by allowing the head to sink into
extension with the patient in a supine position in traction. This
reduction is more easily done by sedating the patient adequately and
inserting a pillow behind the shoulder to allow extension of the head
and neck. Light traction in Gardner-Wells tongs should be applied.
Lateral roentgenograms should be obtained at frequent intervals until
the reduction has been confirmed. Then the head and neck should be
immobilized with the fracture reduced and held in a halo vest without
distraction of the fracture. Apply the orthosis as soon as is feasible
so the patient can sit up and become ambulatory. Immobilization of the
fracture should be continued until the fracture is healed, usually 3 to
4 months; then progressive mobilization of the neck should be
initiated. A soft collar is used until muscle strength has returned.
This fracture is associated with a 15% to 85% incidence of nonunion (15,16,17). -
Type III is
really a fracture through the body of the atlas at the base of the
dens. Treat with very light traction for 2 to 3 days to provide
reduction of the fracture. Follow this with a halo vest that controls
the spine effectively for an additional 12 to 14 weeks. -
Increasingly displaced type II fractures are treated with anterior screw fixation (1).
Although technically demanding, the results are predictable in terms of
fracture union, with rates in the range of 90%. Alternatively,
posterior fusion of C1–C2 with iliac grafting and wiring or screw-based
instrumentation may be considered. In situ
fusion is appropriate if the patient is neurologically intact. Rarely,
a fusion of occiput to C2 is indicated if the fracture is associated
with a C1 ring fracture (unless screw-based instrumentation is
utilized).
-
-
Complications.
As revealed by roentgenography, union of the fracture may not be
achieved in all cases. In a review of 60 odontoid fractures, it was
found that fractures at the junction of the odontoid process with the
body of C2 had a nonunion rate of 36%, which is the usual rate given to
type II fractures (see Anderson and D’Alonzo in Selected Historical Readings).
With type III fractures, only 10% went on to nonunion. It was theorized
that the vertebral body consisted of more cancellous bone, which is
associated with a higher union rate. The use of traction beyond the
first few days is contraindicated because it may produce distraction
and it does not immobilize the fracture. This common practice may
account for the high incidence of nonunion. At 4 months after injury,
flexion and extension films should be obtained. If there is
instability, a posterior C1-C2 fusion should be recommended, although
10% to 15% of neck rotation will be lost (15,16,17).
-
-
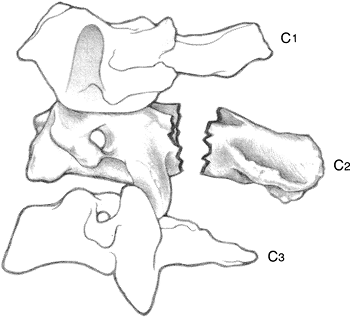
Fracture of C2 vertebra (hangman fracture)
-
Mechanism of injury.
Although the hangman causes this injury by distraction and extension,
the other mechanisms of injury that produce the same fracture seem to
be confusing and indefinite. Patients have remembered “hanging” their
chins on the steering wheel or dashboard or striking their foreheads on
the sun visor of cars involved in accidents. The classic injury is a
bilateral fracture passing through the posterior part of the lateral
masses or pars interarticularis of the axis and into the intervertebral
notch (13). The body of the
P.190
axis is then subluxated or dislocated in relation to the body of C3.
The skull and C1 move as a unit with the body of C2, while the
posterior elements of C2 remain as a unit with the posterior elements
of C3, as shown in Fig. 11-4.![]() Figure 11-4. Classic hangman fracture.
Figure 11-4. Classic hangman fracture. -
Examination.
Involvement of the spinal cord in patients who survive the initial
trauma is relatively uncommon, so the patient may complain of little
more than local pain and stiffness. There is, however, tenderness over
the spinous process of C2. -
Roentgenograms.
Anteroposterior and lateral roentgenograms and tomograms or CT scans
are essential. The retropharyngeal space may be widened on the lateral
view (normal is 4–6 mm at C3). The injury is occasionally accompanied
by other injuries in the lower part of the cervical spine, and these
must be carefully excluded. -
Treatment.
The fracture tends to be reduced with the neck in a neutral position,
but the most appropriate position should be adopted. Halo vest
immobilization should follow a brief 1- to 2-day period of tong
traction and must often continue for 3 months. Traction can produce
distraction and subsequent nonunion or ligamentous instability. If
minimally displaced, a cervical brace (such as a Philadelphia collar)
may be used. The fracture usually heals and primary operative treatment
is unwarranted. -
Complications. Patients rarely require intubation or tracheotomy because of initial severe retropharyngeal swelling.
-
-
Fractures and dislocations of the lower cervical spine (18,19).
In this region of the spine, dislocations without fractures are common,
but fractures and fracture-dislocations do occur. The spinal cord and
nerve roots frequently are involved; in addition to displaced bony
elements, the intervertebral disc can become displaced and function as
the leading “impact force” against the spinal cord (19,20). Injury to the vertebral arteries is not uncommon, particularly with injuries that produce quadriparesis (21).-
Mechanisms of injury
-
Although the effects of a vertical compression
or bursting injury are seen in C1, vertical compression can also
produce injuries lower in the cervical spine. C5 is most commonly
involved with this mechanism. -
An extension injury
produces tearing of the anterior longitudinal ligament with or without
an avulsion fracture of the anterior aspect of one of the vertebral
bodies. Fractures of the pedicles or facets and posterior
P.191
subluxation
can occur. This injury commonly is associated with a rear-end
automobile accident. Subsequent symptoms may last for a prolonged
period of time without objective documentation of any osseous or
soft-tissue abnormalities (see Spence et al. in Selected Historical Readings). -
Flexion injuries
-
A unilateral dislocation or fracture-dislocation
occurs with a dislocation of the facets on one side, with the facets on
the other side remaining intact and in normal relationship to one
another (18). This phenomenon generally occurs in the lower cervical spine, C5–C7. -
Bilateral dislocations or fracture-dislocations
involve the facet joint on both sides. This diagnosis is easier to make
on the lateral cervical roentgenogram because it is associated with
more marked posterior displacement of the upper segment relative to the
lower segment. Because displacement of disc material is common (20),
neurologically intact patients and patients with incomplete spinal cord
injuries should undergo emergent MRI imaging to rule out displacement
of disc material ventral to the spinal cord. -
Examination. Carefully search for bruising, lacerations, or abrasions in the region of the face, forehead, and occiput (22).
Presence and distribution of such lesions often gives an indication of
the mechanism of injury. Assume that any patient with facial or
forehead lacerations who has been involved in a high-speed impact has a
cervical spine fracture until proven otherwise. Local examination of
the neck reveals tenderness over one or more spinous processes, and
there is limitation of movement and muscle spasm. The examination must
include a careful neurologic assessment. It is not enough to decide
whether there is evidence of cord damage. The level of a neurologic
lesion must be accurately defined by both motor and sensory
examinations as well as pathologic reflexes and must be recorded with
the time and date, preferably in a flow-sheet format. Patients must be
reexamined frequently in the first 24 hours after injury, especially
those with incomplete spinal cord injury (19,22,23). -
Initial treatment.
Whether or not neurologic damage is present, reduction of any
displacement should be undertaken. To reduce and treat the fracture
properly, however, the fracture pattern must be understood. This
usually is best assessed by attempting to understand the mechanism of
injury as well as through high-quality roentgenograms. The suggested
method for reduction of dislocations or fracture–dislocations, whether
unilateral or bilateral, is with skull tongs inserted as described in Chap. 9, V.B.
It is prudent to be sure that disc material has not been displaced into
the spinal canal with a prereduction MRI, especially with bilateral
facet dislocations in a neurologically intact individual. While awake
closed reduction despite disc herniation has been successful in certain
cases (24); some patients may require anterior decompression surgery prior to reduction. -
The patient is placed in skull tong traction, usually with 15 lb of weight. Use traction in the direction of the deformity,
not in line with the patient’s body. The weight may be gradually
increased by 5 lb every hour. Obtain lateral roentgenograms every 30 to
60 minutes. Record a neurologic examination at 30-minute intervals.
With a unilateral facet dislocation, after 60 lb (or one third of body
weight) of traction force has been applied, then consider bending the
head away while rotating the upper neck toward the side of the
dislocation. Reduction should be achieved rapidly by this method; then
the weight may be decreased to 5 lb. If reduction is not achieved
rapidly or if the dislocation is old, then consultation with an
experienced spinal surgeon is important because it may be necessary to
proceed with an operation to achieve reduction. Reduction of the
fracture or fracture-dislocation is the best and safest method of
achieving decompression of the spinal cord or roots (19). Laminectomy is contraindicated because it may produce increased instability while adding surgical trauma. -
Management after reduction
is through immobilization by light tong traction for several days with
the neck in the optimum position as demonstrated by lateral
roentgenograms. In the absence of significant neurologic deficit, the
patient may then be placed in a halo vest. If extensive neurologic
deficit is present, then immobilization in bed may be necessary. To
avoid the complications of bed rest (e.g., pneumonia, urinary stasis,
and bed sores), operative stabilization is frequently indicated. Deep
venous thrombosis prophylaxis must be used because of the very high
rates of this complication in spinal cord–injured patients (25).
In unstable injuries, it is wise to use a halo apparatus. Other types
of cervical orthoses occasionally are used but are not as effective as
the halo apparatus and are reserved for stable injuries. For unstable
injuries, surgical stabilization and early mobilization of the patient
is almost always indicated (19).-
Posterior cervical fusion is recommended for most patients with bilateral facet dislocations.
If reduction has been achieved by tong traction, then surgery is
usually delayed 5 to 7 days to avoid the neurologic deterioration that
can occasionally occur in quadriplegic patients. As noted earlier,
before reduction and before surgery, the location of the intervertebral
disc must be determined by CT scanning, myelography, or MRI. If the
disc is retropulsed into the canal, then anterior decompression may be
required prior to posterior surgery. -
The treatment of a unilateral facet dislocation is controversial (17).
Many consultants recommend treatment in a halo vest following reduction
in tong traction. Other authors recommend posterior cervical fusion for
this condition because anatomic alignment can then be maintained.
-
P.192 -
-
-
-
The hyperextension whiplash injury
-
The mechanism of injury is similar to that for the cervical spine extension injuries described in D.1.b.
-
Likewise, the history is similar; for example, the patient was an occupant in a car that was suddenly struck in the rear by another automobile.
-
The examination shows tenderness along the scalene muscles and within the body of the trapezius muscle.
-
In a pure soft-tissue injury without tearing of the anterior longitudinal ligament, the roentgenograms are normal.
-
Recommended treatment
for the first 10 to 14 days includes a properly sized soft collar to
immobilize the neck, sufficient analgesics for pain relief, and rest.
Soft collars are preferable to rigid collars for comfort. Collars
should be high posteriorly and low under the chin to keep the cervical
spine in a neutral or slightly flexed position. Avoid hyperextension in
whiplash injuries and cervical radiculopathy. Cold packs may be used
for the first 24 hours, followed by warm packs. A folded towel can be
used as a neck collar. Ice may be placed within the towel initially;
then a damp warm towel may be used. Corticosteroid injection of the
facet joints has not been proven to be effective in a randomized
controlled trial (26). -
The long-term prognosis for these injuries was reported as follows: 43% of the patients had residual symptoms 5 years after injury (see Hohl in Selected Historical Readings).
There were degenerative changes in 39% of the patients. A poorer
prognosis was predicted if shortly after injury the following findings
were present:-
Pain or numbness in an upper extremity
-
Sharp reversal of the cervical lordosis as seen on the roentgenograms. This is not a completely reliable sign.
-
Restricted motion
at one interspace as seen in flexion-extension roentgenograms; these
should not be obtained until 3 weeks after injury to improve their
sensitivity in detecting instability. -
Need for a cervical collar for more than 12 weeks or for home traction.
-
Need to resume physical therapy more than once because of recurrence of symptoms.
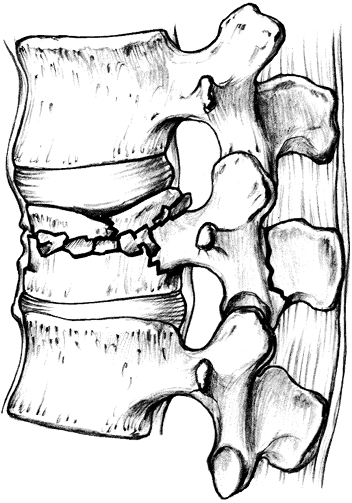
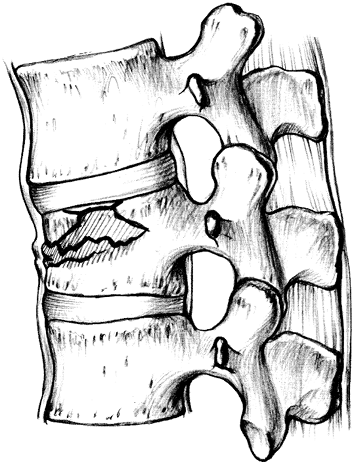 Figure 11-5. Compression fracture of the thoracolumbar spine. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:216, with permission.)
Figure 11-5. Compression fracture of the thoracolumbar spine. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:216, with permission.)
-
-
-
Fractures and fracture-dislocations of the thoracic, thoracolumbar, and lumbar spine. Denis improved upon Holdsworth concepts to develop the three-column theory for thoracolumbar fractures (27). McAfee has shown the utility of using CT to classify fractures to aid in treatment decisions (28).
-
Types of injury (28)
-
Compression fracture (Fig. 11-5).
A wedge compression fracture of the vertebral body is produced by a
flexion force, but the posterior ligament complex (i.e., supraspinous
ligaments, interspinous ligaments, ligamenta flava, and capsules of the
intervertebral joint) remains intact. There is no fracture of the
posterior elements. Kyphotic angulation (as measured by the angle
between lines drawn from the end plates of the injured vertebrae to
those of the adjacent uninjured vertebra) is usually less than 10
degrees, and loss of anterior vertebral height is no greater than 40%.
Therefore, this injury is classified as relatively stable but requires
close observation for progressive kyphotic deformity. -
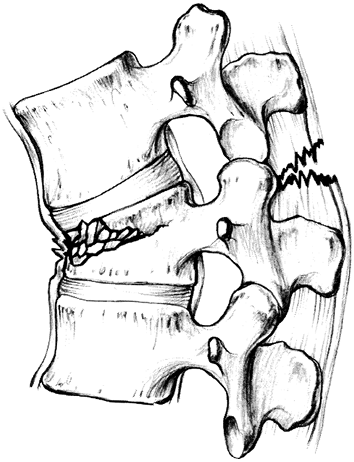
Stable burst fracture (Fig. 11-6).
Burst fractures of the thoracolumbar spine are generally stable. By
reviewing the plain roentgenograms and CT scan, the anterior and middle
columns are parted with bone retropulsed into the spinal cord, but the
posterior column is uninjured (the facet joints and ligaments are
intact). Kyphosis is limited to 15 degrees and loss of vertebral height
is less than 50%. These patients are neurologically intact. -
Unstable burst fracture (Fig. 11-7).
In these injuries, the posterior column is disrupted as well. The
hallmark is pedicle widening on the anteroposterior roentgenogram. The
amount of neurologic injury varies based more on the level of the
injury than the degree of canal compromise by bone fragments. One must
remember that the spinal cord ends at L2, and
P.194
fractures
above this level have greater neurologic involvement. Stenosis of 80%
is tolerated well below this level, whereas stenosis of 30% in the
thoracic spine may be associated with paraplegia.![]() Figure 11-6. Stable burst fracture. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993: 217, with permission.)
Figure 11-6. Stable burst fracture. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993: 217, with permission.) -
Flexion-distraction injury (Fig. 11-8).
These injuries result from failure of the posterior elements in tension
while the anterior and middle columns are compressed. The most common
mechanism is a lap belt in a motor vehicle accident. On the lateral
roentgenogram, widening of the spinous processes is seen. The vertebral
body is wedged anteriorly and occasionally a small fragment of bone is
retropulsed into the canal. The neurologic injury is variable. -
Chance fracture (Fig. 11-9).
Generally, these fractures result from tension failure of all spinal
bony elements as a result of hyperflexion over a secured lap belt.
These injuries, which commonly occur in back seat passengers, are seen
frequently in children. Bowel injuries occur in up to 65% of these
patients because the lap belt provides the fulcrum against the
abdominal wall (29). The injury can be
ligamentous, bony, or both, but there is no compromise of the anterior
elements if the injury is primarily ligamentous. Most often surgery is
indicated. -
Translational injuries (Fig. 11-10)
are caused by shear forces that fracture or dislocate the facets.
Paraplegia is generally the result. Anteroposterior translation of the
vertebral bodies is present on the roentgenograms. Surgical
stabilization is generally advisable.
-
-
Diagnosis.
The diagnosis is suspected from the mechanism of injury or, in the
elderly patient, following a sudden jolt or fall. Tenderness to
palpation or
P.195P.196
percussion over the involved segment is common. Hematomas and gaps between spinous processes may be palpable.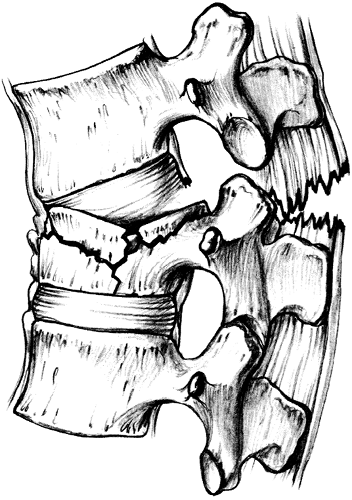 Figure 11-7. Unstable burst fracture. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993: 218, with permission.)
Figure 11-7. Unstable burst fracture. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993: 218, with permission.)![]() Figure 11-8. Flexion-distraction injury. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:219, with permission.)
Figure 11-8. Flexion-distraction injury. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:219, with permission.)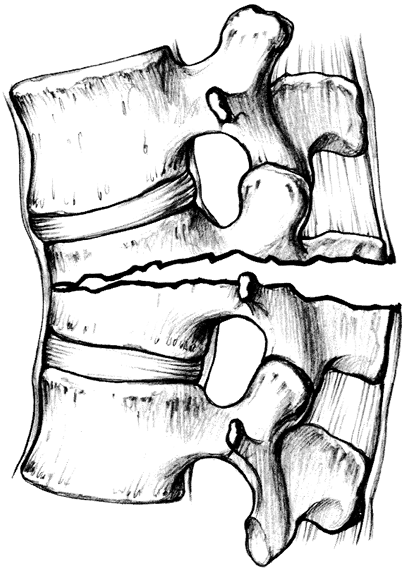 Figure 11-9. Chance fracture. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:221, with permission.)
Figure 11-9. Chance fracture. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:221, with permission.) -
Examination.
On initial examination, a neurologic assessment must be completed. If a
sensory level is detected, mark it on the chart and on the trunk with
the time and date of examination. If there is any motor deficit, then
record it on a simple muscle chart. It is sufficient to record function
of muscle groups rather than of individual muscles. A drawing of the
patient can be helpful to illustrate pertinent neurologic findings. A
flow sheet is another useful device to document changes in the
neurologic status over time. -
Roentgenograms.
Excellent quality anteroposterior and lateral films are required, and
CT scans often are indicated to evaluate the posterior elements and to
assess stability (28). The pattern of injury
must be accurately determined. If there is neurologic involvement and
the roentgenograms and CT scans do not reveal a fracture, MRI is
indicated. This study identifies herniated disc material or hematoma as
the cause of the deteriorating neurologic examination (30,31). -
Treatment. Logroll the patient on a firm mattress until stability of the fracture is assessed.
-
Minor fractures
-
Bed rest on a
firm bed for a few days with light analgesia is usually all that is
required. Patients may be turned in a logrolling fashion
P.197
every 2 to 4 hours. An off-the-shelf Jewett brace or Risser cast is generally used for 12 to 16 weeks.![]() Figure 11-10. Translational injuries. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:222, with permission.)
Figure 11-10. Translational injuries. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:222, with permission.) -
Paralytic ileus
tends to develop, particularly in patients with lumbar compression
fractures. This development should be anticipated and the patient
should take nothing by mouth until normal bowel activity is ensured; IV
fluid maintenance is required. -
As soon as the patient is comfortable in a cast or brace, start extension exercises
to strengthen the thoracic and lumbar spinal extensor muscles. As soon
as good muscle control is obtained, the patient may be allowed to
ambulate. -
Lifting or flexion activities should be avoided for 3 months.
-
-
Major fractures or fracture-dislocations.
Spinal fractures can be missed in unconscious obtunded patients;
complete spine films must be obtained and carefully scrutinized (32).
In a severe anterior compression fracture with a marked kyphosis,
reduction with some type of posterior instrumentation such as a
rod/hook or rod/pedicle screw construct may be indicated. Otherwise, stable fractures
rarely require operative intervention. In a prospective, randomized
study comparing operative and nonoperative treatment of stable
thoracolumbar burst fractures in patients without neurologic deficits,
investigators found no significant difference between the two groups
with respect to return to work, pain scores, spinal deformity, or
health-related quality of life, although complications were more
frequent in the operative group (29). Accordingly, most of these patients should be managed in a well-fitting hyperextension cast or suitable
P.198
orthosis. Unstable fractures should be evaluated for stabilization with appropriate instrumentation by a spine surgeon trained in the use of these devices (27,31,33).-
Stable fractures without neurologic deficit
include most compression injuries and burst fractures resulting from
vertical compression forces. Place the patient on strict bed rest until
the pain is reduced sufficiently to allow an active exercise program.
When good muscle function has been restored, the patient can be
mobilized in a plaster or plastic body jacket or a suitable brace.
Minor degrees of compression should be treated as are compression
fractures elsewhere (see F.5.a). -
Unstable injuries without neurologic involvement.
The most common of these injuries is the unstable burst type. If
nonoperative treatment is selected, then provide external
immobilization for 12 to 16 weeks, depending on the fracture pattern
and physical build of the patient (29,34).
Mild paresthesias or dysesthesias can be seen in this type of injury
without other neurologic symptoms or signs; these do not constitute an
indication for immediate operation. Consider operative intervention if
motor, reflex, or sensory deficits develop. If significant deformity is
likely, then surgery is generally recommended. -
Unstable injuries with progressive neurologic damage.
This is one condition for which surgeons agree that reduction,
decompression of the neural elements, and internal stabilization is
required (31). Methylprednisolone therapy is recommended (12,35). -
Unstable injuries with incomplete neurologic deficit.
Treat these cases with a logrolling frame while the neurologic lesion
is assessed. If it worsens or remains the same, then consider treatment
as noted in the preceding paragraph. If it is improving, then no
operative intervention for the lesion is needed, but the fracture
instability should be evaluated to determine whether operative
stabilization or early mobilization in a cast or custom plastic body
jacket is the method of choice. Parenteral steroid therapy may also be
indicated. -
Unstable fractures with complete neurologic deficit.
If paraplegia is immediate and complete and there is no evidence of
return of function within 48 hours, then early operative stabilization
should be considered to allow earlier rehabilitation.
-
-
Indications for immediate operation
-
An advancing or progressive neurologic deficit
-
Paraplegia in the absence of bony injury and in the presence of a complete block as revealed by MRI or myelography, which may indicate an acute traumatic disc prolapse or hematoma
-
Severe root pain from root compression at the level of the injury another indication for exploration but seldom requiring immediate operation
-
-
-
-
Fractures of the transverse process in the lumbar spine.
These fractures can result from different mechanisms of injury and
should be treated symptomatically. Patients tend to have significant
pain and require heavier analgesia. Consider and rule out associated
renal injury with screening urinalysis and CT scan if indicated.
-
Pseudosubluxation.
Subluxation of the vertebral body of C2 on C3 may be difficult to
evaluate in a child who has sustained neck trauma because this may
present as a normal variant. Careful evaluation of the posterior
intralaminar line (the line of Swischuk) may help differentiate
physiologic subluxation from pathologic subluxation. An intact
posterior intralaminar line is characteristic of pseudosubluxation. -
Disproportionate head-to-torso ratio. Because children up to 6 years of age have a disproportionately larger head size than older children and adults, supine
P.199
positioning on a firm surface results in a slightly flexed position of
the cervical spine. To lessen the potential for associated neurologic
injury or difficulties in interpretation of imaging studies, the torso
should be elevated on padding in order to produce a neutral position of
the cervical spine. -
Spinal cord injury without radiographic abnormality (SCIWORA).
Due to the relative elasticity of the bone and soft tissues in
children, significant disruption and displacement of the soft tissues
can occur at the time of injury, without bony injury. An MRI scan
identifies the soft tissue or hematoma associated with the injury. In a
review of 159 pediatric patients with acute spinal cord or vertebral
injuries, 26 (16%) sustained SCIWORA (36). The
mechanism of injury, its severity, and the prognosis for recovery were
related to the patient’s age. In young children, SCIWORA accounted for
32% of all spinal injuries and tended to be severe, while in older
children, SCIWORA accounted for only 12% of the spinal injuries and had
an excellent prognosis for complete recovery of neurologic function.
CC, Mann FA, Wilson AJ. Helical CT in the primary trauma evaluation of
the cervical spine: an evidence-based approach. Skeletal Radiol 2000;29: 632–639.
DB Jr, Zuluaga A, Fuentes-Bernardo DA, et al. Cervical spine trauma:
how much more do we learn by routinely using helical CT? Radiographics 1996;16:1307–1318; discussion 18–21.
JW, Kaups KL, Cunningham MA, et al. Routine evaluation of the cervical
spine in head-injured patients with dynamic fluoroscopy: a reappraisal.
J Trauma 2001;50:1044–1047.
FH, Dorsey FC, Coleman WP. Recovery of motor function after spinal-cord
injury a randomized, placebo-controlled trial with GM-1 ganglioside. N Engl J Med 1991;324:1829–1838.
MB, Shepard MJ, Collins WF Jr, et al. Methylprednisolone or naloxone
treatment after acute spinal cord injury: 1-year follow-up data.
Results of the second national acute spinal cord injury study. J Neurosurg 1992;76:23–31.
MB, Shepard MJ, Holford TR, et al. Administration of methylprednisolone
for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment
of acute spinal cord injury. Results of the third national acute spinal
cord injury randomized controlled trial. National acute spinal cord
injury study. JAMA 1997;277: 1597–1604.
HH, Anderson PA. Anterior decompression and arthrodesis of the cervical
spine: long-term motor improvement. Part I Improvement in incomplete
traumatic quadriparesis. J Bone Joint Surg Am 1992;74:671–682.
L. Initial evaluation and emergency treatment of the spine-injured
patient. In: Browner B, Jupiter JB, Levine AM, eds. Skeletal trauma, 2nd ed. Philadelphia, PA: WB Saunders, 1992:745–768.
AR, Falatyn SP, Flanders AE, et al. Magnetic resonance evaluation of
the intervertebral disc, spinal ligaments, and spinal cord before and
after closed traction reduction of cervical spine dislocations. Spine 1999;24:1210–1217.
L, Lord SM, Wallis BJ, et al. Lack of effect of intraarticular
corticosteroids for chronic pain in the cervical zygapophyseal joints. N Engl J Med 1994;330: 1047–1050.
PC, Yuan HA, Fredrickson BE, et al. The value of computed tomography in
thoracolumbar fractures. An analysis of one hundred consecutive cases
and a new classification. J Bone Joint Surg Am 1983;65:461–473.
K, Buttermann G, Mehbod A, et al. Operative compared with nonoperative
treatment of a thoracolumbar burst fracture without neurological
deficit. A prospective, randomized study. J Bone Joint Surg Am 2003;85-A:773–781.
RB, Sherman JE, Carr JB. 1991 Volvo Award in experimental studies.
Cauda equina syndrome: neurologic recovery following immediate, early,
or late decompression. Spine 1991;16:1022–1029.
MB, Shepard MJ, Collins WF, et al. A randomized, controlled trial of
methylprednisolone or naloxone in the treatment of acute spinal-cord
injury. Results of the second national acute spinal cord injury study. N Engl J Med 1990;322:1405–1411.
CA, Zabramski JM, Hadley MN, et al. Pediatric spinal cord injury
without radiographic abnormalities: report of 26 cases and review of
the literature. J Spinal Disord 1991;4:296–305.
JH, Harrington PR, Erwin WD. Results of reduction and stabilization of
the severely fractured thoracic and lumbar spine. J Bone Joint Surg (Am) 1978;60:799.